Abstract
Several studies suggest that psychological factors are associated with negative outcomes and in particular higher mortality rates among heart failure (HF) patients. We aimed to evaluate the effect sizes of depression and anxiety on all-cause mortality in HF patients. We conducted a systematic review according to the PRISMA methodology. We searched for studies on depression or anxiety effects on all-cause mortality among HF patients published up to June 2015. A number of 26 and 6 articles met inclusion criteria for depression (total 80,627 patients) and anxiety (total 17,214 patients), respectively. The effect estimates were pooled using random-effect meta-analysis. Depression has significant and moderately heterogeneous effect on all-cause mortality (HR = 1.57; 95 %CI 1.30–1.89, p < 0.001); adjustment for confounders led to a similar effect estimate (HR = 1.40; 95 %CI 1.22–1.60; p < 0.001). Larger studies and higher study prevalence of depression were associated with smaller effect size. The effect of anxiety on mortality outcome was small and not conclusive given the low number of studies (n = 6) (HR = 1.02; 95 % CI 1.00–1.04, p < 0.05). This systematic review and meta-analysis suggests that depression is an important and independent predictor of all-cause mortality among HF patients, while anxiety does not appear to have a strong effect. Further research is recommended toward the detection and treatment of depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is defined as a clinical syndrome in which patients have typical symptoms such as breathlessness, ankle swelling, and fatigue and signs such as elevated jugular venous pressure, pulmonary crackles, and displaced apex beat, resulting from an abnormality of cardiac structure or function [1]. Approximately 1–2 % of the adult population in developed countries has HF, with the prevalence rising to ≥10 % among persons 70 years of age or older [2]. HF is one of the most common causes of hospital readmission and mortality.
Psychological factors such as depression or anxiety are often reported with high prevalence and strong association with negative outcomes in patients with cardiovascular disease [3]. Many studies have reported high rates of depression among HF patients. A prior systematic review and meta-analysis published by Rutledge in 2006 [4] reported an overall aggregated depression prevalence rate of 21.6 % among HF patients, while individual study prevalence estimates ranged from 9 to 60 %. Moreover, in 2005 Konstam [5] reported that approximately 40 % of HF patients may suffer from major anxiety, and overall anxiety levels are 60 % higher than levels seen in the healthy population.
Depression has been linked to increased risk of negative outcomes, such as rehospitalization and mortality among HF patients. According to a previous meta-analysis, the aggregated risk estimate derived from 8 studies suggested a >2-fold risk of death and secondary events for HF patients with heightened depressive symptoms or a depressive disorder [4]. A similar analysis was also published by Fan [6] in 2014 on 9 prospective studies, who reported a pooled Hazard Ratio of 1.51 for patients with depression compared to patients without depression. In both cases the result was strongly heterogeneous but no further analysis, such as meta-regression, was performed to examine the sources of this heterogeneity. On the other hand, there is, to the best of our knowledge, no meta-analysis published about the prevalence of anxiety among HF patients and the effect of anxiety on mortality outcome. Even though anxiety is usually correlated with depression, it has not extensively been studied among patients with HF.
Our aim is to provide an updated systematic review of prospective or retrospective studies and a meta-analysis of the effect of depression and the effect of anxiety on mortality among HF patients. To reach this objective, we searched extensively for available studies investigating the impact of depression and anxiety on mortality of HF patients. Within these studies, we identified also the reported prevalence of depression or anxiety among HF patients.
Methods
Search strategy and selection criteria
This systematic review and meta-analysis were conducted according to the guidelines introduced in the Preferred Reporting Items for Systematic reviews and Meta-analysis (the PRISMA Statement) [7]. The 27 checklist items of the PRISMA methodology followed are given in Appendix 1. Three electronic databases (MEDLINE, BIOSIS and EMBASE) were searched for studies that investigated the relationship between depression or anxiety and mortality among HF patients. No publication time restriction was applied. All papers written in English and published before the 25th of June 2015 were included. Selected journals as well as the references of full text papers were also hand-searched, when necessary, in order to identify studies that meet the inclusion criteria.
The database search string was created according to the PICO model (P population/patient, I intervention/indicator, C comparator/control, O outcome). For the “P” in PICO the “HEART FAILURE” keyword was included. For the “I”, the following keywords: “DEPRESS? OR STRESS OR ANXIETY OR PSYCHOLOG?”. For the “C”, no particular terms were used in our case. For “O”, we used the following keywords: “MORTALITY OR DEATH”. The complete query as used for the databases search is given in Appendix 2.
Study selection
In our analysis, several inclusion and exclusion criteria were defined. All studies that met those criteria were included. The inclusion criteria were articles presenting studies focusing on the association between depression or anxiety and mortality in a HF adult population. All mortality outcomes such as all-cause or cardiac-related mortality were included and studies focusing on inpatient, outpatient or both care settings were taken into account. On the other hand, publications analyzing data that had already been used before for the same purpose, studies introducing no quantitative assessment of the impact of depression or anxiety on the outcome or analyzing the use of antidepressants as primary focus were excluded from our analysis.
Review process and data collection
All titles and abstracts of studies identified by the electronic and hand search were screened by the reviewer (IS) to identify those meeting the inclusion/exclusion criteria. Then, all the selected full texts were screened independently by two reviewers (IS, GJdV) to identify which articles should be included in the systematic review. Any disagreement between the reviewers was resolved by a third reviewer (SP). For each of the selected articles, the reviewers extracted data about author, year of publication, follow-up period, outcome variable, location, study design, study population (size/type), prevalence of depression or anxiety, assessment method of the psychological parameter, other parameters, statistical method and results.
Mendeley 1.13.8 software was used for organizing and managing of the articles.
Data analysis
All studies were categorized according to the psychological factor investigated (depression or anxiety). Information was extracted according to whether the analysis was adjusted for confounders such as age, gender, and clinical severity. For both groups the association between depression or anxiety and mortality was reported by collecting information of the hazard ratios/odds ratios, 95 %CI and/or p values.
Random-effects meta-analysis was applied to combine the results. We decided to pool not only the adjusted effect but also the unadjusted effects in order to avoid the bias of the different adjustments. For the few cases where Odds Ratios were reported, they were converted [8] into Hazard Ratios in order to be comparable with the other Hazard Ratios. In studies where results were presented for several periods of follow-up we selected the longest follow-up period to avoid bias of including multiple results on the same patient data.
Studies collected in our analysis were different with respect to patient population, locations and depression or anxiety assessment methods. The random-effects method allows for heterogeneity by assuming that the effects being estimated in the different studies are not identical, but follow a normal distribution. Heterogeneity across the studies was quantified by the I 2 statistic [9]. The I 2 statistic summarizes the fraction of the variation across studies due to heterogeneity relative to chance. Random-effect meta-regression was used in an attempt to explain between-study heterogeneity and identify possible sources of bias. Meta-regression is a method to quantify the association between the estimated effect of depression and different study characteristics.
Meta analyses were presented in the form of forest plots created with the meta for package for R statistics version 3.0.3 (The R Foundation for Statistical Computing).
Results
Search result
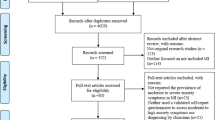
A total of 906 potentially relevant articles was identified from the electronic search and five from the hand search. After removing the duplicates and reviewing the titles and abstracts, we ended up with 62 articles for a full text review. From these, 35 more articles were excluded, leaving 27 articles for the systematic review (Fig. 1).
Characteristics of the selected studies
Depression and mortality
Among the identified studies, 26 reported on the effect of depression. The prevalence of depression varied from 10 to 79 % in the identified literature studies (Table 1). The unadjusted effect of depression is presented in Table 1a, while the effect of depression after adjusting for several confounders in Table 1b. The most common confounders, used in more than 10 studies, were age, gender, NYHA class and (left ventricular) ejection fraction.
There were various techniques used among the studies to assess depression levels. We included all studies assessing for clinically significant depression. The most common scale used was the Beck Depression Inventory (BDI) [10], followed by the Patient Health Questionnaire (PHQ) [11].
The pooled hazard ratio for the unadjusted effect of depression on mortality was strongly significant across 15 studies (HR = 1.57; 95 %CI 1.30–1.89; p < 0.001). The pooled estimation was strongly heterogeneous as reflected by the I 2 statistic (I 2 = 94 %, heterogeneity p < 0.001). The pooled adjusted Hazard Ratio was also significant (HR = 1.40; 95 %CI 1.22–1.60; p < 0.001) and again heterogeneous (heterogeneity p < 0.001; I 2 = 97 %; Fig. 2).
A random-effect meta-regression was performed to understand the sources of the higher than 90 % observed heterogeneity between the studies. The potential study-level covariates analyzed were the study characteristics introduced in Table 1. There was no association found between heterogeneity and the depression assessment method, the adjusted or univariate analysis, the location where the study was conducted, the inpatient or outpatient predictive period, the year of the study, the type of the study and the follow-up period. On the other hand, significant heterogeneity was associated with the total population size (smaller effect in larger studies p < 0.01) and the prevalence of the depression in the study (smaller effect for prevalence >29 %; p < 0.01; Table 2).
Anxiety and mortality
Only six studies analyzing the effect of anxiety on mortality among HF patients were identified with a prevalence of anxiety varying from 9 to 53 % (Table 3). Table 3a shows the unadjusted effects reported in the studies, and Table 3b the reported effects on mortality after adjusting for a group of confounders. Age, NYHA class and (left ventricular) ejection fraction were the most common confounders in the identified studies.
There was no evidence found for anxiety as an independent predictor of mortality. The pooled hazard ratio for the unadjusted effect of anxiety on mortality, which was based on 2 studies, was 1.02 (95 % CI 1.00–1.04; p = 0.24, heterogeneity p = 0.38; I 2 = 0 %). The pooled hazard ratio for the adjusted effect of anxiety on mortality could be based on 5 studies and was identical (HR = 1.02; 95 % CI 1.00–1.04; p = 0.09) and reasonably homogenous (heterogeneity p = 0.97; I 2 = 0 %, Fig. 3).
Discussion
This systematic review was conducted according to the PRISMA guidelines to assess the evidence on the effect of depression (26 studies) and anxiety (6 studies) on all-cause mortality outcome among heart failure (HF) patients. <Key results: 1.6 for depression but very heterogeneous across studies; no effect for anxiety>.
In contrast to other reviews, our study was not limited on follow-up duration or only in prospective studies reporting adjusted effects of the two parameters. We reviewed all studies published quantifying the effect of depression or anxiety.
The prevalence of depression varied among the 26 different studies with an average of approximately 29 % ranging from 10 to 79 %. The meta-analysis showed that the unadjusted risk of death among HF patients facing depression was 1.57 times higher than the risk among HF patients without depression and the pooled estimate of the adjusted Hazard Ratio was 1.40. In both univariate and adjusted analysis, strong heterogeneity among the studies was found. Our findings are more conservative than previous reviews published [4, 6]. Rutledge et al. reported a 2.10 higher adjusted risk of mortality and secondary events based on 8 studies, and Fun et al. reported a pooled adjusted Hazard Ratio of 1.51 based on 9 studies, both with substantial heterogeneity. From our attempt to explain heterogeneity, we found that the effect of depression is weaker in larger studies; this suggests publication bias: small studies were published if they found relatively large effect estimates, while small studies with modest effect estimates were not. The weaker effect in studies with higher prevalence of depression may relate to the use of different cut-offs on an underlying, latent, scale for depression. If a more liberal cut-off was used, those labeled as depressed actually were milder than with a more strict definition of depression.
Our results for anxiety do not have the same weight as the results with respect to depression since anxiety was less studied in the literature. Anxiety had a similar prevalence to depression among the six identified studies (average 29 %, range 9–45 %), but patients with anxiety had no increased risk of death compared to those without anxiety. However, since anxiety is usually correlated with other factors such as depression, further research of anxiety as a covariate to other factors is recommended.
One limitation of our study is related to the variation in follow-up times. Follow-up times varied from 30 days to a number of years; furthermore, there were studies covering different follow-up periods but in these cases we always selected the longest follow-up. Further analysis such as subgroup analysis would be recommended to investigate the effect variation in different follow-up periods; however, limited information in some of the literature publications is restrictive toward this direction.
Moreover, we focused only on mortality. Nevertheless, there is evidence that depression and anxiety are also associated with other adverse events such as readmission. Further investigation is needed also toward this direction.
One limitation of the meta-regression is that even though we tried to cover a broad selection of study-level covariates, there are more that might also be related to the heterogeneity. Further research on different factors’ interactions would be recommended.
The “gold standard” test of causality of a putative risk factor is a randomized clinical trial. Such a trial minimizes concerns about confounders [12–14]. To the best of our knowledge, there is no randomized clinical trial conducted for depression among a HF population. Based on our findings, we strongly recommend such a trial in order to evaluate the causality of depression.
Finally, according to our findings from the meta-regression, depression should not be underestimated in clinical practice within HF population groups where prevalence is low. Furthermore, based on our overall findings on the effect of depression, we recommend further research on the recognition and management of depression in clinical practice which might improve patient outcomes. Further analysis such as subgroup analysis and interventional studies is required for stronger evidence toward this direction.
References
Mcmurray JJV, Adamopoulos S, Anker SD et al (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur J Heart Fail 14:803–869. doi:10.1093/eurjhf/hfs105
Mosterd A, Hoes AW (2007) Clinical epidemiology of heart failure. Heart 93:1137–1146. doi:10.1136/hrt.2003.025270
Ladwig K-H, Lederbogen F, Albus C et al (2014) Position paper on the importance of psychosocial factors in cardiology: update 2013. Ger Med Sci. doi:10.3205/000194
Rutledge T, Reis VA, Linke SE et al (2006) Depression in heart failure. A meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 48:1527–1537. doi:10.1016/j.jacc.2006.06.055
Konstam V, Moser DK, De Jong MJ (2005) Depression and anxiety in heart failure. J Card Fail 11:455–463. doi:10.1016/j.cardfail.2005.03.006
Fan H, Yu W, Zhang Q et al (2014) Depression after heart failure and risk of cardiovascular and all-cause mortality: a meta-analysis. Prev Med (Baltim) 63:36–42. doi:10.1016/j.ypmed.2014.03.007
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. doi:10.1371/journal.pmed.1000100
Higgins JPT, Altman DG, Gøtzsche PC, et al. (2011) The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 343:d5928. doi:10.1136/bmj.d5928
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ Br Med J 327:557–560. doi:10.1136/bmj.327.7414.557
Zich JM, Attkisson CC, Greenfield TK (1990) Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med 20:259–277
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613. doi:10.1046/j.1525-1497.2001.016009606.x
Ioannidis JPA (2005) Contradicted and initially stronger effects in highly cited clinical research. JAMA J Am Med Assoc 294:218–228. doi:10.1001/jama.294.2.218
Evans I, Thornton H, Chalmers I (2008) Testing treatments: better research for better healthcare. Chin J Evid-Based Med. doi:10.1136/bmj.332.7556.1516
Mushlin AI, Ghomrawi H (2010) Health care reform and the need for comparative-effectiveness research. N Engl J Med 362:e6. doi:10.1056/NEJMp0912651
Adams J, Kuchibhatla M, Christopher EJ et al (2012) Association of depression and survival in patients with chronic heart failure over 12 years. Psychosomatics 53:339–346. doi:10.1016/j.psym.2011.12.002
Albert NM, Fonarow GC, Abraham WT et al (2009) Depression and clinical outcomes in heart failure: an OPTIMIZE-HF analysis. Am J Med 122:366–373. doi:10.1016/j.amjmed.2008.09.046
Diez-Quevedo C, Lupón J, González B et al (2013) Depression, antidepressants, and long-term mortality in heart failure. Int J Cardiol 167:1217–1225. doi:10.1016/j.ijcard.2012.03.143
Faller H, Störk S, Schowalter M et al (2007) Depression and survival in chronic heart failure: does gender play a role? Eur J Heart Fail 9:1018–1023. doi:10.1016/j.ejheart.2007.06.011
Faller H, Störk S, Gelbrich G et al (2015) Depressive symptoms in heart failure: independent prognostic factor or marker of functional status? J Psychosom Res. doi:10.1016/j.jpsychores.2015.02.015
Farisa R, Purcell H, Henein MY, Coats AJS (2002) Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 4:541–551. doi:10.1016/S1388-9842(02)00101-0
Friedmann E, Thomas SA, Liu F et al (2006) Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J 152:1–8. doi:10.1016/j.ahj.2006.05.009
Jiang W, Alexander J, Christopher E et al (2001) Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 161:1849–1856. doi:10.1001/archinte.161.15.1849
Jiang W, Kuchibhatla M, Clary GL et al (2007) Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J 154:102–108. doi:10.1016/j.ahj.2007.03.043
Jünger J, Schellberg D, Müller-Tasch T et al (2005) Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 7:261–267. doi:10.1016/j.ejheart.2004.05.011
Kato N, Kinugawa K, Yao A et al (2009) Relationship of depressive symptoms with hospitalization and death in Japanese patients with heart failure. J Card Fail 15:912–919. doi:10.1016/j.cardfail.2009.06.442
Lesman-Leegte I, Van Veldhuisen DJ, Hillege HL et al (2009) Depressive symptoms and outcomes in patients with heart failure: data from the COACH study. Eur J Heart Fail 11:1202–1207. doi:10.1093/eurjhf/hfp155
Moraska AR, Chamberlain AM, Shah ND et al (2013) Depression, healthcare utilization, and death in heart failure a community study. Circ Heart Fail 6:387–394. doi:10.1161/CIRCHEARTFAILURE.112.000118
O’Connor CM, Abraham WT, Albert NM et al (2008) Predictors of mortality after discharge in patients hospitalized with heart failure: an analysis from the organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE-HF). Am Heart J 156:662–673. doi:10.1016/j.ahj.2008.04.030
Sullivan MD, Levy WC, Crane BA et al (2004) Usefulness of depression to predict time to combined end point of transplant or death for outpatients with advanced heart failure. Am J Cardiol 94:1577–1580. doi:10.1016/j.amjcard.2004.08.046
Alhurani AS, Dekker RL, Abed MA et al (2014) The association of co-morbid symptoms of depression and anxiety with all-cause mortality and cardiac rehospitalization in patients with heart failure. Psychosomatics 56:371–380. doi:10.1016/j.psym.2014.05.022
Coyne JC, Rohrbaugh MJ, Shoham V et al (2001) Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol 88:526–529. doi:10.1016/S0002-9149(01)01731-3
Cully JA, Johnson M, Moffett ML et al (2009) Depression and anxiety in ambulatory patients with heart failure. Psychosomatics 50:592–598. doi:10.1176/appi.psy.50.6.592
Konstam V, Salem D, Pouleur H et al (1996) Baseline quality of life as a predictor of mortality and hospitalization in 5025 patients with congestive heart failure. Am J Cardiol 78:890–895. doi:10.1016/S0002-9149(96)00463-8
Murberg TA, Bru E (2001) Social relationships and mortality in patients with congestive heart failure. J Psychosom Res 51:521–527
Rollman BL, Herbeck Belnap B, Mazumdar S et al (2012) A positive 2-item patient health questionnaire depression screen among hospitalized heart failure patients is associated with elevated 12-month mortality. J Card Fail 18:238–245. doi:10.1016/j.cardfail.2011.11.002
Sherwood A, Blumenthal JA, Trivedi R et al (2007) Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med 167:367–373. doi:10.1001/archinte.167.4.367
Smith ORF, Kupper N, Schiffer AA, Denollet J (2012) Somatic depression predicts mortality in chronic heart failure: can this be explained by covarying symptoms of fatigue? Psychosom Med 74:459–463. doi:10.1097/PSY.0b013e31824ef2f4
Van Den Broek KC, Defilippi CR, Christenson RH et al (2011) Predictive value of depressive symptoms and B-type natriuretic peptide for new-onset heart failure and mortality. Am J Cardiol 107:723–729. doi:10.1016/j.amjcard.2010.10.055
Volz A, Schmid J-P, Zwahlen M et al (2011) Predictors of readmission and health related quality of life in patients with chronic heart failure: a comparison of different psychosocial aspects. J Behav Med 34:13–22. doi:10.1007/s10865-010-9282-8
Zuluaga MC, Guallar-Castillón P, Rodríguez-Pascual C et al (2010) Mechanisms of the association between depressive symptoms and long-term mortality in heart failure. Am Heart J 159:231–237. doi:10.1016/j.ahj.2009.11.011
Jiang W, Kuchibhatla M, Cuffe MS et al (2004) Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation 110:3452–3456. doi:10.1161/01.CIR.0000148138.25157.F9
Acknowledgments
The authors would like to thank John Dielis from E-Science & Information Management Department, Philips, Eindhoven, for contributing in querying the databases.
Funding
IS, JJGV and SCP are employed by Philips Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
EWS has no conflict of interest to declare.
Appendices
Appendices
Appendix 1
See Table 4.
Appendix 2
Database search query
S (HEART(W)FAILURE)/TI AND ((DEPRESS? OR STRESS? OR ANXIETY OR PSYCHOLOG?)(S)(MORTALITY OR DEATH))/TI,AB.
Rights and permissions
About this article
Cite this article
Sokoreli, I., de Vries, J.J.G., Pauws, S.C. et al. Depression and anxiety as predictors of mortality among heart failure patients: systematic review and meta-analysis. Heart Fail Rev 21, 49–63 (2016). https://doi.org/10.1007/s10741-015-9517-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-015-9517-4