Abstract
Objective
Coronary artery disease (CAD) is presently the major cause of mortality and morbidity. Anti-hyperlipidemic treatment is one of the main treatment steps in the management of CAD. Statins are the cornerstones in this treatment. Ezetimibe can be reliably used, when statins prove ineffective in treatment, or to reduce their side effects. In the present study we examined the effects of high-dose pravastatin (40 mg) and low-dose pravastatin (10 mg) + ezetimibe (10 mg) combination therapy on lipid and glucose mechanism, as well as inflammation.
Methods
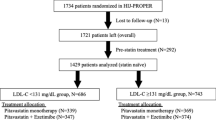
This study registered 100 cases. Of the cases, 50 [57.1 ± 11.1 years (24 (48%) females and 26 (52%) males)] were administered 40 mg/day pravastatin (group 1) and 50 [53.2 ± 12.2 years (27 (54%) females and 23 (46%) males)] were administered 10 mg pravastatin + 10 mg ezetimibe (group 2).
Results
In group 1, total cholesterol fell from 231.1 ± 83.5 mg/dl to 211.3 ± 37.2 mg/dl (p = 0.03), triglyceride from 243.5 ± 96.8 mg/dl to 190.9 ± 55.2 mg/dl (p = 0.003), and LDL cholesterol from 165.7 ± 29.7 mg/dl to 133.4 ± 26.6 mg/dl (p = 0.02). In group 2, total cholesterol dropped from 250.9 ± 51.8 mg/dl to 187.9 ± 34.9 mg/dl (p = 0.001), triglyceride from 270.3 ± 158.9 mg/dl to 154.6 ± 60.7 mg/dl (p = 0.001), and LDL cholesterol from 158.1 ± 47.5 mg/dl to 116.9 ± 26.4 mg/dl (p = 0.001). Insulin resistance decreased from 4.05 ± 2.31 to 3.16 ± 1.90 (p = 0.07) in group 1 and from 2.96 ± 1.50 to 2.05 ± 0.55 (p = 0.009) in group 2. High sensitive C-reactive protein fell from 6.69 ± 6.11 mg/l to 3.02 ± 1.70 mg/l (p = 0.01) in group 1 and from 6.36 ± 2.06 mg/l to 2.68 ± 1.69 mg/l (p = 0.001) in group 2.
Conclusion
Both therapy regimes are effective. However, we found that low-dose pravastatin and ezetimibe combination therapy is more effective than high-dose pravastatin therapy on lipid metabolism, glucose metabolism and inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Coronary heart diseases (CAD) are among important causes of mortality and morbidity, despite the recent developments [1]. Hypercholesterolemia, inflammation and insulin resistance have a significant part in the development and progression of CAD. The foregoing aim of primary and secondary prevention is restoration of elevated LDL–cholesterol (LDL–C) [2]. It is known that the highest benefit is reaped from aggressive LDL–C treatment in coronary artery disease. However, high-dose statin monotherapy either proves ineffective or does not bring about the targeted lipid level due to side effects [3].
Lipid-lowering therapy is a cornerstone in preventing coronary artery disease, particularly in high-risk patients and coroner artery disease .The 3-hydroxy-3-methylglutaryl coenzyme A (HMG–CoA) reductase inhibitors (statins) are the most potent and commonly prescribed drugs for the treatment of hypercholesterolemia. It is known that statins have favorable effects on lipid and glucose metabolism, as well as inflammation. High-dose statin therapy may be ineffective in coronary artery patients and high-risk patients due to its side effects and its efficacy, which is not in a direct relation with dose [3, 4]. This situation brings forth the combined lipid lowering therapy.
Ezetimibe is a new cholesterol-lowering drug that inhibits absorption of dietary and biliary cholesterol across the intestinal wall without affecting absorption of bile acids, fatty acids, fat-soluble vitamins, or triglycerides [5, 6]. Ezetimibe has a complementary mechanism of action to the pravastatin, which inhibit cholesterol synthesis in the liver. There is not enough information about the effects of ezetimibe and pravastatin combined therapy on lipid metabolism, glucose metabolism and inflammation.
In this study we aimed to compare and contrast the effects of high-dose pravastatin (40 mg) and low-dose pravastatin (10 mg) + ezetimibe (10 mg) on lipid metabolism, high-sensitive C-reactive protein (hs–CRP) and insulin resistance.
METHODS
Patient Population
The study registered 100 cases (mean age 53.7 ± 12.0, 49% males and 51% females), of who were diagnosed as primary hyperlipidemia between October 2005 and may 2006 in the cardiology polyclinic of Firat University Medical School and met the inclusion criteria. The study was conducted in accordance with the Helsinki Declaration. The local ethics committee approved the study protocol. All patients were informed about the study before the study started and their consents were taken.
Inclusion Criteria
Eligible patients were men and women 18 through 75 years of age with primary hyperlipidemia and known coronary heart disease (CHD) or 10 years CHD risk > 20%. Entry criteria required triglyceride ≤ 350 mg/dl and LDL–C levels between 370 and 210 mg/dl after a washout period lasting up to 10 weeks or diagnosed new primary hyperlipidemia.
Exclusion Criteria
Prohibited concomitant illnesses and procedures included congestive heart failure; uncontrolled cardiac arrhythmias; history of unstable or severe peripheral artery disease within three months of study entry; unstable angina pectoris; myocardial infarction, coronary bypass surgery, or angioplasty within six months of study entry; obesity; chronic inflamatuvar diseases; collagen tissue diseases; pregnant; hypertension; diabetes mellitus; active or chronic hepatic or hepatobiliary disease; known impairment of renal function; known pancreatic diseases; known coagulopathy; and endocrine or metabolic disease.
Patients taking drugs that could affect glucose, lipid metabolism and inflammation, such as steroids, non-steroid anti-inflammatory drugs, thiazid diuretics, or beta-blockers, were required to have stable doses for 2 weeks before screening. Medications for other disease were maintained and not changed during pravastatin therapy.
Study Designs
Anamneses of the patients included in the study were collected, and their routine physical examination was conducted. Their heights and weights were measured, and body mass indices were calculated. Firat University Biochemistry Laboratories (Elazig, Turkey) performed all clinical laboratory analyses. This was followed by total cholesterol, triglyceride, LDL–C, HDL–cholesterol (HDL–C), glucose, insulin, hs–CRP, blood electrolytes, urea, creatinine, AST, ALT, CK, CK–MB and whole blood analyses. ECG and blood pressure were monitored.
Patients were randomly assigned to receive pravastatin 40 mg/day (group 1) or pravastatin 10 mg/day + ezetimibe 10 mg/day (group 2) for 6 months orally daily. Patients and all study personnel were blinded to treatment assignment and laboratory measurements. Following cessation of all lipid lowering drugs, and during a 4 to 12-week washout period, patients were instructed to follow the National Cholesterol Education Program step I (or stricter) diet (30% of total calories from fat, <10% of calories saturated fatty acids, <300 mg cholesterol per day) [7].
The patients were asked to come for visits in the first, third and sixth months after the commencement of therapy. Whole blood count, routine biochemistry, lipid parameters, glucose, insulin and hs–CRP of the patients were determined and recorded. Insulin resistance was calculated using HOMA formula.
The cases were monitored against the side effects of pravastatin or ezetimibe like headache, asthenia, insomnia, disturbance of gastrointestinal, diarrhea, constipation, nausea, myalgia, increased AST and ALT or increased CK and CK–MB.
Lipid Measurement
Serum levels of total cholesterol, HDL–C, LDL–C and triglyceride were assayed by using Olympus AU 600 Otoanalyser (Olympus Optical, Japan) according to their kit procedure.
Measurement of Inflammatory Markers
For this study, blood was collected into a serum tube at baseline and at 16 weeks. The tubes were centrifuged on site, and the serum was separated and shipped to a core laboratory for storage at −20°C. The paired baseline and 16-week samples were shipped to the laboratory and measured in batches. CRP and SAA were measured by high-sensitivity immunonephelometry assay (Dade Behring Marburg GmbH, Marburg).
Insulin Resistance
Serum insulin levels were evaluated in Immblite-2000 Hormone Analyser (Los Angeles, USA) using immblite-2000 kit, in accordance with chemiluminescence method. Insulin resistance was calculated using HOMA formula [HOMA 12 = fasting insulin (μu/mlt) × fasting blood sugar (mmol/lt)/22.5] [8].
STATISTICAL ANALYSIS
The statistical evaluation of data was conducted in computer media using SPSS 11.00 package software. General descriptive characteristics were assessed as mean±standard deviation (SD). Sex and risk factors were compared between groups using chi-square test. Normal distribution of data between groups was evaluated with student t test. Non-normal distribution of data between groups was assessed with Mann Whitney U test. Paired t test was employed in the evaluation of data of normal distribution before and after treatment within a group, and Wilcoxon test was used for data with non-normal distribution before and after treatment within a group. The lowest level of significance and correlation was accepted as p < 0.05.
RESULTS
The study registered 100 cases (mean age 53.7 ± 12.0; 51% females, and 49% males). The cases were divided into two groups. Group 1 (n = 50) were employed pravastatin 40 mg treatment, with mean age 57.1 ± 11.1 years [24 (48%) females, and 26 (52%) were males], and group 2 (n = 50) were employed pravastatin 10 mg + ezetimibe 10 mg treatment, with mean age 53.2 ± 12.2 years [27 (54% females, and 23 (46%) males]. There were no difference between group 1 and group 2 about base demographical data (p > 0.05). Demographical data about the study groups are presented in Table 1.
The changes in lipid metabolism, glucose metabolism and inflammation (CRP) in groups 1 and 2 after treatment are given in Table 2.
Evaluation of Side Effects
There was not any statistically significant difference between the two groups in terms of side effects. Side effects were observed at a rate of 12% (n = 6) in group 1, and 6% (n = 3) in group 2 (p > 0.05). The drug was not interrupted due to side effects in our patients.
DISCUSSION
Treatment with statins blocks cholesterol biosynthesis, and these drugs are currently the cornerstone of atherosclerotic disease management [9, 10]. Statins are the most potent and commonly prescribed drugs for the treatment of hypercholesterolemia. However, despite widespread use of statins in clinical practice, a large proportion of at-risk patients do not achieve LDL–C goals as recommended by the European Second Joint Task Force [11] and the US National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) guidelines [2]. Nonetheless, target lipid levels are achieved by at least 50% of patients treated with lipid-lowering therapy [12]. The failure to reach target lipid levels may be due, at least in part, to prescribers treating patients with the minimum starting doses of statins [13]. However, treatment with higher statin dosages may be associated with an increased risk of adverse effects, especially if they are coadministered with other lipid-lowering drugs. Because treatment with a statin alone may not be sufficient or appropriate, more treatment options are required to optimize the management of hypercholesterolemia [3, 14]. The combined use of statins with ezetimibe may be an attractive treatment option for patients who require reductions in LDL–C that cannot be achieved with statin monotherapy.
Ezetimibe is the first in a new class of cholesterol absorption inhibitors, the 2-azetidinones. The drug effectively blocks the intestinal absorption of dietary and biliary cholesterol without interfering with the absorption of fat-soluble vitamins [15]. By comparison, statins block the endogenous synthesis of cholesterol in the liver via inhibition of HMG–CoA reductase [16]. Because ezetimibe and statins have distinct and potentially complementary mechanisms of action, it was hypothesized that the combined use of these agents may produce incremental antihypercholesterolemic effects.
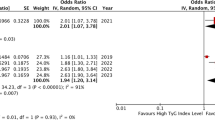
We found that both drugs were effective on the lipid metabolism (Table 2). However, we established that ezetimibe and low-dose pravastatin combination therapy was more effective on the lipid metabolism, relative to high-dose pravastatin therapy. Positive improvements in the lipid metabolism were limited with LDL–C, total cholesterol and triglyceride. High-dose pravastatin monotherapy may prove inadequate in improving the lipid metabolism in patients with atherosclerotic heart disease or high-risk patients [4]. Besides, high dose drug use may be limited by dose-dependent side effects like hepatotoxicity, myotoxicity, and nephrotoxicity [3]. Combination therapy may be needed to obtain the targeted cholesterol levels in atherosclerotic heart disease patients and high-risk patients.
Davis et. al. demonstrated that ezetimibe monotherapy reduced atherosclerosis in hypercholesterolemic mice [17]. Pravastatin is also known to have favorable effects on mortality and morbidity in atherosclerotic heart disease patients [18]. Just like its synergic effect on lipid metabolism, combined use of ezetimibe and pravastatin may have a synergic preventive and therapeutic effect against atherosclerosis. The positive effects that the pravastatin ezetimibe combination therapy had on the lipid metabolism in our study lend support to this hypothesis.
The most common dyslipidemia in the insulin-resistant patient is high TG and low HDL–C [19, 20]. In general, the association has been weak, and more convincingly shown for lipid abnormalities than for coronary artery disease itself [21, 22]. However, a recent prospective study has documented a significantly higher risk for ischemic heart disease in hyperinsulinemic Canadian men independently of serum triglycerides, cholesterol fractions, and apolipoprotein B [23]. Case-control investigations have consistently shown that patients with coronary heart disease are insulin resistant at the whole body level when compared to subjects free of ischemic heart disease on equal grounds of confounding factors (i.e., sex, age, body weight, glucose tolerance, blood pressure, and serum lipid levels) [22, 24, 25]. Furthermore, results of a number of prospective studies indicate that those with coronary artery disease and impaired glucose metabolism have a significantly greater cardiovascular morbidity and mortality compared with those with normal glucose metabolism. Patients with IRS may have a prothrombotic state characterized by increased plasma levels of plasminogen activator inhibitor-1 and fibrinogen levels [26, 27]. A prothombotic state may enhance other mechanisms that play a role in promoting atherogensis [26]. Statins (HMG–CoA reductase inhibitors) are the first drug of choice for individuals at high risk of IRS and with TG levels of less than 500 mg/dl [2]. Low-dose pravastatin and ezetimibe combination therapy improved insulin resistance markedly better than high-dose pravastatin monotherapy (Table 2). This suggests that combined antilipidemic therapy may be a more favorable treatment alternative in high-risk dyslipidemic patients and atherosclerotic heart disease patients. However, larger randomized studies are needed.
High sensitive C-reactive protein, an inflammatory biomarker, has been shown to predict morbidity and mortality from coronary heart disease (CHD) in individuals with or without previously diagnosed CHD, independent of traditional risk factors, including tobacco use and lipid status [28–31]. Statin therapy lowers the risk of cardiovascular events by reducing plasma cholesterol levels, and practice guidelines for patients with known cardiovascular disease emphasize the importance of reaching target goals for LDL cholesterol [2]. However, we have shown that statin therapy results in a greater clinical benefit when levels of the inflammatory biomarker CRP are elevated [32, 33] and that statins lower CRP levels in a manner largely independent of LDL cholesterol levels [33, 34].
Sager et. al. showed that simvastatin + ezetimibe combination therapy reduced hs–CRP levels more effectively than simvastatin monotherapy [35]. Both therapies effectively pulled down hs–CRP, which has an important place in mortality and morbidity in atherosclerotic heart disease. However, the reduction brought about in hs–CRP level by the combination therapy was more marked than the reduction caused by monotherapy. Our study demonstrates that low-dose pravastatin and ezetimibe combination therapy had markedly more positive effects on inflammation (Table 2).
Combined use of ezetimibe and pravastatin lowered cholesterol more effectively by inhibiting the cholesterol originating from the liver, diet and bile in combination. Because ezetimibe and statins have distinct and potentially complementary mechanisms of action, it was hypothesized that the combined use of these agents may produce incremental antihypercholesterolemic effects. Coadministration of ezetimibe and statins provides inhibition of two sources of cholesterol, leading to greater reductions in LDL–C, CRP and insulin resistance than with either agent alone as can be seen in Table 2.
Study Limitation
The major limitation of our study is the low number of our cases. In addition, our patients were followed-up for 6 months, and no long-term follow-up was made. Besides, attempts to change cholesterol levels by diet and/or physical activity were not evaluated.
CONCLUSION
Management of the impaired lipid metabolism, glucose metabolism, and inflammation, which are responsible for mortality and morbidity in coronary artery patients or high-risk patients, is very important. Our study demonstrated that low-dose pravastatin and ezetimibe combination therapy had more favorable effects on the lipid metabolism, glucose metabolism and inflammation, in comparison to high-dose pravastatin monotherapy. However, it would be more appropriate to use ezetimibe and high-dose pravastatin in the combined anti-hyperlipidemic treatment of CAD or high-risk patients.
References
Murray, C. J., and A. D. Lopez. 1997. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 349:1269–1276.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. 2001. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 285:2486–2497.
Kastelein, J., and M. J. van Dam. 2001. A new role for combination therapy in lipid management. Br. J. Cardiol. 8:639–653.
Pearson, T. A., I. Laurora, H. Chu, and S. Kafonek. 2000. The lipid treatment assessment project (L–TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch. Intern. Med. 28(160):459–467.
van Heek, M, C. F. France, D. S. Compton, R. L. Mcleod, N. P. Yumibe, K. B. Alton, E. J. Sybertz, and H. R. Davis, Jr. 1997. In vivo metabolism-based discovery of a potent cholesterol absorption inhibitor, SCH58235, in the rat and rhesus monkey through the identification of the active metabolites of SCH48461. J. Pharmacol. Exp. Ther. 283:157–163.
van Heek, M., C. Farley, D. S. Compton, L. Hoos, and H. R. Davis. 2000. Comparison of the activity and disposition of the novel cholesterol absorption inhibitor, SCH58235, and its glucuronide, SCH60663. Br. J. Pharmacol. 129:1748–1754.
Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). 1993. JAMA 269:3015–3023.
Haffner, S. M., H. Miettinen, and M. P. Stern. 1997. The homeostasis model in the San Antonio Heart Study. Diabetes Care 20:1087–1092.
Anonymous. 2001. Statin therapy—what now? Drug Ther. Bull. 39:17–21.
Libby, P. 2002. Atherosclerosis: the new view. Sci. Am. 286(5):46–55.
Pyorala, K., and D. Wood. 1998. Prevention of coronary heart disease in clinical practice. European recommendations revised and reinforced. Eur. Heart. J. 19:1434–1503.
Primatesta, P., and N. R. Poulter. 2000. Lipid concentrations and the use of lipid lowering drugs: evidence from a national cross sectional survey. BMJ. 321:1322–1325.
Leitersdorf, E. 2002. Selective cholesterol absorption inhibition: a novel strategy in lipid-lowering management. Int. J. Clin. Pract. 56(2):116–119.
Brown, W. V. 2001. Novel approaches to lipid lowering: what is on the horizon? Am. J. Cardiol. 87(5A):23B–27B.
van Heek, M, C. Farley, D. S. Compton, L. Hoos, and H. R. Davis. 2001. Ezetimibe selectively inhibits intestinal cholesterol absorption in rodents in the presence and absence of exocrine pancreatic function. Br. J. Pharmacol. 134(2):409–417.
Miettinen, T. A. 2001. Cholesterol absorption inhibition: a strategy for cholesterol-lowering therapy. Drug Focus 55:710–716.
Davis, H. R. Jr, D. S. Compton, L. Hoos, and G. Tetzloff. 2001. Ezetimibe, a potent cholesterol absorption inhibitor, inhibits the development of atherosclerosis in Apo E knockout mice. Arterioscler. Thromb. Vasc. Biol. 21:2032–2038.
Shepherd, J., S. M. Cobbe, I. Ford, C. G. Isles, A. R. Lorimer, P. W. MacFarlane, J. H. McKillop, and Packard C. J. 1995. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N. Engl. J. Med. 333:1301–1307.
Reaven, G. 1988. The Banting Lecture: the role of insulin resistance in human disease. Diabetes 37:1596–1607.
Ginsberg, H. N. 2003. Treatment for patients with the metabolic syndrome. Am. J. Cardiol. 91:29E–39E.
Fontbonne, A. 1994. Why can high insulin levels indicate a risk for coronary heart disease? Diabetologia 37:953–955.
Reaven, G. M., and A. Laws. 1994. Insulin resistance, compensatory hyperinsulinemia, and coronary heart disease. Diabetologia 37:948–952.
Despres, J. P., B. Lamarche, P. Mauriège, B. Cantin, G. R. Dagenais, S. Moorjani, and P. J. Lupien. 1996. Hyperinsulinemia as an independent risk factor for ischemic heart disease. N. Engl. J. Med. 334:952–957.
Paolisso, G., A. Gambardella, D. Galzerano, A. D’Amore, V. Balbi, M. Varricchio, and F. D’Onofrio. 1993. Metabolic features of patients with and without coronary heart disease but with superimposable cluster of cardiovascular risk factors. Coron. Artery Dis. 4:1085–1091.
Bressler, P., S. R. Bailey, M. Matsuda, and R. A. DeFronzo. 1996. Insulin resistance and coronary artery disease. Diabetologia. 39:1345–50 (Erratum in: Diabetologia 1997;40:366).
Grundy, S. M., B. Howard, S. Smith, Jr, R. Eckel, R. Redberg, and R. O. Bonow. 2002. Prevention Conference, VI: Diabetes and cardiovascular disease: executive summary: conference proceeding for healthcare professionals from a special writing group of the American Heart Association. Circulation 105:2231–2239.
Reaven, G. 1994. Syndrome X: 6 years later. J. Intern. Med. Suppl. 736:13–22.
Ridker, P. M., C. H. Hennekens, J. E. Buring, and N. Rifai. 2000. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N. Engl. J. Med. 342:836–843.
Rifai, L., Rose, J. E. Buring, and N. R. Cook. 2002. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N. Engl. J. Med. 347:1557–1565.
Haverkate, F., S. G. Thompson, S. D. Pyke, J. R. Gallimore, and M. B. Pepys. 1997. Production of C-reactive protein and risk of coronary events in stable and unstable angina European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Lancet 349(9050):426–462.
Pietila, K. O., A. P. Harmoinen, J. Jokiniitty, and A. I. Pasternack. 1996. Serum creactive protein concentration in acute myocardial infarction and its relationship to mortality during 24 months of follow-up in patients under thrombolytic treatment. Eur. Heart. J. 17(9):1345–1349.
Ridker, P. M., N. Rifai, M. A. Pfeffer, F. M. Sacks, L. A. Moye, and S. Goldman. 1998. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Circulation 98:839–844.
Ridker, P. M., N. Rifai, M. Clearfield, J. R. Downs, S. E. Weis, J. S. Miles, and A. M. Gotto, Jr. Air Force/Texas Coronary Atherosclerosis Prevention Study Investigators. 2001. Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N. Engl. J. Med. 344:1959–1965.
Albert, M. A., E. Danielson, N. Rifai, and P. M. Ridker. 2001. Effect of statin therapy on C-reactive protein levels: the pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 286:64–70.
Sager, P. T., L. Melani, L. Lipka, J. Strony, B. Yang, R. Suresh, and E. Veltri. 2003. Ezetimibe Study Group. Effect of coadministration of ezetimibe and simvastatin on high-sensitivity C-reactive protein. Am. J. Cardiol. 92:1414–1418.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dagli, N., Yavuzkir, M. & Karaca, I. The Effects of High Dose Pravastatin and Low Dose Pravastatin and Ezetimibe Combination Therapy on Lipid, Glucose Metabolism and Inflammation. Inflammation 30, 230–235 (2007). https://doi.org/10.1007/s10753-007-9041-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-007-9041-3