Abstract
There is ongoing controversy regarding the association between loop diuretics (LD), especially in high doses, and adverse clinical outcomes in outpatients with heart failure (HF). We performed a systematic review of the evidence for LD in outpatients with HF. We searched MEDLINE, EMBASE, and Cochrane Clinical Trial Collection to identify controlled studies, evaluating the association between LD and morbidity and mortality in patients with HF. The primary endpoint was all-cause mortality and secondary endpoint HF hospitalizations. Quantitative analysis was performed by generating forest plots and pooling adjusted risk estimates across studies using random effects models. Between-study heterogeneity was assessed through Q and I2 statistics. Twenty-four studies with a total of 96,959 patients were included. No randomized studies were identified. Use of LD was associated with increased all-cause mortality compared with non-use (pooled adjusted risk estimates, 1.18; P = 0.001) and increased HF hospitalization rates (pooled adjusted risk estimates, 1.81; P < 0.001). These associations remained significant after excluding studies that included HF patients at discharge from hospital (pooled adjusted risk estimates, 1.31 and 1.89, respectively; P < 0.001 for both). High-dose LD (median dose 80 mg) were also associated with increased all-cause mortality (pooled adjusted risk estimates, 1.99; P < 0.001) compared with low-dose LD. Again, this association remained significant after excluding studies that included HF patients at discharge from hospital (pooled adjusted risk estimates, 1.33; P < 0.001). Existing evidence indicates that LD, especially in high doses, are associated with increased all-cause mortality and HF hospitalization rates. For this reason, prospective, randomized studies are warranted to clarify whether these associations indicate causality or are merely an epiphenomenon due to disease severity. Systematic review registration: PROSPERO database registration number CRD42020153239. Date of registration: 28 April 2020.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Loop diuretics (LD) remain the mainstay of treatment for relieving congestion in patients with heart failure (HF), irrespectively of the underlying ejection fraction [1, 2]. Over 80% of HF outpatients are treated with a per os diuretic, a proportion which is consistent both in selected and unselected HF populations [3,4,5,6]. However, the quality of data supporting this “standard of care” strategy is sub-optimal, based on expert opinions and a single meta-analysis of a few, small in numbers and out of date randomized studies [7], the clinical relevance of which has been directly challenged [8]. In any case, the paucity of hard evidence from large, randomized trials regarding the proper use of diuretics in HF patients is unequivocal and striking [9]. This lack of data becomes even more remarkable when considering that the use of LD, especially in high doses, has been associated with adverse clinical outcomes in HF patients in multiple cohort studies [10,11,12].
To our knowledge, the data concerning LD and clinical outcomes in HF patients has not been systematically reviewed. To this end, we undertook a systematic review and meta-analysis of the use and dose of LD in patients with HF. We examined randomized and non-randomized data and examined subpopulations with exclusively reduced left ventricular ejection fraction (HFrEF) vs. mixed HF populations and those at stable outpatient status vs. patients at hospital discharge.
Methods
The present study was conducted according to the PRISMA statement (Table A1-Appendix) [13]. The review protocol has been registered in PROSPERO: International Prospective Register of Systematic Reviews (number: CRD42020153239) [14].
Identification and selection of studies
MEDLINE, EMBASE, clinicaltrials.gov, and Cochrane Clinical Trial Collection were searched on October 15, 2019, with a combinatorial approach (Boolean operator “AND”) of three broader search terms. The broader search terms were derived using the Boolean operator “OR” between synonyms for “chronic heart failure,” “outcomes,” and “diuretics.” Detailed descriptions of the terms used for MEDLINE and EMBASE searches are outlined in Appendix Table A2. The search was restricted to the period from January 1, 1990, onwards, out of concern for a high risk of imprecision in the clinical diagnosis of HF and the different pharmacologic background (and therefore high possibility of clinical irrelevance) of studies prior to 1990. Only articles written in English were eligible, while there was no restriction regarding publication status. The reference lists of previous reviews and a recent position paper of the European Society of Cardiology relevant to our topic were hand-screened for studies [9, 15, 16], whereas references of the included articles were screened for additional studies. If needed, authors were contacted to request unpublished original papers or further details not available on the official version.
Study eligibility criteria included (a) comparison of loop diuretics (furosemide, torasemide, bumetanide, azosemide) with placebo/control or/and comparison of high doses of loop diuretics (HDLD) with low doses of loop diuretics (LDLD); (b) adult patients diagnosed with HF; (c) follow-up ≥ 6 months, as the administration of LD for a shorter period was considered unlikely to significantly impact outcomes; and (d) report of the outcomes of interest, i.e., all-cause mortality and/or HF hospitalization. HF definition included patients with HF symptoms irrespectively of left ventricular ejection fraction (LVEF). We excluded studies if they included patients with acute HF or compared one LD with another LD or/and another active comparator. However, HF patients at time of hospital discharge were included. Ethical approval was not required, as no patients were recruited.
The search was independently performed by two reviewers (CJK and MB). Mendeley reference manager was used to remove duplicates. All titles and abstracts were screened individually by all authors, in order to select those that met the inclusion criteria. Differences in assessment of eligibility between reviewers were resolved through discussion and consensus.
Risk of bias
Risk of bias (RoB) within studies was assessed using the Cochrane Risk Of Bias In Non-Randomized Studies–of Interventions (ROBINS-I) tool. The assessment was performed at the study level and regarded components recommended by the Cochrane Collaboration for non-randomized studies, namely confounding, selection of participants, classification of interventions, deviations from intended interventions, missing data, measurement of outcomes, and selection of the reported result [17]. For each component, trials were categorized as low, moderate, serious, critical, or as having no information on risk of bias. Two reviewers (CJK and MB) performed their personal assessment and any disagreements were discussed until consensus was reached.
Risk of bias across studies was evaluated by assessing meta-bias. Meta-bias was evaluated by drawing funnel plots of the included studies for the different study outcomes. A rule of thumb of ten studies per study outcome was used as a cut-off to draw funnel plots.
Data extraction
A systematic approach was used to extract the relevant variables from the selected studies. The variables for which data were sought are shown in detail in Table A3 (Appendix) and regarded study identity and design, patient population, intervention, and outcomes. All authors extracted study characteristics and data input was cross-validated between reviewer databases.
Qualitative and statistical analysis
Data were combined in a systematic review, forest plots, and, if appropriate, in a meta-analysis. We set two studies as the minimum number for quantitative synthesis of data in a meta-analysis for each study parameter. Because heterogeneity between studies was expected, we pooled adjusted risk estimates across studies using random effects models with inverse variance weighting as recommended in the Cochrane handbook to summarize the associations between LD use (and dose) on mortality and hospitalizations [18]. For studies evaluating endpoints at multiple time points, short-term outcomes (6 months to 2 years) were used when possible for the pooling of the results. Heterogeneity was assessed by the Q statistic; however, due to its limited power to rule out heterogeneity, a P value threshold of 0.10 was used. A quantitative analysis of the impact of heterogeneity using the I2 statistic was also performed. I2 values > 50% were considered highly heterogeneous.
Three subgroup analyses to explore heterogeneity had been pre-specified (randomized vs. non-randomized studies, studies only with HFrEF [left ventricular ejection fraction ≤ 45%] vs. mixed HF patients and studies examining patients at hospital discharge vs. stable outpatients).
All P values were two-tailed with statistical significance set at 0.05 (if not otherwise specified) and confidence intervals (CI) computed at 95% level. All analyses were performed with the use of Stata 15 Software (StataCorp LLC, TX, USA).
Results
Identified and eligible studies
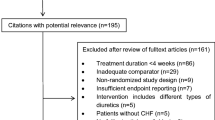
The number of identified and screened studies is indicated in Fig. 1. Our initial search identified a total 3995 studies from 1990 onwards; after removal of duplicates and screening of titles, abstracts, and full-texts, 24 studies were included in the qualitative synthesis (Table 1).
Characteristics of included studies
No randomized controlled trials of the use of or dose of LD in patients with HF were identified. The studies enrolled 96,959 patients who were followed for 6 up to a mean of 70 months. The number of patients analyzed ranged from 173 up to 26,218.
Risk of bias within studies
All included non-randomized studies were assessed as presenting moderate to serious risk of bias, driven primarily by confounding, missing data and selection of the reported result. On the other hand, selection of participants, classification of interventions, deviations from intended interventions, and measurement of outcomes were not identified as major sources of risk of bias among the selected studies.
Risk of bias across studies
Funnel plots were drawn for assessment of meta-bias in regard to all-cause mortality among studies examining LD vs. no LD (Fig. 2a) and high-dose LD vs. low-dose LD (Fig. 2b). Importantly, assessing meta-bias through funnel plots for HF hospitalizations was not feasible as the rule of thumb of ten studies was not fulfilled for this outcome. Funnel plots for both groups of studies (yes vs. no and high- vs. low dose) look asymmetrical as there appear to be more studies missing on the left-hand side. The source of risk of bias across studies can only be speculated and could be attributed to publication bias, substantial heterogeneity, or even chance.
Results of individual studies and synthesis of results
All-cause mortality
All-cause mortality was frequently investigated and reported among studies. Ten studies reported adjusted HRs for the association between all-cause mortality and use of LD (vs. no use), whereas ten was also the number of studies that provided adjusted HRs for the association between all-cause mortality and high doses (vs. low doses) of LD.
LD use (vs. no use) was associated with increased all-cause mortality (pooled adjusted risk estimates, 1.18; 95% CI 1.16–1.20, P = 0.001 [Fig. 3a]), as were high doses of LD (pooled adjusted risk estimates, 1.99; 95% CI 1.86–2.13, P < 0.001) compared with low doses of LD (Fig. 3b).
In additional subgroup analyses for all-cause mortality, LD use (vs. no use) was associated with increased all-cause mortality both among studies which included only patients with HFrEF (N = 4) (pooled adjusted risk estimates, 1.33; 95% CI 1.22–1.45, P < 0.001 [Fig. 4a) and among studies which included mixed HF patients (N = 6) (pooled adjusted risk estimates, 1.17; 95% CI 1.15–1.19, P < 0.001 [Fig. 4b]). Similarly, high doses of LD (vs. low doses) were associated with increased all-cause mortality in both studies with exclusively HFrEF patients (N = 6) (pooled adjusted risk estimates, 1.30; 95% CI 1.16–1.45, P < 0.001 [Fig. 4c]) and among studies which included mixed HF patients (N = 4) (pooled adjusted risk estimates, 2.52; 95% CI 2.32–2.74, P < 0.001 [Fig. 4d]).
Pooled adjusted risk estimates of all-cause mortality for patients receiving vs. not receiving LD among studies including patients with a HFrEF only and b mixed left ventricular ejection fractions. Pooled adjusted risk estimates of all-cause mortality for patients receiving high vs. low doses of LD among studies including patients with c HFrEF only and d mixed left ventricular ejection fractions
In the second subgroup analysis, LD use was associated with increased all-cause mortality among studies which included only patients at hospital discharge (N = 2) (pooled adjusted risk estimates, 1.16; 95% CI 1.14–1.18, P < 0.001 [Fig. 5a]) and among studies which exclusively included HF outpatients (N = 8) (pooled adjusted risk estimates, 1.31; 95% CI 1.25–1.38, P < 0.001 [Fig. 5b]). Similarly, high doses of LD were significantly associated with increased all-cause mortality in both studies with patients at discharge (N = 4) (pooled adjusted risk estimates, 2.88; 95% CI 2.63–3.16, P < 0.001 [Fig. 5c]) and among studies which included only HF outpatients (N = 6) (pooled adjusted risk estimates, 1.33; 95% CI 1.21–1.46, P < 0.001 [Fig. 5d]).
Pooled adjusted risk estimates of all-cause mortality for patients receiving vs. not receiving LD among studies including a patients at hospital discharge and b only outpatients. Pooled adjusted risk estimates of all-cause mortality for patients receiving high vs. low doses of LD among studies including c patients at hospital discharge and d only outpatients
The third pre-specified subgroup analysis (randomized vs. non-randomized studies) could not be performed as no randomized studies were identified.
Heart failure hospitalizations
HF hospitalizations were assessed and reported in less than 50% of the included studies. Five studies reported adjusted HRs for association between HF hospitalizations and use of LD (vs. no use), whereas three studies provided adjusted HRs for association between HF hospitalizations and high doses (vs. low doses) of LD.
LD use was associated with increased risk for HF hospitalizations (pooled adjusted risk estimates, 1.81; 95% CI 1.60–2.05, P < 0.001 [Fig. 6a]). High doses of LD were also associated with increased risk for HF hospitalizations (pooled adjusted risk estimates, 1.58; 95% CI 1.44–1.73, P < 0.001]) compared with low doses of LD (Fig. 6b).
In additional subgroup analyses for HF hospitalizations, LD use (vs. no use) was associated with increased HF hospitalizations among studies which included only HFrEF patients (N = 4) (pooled adjusted risk estimates, 1.89; 95% CI 1.65–2.16, P < 0.001 [Fig. 7a]). Similarly, high doses of LD (vs. low doses) were associated with increased risk for HF hospitalizations in studies with exclusively HF outpatients (N = 2) (pooled adjusted risk estimates, 1.59; 95% CI 1.44–1.74, P < 0.001 [Fig. 7b]). Pooling of HRs for studies with patients including mixed LVEFs was not feasible for either outcome (N = 1 for each).
Pooled adjusted risk estimates of HF hospitalization for a patients receiving vs. not receiving LD and b receiving high vs. low doses of LD among studies including patients with HFrEF only. Pooled adjusted risk estimates of HF hospitalization for c outpatients receiving vs. not receiving LD and d outpatients receiving high vs. low doses of LD
In the second subgroup analysis, LD use was associated with increased HF hospitalizations among studies which included only HF outpatients (N = 4) (pooled adjusted risk estimates, 1.89; 95% CI 1.65–2.16, P < 0.001 [Fig. 7c]), whereas pooling of HRs for studies with patients at hospital discharge was not feasible (N = 1). Similarly, high doses of LD were significantly associated with increased risk for HF hospitalizations in studies with outpatients (N = 2) (pooled adjusted risk estimates, 1.74; 95% CI 1.53–1.97, P < 0.001 [Fig. 7d]), whereas pooling of HRs for studies with patients at hospital discharge was again not feasible (N = 1).
The third pre-specified subgroup analysis (randomized vs. non-randomized studies) could not be performed as no randomized studies were identified.
Discussion
The main findings of this meta-analysis on the associations between LD use and dose with hard clinical outcomes in patients with HF are (a) no contemporary, clinically relevant randomized studies exist; (b) LD use (vs. non-use) and high dose LD (vs. low dose) are significantly associated with increased risk for all-cause mortality and HF hospitalization; (c) these associations are strong and significant both among studies including exclusively patients with HFrEF and studies with mixed HF populations; and (d) these associations are strong and significant in both studies including HF outpatients and HF patients at hospital discharge.
Although our study adheres to PRISMA reporting, it included studies with significant diversity and patient populations with a wide range of HF severity. Notably, all 24 studies were observational; the few randomized controlled trials on the topic have been either LD dose decrease or withdrawal studies and were thus excluded from the analysis [39,40,41]. Nonetheless, our systematic review provides the best, to date, available evidence to suggest that receipt of LD (vs. non-use) and receipt of high-dose LD (vs. low-dose) is significantly associated with increased risk of death and HF hospitalization in patients with chronic HF, irrespectively of ejection fraction and timing of dose investigation (hospital discharge or “stable” outpatient state).
Our study provides evidence to support that LD use, especially in higher doses, is associated with worse clinical outcomes. This of course may be simply a risk marker of greater HF severity among patients who were receiving higher LD doses, but uniquely, our meta-analysis utilized hazard ratios after adjustment for variables that may have affected both LD doses and outcomes. Even after adjustment for these potential confounders, the risk associated with LD use remained approximately 20% higher for all-cause death and approximately 80% increased for HF hospitalizations. On the other hand, high LD dose also presented with a twofold higher risk for all-cause mortality. This magnitude of risk excess after extensive adjustment suggests that it is likely, although not proven, that LD use, especially in higher doses, might not only represent markers of HF severity but also true risk factors for worse outcomes. In their study, Mielniczuk et al. [23] observed that the association between LD and adverse outcomes was rendered insignificant after adjustment for clinical stability, implying that higher doses of LD were a proxy for clinical instability and were not responsible on their own for the excessive mortality; however, in another analysis from the European Long-Term HF registry among > 8000 HF outpatients, it was demonstrated that associations between LD dose and outcomes were independent of clinical stability and other factors of disease severity [36]. Several mechanisms have been proposed as putative explanations for the unfavorable associations between LD and the clinical outcomes of HF patients. LD cause depletion of the effective blood volume and through this stimulate the sympathetic nervous and renin-angiotensin-aldosterone systems, contributing to further HF progression and dismal outcomes [42, 43]. The association of high-dose LD with increased mortality in patients with elevated but not normal blood urea nitrogen further suggests that neurohormonal activation may mediate these dismal effects [24]. Others have implicated electrolyte depletion and induction of fatal arrhythmias as a main contributor to the negative effects of LD [44]. Moreover, high doses of LD have been associated with an increased incidence of renal dysfunction in HF patients [45], a well-established predictor of morbidity and mortality in patients hospitalized for HF decompensation [45]. Furthermore, inappropriately high doses of LD might hamper up-titration of guideline-directed medical therapy and may result through this mechanism in sub-optimal outcomes [46].
Limitations
Our study has several important limitations. First, heterogeneity in the criteria employed to diagnose HF and HFrEF and in the design of studies represent major limitations, as they may have resulted in heterogeneous patient populations. Furthermore, study outcomes were not consistently reported in all included studies. All these limitations may in part be responsible for significant heterogeneity observed among the pooled analyses for some outcomes. Moreover, this meta-analysis was not performed on a patient level but collected aggregate data from studies of different cohorts. This fact precluded performance of subgroup analysis in a specific subpopulation.
Despite these caveats, this meta-analysis may have significant therapeutic implications. In view of the aggregate dismal associations demonstrated, LD should be used at the lowest possible dose and should be adjusted to individual needs. The feasibility, clinical parameters which can guide, and potential beneficial effects of such a strategy have been recently recognized [46, 47].
Conclusions
Existing evidence indicates that LD, especially in high doses, are associated with increased all-cause mortality in patients with HF. The use of LD is also associated with higher rates of HF hospitalizations. Although this study represents the most comprehensive, to date, review of associations of LD use and dose with hard clinical outcomes in patients with HF, large prospective studies are warranted to provide definitive answers.
Data availability
Not provided.
References
Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Katz SD, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WH, Teerlink JR, Walsh MN (2010) HFSA 2010 comprehensive heart failure practice guideline. J Card Fail 16(6):e1–e194
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force Members; Document Reviewers (2016) 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8):891–975
Peacock WF, Costanzo MR, De Marco T, Lopatin M, Wynne J, Mills RM, Emerman CL, ADHERE Scientific Advisory Committee and Investigators (2009) Impact of intravenous loop diuretics on outcomes of patients hospitalized with acute decompensated heart failure: insights from the ADHERE registry. Cardiology 113(1):12–19
Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, Ferrari R, Piepoli MF, Delgado Jimenez JF, Metra M, Fonseca C, Hradec J, Amir O, Logeart D, Dahlström U, Merkely B, Drozdz J, Goncalvesova E, Hassanein M, Chioncel O, Lainscak M, Seferovic PM, Tousoulis D, Kavoliuniene A, Fruhwald F, Fazlibegovic E, Temizhan A, Gatzov P, Erglis A, Laroche C, Mebazaa A, Heart Failure Association (HFA) of the European Society of Cardiology (ESC) (2016) European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail 18(6):613–625
Cohn JN, Tognoni G, Valsartan Heart Failure Trial Investigators (2001) A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med 345(23):1667–1675
Zannad F, JJ MM, Krum H, van Veldhuisen DJ, Swedberg K, Shi H, Vincent J, Pocock SJ, Pitt B, EMPHASIS-HF Study Group (2011) Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 364(1):11–21
Faris RF, Flather M, Purcell H, Poole-Wilson PA, Coats AJ (2012) Diuretics for heart failure. Cochrane Database Syst Rev (2):CD003838
Kapelios CJ, Malliaras K, Nanas JN (2016) Dosing of loop diuretics in chronic heart failure: it’s time for evidence. Eur J Heart Fail 18(10):1298
Kapelios CJ, Malliaras K, Kaldara E, Vakrou S, Nanas JN (2018) Loop diuretics for chronic heart failure: a foe in disguise of a friend? Eur Heart J Cardiovasc Pharmacother 4(1):54–63
Kapelios CJ, Kaldara E, Ntalianis A, Sousonis V, Repasos E, Sfakianaki T, Vakrou S, Pantsios C, Nanas JN, Terrovitis JV (2015) High furosemide dose has detrimental effects on survival of patients with stable heart failure. Hell J Cardiol 56:154–159
Eshaghian S, Horwich TB, Fonarow GC (2006) Relation of loop diuretic dose to mortality in advanced heart failure. Am J Cardiol 97:1759–1764
Abdel-Qadir HM, Tu JV, Yun L, Austin PC, Newton GE, Lee DS (2010) Diuretic dose and long-term outcomes in elderly patients with heart failure after hospitalization. Am Heart J 160:264–271.e1
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Available online at: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=153239. Last accessed May 6, 2020
Simonavičius J, Knackstedt C, Brunner-La Rocca HP (2019) Loop diuretics in chronic heart failure: how to manage congestion? Heart Fail Rev 24(1):17–30
Mullens W, Damman K, Harjola VP, Mebazaa A, Brunner-La Rocca HP, Martens P, Testani JM, Tang WHW, Orso F, Rossignol P, Metra M, Filippatos G, Seferovic PM, Ruschitzka F, Coats AJ (2019) The use of diuretics in heart failure with congestion—a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 21(2):137–155
Sterne JAC, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JPT (2016) ROBINS-I: a tool for assessing risk of bias in non-randomized studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Higgins JPT, Green S, eds (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. www.cochrane-handbook.org
Neuberg GW, Miller AB, O'Connor CM, Belkin RN, Carson PE, Cropp AB, Frid DJ, Nye RG, Pressler ML, Wertheimer JH, Packer M, PRAISE Investigators (2002) Prospective randomized amlodipine survival evaluation. Diuretic resistance predicts mortality in patients with advanced heart failure. Am Heart J 144(1):31–38
Domanski M, Norman J, Pitt B, Haigney M, Hanlon S, Peyster E, Studies of Left Ventricular Dysfunction (2003) Diuretic use, progressive heart failure, and death in patients in the studies of left ventricular dysfunction (SOLVD). J Am Coll Cardiol 42(4):705–708
Ahmed A, Husain A, Love TE, Gambassi G, Dell'Italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC (2006) Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J 27(12):1431–1439
Domanski M, Tian X, Haigney M, Pitt B (2006) Diuretic use, progressive heart failure, and death in patients in the DIG study. J Card Fail 12(5):327–332
Mielniczuk LM, Tsang SW, Desai AS, Nohria A, Lewis EF, Fang JC, Baughman KL, Stevenson LW, Givertz MM (2008) The association between high-dose diuretics and clinical stability in ambulatory chronic heart failure patients. J Card Fail 14(5):388–393
Testani JM, Cappola TP, Brensinger CM, Shannon RP, Kimmel SE (2011) Interaction between loop diuretic-associated mortality and blood urea nitrogen concentration in chronic heart failure. J Am Coll Cardiol 58:375–382
Hamaguchi S, Kinugawa S, Tsuchihashi-Makaya M, Goto D, Yamada S, Yokoshiki H, Takeshita A, Tsutsui H, JCARE-CARD Investigators (2012) Loop diuretic use at discharge is associated with adverse outcomes in hospitalized patients with heart failure: a report from the Japanese cardiac registry of heart failure in cardiology (JCARE-CARD). Circ J 76(8):1920–1927
Dini FL, Ghio S, Klersy C, Rossi A, Simioniuc A, Scelsi L, Genta FT, Cicoira M, Tavazzi L, Temporelli PL (2013) Effects on survival of loop diuretic dosing in ambulatory patients with chronic heart failure using a propensity score analysis. Int J Clin Pract 67(7):656–664
Vidula H, Butler J, Subacius H, Fonarow G, Nodari S, Konstam M, Gheorghiade M (2013) Diuretic dose and outcomes among hospitalized heart failure patients: insights from the EVEREST trial. J Am Coll Cardiol 61:E690 Abstract
Damman K, Kjekshus J, Wikstrand J, Cleland JG, Komajda M, Wedel H, Waagstein F, McMurray JJ (2016) Loop diuretics, renal function and clinical outcome in patients with heart failure and reduced ejection fraction. Eur J Heart Fail 18(3):328–336
Miura M, Sugimura K, Sakata Y, Miyata S, Tadaki S, Yamauchi T, Onose T, Tsuji K, Abe R, Oikawa T, Kasahara S, Nochioka K, Takahashi J, Shimokawa H, CHART-2 Investigators (2016) Prognostic impact of loop diuretics in patients with chronic heart failure—effects of addition of renin-angiotensin-aldosterone system inhibitors and β-blockers. Circ J 80(6):1396–1403
Pellicori P, Cleland JG, Zhang J, Kallvikbacka-Bennett A, Urbinati A, Shah P, Kazmi S, Clark AL (2016) Cardiac dysfunction, congestion and loop diuretics: their relationship to prognosis in heart failure. Cardiovasc Drugs Ther 30(6):599–609
Sargento L, Simões AV, Longo S, Lousada N, Reis RP (2017) Furosemide prescription during the dry state is a predictor of long-term survival of stable, optimally medicated patients with systolic heart Failure.J. Cardiovasc Pharmacol Ther 22(3):256–263
Galochkin S, Padaryan S, Babaeva L, Shavarova E, Villevalde S, Kobalava Z (2017) Predictors of six-month mortality after discharge in patients hospitalized with decompensated chronic heart failure. Eur J Heart Fail 19(Suppl. S1):486 Abstract
Costa J, Simone L, Héroguelle V, Nazeyrollas P, Metz D (2017) Furosemide doses and long-term mortality after discharge from heart failure episode: the FACT–HF study. Arch Cardiovasc Dis Suppl 9:39 Abstract
Laszczyńska O, Severo M, Friões F, Lourenço P, Silva S, Bettencourt P, Lunet N, Azevedo A (2017) Prognostic effect of the dose of loop diuretic over 5 years in chronic heart failure. J Card Fail 23(8):589–593
Gonzalez-Loyola F, Abellana R, Verdú-Rotellar JM, Bustamante Rangel A, Clua-Espuny JL, Muñoz MA (2018) Mortality in heart failure with atrial fibrillation: role of digoxin and diuretics. Eur J Clin Investig 48(11):e13014
Kapelios C, Laroche C, Crespo-Leiro MG, Piepoli M, Coats A, Anker SD, Filippatos G, Maggioni A, Seferovic P, Rosano G, Mebazaa A, Lainscak M, Hoes A, Ruschitzka F, Lund LH (2018) High-dose loop diuretics are associated with adverse clinical outcomes in outpatients with chronic heart failure and mid-range and preserved ejection fraction: observations from the ESC heart failure. Eur J Heart Fail 20(Suppl. S1):7 Abstract
Okabe T, Yakushiji T, Kido T, Oyama Y, Igawa W, Ono M, Ebara S, Yamashita K, Yamamoto MH, Saito S, Amemiya K, Isomura N, Ochiai M (2018) The association between high-dose loop diuretic use at discharge and cardiovascular mortality in patients with heart failure. ESC Heart Fail 5(1):87–94
Parén P, Dahlström U, Edner M, Lappas G, Rosengren A, Schaufelberger M (2018) Association of diuretic treatment at hospital discharge in patients with heart failure with all-cause short- and long-term mortality: a propensity score-matched analysis from SwedeHF. Int J Cardiol 257:118–124
Fröhlich H, Rosenfeld N, Täger T, Goode K, Kazmi S, Hole T, Katus HA, Atar D, Cleland JGF, Agewall S, Clark AL, Frankenstein L, Grundtvig M (2019) Epidemiology and long-term outcome in outpatients with chronic heart failure in northwestern Europe. Heart 105(16):1252–1259
Kapelios CJ, Kaldara E, Ntalianis A, Nana E, Pantsios C, Repasos E, Margari Z, Sousonis V, Malliaras K, Nanas JN (2014) Lowering furosemide dose in stable chronic heart failure patients with reduced ejection fraction is not accompanied by decompensation: a randomized study. Int J Cardiol 177(2):690–692
McKie PM, Schirger JA, Benike SL, Harstad LK, Chen HH (2014) The effects of dose reduction of furosemide on glomerular filtration rate in stable systolic heart failure. JACC Heart Fail 2(6):675–677
Francis GS, Siegel RM, Goldsmith SR, Olivari MT, Levine TB, Cohn JN (1985) Acute vasoconstrictor response to intravenous furosemide in patients with chronic congestive heart-failure—activation of the neurohumoral axis. Ann Intern Med 103:1–6
Bayliss J, Norell M, Canepa-Anson R, Sutton G, Poole-Wilson P (1987) Untreated heart-failure—clinical and neuroendocrine effects of introducing diuretics. Br Heart J 57:17–22
Cooper HA, Dries DL, Davis CE, Shen YL, Domanski MJ (1999) Diuretics and risk of arrhythmic death in patients with left ventricular dysfunction. Circulation 100:1311–1315
Damman K, Valente MA, Voors AA, O'Connor CM, van Veldhuisen DJ, Hillege HL (2014) Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J 35(7):455–469
Kapelios CJ, Laroche C, Crespo-Leiro MG, Anker SD, Coats AJS, Díaz-Molina B, Filippatos G, Lainscak M, Maggioni AP, McDonagh T, Mebazaa A, Metra M, Moura B, Mullens W, Piepoli MF, Rosano GMC, Ruschitzka F, Seferovic PM, Lund LH, On behalf of the Heart Failure Long Term Registry Investigators Group (2020) Association between loop diuretic dose changes and outcomes in chronic heart failure: observations from the ESC EORP heart failure long-term registry. Eur J Heart Fail. https://doi.org/10.1002/ejhf.1796
Rohde LE, Rover MM, Figueiredo Neto JA, Danzmann LC, Bertoldi EG, Simões MV, Silvestre OM, Ribeiro ALP, Moura LZ, Beck-da-Silva L, Prado D, Sant'Anna RT, Bridi LH, Zimerman A, Raupp da Rosa P, Biolo A (2019) Short-term diuretic withdrawal in stable outpatients with mild heart failure and no fluid retention receiving optimal therapy: a double-blind, multicentre, randomized trial. Eur Heart J 40(44):3605–3612
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 28 kb).
Rights and permissions
About this article
Cite this article
Kapelios, C.J., Bonou, Μ., Malliaras, K. et al. Association of loop diuretics use and dose with outcomes in outpatients with heart failure: a systematic review and meta-analysis of observational studies involving 96,959 patients. Heart Fail Rev 27, 147–161 (2022). https://doi.org/10.1007/s10741-020-09995-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-020-09995-z