Abstract
Long waits for health care are hypothesized to cause negative health outcomes due to delays in diagnosis and treatment. This study uses administrative data to examine the relationship between time spent waiting for outpatient care and the risk of hospitalization for an ambulatory care sensitive condition (ACSC). Data on the number of days until the next available appointment were extracted from Veterans Affairs (VA) medical centers. Two methodological issues arose. First, the simultaneous determination of individual health status and wait times due to medical triage was overcome by developing an exogenous wait time measure. Second, selection bias due to unobserved case mix differences was minimized by separating in time the sample selection period from the period when wait times and outcomes were measured. Exogenous facility-level wait time was the main variable of interest in a fixed effects stacked heteroskedastic probit regression model that predicted the probability of ACSC hospitalization in each month of a six-month period. There was a significant and positive relationship between facility-level wait times and the probability of experiencing an ACSC hospitalization, especially for facility-level wait times of 29 days or more. Further research is needed to replicate these findings in other populations and among those with different clinical histories. As well, policymakers and researchers need an improved understanding of the causes of long wait times and interventions to decrease wait times.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Background
The Institute of Medicine’s Committee on the Quality of Health Care in America (2004) highlighted reducing delays as one of six aims for improving the quality of America’s health care system. The main reason to reduce delays is because long waits for healthcare are assumed to negatively affect health outcomes due to delays in diagnosis and treatment (Institute of Medicine (IOM) 2004; Kenagy et al. 1999). Despite the declared importance of ensuring timely access to care, little research has examined the empirical association between waiting for outpatient care and health outcomes.
The lack of research on the consequences of waiting for outpatient care may be due to the scarcity of administrative data on wait times in American health care systems. The Veterans Affairs (VA) health care system is an important exception because each month it automatically extracts data from its outpatient scheduling system on how long veterans are waiting for appointments. This data collection effort was implemented as a response to a VA policy goal that by 1998, 90% of veterans seeking care would be seen in both primary and specialty care within 30 days of the appointment request (US GAO 2001).
Using these data on waiting times until the next available appointment, we recently examined the association between waiting for outpatient care in the VA and mortality among veterans who had visited a geriatric outpatient clinic in federal fiscal year (FFY) 2001 (October 2000–September 2001). Veterans who visited medical centers with facility-level wait times of 31 days or more were 21% more likely to die in a six month follow-up period compared to veterans who visited facilities with wait times of less than 31 days (Prentice et al. 2007). This article extends that work by examining the association between waiting for outpatient care and experiencing a hospitalization due to an ambulatory care sensitive condition (ACSC), also known as a potentially preventable hospitalization.Footnote 1
ACSC hospitalizations are an ideal outcome to examine the consequences of waiting for outpatient care because these hospitalizations can be avoided if patients receive timely and effective outpatient care. Appropriate outpatient care prevents the onset of certain conditions, controls some chronic diseases to prevent progression, or controls an acute episode of the disease (Culler et al. 1998). For example, suppose a diabetic patient has an ulcer on his toe that is not healing and he cannot get a podiatry appointment quickly. He may be at increased risk of gangrene and being hospitalized for a lower-extremity amputation (AHRQ 2001). Common ACSCs among adults include asthma, diabetes, hypertension, congestive heart failure, and chronic obstructive pulmonary disease (AHRQ 2001;Culler et al 1998).
This article is the first to test the assumption that long waits for outpatient care increase the risk of experiencing an ACSC hospitalization. It also examines the two main methodological challenges that arise when examining the relationship between waiting for outpatient care and ACSC hospitalization: (1) the simultaneous determination of individual health status and wait times due to medical triage and (2) potential selection that may occur at facilities with relatively long wait times. This selection could bias estimates in either direction. For example, facilities with relatively long wait times may attract fewer severely ill patients because very sick patients cannot wait and must go elsewhere for their care. This would reduce the observed relationship between wait times and outcomes. In contrast, wealthier individuals may choose to use non-VA care when faced with long waits and if wealth is correlated with health, then facilities with relatively long wait times may attract sicker patients, amplifying the observed relationship between wait times and outcomes.
2 Methods
2.1 Study population
The study population included VA patients age 65 or older who visited at least one of three types of geriatric outpatient clinics during the 2001 federal fiscal year (FFY; October, 2000 to September, 2001). The three types of geriatric outpatient clinics are (1) geriatric primary care, (2) geriatric clinic and (3) geriatric evaluation and management. Appointments at geriatric outpatient clinics are focused on preventing, evaluating and managing illnesses and conditions that are specifically associated with aging and feature providers who are trained in the management of these conditions (VHA 2004). This sample was ideal for examining whether long wait times were associated with negative health outcomes. Since these patients are older and more frail than the general population they ought to be particularly sensitive to variation in the timeliness of access to medical care.
2.2 Waiting time data
We hypothesized that individuals who wait longer for medical care are at increased risk of experiencing an ACSC hospitalization. Thus, the main explanatory variable of interest was the wait until the next available appointment at a VA facility.Footnote 2 The VA keeps monthly data on the average number of days between the request for an appointment and when the appointment is actually scheduled. Services in the VA can be provided at a parent station, such as a medical center, or a sub-station, such as a community-based outpatient clinic. Wait times are kept for each type of clinic appointment (e.g. urology, primary care, and laboratory) within a parent station and for all clinic appointments at sub-stations under a parent station. To create a performance measure for tracking wait times, the VA aggregates wait times by appointment type at the parent station level on a monthly basis using a weighted average (Baar 2005b).Footnote 3
Although there are data available on all types of appointments, past performance measures in the VA have focused on the wait times for 49 types of appointments. These 49 clinic appointment types were chosen because they are (1) appointment types with high volumes, (2) appointment types that cover 93% of office-based patient–provider interactions in the VA (versus other services, such as labs or telephone consultations) and (3) appointment types that represent all major sub-specialties of medicine (e.g. mental health, orthopedics) (Baar 2005a). As in our previous work (Prentice et al. 2007), our wait time measure is based on these 49 appointment types in addition to appointments in a geriatric clinic or for geriatric evaluation and management because the study population was based on visiting a geriatric outpatient clinic (49 + 2 = 51 appointment types). Note that geriatric primary care was already included as one of the 49 appointment types.
2.3 Individualized wait times
Data are available on the date, the facility and the appointment type used by each patient in the study population. Thus, it was tempting to calculate a wait time measure based on services each individual actually used in 2001 and to associate this measure with health outcomes. However, this approach is problematic due to medical triage.
In many medical practices, providers identify those who are in the poorest health when calling to request an appointment and schedule these patients with appointments first (Murray et al. 2003). In the VA context, medical providers may triage the sickest patients in two different ways. First medical providers may identify those who are in the poorest health and schedule these patients first within a specific type of appointment (e.g. general internal medicine). Second, medical providers may refer patients in the poorest health to other types of appointments with shorter waits (e.g. patients referred from general internal medicine to primary care). Therefore, triage can happen both within an appointment type and between different appointment types in the VA. Unobserved individual health status differences are likely to affect the services an individual uses which in turn affects individual wait times as well as outcomes.
The top panel of Table 1 illustrates this problem. It shows the mean, median and interquartile range of wait times that were calculated for July, August and September based on the appointment types an individual actually used in each of those months by whether or not the individual experienced an ACSC hospitalization in that month. Note this is still not the actual time individual patients waited for appointments. The VA averages together the individual wait times and reports an average wait for the entire parent station for each appointment type. We averaged together this parent station level wait time for all clinic appointments used by each individual.
Individuals with an ACSC hospitalization had consistently shorter individualized wait times. The mean and median wait times among individuals who did not have an ACSC hospitalization were between 1 and 4 days longer than the mean and median wait times among individuals who had an ACSC hospitalization. Thus, if our wait time measure were based on services individuals actually used, it would appear that waiting for health care reduced the probability of experiencing an ACSC hospitalization.
The simultaneous determination of unobserved individual health status, wait times and health outcomes confounds any attempt to study the effect of individualized wait times on outcomes. Although statistical controls for observable differences in health status will reduce the severity of this problem, we are not able to measure health status precisely enough to eliminate it. Consequently, to properly isolate the effect of waiting on outcomes we calculated a wait time that is exogenous to the individual (not affected by prior individual health status).
2.4 Exogenous wait time measure
Our exogenous wait time measure is a refined version of a measure that we have used in our previous work (Prentice et al. 2007). An example of this exogenous wait time calculation is given in Appendix A. To calculate wait times that were exogenous to the individual we set out to construct a wait time that would apply to the same “representative” patient at each parent station, eliminating the simultaneous effect of unmeasured prior individual health status on both wait time and outcome. We computed the proportion of each type of clinic appointment used by the entire sample between October 2000 and March 2001 (the sample selection period discussed below).Footnote 4 This proportion was multiplied by the wait in days for each type of appointment at a parent station, and these products were summed for all appointment types in the parent station. Multiplying the wait time for an appointment type by its proportion in the whole sample gives greater weight to the wait times of appointment types that were used more frequently by the entire sample.
There were two adjustments made to the general calculation just described. First, if no appointments were requested as next available within a month for a certain type of clinic appointment, the wait time is missing. As in our previous work, we imputed wait times that were missing with zero under the assumption that if no next available appointments were requested, individuals could use these services right away.Footnote 5 We confirmed this assumption by (1) finding recorded utilization at these clinic appointments in FY 2001 or (2) finding that a type of clinic appointment was missing in one month but had a wait time in other months implying this type of service did not have next available appointments scheduled each month. We also confirmed that waiting times for one type of appointment (e.g. primary care) are determined independently from other types of appointments (e.g. general internal medicine). However, due to a large number of missing wait times, we excluded appointment types for opioid substitution, speech pathology, radiation therapy treatment, recreational therapy services and intensive substance abuse treatment for a final total of 46 appointment types (51 − 5 = 46). These clinic types were missing 20% or more of their wait time data and would require a large number of zeroes to be imputed.
The second adjustment was made to the proportions if a parent station did not use all 46 clinic stops. The appointment types parent stations rely on may differ. For example, the same services provided under Women’s Clinic at Station X could be coded under Primary Care at Station Y and Station Y may not use the Women’s Clinic code. If parent stations did not use some appointment types, the national proportions of these appointment types were equally distributed among the appointment types a parent station did use (see Appendix A for a detailed example). Thus, the proportions added up to 1 for each parent station in each month. All individuals who visited the same parent station were assigned the same exogenous wait time for that station in each month.
The bottom panel of Table 1 shows the mean, median and interquartile range of exogenous wait times that were calculated for July, August and September by whether or not the individual experienced an ACSC hospitalization in that month. In contrast to the top panel in Table 1, there is either little difference in the mean and median wait times of individuals who did and did not experience an ACSC hospitalization or individuals who experienced an ACSC hospitalization waited slightly longer.
2.5 Sample selection
A second way that unobserved prior health status could affect both waiting times and outcomes is through sample selection. If, for example, facilities with relatively long wait times attract fewer severely ill patients (because they go elsewhere rather than wait), then long wait times could be associated with relatively favorable outcomes because of unobserved and uncontrolled casemix differences. Alternatively, if wealthier individuals are more likely to use services outside of the VA versus wait, and wealth is correlated with health, then facilities with long waits may attract more severely ill patients.
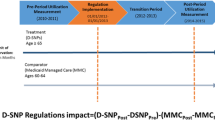
One way to address this problem is to separate in time the selection of the sample and the measurement of outcomes.Footnote 6 If the sample were selected far enough from the outcome measurement, we could study the effect of recent waiting times on outcomes without worrying that sample selection might be correlated with either one. We were able to separate by three months the selection of the study sample (October 2000–March 2001) from the computation of wait times and the assessment of outcomes (July–December 2001). Although sample selection may have been correlated with wait times during the selection period, wait times changed substantially between the two periods. The correlation between average parent station wait times during the first third of the year (January–March) and the last half (July–December) was 0.58.
Therefore, the study population consisted of patients who (1) visited a geriatric outpatient clinic between October 2000 and March 2001 and (2) survived through June 30, 2001. Patients could only enter the sample through March 31, 2001. Starting in July 2001, our measure of wait time was the facility-level exogenous wait time for each month between July and December 2001. For each patient we estimated the probability of experiencing an ACSC hospitalization in each month between July and December 2001 as the outcome (see details under Analyses). Individuals who visited more than one parent station during the sample selection period were excluded (n = 982; 3%) because these individuals had more than one facility-level wait time.
Patients who did not have any outpatient visits between July 2001 and December 2001 were still included in the sample. These patients may not have an outpatient visit because they went outside of the VA system for healthcare, potentially due to long waits for VA care. If these individuals are getting healthcare sooner by going outside of the VA, they may be at a lower risk for ACSC hospitalization compared to individuals who wait for care in the VA. Therefore, it is the more conservative approach to include these individuals in the sample instead of limiting the sample to VA users during the outcome period. The final sample size is 33,538.
2.6 Outcome
The outcome of interest is experiencing an ACSC hospitalization. The dates and ICD-9 codes of all inpatient hospitalizations between July and December 2001 were extracted from both the VA National Patient Care Database (NPCD) and the Medicare MedPAR file. The Medicare data was used to account for hospitalizations that occur outside of the VA system. We used AHRQ methodology to determine which hospitalizations were potentially preventable and excluded hospitalizations for pediatric conditions (e.g. pediatric asthma) (AHRQ 2001). Please refer to AHRQ (2001) for a complete description of the methodology.
2.7 Risk adjustment
Since prior individual health status can confound the relationship between waiting for health care and outcomes, we account for multiple measures of prior individual health status following similar models in the literature (Berlowitz et al. 1997; Mukamel et al. 2000; Porell et al. 1998; Selim et al. 2002) and our previous work (Prentice et al. 2007).Footnote 7 Explanatory variables include age, gender, principal diagnoses and the Charlson index as a measure of the number and seriousness of co-morbid conditions (Charlson et al. 1987; Deyo et al. 1992).Footnote 8 Diagnosis codes from VA inpatient encounters in the 365 days prior to the date of each patient’s first geriatric clinic visit were grouped according to the classification system developed by Rosen et al. (2000). Some of the diagnosis categories developed by Rosen et al. (2000) overlap with diagnosis categories used in the Charlson index. We estimated models that only included either the Charlson index or the diagnosis categories as a test for collinearity. Results were qualitatively similar so both measures were included in the models presented.
Models also included an indicator variable for whether or not an individual experienced an ACSC hospitalization in the 365 days before their first geriatric clinic visit. This variable reflects variation in self-care among patients as well as the effects of past outpatient care. In addition, it isolates the population who are at greatest risk for experiencing a preventable hospitalization because those who have experienced an ACSC hospitalization in the past are known to have conditions that would make them susceptible to experiencing future ACSC hospitalizations. This variable has a significant effect in the models, and the other explanatory variables have similar estimated effects regardless of whether previous ACSC hospitalization is excluded or included.
We used duration analyses to predict the odds of experiencing an ACSC hospitalization in each month between July and December 2001 (see Analyses for details). As time passes, individuals may be at greater risk of experiencing an ACSC hospitalization due to failing health. To control for this we included a variable that counts up the number of observations for each person. For example, the variable was 1 for the July observation, 2 for the August observation, and so on.
Finally, to control for differences in case mix between facilities, a historical 3 month average ACSC hospitalization rate (October through December 2000) for each facility was included as an explanatory variable. Facilities that generally treated patients with a greater burden of illness would be expected to have higher ACSC hospitalization rates.
2.8 Analyses
Data were analyzed using STATA 9.0 (StataCorp et al. 2005). We report the coefficients and marginal effects from stacked heteroskedastic probit models that predict the probability of experiencing an ACSC hospitalization. Each individual had one observation for each month he or she was alive between July and December 2001. Individuals who died were censored in the month that they died. For example, an individual who lived through December 31, 2001 would have six observations. However, an individual who died on August 15, 2001 would have one observation for July and one observation for August. The probability of experiencing an ACSC hospitalization was predicted in each month with a model that included the individual-level risk adjustment variables, a lagged facility-level ACSC hospitalization rate and a facility-level wait time. Facility-level wait time changed each month and was therefore a time varying covariate. All other covariates were time invariant.
Since there were multiple observations per person, observations within individuals are not independent of one another. To account for this we calculated robust standard errors, clustering on individuals. Similarly, observations for individuals who visited the same facilities are likely not independent from one another. Facilities with fewer observations had greater residual variance. To account for this we used a heteroskedastic probit model specifying that the variance of the disturbance term is a linear function of the number of observations per facility divided by 10,000 (Greene 1993). The significant result on the likelihood ratio test of heteroskedasticity (χ2 = 5.81, P = 0.012-Table 3; χ2 = 6.25, P = 0.012-Table 4; χ2 = 6.52, P = 0.011-Table 5) confirmed that this model explained the heteroskedasticity well.
We tested several different functional forms of the wait time including a linear form, categories based on deciles, and categories based on quintiles. The linear form and deciles gave the most detailed understanding of the relationship between facility-level wait times and the probability of experiencing an ACSC hospitalization. We categorized facility-level wait times into less than 22.5 days, 22.50–25.99 days, 26.00–28.99 days, 29.00–31.49 days, 31.50–34.49 days, 34.50–37.49 days, 37.50–40.99 days, 41.00–44.99 days, 45.00–48.99 days, and greater than or equal to 49 days.
Finally, we report heteroskedastic probit (Table 3) and fixed effects heteroskedastic probit models (Tables 4–5). In the fixed effects models, dummy variables for each facility were included to control for unobserved facility characteristics that may be correlated with wait times and that may cause ACSC hospitalizations. In our sample, facilities that are chronically congested and have longer waits have healthier individuals. For example, about 25% of the veterans who visited facilities with an average wait time of 45 days or more had a neurological disease or psychiatric disease, compared to about 31% of veterans across the whole sample with each of these diseases. Similarly, veterans who visited facilities with an average wait time of 45 days were diagnosed with a mean of 2.51 diseases compared to 2.79 for the entire sample and only 4.6% of the veterans who visited facilities with an average wait time of 45 days or more experienced a previous ACSC hospitalization compared to 5.5% in the overall sample. Veterans who visit facilities with an average wait time of less than 45 days do not appear consistently healthier than the overall sample. The fixed effects models ought to do a better job of controlling for unobserved differences in health status due to wait time related selection effects. We present a model without fixed effects as well for comparison.
3 Results
Of the 152 VA medical centers with wait time data, 86 had patients who visited a geriatric outpatient clinic at only one parent station between October 2000 and March 2001. The sample included facilities from 44 states and Washington D.C. States that did not have facilities in the sample include Alaska, New Hampshire, New Jersey, North Dakota, Louisiana and West Virginia. The median facility-level wait time between July and December 2001 was 32.9 days. About 25% of the facility-months had wait times less than or equal to 25.8 and 25% of the facilities had wait times greater than or equal to 42.8 days.
Table 2 gives health status statistics for the geriatric sample, which is elderly and in generally poor health. Ninety-six percent of the sample was male and the mean age was 78 years. About a third of the patients had endocrine disease, neurological disease, psychiatric disease, or sensory disease, and about 20% of the sample had cancer and/or pulmonary disease. Eighty-two percent of the sample had been diagnosed with heart disease. The average patient in the sample had diagnoses in 2.79 of these disease categories, and the mean rating on the Charlson comorbidity index was 0.77. Five and a half percent of the sample had experienced at least one ACSC hospitalization in the previous federal fiscal year. Three percent of the sample died during the 6 month outcome period between July and December 2001 and 5.5% of the sample (n = 1803) experienced at least one ACSC hospitalization in the 6 month outcome period. Seventeen percent of those experiencing an ACSC hospitalization had more than one ACSC hospitalization (n = 365) during the outcome period.
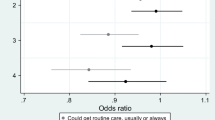
Table 3 shows the coefficients, marginal effects and P-values for the stacked heteroskedastic probit model without fixed effects that predicts the probability of experiencing an ACSC hospitalization in each month between July and December 2001. The probability of experiencing an ACSC hospitalization was significantly increased for veterans who visited a facility with wait times between 34.50 and 44.99 days compared to veterans who visited a facility with wait times of less than 22.5 days. However, veterans who visited a facility with wait times ≥45 days did not significantly differ in their probability of being hospitalized for an ACSC compared to veterans who visited facilities with wait times of less than 22.5 days.
In contrast, Table 4 reports the coefficients, marginal effects and P-values for a fixed effects heteroskedastic probit model with wait time categorized in the same deciles that are reported in Table 3. Except for the coefficient for facility-level wait times between 31.50 and 34.49 which is significant at the P < 0.10 level, the probability of experiencing an ACSC hospitalization for wait times was significantly increased for veterans who visited a facility with wait times greater than 29 days compared to veterans who visited facilities with wait times of less than 22.5 days. Specifically, the probability of experiencing an ACSC hospitalization increased by 0.30 percentage points for facility-level waits between 29 and 31.49 days, 0.23 percentage points for facility-level waits between 31.50 and 34.49 days, 0.38 percentage points for facility-level waits between 34.50 and 37.49 days, 0.36 percentage points for facility-level waits between 37.50 and 44.99 days, 0.34 percentage points for facility-level waits between 45 and 48.99 days and 0.57 percentage points for facility-level waits of 49 days or more. Generally, the probability of experiencing an ACSC hospitalization increases as facility-level wait time increases.
The positive and significant relationship between facility-level waits and the probability of experiencing an ACSC hospitalization is further confirmed in Table 5. This table reports the coefficients, marginal effects and P-values of a fixed effects heteroskedastic probit model where wait time is a linear variable. The probability of experiencing an ACSC hospitalization is significantly increased by 0.010 percentage points for each day the facility-level wait increases.
Other explanatory variables to control for facility-level case mix and individual health status generally have the expected association with the probability of experiencing an ACSC hospitalization (Tables 3–5). Females had a significantly lower probability of experiencing an ACSC hospitalization than males. Age, the Charlson index of comorbidity and the lagged facility-level ACSC hospitalization rate all had significant positive effects on the probability of being hospitalized for an ACSC. Veterans who were previously hospitalized for an ACSC condition were about 1.9 percentage points more likely to be hospitalized for an ACSC condition in the outcome period. Veterans who had a diagnosis of heart, endocrine or pulmonary disease in the prior year had significantly higher probabilities of experiencing an ACSC hospitalization compared to veterans who were not diagnosed with each of these diseases.
4 Discussion
These results show that visiting facilities with longer wait times increased the probability of experiencing an ACSC hospitalization even when controlling for prior individual health status. Although, there is a significant positive association between facility-level wait times in a linear form and the probability of experiencing an ACSC hospitalization (Table 5), the decile categorization of wait times suggests there is a step function effect. Generally, veterans who visit facilities with waits of greater than 29 days have a higher probability of experiencing an ACSC hospitalization compared to veterans who visit facilities with waits of less than 22.5 days. In contrast, veterans who visit facilities with waits between 22.5 and 28.99 days are not at an increased risk of ACSC hospitalization compared to those who visit facilities with waits of less than 22.5 days. These results are consistent with our previous work that found that visiting facilities with longer waits for outpatient care increased risk-adjusted mortality among the same population of veterans. A step function effect was also found in this research with veterans who visited facilities with waits of 31 days or more significantly more likely to die in the six month follow-up period compared to veterans who visited a facility with wait times of less than 31 days (Prentice et al. 2007). In contrast, to our previous work, however, our current models suggest that there are additional negative consequences for wait times greater than or equal to 49 days. The marginal effects at these long wait times was nearly twice as large as the effect for waits between 29 and 48.9 days.
We conducted a robustness check that examined the relationship between waiting for outpatient care and hospitalizations due to trauma to further confirm the reported relationship between waiting for outpatient care and ACSC hospitalization. If long waits for outpatient care increase the probability of ACSC hospitalization due to delays in diagnosis and treatment, then there should not be a relationship between waiting for outpatient care and hospitalizations due to events that could not be prevented with outpatient care (e.g. accidents, fractures). We selected hospitalizations that had an admission principal diagnosis (ICD-9) code which were indicative of trauma (e.g. fractures, dislocation, intracranial injury, burns). Three quarters of the hospitalizations identified were due to fracture, and almost half were due to hip fracture which was not surprising given the geriatric nature of the sample.
Appendix B presents fixed effects heteroskedastic probit models that predict hospitalizations due to trauma controlling for wait time, age, gender and health conditions. There was no systematic relationship between waiting times and trauma hospitalizations. The waiting time variables in both the decile and linear context were non-significant. However, age and being diagnosed with a neurological condition were positively and significantly associated with traumatic hospitalizations at the P < 0.05 level. The probability of falling or injury likely increases as one ages or if one has a condition that may affect balance and stability. These results further support our finding that waiting for outpatient care increases the likelihood of experiencing an ACSC hospitalization.
Our sample is all individuals who visited a geriatric outpatient clinic in 2001. For this specific geriatric population, the VA goal to schedule appointments within 30 days of a request for an appointment seems reasonable if the goal is to prevent potentially negative health outcomes resulting from delayed access to care. However, individuals in the sample could have a wide range of clinical conditions and the effect of wait times on the likelihood of experiencing an ACSC hospitalization may be stronger for some clinical conditions than for others. Future research should examine the relationship between waiting for care and different types of health outcomes among populations that are more narrowly defined (e.g. diabetics) and determine the threshold that individuals can wait before more serious health outcomes develop.
If future research supports the idea that long waits for outpatient care negatively affects health for different clinical populations, there are potential health improvements and cost savings that could result from the U.S. health care system beginning to monitor wait times and implement policies to decrease them where needed. Some strategies for shortening wait times are already known and can be implemented through appropriate health care policy. For example, several studies have found that wait times can be shortened by implementing the Advanced Clinic Access model (Gordon et al. 2004; Murray et al. 2003; VanDeusen Lukas et al. 2004). The Advanced Clinic Access model changes how appointments are scheduled, analyzing the supply of appointments relative to the demand for appointments and changing scheduling procedures so that demand is met. After clearing the backlog of patients waiting for appointments, facilities then attempt to see patients the same day appointments are requested. Since all physicians maintain open slots in their schedule, patients see their regular physician, eliminating recheck appointments that result when a patient goes to a different clinician because of a long wait to see their regular clinician (Murray et al. 2003). The results of this study strengthen the case for broad implementation of interventions such as Advanced Clinic Access especially if costly health outcomes, such as inpatient hospitalizations, could potentially be prevented.
However, future research is also needed to improve policymakers’ and researchers’ understanding of the supply and demand characteristics that affect the length of time patients wait for outpatient care. No scheduling system, including Advanced Clinic Access, will be successful if demand for services is consistently greater than clinic capacity (Murray et al. 2003). This is likely to be the case for some components of the U.S. health care system and costlier interventions such as increasing the supply of physicians will be required. Policymakers in the United States should consider applying strategies used by international health care systems to manage and decrease wait times. Examples of these strategies include setting waiting time targets, targeting funding to increase hospital and health care system capacity, and addressing potential health care system inefficiencies by identifying and sharing good practices (Wilcox et al. 2007).
Notes
Hospitalizations that potentially could have been prevented through appropriate outpatient care have been referred to as “ambulatory care sensitive,” “preventable,” “avoidable,” or “prevention quality indicators” (AHRQ 2001; Culler et al. 1998). We use the term ACSC hospitalization throughout this article.
The wait time measure is based on next available appointments versus follow-up appointments that may be scheduled in advance. This may reduce the impact of waiting time on health outcomes. However, patients cannot request follow-up appointments until the doctor has requested to see them again. Our wait time measure based on next available appointments is an overall measure of congestion at different VA facilities and both newly requested and follow-up appointments at facilities with greater congestion will be delayed. Furthermore, patients who need to reschedule follow-up visits or who have complications between follow-up visits will require next available appointments and rely on the appointment type our wait time measure is based on.
For ease of presentation, “facility” and “parent station” are used interchangeably throughout the article to refer to a VA parent station.
Only 37% of the clinic visits in the entire sample were to a geriatric outpatient clinic. Thus, the sample used a wide range of health care services beyond geriatric outpatient clinics.
In the final sample, 12% of the clinic appointments were imputed with 0.
The standard correction for selection bias involves estimating a first stage selection model and explicitly accounting for the expected value of the disturbance term from that model in the second stage equation of interest. Because we do not have veterans in our sample who chose not to come to a VA medical center for care, we cannot take this approach.
Our previous work examining the relationship between wait times and mortality included the same explanatory variables to risk-adjust for prior individual health status presented in this article. However, the mortality models also included whether or not a patient had a 50% or more service-connected disability (e.g. a condition or disability that the VA has determined was incurred or aggravated by military service). In models predicting ACSC hospitalization, service-connected disability had no significant effect. It was excluded in the final models because of the loss of observations due to missing values on service-connected disability.
References
Baar, B.: New patient montitor: data definitions. Veteran Health Administration Support Services Center (2005a)
Baar, B.: Next available detail data: Data definitions. Veterans Health Administration Support Services Center (2005b)
Berlowitz, D.R., Brandeis, G.H., Anderson, J., Du, W., Brand, H.: Effect of pressure ulcers on the survival of long-term care residents. J. Gerontol. A Biol. Sci. Med. Sci. 52(2), M106–M10 (1997)
Charlson, M.E., Pompei, P., Ales, K.L., MacKenzie, C.R.: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40(5), 373–383 (1987)
Culler, S.D., Parchman, M.L., Przybylski, M.: Factors related to potentially preventable hospitalizations among elderly. Med. Care 36(6), 804–817 (1998)
Deyo, R.A., Cherkin, D.C., Ciol, M.A.: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J.Clin. Epidemiol. 45(6), 613–619 (1992)
Gordon, P., Chin, M.: Achieving a New Standard in Primary Care for Low-income Populations: Case Studies of Redesign and Change Through a Learning Collaborative. pp. 17. The Commonwealth Fund, New York (2004)
Greene, W.H.: Econometric Analysis, 2nd edn. Prentice Hall, Upper Saddle River (1993)
Institute of Medicine (IOM): The Committee on the Quality of Health Care in America, Crossing the Quality Chasm: A New Health System for the 21st Century. Institute of Medicine, Washington D.C. (2004)
Kenagy, J.W., Berwick, D.M., Shore, M.F.: Service quality in health Care. J. Am. Med. Assoc. 281(7), 661–65 (1999)
Mukamel, D.B., Spector, W.D.: Nursing home costs and risk-adjusted outcome measures of quality. Med. Care 38(1), 78–89 (2000)
Murray, M., Berwick, D.M.: Advanced access: reducing waiting and delays in primary care. J. Am. Med. Assoc. 289, 1035–40 (2003)
Murray, M., Bodenheimer, T., Rittenhouse, D., Grumbach, K.: Improving timely access to primary care: case studies of the advanced access model. J. Am. Med. Assoc. 289(8), 1042–46 (2003)
Porell, F., Caro, F.G., Silva, A., Monane, M.: A longitudinal analysis of nursing home outcomes. Health Serv. Res. 33(4), 835–65 (1998)
Prentice, J.C., Pizer, S.D.: Delayed access to health care and mortality. Health Serv. Res. 42(2), 644–662 (2007)
AHRQ: Quality indicators-guide to prevention quality indictors: hospital admission for ambulatory care sensitive conditions. Agency for Healthcare Research and Quality Rockville; AHRQ Pub No. 02-R0203 (2001)
Rosen, A., Wu, J., Chang, B.H., Berlowitz, D., Ash, A., Moskowitz, M.: Does diagnostic information contribute to predicting functional decline in long-term care? Med. Care 38(6), 647–59 (2000)
Selim, A.J., Berlowitz, D.R., Fincke, G., Rosen, A.K., Ren, X.S., Christiansen, C.L., Cong, Z., Lee, A., Kazis, L.: Risk-adjusted mortality rates as a potential outcome indicator for outpatient quality assessments. Medical Care 40(3), 237–45 (2002)
StataCorp. STATA (release 9.0) Statistical Software. StataCorp, College Station, TX (2005)
United States Government Accounting Office (U.S. GAO): More national action needed to reduce waiting times, but some clinics have made progress. United States General Accounting Office. GAO-01–953, (2001)
VanDeusen Lukas, C., Meterko, M., Mohr, D., Seibert, M.N.: The Implementation and Effectiveness of Advanced Clinic Access. Health Services Research and Development Management Decision and Research Center. Office of Research and Development, Department of Veteran Affairs, Boston (2004)
Veterans Health Administration (VHA): Decision support office, “summary of active stop codes; Reference I.,” Washington D.C., 2004. [accessed on January 15, 2005]. Available at http://vaww.dss.med.va.gov/programdocs/pd_oident.asp
Wilcox, S., Seddon, M., Dunn S., Edwards, R.T., Pearse, J., Tu, J.V.: Measuring and reducing waiting times: a cross-national comparison of strategies. Health Affairs 26(4), 1078–1087 (2007)
Acknowledgements
Salary support for Dr. Prentice was provided by a Health Services Research Fellowship from the Center for Health Quality, Outcomes and Economic Research in the Department of Veteran Affairs. Additional support was provided under Grant Nos. IIR-04-233-1 & IAD-06-112-3 from the Department of Veterans Affairs, Health Services Research & Development Service. The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Example of exogenous wait time calculation*
Appointment type | October–March (Sample selection period) | July wait times | August wait times | ||||
|---|---|---|---|---|---|---|---|
Station 1 | Station 2 | Station 1 | Station 2 | Station 1 | Station 2 | ||
# of appointments | # of appointments | National proportion of appointments | Wait in days | Wait in days | Wait in days | Wait in days | |
Primary care | 18 | 13 | 0.37 | 20.8 | 36.5 | 15.2 | 34.2 |
Psychology | 8 | 13 | 0.25 | 33.2 | Missing | 20.9 | 10.0 |
Optometry | 12 | 10 | 0.26 | 25.5 | 27.4 | 23.8 | 28.4 |
Women’s clinic | 10 | – | 0.12 | 21.2 | – | 22.5 | – |
Wait time calculation | (0.37 × 20.8) + (0.25 × 33.2) + (0.26 × 25.5) + (0.12 × 21.2) = 25.17 | (0.41 × 36.5) + (0.29 × 00.0) + (0.30 × 27.4) = 23.19 | (0.37 × 15.2) + (0.25 × 33.2) + (0.26 × 25.5) + (0.12 × 21.2) = 20.02 | (0.41 × 34.2) + (0.29 × 10.0) + (0.30 × 28.4) = 25.44 | |||
Appendix B
Coefficients and P-values of a Fixed Effects Heteroskedastic Stacked Probit Model Predicting Hospitalizations Due to Trauma, 2001 (n = 187, 526 person months; 31,830 people)§
Independent variables | Coefficient | P value | Coefficient | P value |
|---|---|---|---|---|
Facility wait time in days–linear | 0.0023 | 0.499 | ||
Facility wait time in days (Ref = <22.5 days) | ||||
22.50–25.99 days | −0.0249 | 0.732 | ||
26.00–28.99 days | −0.0248 | 0.749 | ||
29.00–31.49 days | −0.0823 | 0.425 | ||
31.50–34.49 days | −0.0043 | 0.954 | ||
34.50–37.49 days | −0.0381 | 0.655 | ||
37.50–40.99 days | 0.1143 | 0.196 | ||
41.00–44.99 days | −0.0634 | 0.534 | ||
45.00–48.99 days | 0.0316 | 0.751 | ||
> = 49 days | 0.1419 | 0.378 | ||
Female (Ref = male) | 0.0660 | 0.371 | 0.0662 | 0.366 |
Age | 0.0150 | <0.001 | 0.0150 | <0.001 |
Charlson index | 0.0052 | 0.591 | 0.0051 | 0.596 |
Cancer (Ref = no)* | −0.1061 | 0.112 | −0.1061 | 0.106 |
Endocrine disease (Ref = no) | 0.0223 | 0.680 | 0.0212 | 0.693 |
Heart disease (Ref = no) | −0.0340 | 0.589 | −0.0332 | 0.592 |
Neurological disease (Ref = no) | 0.1079 | 0.047 | 0.1077 | 0.046 |
Psychiatric disease (Ref = no) | 0.0899 | 0.085 | 0.0907 | 0.082 |
Pulmonary disease (Ref = no) | −0.0202 | 0.718 | −0.0197 | 0.724 |
Sensory disease (Ref = no) | −0.0437 | 0.426 | −0.0434 | 0.429 |
Other disease (Ref = no) | 0.0735 | 0.232 | 0.0731 | 0.233 |
Number of disease categories | 0.0328 | 0.453 | 0.0325 | 0.455 |
Count of observations per person@ | 0.0107 | 0.250 | 0.0104 | 0.228 |
Number of observations per clinic divided by 10000 | −0.3254 | 0.126 | −0.3301 | 0.123 |
Likelihood ratio test of heteroskedacity | Likelihood ratio test of heteroskedacity | |||
χ2 = 2.34, degrees of freedom = 1; P = 0.126 | χ2 = 2.38, degrees of freedom = 1; P = 0.123 | |||
Rights and permissions
About this article
Cite this article
Prentice, J.C., Pizer, S.D. Waiting times and hospitalizations for ambulatory care sensitive conditions. Health Serv Outcomes Res Method 8, 1–18 (2008). https://doi.org/10.1007/s10742-007-0024-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10742-007-0024-5