Abstract
The evolution of white blood cells after ST elevation myocardial infarction (STEMI) and their association with infarct size and major adverse cardiac events (MACE) remains unclear. Two hundred eleven patients underwent CMR after STEMI. Infarct mass (grams) was determined. Neutrophil, lymphocyte, and monocyte counts (×1,000 cells/ml) were measured upon arrival and at 12, 24, 48, 72, and 96 h. Patients with large infarctions (3rd tertile ≥ 28.5 g vs. 1st and 2nd tertiles < 28.5 g) showed a larger neutrophil count at 12 h (14.8 ± 4.8 vs. 11.4 ± 3.3, p < 0.0001) and an increased monocyte count (maximum at 24 h (0.65[0.50–0.91] vs. 0.55[0.42–0.71], p = 0.004)) but no difference in lymphocyte count. Neutrophil count at 12 h independently predicted large infarctions (OR 1.14, 95%CI [1.04–1.26], p = 0.008). During follow-up (median 504 days), 25 MACE occurred. Neutrophil count at 96 h independently predicted MACE (HR 1.2, 95%CI [1.1–1.4], p = 0.003). Large infarctions show a marked neutrophil peak and an increasing monocyte count. Neutrophil count independently predicts large infarctions and MACE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Elevated white blood cell count in ST segment elevation myocardial infarction (STEMI) is associated to adverse outcome [1, 2]. Larger infarct size and microvascular obstruction have been suggested as the mechanisms underlying this association [1–6].
The pathophysiological role and the temporal evolution of white blood cells during the first hours and days after STEMI have not been completely unraveled yet. Most studies addressing this question have been based on single measurements of total white blood cell count at baseline.
Cardiovascular magnetic resonance (CMR) allows for a state-of-the-art analysis of post-infarct patients, including accurate assessment total infarct mass, the extent of transmural necrosis, and microvascular obstruction. The relationship between the temporal evolution of white blood cell subtypes and CMR-derived infarct mass as well as the association with adverse outcome during follow-up have not been well-defined.
For that purpose, we evaluated the relationship between the temporal evolution of white blood cell subtypes within the first hours and days after a first STEMI with CMR-derived infarct mass. Further, we assessed the value of white blood cell subtypes for predicting major adverse cardiac events (MACE) during follow-up.
Materials and Methods
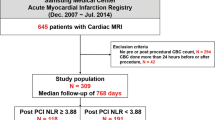
We prospectively included 267 consecutive patients admitted to a university hospital for a first STEMI treated with reperfusion therapy. Stable clinical course during the first week, no contraindication to CMR, and no condition related to leucocytosis apart from the index myocardial infarction were inclusion criteria.
We excluded 56 patients due to death (12 cases), re-infarction (seven cases), clinical instability precluding CMR (15 cases), claustrophobia (five cases), cardiac surgery (two cases), infections (nine cases), corticoids treatment (five cases), and leukemia (one case). Therefore, the final study group comprised 211 patients.
The local ethics committee approved the research protocol. Informed consent was obtained from all subjects.
Blood Samples and ECG
Neutrophil, lymphocyte, and monocyte counts (×1,000 cells/ml) were determined upon patient arrival and at 12, 24, 48, 72, and 96 h after revascularization by an automated blood cell counter.
Creatine kinase MB mass (nanograms per milliliter) was immunologically measured (Immulite assay, Diagnostic Products Corporation, Los Angeles, CA, USA) in at least six consecutive blood samples over the first 72 h. The maximum creatine kinase MB mass value was determined.
The percentage of sum of ST segment resolution 90 min after reperfusion was determined. Complete ST segment resolution was regarded for a resolution >70%.
Cardiac Catheterization
The infarct-related artery was the left anterior descending artery in 125 patients (59%), the right coronary artery in 72 (34%), and the left circumflex artery in 14 (7%).
The reperfusion strategy was left to the discretion of the attending cardiologists: 125 patients (59%) were treated with thrombolysis and 86 (41%) were submitted to primary percutaneous revascularization. Time from chest pain onset to reperfusion was recorded.
Out of 125 patients treated with thrombolytic agents, rescue angioplasty was carried out within the first 3 h after thrombolytic administration in 27 patients (22%). In the remaining 98 patients treated with thrombolytic agents, cardiac catheterization was performed at least 24 h after myocardial infarction.
Overall, 176 patients (83%) were treated with a stent: 74 in the context of primary percutaneous revascularization and 102 in the routine cardiac catheterization after thrombolysis.
Thrombolysis In Myocardial Infarction (TIMI) flow in the initial and final angiographies, as well as myocardial blush grade in the final angiography, were determined offline by an experienced observer unaware of CMR results using the standard software (Integris HM3000, Philips, Best, The Netherlands). TIMI 3 flow and myocardial blush grade 2–3 were regarded as normal [7].
CMR
CMR (1.5-T scanner, Sonata Magnetom, Siemens, Erlangen, Germany) was performed 9 ± 6 days (at least 48 h after cardiac catheterization) after myocardial infarction according to our laboratory protocol [8, 9]. All images were acquired by a phased-array body surface coil during breath-holds and were electrocardiogram-triggered.
Cine images (steady-state free precession sequence, repetition time/echo time = 3.2/1.6 ms, flip angle = 61°, matrix = 256 × 128, slice thickness = 6 mm, temporal resolution = 26 ms) were acquired in 2-, 3-, 4-chamber views and every 1 cm in short-axis views.
Late enhancement imaging was performed at least 10 min after administering 0.1 mmol/kg of gadolinium-diethylenetriaminepentaacetic acid (Magnograf, Juste S.A.Q.F., Madrid, Spain) at a flow rate of 3 ml/s. A segmented inversion recovery steady-state free precession sequence was used (repetition time/echo time = 2.5/1.1 ms, slice thickness = 6 mm, flip angle = 50°, matrix = 195 × 192) nullifying myocardial signal.
CMR Data Analysis
CMR studies were analyzed by two experienced observers blinded to all patient data using customized software (QMASS MR 6.1.5, Medis, Leiden, The Netherlands). Segments location was defined applying the 17-segment model [10].
End-diastolic and end-systolic volume indexes (ml/m2), ejection fraction (percent), and left ventricular mass (grams) were quantified by manual definition of endocardial borders of all short-axis slices in cine images.
In late enhancement imaging, all short-axis view slices were separately analyzed, and the presence of late enhancement was quantitatively defined as the presence of a signal intensity >2 standard deviations in comparison with a remote non-infarcted area in the same slice [9]. Infarct mass (grams) and the number of segments showing transmural necrosis (>50% of wall thickness) were determined (Fig. 1).
Microvascular obstruction was visually defined as a lack of contrast uptake in the core of a segment surrounded by tissue showing late enhancement. The number of segments showing microvascular obstruction was determined.
In our institution, inter- and intra-observer variability for all CMR indexes analyzed in the present study were <5%.
End-Points and Follow-Up
The end-points of the study were large infarct size and MACE.
Patients were categorized according to tertiles of infarct mass (T1 < 15.6 g,T2 = 15.7–28.4 g, T3 ≥ 28.5 g). Patients in the 3rd tertile were considered to have large infarctions and were compared with the two lower tertiles.
MACE consisted of cardiac death, admission for nonfatal myocardial infarction [11], or for heart failure [12], whichever occurred first. Three cardiologists reviewed all events, and consensus was required to designate a MACE.
Statistical Analysis
Data were tested for normal distribution using the Kolmogorov–Smirnov test.
Parametric variables were expressed as the mean ± standard deviation and compared using Student’s t test. Nonparametric variables were expressed as the median with the interquartile range and compared using the Mann–Whitney U test. Group percentages were compared using the chi-square test or Fisher’s exact test where appropriate.
We determined the independent value of white blood cell subtypes (neutrophils, lymphocytes, and monocytes) for predicting large infarctions using a forward logistic regression model adjusted for baseline and angiographic characteristics if they had a p value <0.05 in the univariate analyses. Odds ratios (OR) with the respective 95% confidence intervals (95% CI) were computed.
The association of white blood cell subtypes with time to MACE was assessed by means of a Cox proportional hazard regression model using stepwise multivariate procedures adjusted for baseline, angiographic, and CMR characteristics yielding a p < 0.05 in the univariate analyses. Traditional risk factors were also included in the model. Hazard ratios (HR) with the corresponding 95% CI were computed.
Survival distributions for the time to event were estimated with the Kaplan–Meier method and compared using the log-rank test.
For dichotomic analysis of white blood cell subtypes, cutoff values were derived from ROC curve analysis by maximizing the observed overall diagnostic accuracy (minimizing the number of false positives plus the number of false negatives).
Statistical significance was considered for two-tailed p value <0.05. SPSS 13.0 (SPSS Inc, Chicago, IL, USA) was used.
Results
Evolution of White Blood Cells after STEMI
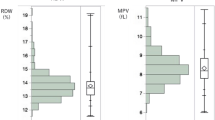
The baseline and CMR characteristics of the 211 patients included in the study are shown in Table 1. For angiographic parameters, see online Supplementary Table 1. The evolution of white blood cell subtypes is displayed in Fig. 2. Characteristically, neutrophil count peaked in the first measurement (12 h) after revascularization. Conversely, a marked drop in lymphocyte count could be observed at that time point. Monocyte count steadily increased in the days after STEMI reaching a maximum at 48 h after revascularization (Fig. 2).
Evolution of white blood cells after reperfused ST elevation myocardial infarction. Temporal evolution of white blood cells (×1,000 cells/ml) in the whole study group; a neutrophils, b lymphocytes, c monocytes. Neutrophil counts are expressed as the mean ± standard deviation. Lymphocyte and monocyte counts are expressed as the median with the interquartile range.
Association of White Blood Cells with Infarct Mass
The characteristics of patients with and without large infarctions are displayed in Table 1 and online Supplementary Table 1. The evolution of white blood cell subtypes after STEMI according to infarct size is displayed in Fig. 3.
Evolution of white blood cells according to infarct size. Temporal evolution of white blood cells (×1,000 cells/ml) according to infarct size (large infarction vs. smaller infarction); a neutrophils, b lymphocytes, c monocytes. Neutrophil counts are expressed as the mean ± standard deviation. Lymphocyte and monocyte counts are expressed as the median with the interquartile range. MI myocardial infarction.
Patients with large infarctions had a significantly higher neutrophil count on arrival and at all measurements after revascularization with a marked peak at 12 h after revascularization. There was no significant difference in lymphocyte count between both groups. Monocyte count steadily increased and from 12 h after revascularization, patients with large infarctions displayed a significant higher monocyte count compared to patients with smaller infarctions until 96 h after revascularization.
A multivariate logistic regression analysis, adjusted for baseline characteristics, angiographic parameters, and white blood cell subtypes for prediction of large infarction, was performed. Neutrophil count at 12 h after revascularization was the only white blood cell subtype independently associated with large infarctions (OR 1.14, 95%CI [1.04–1.26], p = .003, per each 1,000 cells/ml increase). Anterior infarction, peak creatinine kinase MB and ST segment resolution >70% were also independent predictors of large infarctions (Table 2).
Association of White Blood Cells with MACE
During follow-up (median 504; range [168–1,043] days), 25 MACE (six cardiac deaths, five nonfatal myocardial infarctions, and 14 readmissions for heart failure) occurred. Baseline characteristics, angiographic, and CMR parameters related to MACE are shown in Table 3. For angiographic characteristics, see online Supplementary Table 2.
The evolution of white blood cell subtypes after STEMI according to MACE is displayed in Fig. 4. Patients with MACE showed a similar pattern of white blood cell subtypes evolution after revascularization as did patients with large infarctions.
Evolution of white blood cells according to major adverse cardiac events. Temporal evolution of white blood cells (×1,000 cells/ml) according to major adverse cardiac events during follow-up; a neutrophils, b lymphocytes, c monocytes. Neutrophil counts are expressed as the mean ± standard deviation. Lymphocyte and monocyte counts are expressed as the median with the interquartile range. MACE major adverse cardiac events.
In a multivariate analysis, adjusted for baseline, angiographic, and CMR characteristics as well as traditional risk factors (male gender, age, diabetes, hypertension), neutrophil count at 96 h after revascularization was the only white blood cell subtype independently related to MACE (HR 1.2, 95% CI [1.1–1.4], p = .003, per 1,000 cells/ml increase) during follow-up. Previous coronary artery disease and the number of segments showing transmural necrosis were also related to MACE during follow-up. Results and variables tested in the multivariate analysis are shown at the foot of Table 4.
Neutrophil count at 96 h after revascularization was the only white blood cell subtype related to MACE. Using ROC curve analysis, patients were categorized according to the best cutoff of neutrophil count at 96 h for predicting MACE (≤5.1 vs. >5.1 × 1,000 cells/ml). Using this cutoff, 67% of patients displayed a high neutrophil count at 96 h.
High neutrophil count at 96 h was associated with a higher probability of MACE, cardiac death, and readmission for heart failure but not reinfarction during follow-up (Fig. 5). Accordingly, patients with elevated neutrophil count at 96 h displayed significantly higher rates of MACE, cardiac death, and readmission for heart failure but not reinfarction (Table 5).
Discussion
The present study shows that distinctive patterns in the temporal evolution of white blood cell subtypes can be observed according to infarct size after STEMI.
Patients with large infarctions and with MACE during follow-up display higher neutrophil counts after revascularization and an increasing monocyte count over time while no difference in lymphocyte count between the two groups could be detected.
Neutrophil count after revascularization independently relates to both CMR-derived infarct mass and MACE during follow-up.
Neutrophils
A vast body of experimental and clinical data supports the role of pro-inflammatory cells in the development of microvascular and myocardial injury after infarction, mainly involving neutrophils [1, 3, 6]. CMR represents the state-of-the-art technique for a comprehensive evaluation of patients after myocardial infarction with accurate assessment of infarct size [8, 9, 13]. This study demonstrates a relationship of neutrophil count with CMR-derived infarct size and with MACE during follow-up.
Neutrophils seem to be attracted to the ischemic myocardium by complement components. Thereafter, cell-surface adhesion molecules mediate endothelial rolling, adhesion, and plugging, playing an important role on microvascular obstruction, hypoxia, and indirect necrosis of myocytes. After transendothelial migration, adherence to cardiac myocytes stimulates oxidative and direct cell injury [1, 6].
In our study group, patients with large infarctions presented with significantly elevated neutrophil count and displayed a sharp boost in the first blood sample after revascularization and significantly higher values throughout all measurements. Moreover, in a multivariable analysis adjusted for baseline characteristics and angiographic parameters, neutrophil count at 12 h after revascularization was the only white blood cell subtype independently related to large infarctions.
Nevertheless, we cannot definitively discern whether a higher neutrophil count is a contributor to or merely a consequence of a wider myocardial damage. Experimental data have shown that a drastic reduction in infarct size is observed after depletion of neutrophils, supporting the concept of the primary role of these cells on myocardial and microvascular injury [1, 6].
The observation that neutrophil count displayed a decrease onwards from 12 h might explain why several therapeutic options aiming at blockade of neutrophils have only been effective in the experimental area but not in the clinical field [14]. Indeed, an early and fast block of neutrophil effects immediately after the onset of myocardial infarction is only possible under experimental conditions advocating other inflammatory targets for further investigation.
Although neutrophils are the first leucocytes to be found in damaged tissue, they are removed from myocardial tissue after phagocytosis of cellular debris and do not appear to play a further role in subsequent infarct healing [4, 5, 15]. The sharp but transient rise of neutrophil count detected in our study group supports this concept.
Elevated white blood cell count in STEMI is associated to adverse outcome [1, 2]. In the present study, patients with MACE displayed an elevated neutrophil count at all time points after revascularization, and there was an independent association of neutrophil count at 96 h after revascularization and prognosis even adjusted for strong prognosticators as infarct mass.
In a separate analysis, this study shows that a higher neutrophil count (>5.1 × 1,000 cells/ml) at 96 h after revascularization was significantly associated with cardiac death and readmission for heart failure but was not associated with reinfarction. A possible explanation for this finding is that these patients display larger infarctions with little viable myocardium left in the infarcted territory as the substrate for reinfarction.
Monocytes
Monocytes are transformed into macrophages and outnumber neutrophils at two to three days after infarction. Monocytes play a major role in tissue repair after myocardial infarction, and monocyte-related cytokines stimulate healing processes and promote peripheral monocytosis [5].
We detected a steady increase in monocyte count over the first 96 h in both small and in large infarctions, but patients with large infarctions displayed significantly higher monocyte counts after revascularization.
Few studies have analyzed the relationship between the temporal evolution of monocyte count and infarct size. High monocyte count has been linked to depressed left ventricular ejection fraction and remodeling [5] and to a lower degree of systolic recovery [4] after myocardial infarction. The results of our study are in line with these previous results by showing that high monocyte counts relate to larger infarctions.
Lymphocytes
The prevailing theory, that organ failure in stress situations like sepsis or trauma results from an uncontrolled inflammatory response, has been recently challenged [16, 17]. It has been suggested that after a short hyperinflammatory period, the body’s normal stress response is activation of lymphopenia-mediated anti-inflammatory mechanisms. However, prolonged depression of immune function can culminate in organ failure and death [16].
Lymphocytes can be defined as the strategists of the immune system. Via cytokines, they regulate important intermediate steps responsible for a pro-coagulant milieu that finally might lead to vascular plugging and obstruction of the microvasculature [18]. We have recently demonstrated that severe lymphopenia following STEMI is associated with microvascular obstruction [19].
In the present study, we observed a drop in lymphocyte count regardless of infarct size. This observation supports the hypothesis that, confronted with a potent pro-inflammatory stimulus such as myocardial infarction, the body might respond with a reactive lymphopenia in order to protect the heart from an overshoot of pro-inflamatory products of neutrophils and activated monocytes [18, 20].
Conclusions
This study demonstrates the value of white blood cell subtypes for predicting infarct size and outcome in a large group of STEMI patients of which the vast majority was treated with percutaneous coronary intervention before undergoing the CMR study.
Further, it shows that after STEMI, distinctive patterns in the temporal evolution of white blood cell subtypes can be observed according to infarct size. Patients with larger infarctions display a marked neutrophil peak at 12 h after revascularization and a larger increase in monocyte count over time. Neutrophil count at 12 h after revascularization was the only white blood cell subtype independently related to large infarctions
An elevated neutrophil count at 96 h was an independent predictor of adverse outcome during follow-up, even adjusted for strong prognosticators and infarct size.
The ultimate role of the temporal evolution of white blood cell subtypes in the pathophysiology of myocardial infarction, the impact on infarct size as well as potential therapeutic implications deserve further investigation.
Abbreviations
- CMR:
-
Cardiovascular magnetic resonance imaging
- STEMI:
-
ST elevation myocardial infarction
- MACE:
-
Major adverse cardiac events
- TIMI:
-
Thrombolysis in myocardial infarction
References
Nunez, J., E. Nunez, J. Sanchis, V. Bodi, and A. Llacer. 2006. Prognostic value of leukocytosis in acute coronary syndromes: The cinderella of the inflammatory markers. Current Medicinal Chemistry 13(18): 2113–2118.
Barron, H.V., C.P. Cannon, S.A. Murphy, E. Braunwald, and C.M. Gibson. 2000. Association between white blood cell count, epicardial blood flow, myocardial perfusion, and clinical outcomes in the setting of acute myocardial infarction: A thrombolysis in myocardial infarction 10 substudy. Circulation 102(19): 2329–2334.
Kirtane, A.J., A. Bui, S.A. Murphy, H.V. Barron, and C.M. Gibson. 2004. Association of peripheral neutrophilia with adverse angiographic outcomes in ST-elevation myocardial infarction. American Journal of Cardiology 93(5): 532–536.
Mariani, M., R. Fetiveau, E. Rossetti, A. Poli, F. Poletti, P. Vandoni, et al. 2006. Significance of total and differential leucocyte count in patients with acute myocardial infarction treated with primary coronary angioplasty. European Heart Journal 27(21): 2511–2515.
Maekawa, Y., T. Anzai, T. Yoshikawa, Y. Asakura, T. Takahashi, S. Ishikawa, et al. 2002. Prognostic significance of peripheral monocytosis after reperfused acute myocardial infarction:a possible role for left ventricular remodeling. Journal of the American College of Cardiology 39(2): 241–246.
Frangogiannis, N.G., C.W. Smith, and M.L. Entman. 2002. The inflammatory response in myocardial infarction. Cardiovascular Research 53(1): 31–47.
Henriques, J.P., F. Zijlstra, A.W. van’t Hof, M.J. de Boer, J.H. Dambrink, M. Gosselink, et al. 2003. Angiographic assessment of reperfusion in acute myocardial infarction by myocardial blush grade. Circulation 107(16): 2115–2119.
Bodi, V., J. Sanchis, M.P. Lopez-Lereu, A. Losada, J. Nunez, M. Pellicer, et al. 2005. Usefulness of a comprehensive cardiovascular magnetic resonance imaging assessment for predicting recovery of left ventricular wall motion in the setting of myocardial stunning. Journal of the American College of Cardiology 46(9): 1747–1752.
Bodi, V., J. Sanchis, M.P. Lopez-Lereu, J. Nunez, L. Mainar, M. Pellicer, et al. 2007. Evolution of 5 cardiovascular magnetic resonance-derived viability indexes after reperfused myocardial infarction. American Heart Journal 153(4): 649–655.
Cerqueira, M.D., N.J. Weissman, V. Dilsizian, A.K. Jacobs, S. Kaul, W.K. Laskey, et al. 2002. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4): 539–542.
Thygesen, K., J.S. Alpert, and H.D. White. 2007. Universal definition of myocardial infarction. Journal of the American College of Cardiology 50(22): 2173–2195.
Dickstein, K., A. Cohen-Solal, G. Filippatos, J.J. McMurray, P. Ponikowski, P.A. Poole-Wilson, et al. 2008. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). European Heart Journal 29(19): 2388–2442.
Pennell, D.J., U.P. Sechtem, C.B. Higgins, W.J. Manning, G.M. Pohost, F.E. Rademakers, et al. 2004. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report. European Heart Journal 25(21): 1940–1965.
Faxon, D.P., R.J. Gibbons, N.A. Chronos, P.A. Gurbel, and F. Sheehan. 2002. The effect of blockade of the CD11/CD18 integrin receptor on infarct size in patients with acute myocardial infarction treated with direct angioplasty: The results of the HALT-MI study. Journal of the American College of Cardiology 40(7): 1199–1204.
Gibson, W.J., and C.M. Gibson. 2006. The association of impaired myocardial perfusion and monocytosis with late recovery of left ventricular function following primary percutaneous coronary intervention. European Heart Journal 27(21): 2487–2488.
Hotchkiss, R.S., C.M. Coopersmith, and I.E. Karl. 2005. Prevention of lymphocyte apoptosis—a potential treatment of sepsis? Clinical Infectious Diseases 41(Suppl 7): S465–S469.
Munford, R.S., and J. Pugin. 2001. Normal responses to injury prevent systemic inflammation and can be immunosuppressive. American Journal of Respiratory and Critical Care Medicine 163(2): 316–321.
Steppich, B.A., P. Moog, C. Matissek, N. Wisniowski, J. Kuhle, N. Joghetaei, et al. 2007. Cytokine profiles and T cell function in acute coronary syndromes. Atherosclerosis 190(2): 443–451.
Bodi, V., J. Sanchis, J. Nunez, E. Rumiza, L. Mainar, M.P. Lopez-Lereu, et al. 2009. Post-reperfusion lymphopenia and microvascular obstruction in ST-segment elevation acute myocardial infarction. Revista Espanola de Cardiologia 62(10): 1109–1117.
Bodi, V., J. Sanchis, J. Nunez, L. Mainar, G. Minana, I. Benet, et al. 2008. Uncontrolled immune response in acute myocardial infarction: Unraveling the thread. American Heart Journal 156(6): 1065–1073.
Acknowledgments
This study was supported by the “Instituto de Salud Carlos III” with FIS PI080128 and Heracles grants and by the Spanish Society of Cardiology with a FEC grant.
Conflict of interest statement
No conflict of interest exists in the present study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Online Table 1
Cardiac catheterization data of the whole study group and of patients with and without large infarction (DOC 31 kb)
Online Table 2
Cardiac catheterization data of patients with and without major adverse cardiac events (DOC 31 kb)
Rights and permissions
About this article
Cite this article
Husser, O., Bodi, V., Sanchis, J. et al. White Blood Cell Subtypes after STEMI: Temporal Evolution, Association with Cardiovascular Magnetic Resonance—Derived Infarct Size and Impact on Outcome. Inflammation 34, 73–84 (2011). https://doi.org/10.1007/s10753-010-9209-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-010-9209-0