Abstract
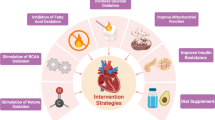
Heart failure (HF) is a clinical syndrome caused by a decline in cardiac systolic or diastolic function, which leaves the heart unable to pump enough blood to meet the normal physiological requirements of the human body. It is a serious disease burden worldwide affecting nearly 23 million patients. The concept that heart failure is “an engine out of fuel” has been generally accepted and metabolic remodeling has been recognized as an important aspect of this condition; it is characterized by defects in energy production and changes in metabolic pathways involved in the regulation of essential cellular functions such as the process of substrate utilization, the tricarboxylic acid cycle, oxidative phosphorylation, and high-energy phosphate metabolism. Advances in second-generation sequencing, proteomics, and metabolomics have made it possible to perform comprehensive tests on genes and metabolites that are crucial in the process of HF, thereby providing a clearer and comprehensive understanding of metabolic remodeling during HF. In recent years, new metabolic changes such as ketone bodies and branched-chain amino acids were demonstrated as alternative substrates in end-stage HF. This systematic review focuses on changes in metabolic substrate utilization during the progression of HF and the underlying regulatory mechanisms. Accordingly, the conventional concepts of metabolic remodeling characteristics are reviewed, and the latest developments, particularly multi-omics studies, are compiled.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Heart failure (HF) is a clinical syndrome caused by a decline in cardiac systolic or diastolic function, which is a serious disease burden worldwide affecting nearly 23 million patients [1, 2]. In recent years, with increasing resuscitation rates of myocardial infarction, the incidence of HF has gradually increased as some patients with myocardial infarction progress into HF [3]. In the last 30 years, great progress has been made in both basic research and clinical treatments for HF, and the risk of sudden death in HF patients has significantly decreased [4, 5]. However, the overall mortality of HF patients remains high; the 5-year survival rate is only 50% [6].
The pathophysiological process of HF contains a concealed phase, compensated stage, and decompensated stage. And it can be defined as HF with preserved ejection fraction (HFpEF) or HF with reduced ejection fraction (HFrEF) in clinical practice [2]. This review mainly focused on HFrEF, because HFpEF was complicated and poorly recognized until recently. In the compensatory stage of HFrEF, the cardiac systolic function is still intact with the occurrence of compensatory cardiac hypertrophy. The decompensated HF phase is HF in the traditional sense, in which systolic function is decreased with distinct clinical presentations of HF. During end-stage HF, cardiac function is severely impaired and cannot maintain basic vital functions [7]. During the entire process of HF progression, there are adaptive or maladaptive alterations in myocardial metabolism, which usually precedes changes in cardiac function [8].
The concept that HF is “an engine out of fuel” has been generally accepted [9] and research studies on its specific mechanisms have become increasingly complex. Metabolic alterations are one of the most significant changes in HF, and mainly manifest as a 30% decrease in ATP concentration and inhibition of ATP transport through the creatine kinase (CK) system. The alterations are accompanied by the switching of main energy substrates from fatty acids (FAs) to glucose [10]. This study systematically reviews the traditional view and recent advances of substrate utilization alterations during HF progression and the underlying molecular mechanisms.
Substrate utilization in the normal heart
The heart is a huge energy-consuming organ that consumes about 6 kg ATP a day to pump out 10 tons of blood throughout the body [7]. The procedures underlying cardiac energy metabolism can be divided into three parts: (1) Substrate utilization. This process includes nutrient intake, degradation (e.g., fatty acid β-oxidation, glycolysis), and the tricarboxylic acid (TCA) cycle. (2) Oxidative phosphorylation. In this process, nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FADH2) produced from the substrate utilization are passed through the electron transport chain (ETC) in the inner mitochondrial membrane to phosphorylate ADP to synthesize the high-energy phosphate compound ATP. (3) ATP transport and utilization through creatine kinase (CK) system [7].
Substrate utilization is the first step of energy metabolism in the heart. Under fasting conditions, more than 70% of the energy required by a normal heart is mainly provided by fatty acid oxidation (FAO), while glucose, lactic acid, and amino acids provide the remaining 30% [11]. Studies have shown that under different conditions, the proportion of FAO in energy metabolism of the heart can range from very small percentage to almost 100%. This shows that the conversion of substrate utilization under normal and disease states plays an important role in energy metabolism in the heart [12].
Glucose metabolic pathways and their regulatory mechanisms
Glucose uptake in cardiomyocytes is mainly regulated by membrane translocation of the glucose transporter 1 (GLUT1) and 4 (GLUT4), followed by phosphorylation into 6-phosphoglucose (G6P) by hexokinase. Adult cardiomyocytes mainly express GLUT4 and hexokinase II, while the fetal heart mainly expresses GLUT1 and hexokinase I [13]. G6P can be stored as glycogen and can also enter glycolysis through the action of phosphofructokinase 1, after which, it is converted into pyruvate. Pyruvate can then undergo anaerobic oxidation in the cytoplasm to synthesize lactic acid and can also enter the mitochondria through pyruvate transporters. Under the action of pyruvate dehydrogenase (PDH), acetyl-CoA is synthesized and enters the TCA cycle [7]. Glucose oxidation is mainly regulated by the PDH complex, which includes PDH, PDH kinase (PDK), and PDH phosphorylase (PDP), all of which undergo multiple regulations. PDK phosphorylation suppresses PDH activity, whereas PDP can dephosphorylate PDH and reverse this suppression effect [14]. A decrease in acetyl-coenzyme A (CoA)/CoA and NADH/NAD+ ratios and pyruvate can suppress PDK, whereas an increase in the calcium (Ca2+)/magnesium (Mg2+) ratio can promote PDP activity, thereby activating PDH [11]. In addition, glucose can enter into the pentose phosphate pathway, which promotes the production of reactive oxygen species (ROS). Therefore, inhibition of this pathway can effectively decrease oxidative stress responses and improve energy metabolism in the failing heart [15] (Fig. 1).
Glucose and fatty acid metabolic pathways. G6P, glucose 6-phosphate; ACC, acetyl-CoA carboxylase; MCD, malonyl-CoA decarboxylase; TCA, tricarboxylic acid; OAA, oxaloacetate; Su-CoA, Succinyl-CoA; α-KG, α-ketoglutarate; UCP, uncoupling proteins; NADH, nicotinamide adenine dinucleotide; FADH2, flavin adenine dinucleotide 2
FA metabolism and the regulatory mechanisms
FAs that are supplied to the myocardium are mainly free fatty acids (FFAs) and FAs released from triacylglycerol (TAG). They enter cells through passive diffusion or carrier-mediated pathways. Carriers that participate in the uptake of FAs include fatty acid translocase (FAT/CD36), the plasma membrane isoform of fatty acid-binding protein (FABPpm), and fatty acid transport protein (FATP1/6). FAT/CD36 is recognized as the major factor that affects FA uptake in cardiomyocytes. In fact, 50–60% of FAs in the heart are transported through FAT/CD36, and knockdown of CD36 in 3T3-L1 adipocytes resulted in a significant decrease in both basal and insulin-stimulated FA uptake. Myocardial contractions promote the translocation of FAT/CD36 between intracellular endosomes and the plasma membrane, which also regulates FA uptake [12] (Fig. 1).
FAs that have entered cells are converted into fatty acyl-CoA catalyzed by long-chain acyl-CoA synthetases. Fatty acyl-CoAs can participate in the synthesis of a variety of intracellular lipid intermediates such as TAG, diacylglycerol, and glycerides in the cytoplasm [12]. These lipid intermediates participate in development of insulin resistance, cardiac insufficiency, and HF. Therefore, in theory, increasing FAO could decrease the production of lipid intermediates, thereby inhibiting their toxic effects on the myocardium, but this has not been consistently shown among studies [16]. Moreover, the catabolism of endogenous TAG also plays an important role in myocardial energy metabolism [17]. When the myocardium is infused with glucose, FAs derived from endogenous TAGs supply 36% of energy to the heart, while this percentage will decrease to 11% when FFA (palmitic acid) was infused to the heart.
An essential metabolic pathway for long-chain fatty acyl-CoAs in the cytoplasm is catalysis by carnitine palmitoyltransferase (CPT-1) on the outer mitochondrial membrane into long-chain acylcarnitines to enter the mitochondria. This step is regulated at multiple levels, of which allosteric inhibition of CPT-1 by malonyl-CoA is the essential mechanism [18]. Acetyl-CoA is converted into malonyl-CoA by acetyl-CoA carboxylase (ACC), which could also be converted to acetyl-CoA by malonyl-CoA decarboxylase (MCD). The balance between these two processes determines the concentration of malonyl-CoA [19]. ACC has two isoforms in the myocardium, ACCα and ACCβ, with the latter predominating. ACC and FAO in the myocardium are negatively correlated and ACC activity is mainly regulated by AMPK. AMPK can phosphorylate ACCα and ACCβ, leading to their inactivation, which decreases malonyl-CoA levels [20]. In addition, it was verified in skeletal muscles that MCD can be phosphorylated by AMPK, thereby increasing its activity and promoting the conversion of malonyl-CoA to acetyl-CoA (this phenomenon is not seen in the myocardium) [21] (Fig. 1).
AMPK plays the role of “energy sensor” as increases in ADP/ATP and creatine (Cr)-PCr ratios can activate AMPK, thereby increasing FAO, glucose uptake, and glycolysis. At the same time, AMPK can inhibit oxidative stress during HF progression [22]. However, mice with heart-specific AMPK deficiency show a dilated cardiomyopathy phenotype, which is accompanied by decreases in myocardial protein phosphorylation and calcium signal dysfunction, but not abnormalities in glucose and FA metabolism [23]. This indicated that AMPK can carry out energy regulation through its complex and synergistic effects.
Long-chain acylcarnitines that have entered the mitochondria penetrate the inner mitochondrial membrane through the action of carnitine: acylcarnitine translocase (CACT), followed by reconversion to acyl-CoA by carnitine palmitoyltransferase-2 (CPT2) to prepare for FAO. FAβ-oxidation involves four types of enzymes: acyl-CoA dehydrogenases, enoyl-CoA hydratase, hydroxyacyl-CoA dehydrogenase, and 3-ketoacyl-CoA thiolase (3-KAT), all of which are negatively regulated by oxidation products. Among these products, the most important is feedback inhibition of 3-KAT by acetyl-CoA [24]. When energy demand is decreased with the decrease of TCA cycle and ETC activity, the accumulation of acetyl-CoA and NADH can suppress FAO enzymes to inhibit β-oxidation. At the same time, the PDH complex in glucose metabolism can promote the synthesis of acetyl-CoA and NADH, and has direct inhibitory effects on β-oxidation [12]. Therefore, FAO is dependent on the energy demand of the heart and availability of glucose substrates (Fig. 1).
The transcriptional regulation of enzymes and transporters associated with FA metabolism is of particular concern. The major transcription factors are peroxisome proliferator-activated receptor (PPARs) family and peroxisome proliferator-activated receptor gamma coactivator 1 (PGC1-α/β). PPARs are members of the ligand-activated nuclear receptor superfamily, and can dimerize with the retinoid X receptor (RXR) to bind to the PPAR response elements (PPRE) on the promoter of target genes to promote the transcription. The ligands of PPARs include FAs and intracellular lipid intermediates [25]. One family member of PPARs, PPARα, is highly expressed in the myocardium and is the main transcriptional regulator of FA metabolism. The target genes of PPARα cover fatty acid uptake (FAT/CD36), storage (DGAT, FABP), mitochondrial fatty acid uptake (CPT1), β-oxidation (medium-chain acyl-CoA dehydrogenase [MCAD], 3-KAT), mitochondrial uncoupling proteins (UCP2/3), and glucose oxidation (PDK4) [12]. Overexpression of PPARα in the heart or treatment with PPARα agonist (GW7647) can significantly promote the expression of these enzymes and thus increase FA utilization; the addition of PPARα ligands can further strengthen this effect [26]. Conversely, PPARα double knockouts were shown to cause a decrease in FA oxidation and increase in glucose oxidation levels [27]. In addition, PPARα is regulated at multiple levels by upstream regulators such as KLF5 [28].
Another member of the PPAR family, PPARβ/δ, was recently shown to participate in the regulation of β-oxidation but does not increase FA uptake. It was found that mice with conditional double knockout of PPARβ/δ in the heart had decreased FAO, which was accompanied by cardiomyopathy due to lipid accumulation in cardiomyocytes. [29]. Conversely, mice overexpressing PPARβ/δ had a high expression of genes associated with FA oxidation, and did not show lipid accumulation and had normal cardiac function. Those mice also presented increased glucose uptake and oxidation [30]. The transcriptional coactivators PGC1-α and PGC-1β are highly expressed in cardiac tissue and participate in mitochondrial biogenesis. Its co-activated nuclear receptor superfamily members include PPARs, the estrogen-related receptor (ERR), and nuclear respiratory factor-1 (Nrf-1) [31]. Pathological (diabetes, fasting) or physiological (physical training) upregulation of PGC-1 can significantly increase mitochondrial biogenesis, FAO, and oxidative phosphorylation, whereas the downregulation of PGC-1 (fetal heart, cardiac hypertrophy, HF) had the opposite effects [31].
Interactions between FA and glucose metabolism (Randle cycle)
As two major energy substrates of heart metabolism, FA and glucose oxidation can maintain relative homeostasis under mutual regulation, a phenomenon known as the Randle cycle [7]. It is also known as the glucose-FA cycle, as this metabolic process involves the competition of glucose and FAs for substrate utilization. FFA acts as ligands to activate PPARα, which upregulates PDK expression, and PDK phosphorylation inactivates PDH to prevent pyruvate from entering the mitochondria, resulting in suppression of glucose oxidation. Simultaneously, acetyl-CoA and NADH produced during FAO can upregulate PDK activity to produce similar effects [32]. At the same time, citrate, the intermediate metabolite of TCA, can inhibit PFK1 and indirectly inhibit hexokinase activity by increasing G6P. Conversely, acetyl-CoA formed from glucose oxidation metabolism can inhibit 3-KAT, while NADH can inhibit hydroxyacyl-CoA dehydrogenase and acyl-CoA dehydrogenase to inhibit FAO. Acetyl-CoA is carboxylated by ACC to become malonyl-CoA, thereby inhibiting CPT-1 and preventing the translocation of acyl-CoA into the mitochondria [33]. The inhibitory effects of FAO on aerobic glucose oxidation far exceed its inhibitory effects on glycolysis. This causes glycolysis to be decoupled from glucose oxidation, resulting in elevated intracellular lactic acid levels and increased cellular acidity. Elimination of these protons requires the accumulation of more Ca2+ and Na+, which consumes large amounts of ATP [33].
Energy metabolism during compensated HF
During the compensated phase of HF, the heart ejection fraction is still preserved, and the hearts mostly present as left ventricular hypertrophy (LVH), although some cases of right ventricular hypertrophy due to pulmonary hypertension [34]. Although cardiac function is preserved at this phase, structural and metabolic remodeling of the ventricle already occurs. These patients can be classified as pressure overload-induced cardiac hypertrophy, volume overload-induced cardiac hypertrophy, and hypertrophy after myocardial infarction, according to etiology. This review mainly examines pressure overload-induced cardiac hypertrophy, which is more commonly seen in clinical practice.
Substrate utilization remodeling
It is perplexing that different types of HF animal model or even the same animal model with a different condition have inconsistent results regarding metabolic phenotype of cardiac failure, which adds to the difficulty in understanding HF metabolic mechanisms. In the spontaneously hypertensive rat model of LVH, FAO was significantly inhibited (60–80% reduction), while glucose oxidation was moderately increased and the glucose/FA oxidation ratio was increased by 4~5-fold. This ensured and met the cardiac energy requirements for beating [35]. In a LVH swine model induced by ascending aortic banding, there were no differences in glucose, lactic acid, and FFA uptake in the LVH group in the resting state between LVH and control group, while glucose uptake and oxidation and anaerobic glycolysis were significantly increased under dobutamine stimulation in the LVH group [36]. Yet, different metabolic characteristics have been observed in recent studies. In a rat model of supra-renal aortic constriction, there was no evidence on switching of substrate utilization from FA to glucose with different degrees of compensatory hypertrophy [37], but the lactic acid levels were increased, an indication that anaerobic glycolysis was increased [38]. A similar phenomenon was observed in Dahl salt-sensitive rats with high-salt diet [39]. Another rat model induced by transverse aorta constriction also showed no changes in exogenous FA metabolism during the LVH, while endogenous TAG oxidation was increased [40].
In recent years, multi-omics study give a chance to comprehensively illustrate the metabolic remodeling in the myocardium regardless of animal model or human-derived myocardium. Through combination of metabolome and transcriptome profiling of pressure-overload mouse model of HF, it was demonstrated that the genes associated with glycolysis and FAO were still preserved, while the tissue metabolite profiles revealed activation of glucose oxidation in the LVH stage [41]. Most recently, Transcriptomics profiling were used to demonstrate that the genes associated with glucose metabolism pathways were significantly upregulated in a LVH stage of PLNR9C/+ dilated cardiomyopathy mouse model, but no significant changes occurred in genes associated with FA metabolism pathways [42]. Based on evidences from more and more large-scale profiling study, it is tempting to assume that FA metabolism is unchanged (or slightly increased) while glucose metabolism (aerobic oxidation and anaerobic glycolysis) is increased during the compensated phase of HF.
Currently, there is still a debate on whether changes in energy metabolism in LVH are adaptive or pathological changes and various metabolic modulating agents/drugs have obtained many inconsistent conclusions in animal models and clinical studies [43, 44]. Recent studies have shown that glucose uptake is increased before LVH, which causes intracellular G6P accumulation and systolic dysfunction. In addition, G6P can promote activation of mechanistic target of rapamycin (mTOR) and an increase in endoplasmic reticulum stress, which increases cardiotoxicity. It has been postulated that increased glucose metabolism is a type of pathological response rather than an adaptive or compensatory response. This hypothesis was also confirmed in transgenic mice study. Decreased glucose utilization due to GLUT1 deficiency does not accelerate HF progression [45], whereas the upregulation of GLUT1 increases glucose uptake and oxidation and decreases FAO, which can decrease myocardial metabolic adaptability and promote systolic dysfunction [46]. Therefore, clinical application of employing fluorodeoxyglucose (FDG)-positron emission tomography (PET) to track glucose uptake has important significance in the early diagnosis of HF. In addition, early intervention to prevent glucose uptake using medication (i.e., propranolol) can prevent pathological metabolic remodeling and preserve cardiac function [47].
Substrate utilization modeling during HF
HF occurs when cardiac energy metabolism is insufficient to maintain the requirements for work, thereby resulting in signs and symptoms of cardiac dysfunction. At the molecular level, there is a significant reduction of ATP and PCr in failing myocardium, which results from the entire process of metabolism involving substrate utilization, oxidative phosphorylation, and the CK system. There have been many studies on substrate utilization in HF but with heterogeneous results. Among these results, there is a consensus that FA metabolism is reduced in human failing heart [48] and most decompensated HF models including volume overload, pressure overload, and pacing in murine or dogs, [9, 49,50,51,52,53] whereas changes in glucose metabolism are still a subject of debate.
Glucose utilization and its regulation
There has been much dispute on the role of glucose metabolism in HF progression. PET scans in clinical studies showed that FA uptake was decreased while glucose uptake and overall metabolic rates were increased in idiopathic dilated cardiomyopathy (IDCM) [54]. There has been a large heterogeneity in the results from animal models. It was found that glucose uptake was decreased in a transverse aortic constriction mouse model [55], while glucose uptake was generally unchanged in a rat model of HF after myocardial infarction [56]. However, glucose uptake was even increased in Dahl salt-sensitive rats [39] and pacing-induced dog HF models [57], which was thought to be associated with switching of glucose transporters from GLUT4 to GLUT1 [13]. Considering that glucose may present different metabolic status in different stages/degree of HF from these controversial studies, it is important to illustrate the dynamic alterations of glucose utilization including glucose uptake and oxidation during progression of HF. As glucose oxidation levels cannot be measured using non-invasive methods, most evidences were from well-defined animal models [10]. In a transverse aortic constriction rat model of HF with continuous monitoring from a normal heart to a failing heart, it was found that glucose oxidation was initially increased, remained unchanged during the compensated HF phase, and decreased at the decompensated phase (end-stage HF) which was accompanied by the decreased expression of glycolysis-associated enzymes (i.e., GAPDH, PGM, PFK) and the PDH complex [58]. It was reported that decreased utilization of glucose at end-stage HF might be associated with downregulation of HIF-1α expression and insulin resistance [39]. In recent years, multi-omics techniques such as transcriptomics, proteomics, and metabolomics have been used to profile comprehensive cardiac energy metabolism characteristics in normal and failing human heart. And the results are consistent that genes associated with glucose uptake and glycolysis are significantly downregulated with the decrease of intermediate metabolites involved in glucose utilization in end-stage human failing heart [59].
There is a tendency to believe that aerobic glucose oxidation is increased during the early stages of HF progression, which increases cardiac efficiency to maintain heart function. As the disease progresses, aerobic oxidation is gradually reduced. And a significant reduction in glucose utilization is observed because of insulin resistance and other factors at end-stage HF. Furthermore, due to mitochondrial dysfunction, accompanied by impaired oxidative phosphorylation, anaerobic glycolysis is increased for energy supply with lactate acid accumulation as “fetal heart metabolic profile”, which further exacerbates energy deficiency in the heart [60, 61].
FA utilization
It is widely accepted that FA utilization shows a continuous decrease during HF progression and end-stage HF [48, 62, 63]. FA uptake shows a consistent decrease in high-salt induced and pacing-induced HF models, which is accompanied by the reduced expression of genes associated with fatty acid transport (e.g., FAT, ACS, CPT1) [7, 58]. This phenomenon was verified by in vivo non-invasive evaluation of HF patients as well as gene expression analysis of failing myocardium from heart transplant [41, 59]. As the same time, fatty acid oxidation also presents a significant decrease at decompensated HF stage, which is the consensus from different animal models and clinical studies.
In recent years, the development and application of multi-omics technologies have enabled us to better understand the metabolic remodeling in the failing heart. An integrated omics-based analysis of a guinea pig model of HF showed that mitochondrial proteins like FAO and anti-oxidant enzymes were significantly decreased, accompanied by a significant decrease in fatty acid oxidation intermediate metabolites such as acyl-CoA [64]. A mouse transverse aortic constriction HF model showed similar effects [53]. An integrated genomics, proteomics, and metabolomics study verified that the expression of enzymes associated with FAO and pyruvate metabolism were significantly downregulated in end-stage HF human ventricular myocardium, which was accompanied by a significant decrease in short-chain acylcarnitines and TCA cycle intermediates [59]. At the same time, due to defects in long-chain fatty acid uptake and oxidation by mitochondria, levels of long-chain acylcarnitines were significantly elevated in the peripheral blood of HF patients [65, 66], which was associated with the malignant prognosis of patients. In addition, plasma long-chain acylcarnitine levels decreased after treatment with left ventricular assist devices (LVADs), suggesting improvements in FA utilization [67].
Regulation of FA supply
It is currently unclear whether FA metabolic remodeling is an adaptive or maladaptive change. It has traditionally been believed that elevated plasma FFA levels in chronic HF patients inhibit glucose uptake, promote insulin resistance, and increase ROS levels to cause cardiac dysfunction, and increase mitochondrial UCP levels to increase ineffective thermogenesis. Reduced FAO levels cause the accumulation of long-chain acyl-CoAs, TAG, and other toxic lipid metabolic intermediates to accelerate HF progression. However, hypolipidemic agents did not show consistent outcomes when used in HF patients. Clinical studies have shown that the use of trimetazidine to decrease blood FFA levels promoted the switching of metabolic substrate from FA to glucose, increased cardiac efficiency, improved cardiac function, and delayed HF progression [68, 69], However, in clinical trials in which acipimox was given to IDCM patients and normal patients, it was found that the rapid downregulation of FFA inhibited cardiac function and reduced cardiac efficiency in HF patients, whereas decreased myocardial oxygen consumption and increased efficiency were observed in healthy hearts. Alternatively, in IDCM, there was a larger decrease in cardiac efficiency, which was accompanied by a greater reduction in FFA uptake and higher β-oxidation levels, indicating that IDCM patients need sufficient FFAs for proper cardiac function [70, 71]. The abovementioned studies show that the remodeling of substrate utilization in HF may involve other complex regulatory mechanisms, and that the rapid correction of substrates should be avoided in clinical practice. The mechanism of metabolic substrate supply influencing HF requires further study.
Regulation of FA oxidation
A large number of studies have verified that the expression and activity of proteins associated with FA uptake and oxidation during the progressive stage of HF are decreased. Martin et al. [72] examined the samples from a heart transplant, and found that CPT2 activity was significantly decreased in HF explanted hearts, while CPT1 activity was unchanged, compared to normal donor hearts. Clinicopathological study showed that the mRNA and protein levels of enzymes involved in the β-oxidation pathway, particularly long-chain fatty acyl CoA dehydrogenase and MCAD, showed significantly decreased in the hearts from HF patients [73]. An end-stage HF dog model induced by rapid ventricular rate also showed downregulation of enzymes associated with FAO and reduced CPT1 activity, and similar conclusions were obtained in various swine and murine HF models [39, 58, 74]. The downregulation of mRNA is usually more significant than changes in protein expression and enzyme activity. This shows that besides the feedback regulation between intermediate metabolites and interactions between glucose and FA metabolism (Randle cycle) as mentioned in previous papers, the regulation of transcriptional levels also plays an important role in this process [12]. Studies on the transcriptional regulation of FA metabolism have mainly focused on a few important transcriptional factors, particularly PPARs and its co-activator PGC-1 [75]. As aforementioned, PPAR, RXR, and PGC-1α form the PPAR/RXR/PGC-1α complex, which participates in the regulation of almost all steps in FA oxidation.
It was widely observed that PPARα expression and activity is decreased during HF progression, accompanied by the downregulation of genes associated with FA oxidation, which was verified by clinicopathology studies of HF patients as well as in vivo and in vitro studies from different swine, dog, and murine HF models [12]. The regulation of cardiac FA metabolism through PPARs has been verified to some extent in animal models, but the effect has not been consistent [25]. In a transverse aortic constriction mouse model, overexpression of PPARα in the early stage of HF maintained energy metabolism and preserved cardiac function [76]. Another study showed that the PPARα agonist GW7647 alleviated post-ischemic contractile dysfunction in neonatal rabbits [26]. Moreover, a recent study has shown that silent information regulator 1 (Sirt 1) can compete with RXR for binding to PPARα to form Sirt1-PPARα heterodimers without transcriptional activity, thereby inhibiting FA metabolism and accelerating HF progression [77]. However, rats with myocardial infarction-induced HF showed increased MCAD activity after treatment with PPARα agonist fenofibrate, but left ventricular function was not improved [78]. Furthermore, in a severe aortic hypertensive rat model, treatment with fenofibrate led to the upregulation of the expression of PPARα-associated lipid metabolism genes, and aggravated left ventricular dysfunction [79]. A similar worsening effect was observed in a porcine tachycardia-induced HF model treated with fenofibrate [80]. These studies indicate that inhibition of FA oxidation gene expression via the downregulation of PPARα may not be the cause for the pathological progression of HF, but could be adaptive compensatory effects.
Research on PPARβ/δ has also garnered interest in recent years. It was found that the expression of β-oxidation genes was decreased in PPARβ/δ-deficient mice, while lipid accumulation was observed in cardiomyocytes at the same time [81]. Overexpression of PPARβ/δ increases glucose utilization and does not cause lipid accumulation or cardiac dysfunction [30]. Treatment of infarct-induced HF rats with the PPARβ/δ agonist GW610742X switched substrate utilization to mainly glucose metabolism without alteration in the expression of genes associated with FA metabolism, and this remodeling did not influence ventricular remodeling and HF progression [12]. A recent study found that myocardial ischemia can induce the production of miR-199a-214 in a pressure-overload mouse HF model, which represses PPARδ expression, thereby downregulating FAO and accelerating the worsening of HF [82]. There have been an increasing number of research studies on PPARβ/δ; drugs against this target will aid in revealing its role in cardiac metabolism [29]. The expression of PGC-1α and its co-activator ERR were found to be downregulated in the failing heart of HF patients, and changes in the PGC-1α targeted FA oxidation genes showed a negative correlation with left ventricular ejection fraction [83]. In a pressure-overload HF rat model, PGC-1β deficiency led to a decrease in glucose metabolism and increased oxidative stress, which accelerated HF progression [84]. These studies show that PGC-1 is an important regulatory factor that participates in FA metabolic remodeling in HF.
Alternative substrate utilization and metabolism
With the rapid development of lipidomics, metabolomics, transcriptomics, and proteomics, studies on HF are no longer limited to glucose and FA metabolism, as more metabolites have been found to participate in the pathophysiological process of HF [85, 86]. Recent lipidomics and mitochondrial proteomics studies confirmed that intermediate metabolites and crucial enzymes in glucose and lipid metabolism showed varying degrees of downregulation in a mouse HF model. However, key enzymes in ketone metabolism pathways, such as 3-hydroxybutyrate dehydrogenase 1 (BDH1), showed significantly upregulated, which was accompanied by significant activation of ketone (such as β-hydroxybutyrate and acetoacetic acid) metabolism. Therefore, it can be hypothesized that ketone bodies may act as alterative substrates in the failing heart when the glucose and lipid metabolism is decreased [62]. In the failing heart, glucose and fatty acid utilization is significantly suppressed due to insulin resistance and other factors; and ketone bodies are small molecular energy substrates that are rapidly metabolized, and can be utilized by the heart, thereby increasing cardiac efficiency [87]. At the same time, lipidomics and metabolomics studies on end-stage human failing heart from heart transplant confirmed that the failing heart utilizes ketone bodies as substrates for alternative metabolism, and levels of ketone bodies (β-hydroxybutyrate and acetoacetic acid) in the peripheral blood of HF patients are significantly higher than those in normal subjects, suggesting a cross-talk between the liver and heart to produce more ketone bodies for myocardial utilization in HF patients [48]. Exhaled ketone body (acetone) concentration and plasma ketone concentration are also demonstrated to be associated with cardiac function and the malignant prognosis in chronic HF patients [88, 89]. These studies confirmed that the end-stage failing heart utilizes large amounts of ketone bodies for oxidation to supply energy, which may provide a new direction for the treatment of this condition [90, 91] (Fig. 2).
Metabolic remodeling of glucose and fatty acid oxidation and alternative substrate utilization from non-failing to end-stage heart failure. β-OHB, β-hydroxybutyrate; AcAc, acetoacetate; AcAc-CoA, acetoacetate-CoA; TCA, tricarboxylic acid; BCAA, branched-chain amino acids; BCKA, branched-chain α-keto acids; BCKD, BCKA dehydrogenase
Recent studies have shown that branched-chain amino acids (BCAAs) similarly play important roles in the pathophysiology of end-stage HF. A combination of gas chromatography-mass spectrometry and liquid chromatography-mass spectrometry (LC-MS)-based metabolomics techniques showed that BCAA metabolism was significantly increased in mouse models of HF that underwent transverse aortic constriction [53]. Sun et al. [63] further performed transcriptome analysis for this HF model to demonstrate that the expression of BCAA catabolic genes in the failing heart was significantly decreased, which was accompanied by the significant accumulation of branched-chain α-keto acids (BCKAs) in the myocardium, compared with un-failing hearts. Transgenic mouse models (PP2Cm-Knock Out) revealed that BCAA catabolic defects promoted pressure overload-induced HF progression, which manifested as BCKA-mediated inhibition of mitochondrial respiration and ROS production in myocardium, all of which promoted mitochondrial dysfunction, resulting in HF. Similar results were also observed in infarct-induced HF murine models [92]. Furthermore, increasing BCAA metabolism in myocardium can effectively improve cardiac function and ameliorate HF progression in transverse aortic constriction-induced mouse model [63], which was confirmed in rats [93]. An exploratory clinical trial on the efficacy of BCAA supplementation in combination with cardiac rehabilitation for HF patients is launched to determine whether BCAA addition could improve cardiac function and exercise capacity for HF patients [94]. Thus, in addition to changes in glucose and FA metabolism during HF, metabolic remodeling of small molecular substrates such as ketone bodies and amino acids also plays important roles in the occurrence and development of HF [95]. Understanding the pathophysiological mechanisms of these metabolic pathways may provide new targets for HF treatment. (Fig. 2).
Mitochondrial fusion/fission and regulation of myocardial energy metabolism
In recent years, the process of mitochondrial dynamics has been gradually recognized, particularly in oncology. The mitochondria are a highly dynamic organelle that shows significant dynamic changes in number, subcellular spatial distribution, and morphological structure in response to external environmental stimuli. Dynamic changes in the morphological structure of mitochondria were first discovered in the 1950s, when it was found that stimulation with CoA or dinitrophenol can stimulate the fusion and fission of mitochondria [96]. Mitochondrial fusion can result in the formation of a continuous reticular structure so that various mitochondrial components are sufficiently mixed to facilitate respiration and ATP synthesis efficiency. On the contrary, mitochondrial fission can cause the formation of smaller individual mitochondria that can facilitate different functions, including eliminating damaged mitochondria through mitochondrial autophagy, promotion of mitochondrial apoptosis, and producing new mitochondria for cell growth, division, and proliferation via biosynthesis process [97]. Mitochondrial fusion and fission are core mechanisms in mitochondrial dynamics, which can affect their total number and subcellular distribution. These are highly matured biological systems that require the participation of a series of proteins. Proteins known to participate in mitochondrial fusion include MFN1, MFN2, and OPA1, whereas proteins that involve fusion include DRP1, FIS1, and MFF. Defects in mitochondrial dynamics can result in various cardiovascular diseases such as ischemia/reperfusion injury [97], HF, and diabetic cardiomyopathy [98]. An example is that imbalanced OPA1 processing, which leads to mitochondrial fragmentation, can cause HF in mice [99]. Key proteins that participate in mitochondrial fusion and fission (such as OPA1 and DRP1) are regulated at various levels including transcription, post-translation modifications (PTMs), and proteasome-dependent protein degradation [98, 100]. One such regulation that is of concern is the regulatory effects of PGC-1 on mitochondrial fusion and fission [101]. In PGC-1α-/PGC-1β-deficient neonatal mice, the levels of mitochondrial fusion proteins (Mfn1, Opa1) were significantly downregulated while levels of fission genes (Drp1, Fis1) were upregulated and mitochondria showed fragmentation, demonstrating energy deficiency and even a lethal cardiomyopathy phenotype [101]. In addition, mitochondrial ROS produced in the failing heart can further induce the PTM of DRP1 and OPA1 to promote mitochondrial fission, aggravating energy deficiency in the heart [102]. Further studies are needed to understand the role of mitochondrial fusion and fission during HF development, and the relationship between mitochondrial dynamics and metabolic substrates selectivity. The regulation of mitochondrial dynamics may provide new targets for HF treatment.
Perspectives
There have been decades of research on HF energy metabolism, and large numbers of metabolic regulation targets have been identified. A limited number of metabolic drugs have been used for HF patients, and small-scale clinical trials are being conducted for some drugs, while a considerable number of these drugs are still in the preclinical research phase. Improvements in transcriptomics, proteomics, and metabolomics will provide a comprehensive understanding of the energy metabolism processes and regulation mechanisms that occur in the normal and failing heart. Most recently, an emerging technology, namely isotope metabolites flux, has led to a clear understanding of the spectrum of energy metabolism in vivo [103, 104]. In addition to tracing metabolites for animal models in vivo or Langendorff-perfused murine hearts ex vivo [105, 106], this technique is currently being applied to illustrate human tumor metabolism in which researchers intravenously inject isotope-labeled metabolic substrates (such as 13C-glucose) into the body before tumor resection surgery. Subsequently, metabolomics tests (using LC-MS/MS) will be performed on the resected tissues immediately after surgical resection of the tumor to analyze the whole metabolic processes of the isotope-labeled substrates [103]. Similarly, the use of the above technique will further provide direct in vivo evidence of energy metabolism remodeling during HF progression by examining human heart tissue derived from biopsy, LVAD implant, or heart transplant.
References
Shen L et al (2017) Declining risk of sudden death in heart failure. N Engl J Med 377(1):41–51
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602
Velazquez EJ et al (2016) Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med 374(16):1511–1520
Filion KB et al (2016) A multicenter observational study of incretin-based drugs and heart failure. N Engl J Med 374(12):1145–1154
Felker GM et al (2017) Effect of natriuretic peptide-guided therapy on hospitalization or cardiovascular mortality in high-risk patients with heart failure and reduced ejection fraction: a randomized clinical trial. JAMA 318(8):713–720
Ho KK et al (1993) The epidemiology of heart failure: the Framingham Study. J Am Coll Cardiol 22(4 Suppl A):6A–13A
Doenst T, Nguyen TD, Abel ED (2013) Cardiac metabolism in heart failure: implications beyond ATP production. Circ Res 113(6):709–724
Byrne NJ et al (2016) Normalization of cardiac substrate utilization and left ventricular hypertrophy precede functional recovery in heart failure regression. Cardiovasc Res 110(2):249–257
Neubauer S (2007) The failing heart—an engine out of fuel. N Engl J Med 356(11):1140–1151
Stanley WC, Recchia FA, Lopaschuk GD (2005) Myocardial substrate metabolism in the normal and failing heart. Physiol Rev 85(3):1093–1129
Fillmore N, Lopaschuk GD (2013) Targeting mitochondrial oxidative metabolism as an approach to treat heart failure. Biochim Biophys Acta 1833(4):857–865
Lopaschuk GD et al (2010) Myocardial fatty acid metabolism in health and disease. Physiol Rev 90(1):207–258
Szablewski L (2017) Glucose transporters in healthy heart and in cardiac disease. Int J Cardiol 230(1):70–75
Liu LX et al (2017) PDK4 inhibits cardiac pyruvate oxidation in late pregnancy. Circ Res 121(12):1370–1378
Vimercati C et al (2014) Beneficial effects of acute inhibition of the oxidative pentose phosphate pathway in the failing heart. Am J Physiol Heart Circ Physiol 306(5):H709–H717
Schulze PC, Drosatos K, Goldberg IJ (2016) Lipid use and misuse by the heart. Circ Res 118(11):1736–1751
Carley AN, Lewandowski ED (2016) Triacylglycerol turnover in the failing heart. Biochim Biophys Acta 1861(10):1492–1499
Jenei ZA et al (2011) Packing of transmembrane domain 2 of carnitine palmitoyltransferase-1A affects oligomerization and malonyl-CoA sensitivity of the mitochondrial outer membrane protein. FASEB J 25(12):4522–4530
Abdurrachim D et al (2015) Good and bad consequences of altered fatty acid metabolism in heart failure: evidence from mouse models. Cardiovasc Res 106(2):194–205
O’Neill HM et al (2014) AMPK phosphorylation of ACC2 is required for skeletal muscle fatty acid oxidation and insulin sensitivity in mice. Diabetologia 57(8):1693–1702
Saha AK et al (2000) Activation of malonyl-CoA decarboxylase in rat skeletal muscle by contraction and the AMP-activated protein kinase activator 5-aminoimidazole-4-carboxamide-1-beta-D-ribofuranoside. J Biol Chem 275(32):24279–24283
Barreto-Torres G et al (2015) The beneficial effects of AMP kinase activation against oxidative stress are associated with prevention of PPARalpha-cyclophilin D interaction in cardiomyocytes. Am J Physiol Heart Circ Physiol 308(7):H749–H758
Sung MM et al (2015) AMPK deficiency in cardiac muscle results in dilated cardiomyopathy in the absence of changes in energy metabolism. Cardiovasc Res 107(2):235–245
Ashrafian H, Frenneaux MP, Opie LH (2007) Metabolic mechanisms in heart failure. Circulation 116(4):434–448
Abushouk AI et al (2017) Peroxisome proliferator-activated receptors as therapeutic targets for heart failure. Biomed Pharmacother 95(1):692–700
Lam VH et al (2015) Activating PPARalpha prevents post-ischemic contractile dysfunction in hypertrophied neonatal hearts. Circ Res 117(1):41–51
Smeets PJ et al (2008) Cardiac hypertrophy is enhanced in PPAR alpha−/− mice in response to chronic pressure overload. Cardiovasc Res 78(1):79–89
Drosatos K et al (2016) Cardiac myocyte KLF5 regulates Ppara expression and cardiac function. Circ Res 118(2):241–253
Palomer X et al (2016) PPARbeta/delta and lipid metabolism in the heart. Biochim Biophys Acta 1861(10):1569–1578
Burkart EM et al (2007) Nuclear receptors PPARbeta/delta and PPARalpha direct distinct metabolic regulatory programs in the mouse heart. J Clin Invest 117(12):3930–3939
Riehle C, Abel ED (2012) PGC-1 proteins and heart failure. Trends Cardiovasc Med 22(4):98–105
Abo AO, Lopaschuk GD (2014) Role of CoA and acetyl-CoA in regulating cardiac fatty acid and glucose oxidation. Biochem Soc Trans 42(4):1043–1051
Guo Z (2015) Pyruvate dehydrogenase, Randle cycle, and skeletal muscle insulin resistance. Proc Natl Acad Sci U S A 112(22):E2854
Gomez-Arroyo J et al (2013) Metabolic gene remodeling and mitochondrial dysfunction in failing right ventricular hypertrophy secondary to pulmonary arterial hypertension. Circ Heart Fail 6(1):136–144
Christe ME, Rodgers RL (1994) Altered glucose and fatty acid oxidation in hearts of the spontaneously hypertensive rat. J Mol Cell Cardiol 26(10):1371–1375
Massie BM et al (1995) Myocardial high-energy phosphate and substrate metabolism in swine with moderate left ventricular hypertrophy. Circulation 91(6):1814–1823
Degens H et al (2006) Cardiac fatty acid metabolism is preserved in the compensated hypertrophic rat heart. Basic Res Cardiol 101(1):17–26
Seymour AM et al (2015) In vivo assessment of cardiac metabolism and function in the abdominal aortic banding model of compensated cardiac hypertrophy. Cardiovasc Res 106(2):249–260
Kato T et al (2010) Analysis of metabolic remodeling in compensated left ventricular hypertrophy and heart failure. Circ Heart Fail 3(3):420–430
O’Donnell JM et al (2008) The absence of endogenous lipid oxidation in early stage heart failure exposes limits in lipid storage and turnover. J Mol Cell Cardiol 44(2):315–322
Lai L et al (2014) Energy metabolic reprogramming in the hypertrophied and early stage failing heart: a multisystems approach. Circ Heart Fail 7(6):1022–1031
Burke MA et al (2016) Molecular profiling of dilated cardiomyopathy that progresses to heart failure. JCI Insight 1(6):e86898
Lionetti V, Stanley WC, Recchia FA (2011) Modulating fatty acid oxidation in heart failure. Cardiovasc Res 90(2):202–209
Heggermont WA et al (2016) Metabolic support for the heart: complementary therapy for heart failure? Eur J Heart Fail 18(12):1420–1429
Pereira RO et al (2014) GLUT1 deficiency in cardiomyocytes does not accelerate the transition from compensated hypertrophy to heart failure. J Mol Cell Cardiol 72(1):95–103
Yan J et al (2009) Increased glucose uptake and oxidation in mouse hearts prevent high fatty acid oxidation but cause cardiac dysfunction in diet-induced obesity. Circulation 119(21):2818–2828
Kundu BK et al (2015) Remodeling of glucose metabolism precedes pressure overload-induced left ventricular hypertrophy: review of a hypothesis. Cardiology 130(4):211–220
Bedi KJ et al (2016) Evidence for Intramyocardial disruption of lipid metabolism and increased myocardial ketone utilization in advanced human heart failure. Circulation 133(8):706–716
Peterzan MA et al (2017) Metabolic remodeling in hypertrophied and failing myocardium: a review. Am J Physiol Heart Circ Physiol 313(3):H597–H616
El AZ et al (1992) Fatty acid oxidation and mechanical performance of volume-overloaded rat hearts. Am J Phys 262(4 Pt 2):H1068–H1074
Pound KM et al (2009) Substrate-enzyme competition attenuates upregulated anaplerotic flux through malic enzyme in hypertrophied rat heart and restores triacylglyceride content: attenuating upregulated anaplerosis in hypertrophy. Circ Res 104(6):805–812
Lei B et al (2004) Paradoxical downregulation of the glucose oxidation pathway despite enhanced flux in severe heart failure. J Mol Cell Cardiol 36(4):567–576
Sansbury BE et al (2014) Metabolomic analysis of pressure-overloaded and infarcted mouse hearts. Circ Heart Fail 7(4):634–642
Davila-Roman VG et al (2002) Altered myocardial fatty acid and glucose metabolism in idiopathic dilated cardiomyopathy. J Am Coll Cardiol 40(2):271–277
Zhabyeyev P et al (2013) Pressure-overload-induced heart failure induces a selective reduction in glucose oxidation at physiological afterload. Cardiovasc Res 97(4):676–685
Amorim PA et al (2010) Myocardial infarction in rats causes partial impairment in insulin response associated with reduced fatty acid oxidation and mitochondrial gene expression. J Thorac Cardiovasc Surg 140(5):1160–1167
Osorio JC et al (2002) Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid X receptor-alpha in pacing-induced heart failure. Circulation 106(5):606–612
Doenst T et al (2010) Decreased rates of substrate oxidation ex vivo predict the onset of heart failure and contractile dysfunction in rats with pressure overload. Cardiovasc Res 86(3):461–470
Gupte AA et al (2014) Mechanical unloading promotes myocardial energy recovery in human heart failure. Circ Cardiovasc Genet 7(3):266–276
Tuunanen H, Ukkonen H, Knuuti J (2008) Myocardial fatty acid metabolism and cardiac performance in heart failure. Curr Cardiol Rep 10(2):142–148
Riehle C, Abel ED (2016) Insulin signaling and heart failure. Circ Res 118(7):1151–1169
Aubert G et al (2016) The failing heart relies on ketone bodies as a fuel. Circulation 133(8):698–705
Sun H et al (2016) Catabolic defect of branched-chain amino acids promotes heart failure. Circulation 133(21):2038–2049
Foster DB et al (2016) Integrated omic analysis of a guinea pig model of heart failure and sudden cardiac death. J Proteome Res 15(9):3009–3028
Hunter WG et al (2016) Metabolomic profiling identifies novel circulating biomarkers of mitochondrial dysfunction differentially elevated in heart failure with preserved versus reduced ejection fraction: evidence for shared metabolic impairments in clinical heart failure. J Am Heart Assoc 5(8):e003190
Ruiz M et al (2017) Circulating acylcarnitine profile in human heart failure: a surrogate of fatty acid metabolic dysregulation in mitochondria and beyond. Am J Physiol Heart Circ Physiol 313(4):H768–H781
Ahmad T et al (2016) Prognostic implications of long-chain acylcarnitines in heart failure and reversibility with mechanical circulatory support. J Am Coll Cardiol 67(3):291–299
Fragasso G et al (2006) A randomized clinical trial of trimetazidine, a partial free fatty acid oxidation inhibitor, in patients with heart failure. J Am Coll Cardiol 48(5):992–998
Fragasso G et al (2011) Effect of partial inhibition of fatty acid oxidation by trimetazidine on whole body energy metabolism in patients with chronic heart failure. Heart 97(18):1495–1500
Tuunanen H et al (2006) Free fatty acid depletion acutely decreases cardiac work and efficiency in cardiomyopathic heart failure. Circulation 114(20):2130–2137
Salerno A et al (2015) Effects of short-term manipulation of serum FFA concentrations on left ventricular energy metabolism and function in patients with heart failure: no association with circulating bio-markers of inflammation. Acta Diabetol 52(4):753–761
Martin MA et al (2000) Myocardial carnitine and carnitine palmitoyltransferase deficiencies in patients with severe heart failure. Biochim Biophys Acta 1502(3):330–336
Fillmore N, Mori J, Lopaschuk GD (2014) Mitochondrial fatty acid oxidation alterations in heart failure, ischaemic heart disease and diabetic cardiomyopathy. Br J Pharmacol 171(8):2080–2090
Wang Y et al (2013) Integrated proteomic and metabolomic analysis reveals the NADH-mediated TCA cycle and energy metabolism disorders based on a new model of chronic progressive heart failure. Mol BioSyst 9(12):3135–3145
Warren JS et al (2017) Metabolic reprogramming via PPARalpha signaling in cardiac hypertrophy and failure: from metabolomics to epigenetics. Am J Physiol Heart Circ Physiol 313(3):H584–H596
Kaimoto S et al (2017) Activation of PPAR-alpha in the early stage of heart failure maintained myocardial function and energetics in pressure-overload heart failure. Am J Physiol Heart Circ Physiol 312(2):H305–H313
Oka S et al (2015) Peroxisome proliferator activated receptor-alpha association with silent information regulator 1 suppresses cardiac fatty acid metabolism in the failing heart. Circ Heart Fail 8(6):1123–1132
Morgan EE et al (2006) Effects of chronic activation of peroxisome proliferator-activated receptor-alpha or high-fat feeding in a rat infarct model of heart failure. Am J Physiol Heart Circ Physiol 290(5):H1899–H1904
Ogata T et al (2004) Myocardial fibrosis and diastolic dysfunction in deoxycorticosterone acetate-salt hypertensive rats is ameliorated by the peroxisome proliferator-activated receptor-alpha activator fenofibrate, partly by suppressing inflammatory responses associated with the nuclear factor-kappa-B pathway. J Am Coll Cardiol 43(8):1481–1488
Brigadeau F et al (2007) The PPARalpha activator fenofibrate slows down the progression of the left ventricular dysfunction in porcine tachycardia-induced cardiomyopathy. J Cardiovasc Pharmacol 49(6):408–415
Cheng L et al (2004) Cardiomyocyte-restricted peroxisome proliferator-activated receptor-delta deletion perturbs myocardial fatty acid oxidation and leads to cardiomyopathy. Nat Med 10(11):1245–1250
El AH et al (2013) The hypoxia-inducible microRNA cluster miR-199a approximately 214 targets myocardial PPARdelta and impairs mitochondrial fatty acid oxidation. Cell Metab 18(3):341–354
Sihag S et al (2009) PGC-1alpha and ERRalpha target gene downregulation is a signature of the failing human heart. J Mol Cell Cardiol 46(2):201–212
Riehle C et al (2011) PGC-1beta deficiency accelerates the transition to heart failure in pressure overload hypertrophy. Circ Res 109(7):783–793
Lopaschuk GD, Ussher JR (2016) Evolving concepts of myocardial energy metabolism: more than just fats and carbohydrates. Circ Res 119(11):1173–1176
Wende AR et al (2017) Metabolic origins of heart failure. JACC Basic Transl Sci 2(3):297–310
Cotter DG, Schugar RC, Crawford PA (2013) Ketone body metabolism and cardiovascular disease. Am J Physiol Heart Circ Physiol 304(8):H1060–H1076
Yokokawa T et al (2016) Exhaled acetone concentration is related to hemodynamic severity in patients with non-ischemic chronic heart failure. Circ J 80(5):1178–1186
Obokata M et al (2017) Association between circulating ketone bodies and worse outcomes in hemodialysis patients. J Am Heart Assoc 6(10):e006885
Taegtmeyer H (2016) Failing heart and starving brain: ketone bodies to the rescue. Circulation 134(4):265–266
Kolwicz SJ, Airhart S, Tian R (2016) Ketones step to the plate: a game changer for metabolic remodeling in heart failure? Circulation 133(8):689–691
Wang W et al (2016) Defective branched chain amino acid catabolism contributes to cardiac dysfunction and remodeling following myocardial infarction. Am J Physiol Heart Circ Physiol 311(5):H1160–H1169
Tanada Y et al (2015) Branched-chain amino acids ameliorate heart failure with cardiac cachexia in rats. Life Sci 137(1):20–27
Takata M et al (2017) An exploratory study on the efficacy and safety of a BCAA preparation used in combination with cardiac rehabilitation for patients with chronic heart failure. BMC Cardiovasc Disord 17(1):205
Huynh K (2016) Heart failure: ketone bodies as fuel in heart failure. Nat Rev Cardiol 13(3):122–123
Biesele JJ, Tobioka M (1956) Mitochondria in living cells: an analysis of movements. J Biophys Biochem Cytol 2(4 Suppl):319–324
Maneechote C et al (2017) Roles of mitochondrial dynamics modulators in cardiac ischaemia/reperfusion injury. J Cell Mol Med 21(11):2643–2653
Nan J et al (2017) TNFR2 stimulation promotes mitochondrial fusion via Stat3- and NF-kB-dependent activation of OPA1 expression. Circ Res 121(4):392–410
Wai T et al (2015) Imbalanced OPA1 processing and mitochondrial fragmentation cause heart failure in mice. Science 350(6265):aad0116
Nan J et al (2017) Molecular regulation of mitochondrial dynamics in cardiac disease. Biochim Biophys Acta 1864(7):1260–1273
Martin OJ et al (2014) A role for peroxisome proliferator-activated receptor gamma coactivator-1 in the control of mitochondrial dynamics during postnatal cardiac growth. Circ Res 114(4):626–636
Tsushima K et al (2018) Mitochondrial reactive oxygen species in Lipotoxic hearts induce post-translational modifications of AKAP121, DRP1, and OPA1 that promote mitochondrial fission. Circ Res 122(1):58–73
Hensley CT et al (2016) Metabolic heterogeneity in human lung tumors. Cell 164(4):681–694
Faubert B et al (2017) Lactate metabolism in human lung tumors. Cell 171(2):358–371.e9
Li Q et al (2015) Multiple mass isotopomer tracing of acetyl-CoA metabolism in Langendorff-perfused rat hearts: channeling of acetyl-CoA from pyruvate dehydrogenase to carnitine acetyltransferase. J Biol Chem 290(13):8121–8132
Nadtochiy SM et al (2015) Metabolomic profiling of the heart during acute ischemic preconditioning reveals a role for SIRT1 in rapid cardioprotective metabolic adaptation. J Mol Cell Cardiol 88(1):64–72
Funding
This study was funded by CAMS Innovation Fund for Medical Sciences (2016-I2M-1-015) and the National Natural Science Foundation of China (81670376).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Chen, L., Song, J. & Hu, S. Metabolic remodeling of substrate utilization during heart failure progression. Heart Fail Rev 24, 143–154 (2019). https://doi.org/10.1007/s10741-018-9713-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-018-9713-0