Abstract
Heart failure remains a major cause of death and disability, requiring rapid development of new therapies. Bone marrow-derived mesenchymal stem cell (MSC)-based therapy is an emerging approach for the treatment of both acute and chronic heart failure. Following successful experimental studies in a range of models, more than 40 clinical trials of MSC-based therapy for heart failure have now been registered, and the results of completed clinical trials so far have shown feasibility and safety of this approach with therapeutic potential suggested (though preliminarily). However, there appear to be several critical issues to be solved before this treatment could become a widespread standard therapy for heart failure. In this review, we comprehensively and systemically summarize a total of 73 preclinical studies and 11 clinical trial reports published to date. By analyzing the data in these reports, (1) improvement in the cell delivery method to the heart in order to enhance donor cell engraftment, (2) elucidation of mechanisms underpinning the therapeutic effects of the treatment differentiation and/or treatment secretion, and (3) validation of the utility of allogeneic MSCs which could enhance the efficacy and expand the application/indication of this therapeutic approach are highlighted as future perspectives. These important respects are further discussed in this review article with referencing latest scientific and clinical information.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of heart failure
Heart failure remains a major cause of death and disability, and the number of patients is predicted to sour along with the increase in the aged population [1]. Cardiac function of these patients is increasingly compromised with the progression of adverse ventricular remodeling, and many eventually develop fatal end-stage heart failure [2–4]. Current medical therapies have limited efficacy for heart failure, and heart transplantation is the only radical treatment but is problematic because of donor shortage. Therefore, the development of new therapies for the treatment of heart failure is a high priority.
Mesenchymal stem cell-based therapy
Stem cell therapy is a promising new approach for the treatment of heart failure. Many types of stem/progenitor cells have been studied as donor for this treatment, and several types of stem cells have been injected into patients with acute myocardial infarction (MI) or chronic heart failure. Based on the preclinical and clinical data available to date, bone marrow-derived mesenchymal stem (stromal) cells (MSCs) are among the most promising cell types because of following reasons. First, good medical practice–compliant protocols to isolate/expand a sufficient number of MSCs from bone marrow, which are feasible in the treatment of heart failure, have been established [5]. Second, since the first clinical trial in 1995 [6], more than 2,000 patients have been administered with allogeneic or autologous MSCs for the treatment of various diseases, including graft-versus-host disease (GVHD), hematologic malignancies, cardiovascular diseases, and neurologic diseases [7]. Results of these trials have collectively suggested safety and feasibility of MSC injection. Third, there are extensive preclinical evidence that MSC transplantation is safe and effective to treat acute MI and chronic heart failure using a variety of models (see “Preclinical studies” section) [8, 9]. Although cardiomyogenic differentiation of MSCs may be insignificant in vivo, grafted MSCs are able to secrete a range of factors, which help recovery of failing myocardium undergoing adverse remodeling (“paracrine effect”; see “Mechanism of MSC-based therapy” section). Fourth, over 40 clinical trials of MSC transplantation for treating heart failure have been registered, and results of completed clinical trials so far have suggested not only safety but also therapeutic effect of this approach (see “Clinical trials” section). Fifth, unlike other donor cell types, MSCs may be useful as allogeneic donor (see “Use of allogeneic MSCs” section) [10].
Definition of MSC
Friedenstein and colleagues originally identified MSCs as (1) adherent cells, (2) fibroblast-like cells, and (3) colony-forming unit-fibroblasts with a high replicative capacity [11–13]. Pittenger et al. [14] reported that MSCs postulate potential toward multiple mesenchymal lineages. Following the discovery of MSCs in bone marrow [13], MSCs have been isolated from a range of tissues. Among these, this review focuses on bone marrow-derived MSCs, which have been most extensively studied in preclinical and clinical research for targeting not only heart failure but also many other organ diseases, with providing promising results. Although there remains insufficiency of consensus on the definition of MSCs, the Mesenchymal and Tissue Stem Cell Committee of the International Society for Cellular Therapy proposed a minimal criteria to define human MSCs as cells that (1) possess plastic adherent ability, (2) express CD105, CD73, and CD90, (3) do not express CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA-DR, and (4) differentiate to osteoblasts, adipocytes, and chondroblasts [15].
Aim of this review article
There is convincing preclinical evidence supporting the value of MSCs as a source for stem cell therapy for the treatment of heart failure. This has encouraged initiation of many clinical studies, which has provided promising results so far. However, there appear to be several critical issues to be solved for this treatment to become a widespread standard therapy for heart disease. This review summarizes previous and latest preclinical and clinical information and discusses solution of unsolved issues for future success of MSC-based therapy for heart disease.
Preclinical studies
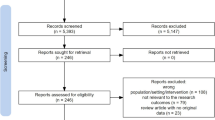
There are a large number of preclinical studies that investigated MSC-based therapy for heart diseases, among which we have selected those clearly describing the therapeutic effect in terms of cardiac function improvement (Table 1). There are 73 reports, of which 10, 41, 1, 17, 2, and 2 reports used heart disease models in mouse, rat, rabbit, swine, sheep, and canine, respectively. Approximately 56 % (41/73) of the reports are rat studies; 29 % (21/73) used large animal models. In these 21 large animal studies, a total of 23 treatment groups using a range of protocols were investigated for the effects (some reports studied multiple treatment groups). The majority (17 out of 23) of the study groups used acute MI models, while 6 employed chronic heart failure models. As a route for cell delivery, intramyocardial (IM) injection of MSC suspension was used in 16 treatment groups and intravenous (IV) injection of that was used in 2 groups. In addition, 6, 15, and 1 treatment groups used autologous, allogeneic, and xenogenic transplantation models, respectively (data missing in one report). In these treatment groups collectively, 17 groups showed improvement in cardiac function, while six groups showed negative results. Ratios of groups showing negative effects were nearly similar between acute MI models (4/17 = 24 %) and chronic heart failure models (2/6 = 33 %). These preclinical studies imply several important considerations for the future development of MSC-based therapy.
Firstly, it is likely that MSC-based therapy using either syngeneic, allogeneic, or xenogeneic MSCs is safe. There are no reports providing evidence of tumor formation in the heart or other organs, or arrhythmia occurrence following MSC transplantation in large animal or rat models. Although there are a few reports suggesting tumor or bone formation after MSC transplantation in mouse [16, 17], these adverse events might have occurred due to chromosomal instability specific to mice [18, 19]. Anyway, these possible complications should continue to be carefully monitored in further preclinical research and clinical trials.
Secondly, these preclinical studies suggest that it is important to improve the cell delivery route. The majority of previous studies used IM, intracoronary (IC), or IV injection (Table 1). However, analyses of donor cell survival in the heart showed that all of these cell delivery methods are associated with disappointingly poor retention and survival of donor cells [20]. Refinement of these methods, or development of new technologies such as the cell sheet technique [21, 22], is needed to enhance donor cell engraftment and obtain the maximum benefits from MSC-based therapy. This issue will be further discussed in “Cell delivery route to the heart” section.
The third issue raised is the mechanism by which MSCs improve cardiac function. Originally, cardiomyogenic differentiation was expected to be the major mechanism for MSCs to recover damaged myocardium based on in vitro findings indicating cardiomyogenic potency of MSCs [23]. However, accumulating preclinical evidence indicates that differentiation of MSCs to cardiomyocytes does not occur to a significant extent in vivo [24]. Instead, the “paracrine effect” derived from secretion of MSCs is now believed to be the dominant mechanism. MSCs can secrete a group of cytokines, growth factors, and chemokines, which would beneficially modulate failing myocardium by reducing pathological fibrosis, increasing neovascular formation, attenuating cardiomyocyte apoptosis and hypertrophy, reducing inflammation, and stimulating endogenous stem/progenitor cells for myocardial regeneration [25–30]. This aspect will be further discussed in “Mechanism of MSC-based therapy” section.
Fourth, MSCs have a great advantage over other cell types as donor for cell therapy in being able to be used as allogeneic donor. MSCs have relatively low-immunogenic phenotypes and possess a powerful immunosuppressive secretion [10], allowing transplanted allogeneic or xenogeneic MSCs to survive and function to improve cardiac function without causing significant immunorejection. In previous large animal studies, 13 out of 16 (81 %) treatment groups using allogeneic and xenogeneic transplantation models showed positive therapeutic effects without showing serious complications, indicating great potential of this strategy. This issue will be further discussed in “Use of allogeneic MSCs” section.
Finally, among 23 treatment groups studied in the previous preclinical reports in large animals we listed, only seven treatment groups were investigated for the effects for more than 12 weeks. While five groups showed positive cardiac function improvement, while remaining 2 groups showed contradicting results. Further preclinical studies and clinical trials to investigate the long-term effect of MSC-based therapy are warranted.
Clinical trials
Promising results of preclinical studies have encouraged clinicians to undertake clinical trials of MSC-based therapy for heart diseases (Table 1). Currently, more than 40 clinical trials have been registered to evaluate the safety and/or efficacy of MSCs for the treatment of several types of heart diseases, including acute MI, ischemic heart failure, dilated cardiomyopathy, and Duchenne muscular dystrophy [31]. The results of 11 clinical trials have been reported to date (Table 2). Target diseases were either acute/subacute MI or ischemic heart failure, which were treated with MSC transplantation as a sole therapy [32–36] or in conjunction with percutaneous catheter intervention (PCI) [37–42] or coronary artery bypass surgery [37]. The results from these trials collectively showed that transplantation of MSCs was feasible and safe for the treatment of heart diseases. Although the patient numbers and observation periods may not be sufficient, there has been no report of serious cardiovascular adverse events, including tumor formation and arrhythmia occurrence, after MSC transplantation. This is generally consistent to the results from clinical trials of MSC-based therapy in other organs diseases. To date, more than 2,000 people have been injected with MSCs [43], and systemic analysis of these trials has confirmed the safety of MSC injection [7]. Efficacy of MSC-based therapies observed in these clinical trials is inconsistent, although many of them were not designed to evaluate the effect of the therapy. Improvement in LVEF was seen in 7 out of 11 trials (64 %) compared with the control groups or baseline, and even four “negative” reports suggested some benefits from MSC-based therapy including MI size reduction, wall motion score, and improvement in NYHA score. It is important to understand that LVEF is not the perfect indicator of the cell therapy efficacy, although it has been most frequently used as an endpoint. It is a load-dependent factor [32, 33], and the technique for measurement may not be fully consistent among centers and examiners (Table 2). Development of more objective and reproducible indicators, i.e., infarct size, is warranted.
The first randomized trial was reported by Chen and colleagues in 2004 [38]. PCI was performed within 12 h following the onset of acute MI, and then, patients were randomly divided into two arms: additional treatment of autologous MSCs injection via IC injection and normal saline. The average period from PCI to MSC or saline injection was 18.4 and 18.2 days, respectively. MSC injection group displayed significant improvement in cardiac function at 6 months after the treatment without any complications including arrhythmia occurrence. A recent C-CURE trial reported a corresponding result. IM injection of MSCs improved cardiac function for 2 years, without occurrence of adverse events, in chronic ischemic heart failure patients [34]. More recently, the TAC-HFT trial has reported that IM injection of autologous MSCs was similarly safe to IM injection of autologous bone marrow mononuclear cells during the 1-year follow-up period, but that MSCs appeared to achieve superior therapeutic effects [32]. Although LVEF was not changed, improvement in quality of life and reduction in infarct size were found after MSC injection. Not only autologous MSCs but also allogeneic MSCs have been injected to patients with heart disease, resulting in preliminary but promising outcome. The POSEIDON trial compared the safety and effects in IM injection of autologous MSCs and allogeneic MSCs for 13 months in patients with chronic ischemic heart failure [33]. There was no severe immunological response after allogeneic MSC injection with some therapeutic benefits, which appeared to be similar to those by autologous MSC injection.
These previous clinical trials raised several issues for consideration. Firstly, MSC doses are largely different between clinical trials, requiring further comparison (dose–effect) studies. Secondly, many cell delivery routes, including IM, IC, and IV injection, were used. Given preclinical information (“Preclinical studies” section), we will need to compare and improve these current methods and also develop novel cell delivery technologies. Thirdly, the methods of MSCs isolation and expansion have not been standardized. Culture materials (flask and culture medium and supplement), seeding density, passaging methods, and cryostorage protocols widely differ among trials, though these could significantly affect the quality of MSCs [39, 40]. In addition, longer-term safety and effect need to be investigated. Global consensus of the MSC preparation protocols and appropriately designed further clinical trials are warranted. Finally, although LVEF has been commonly used as the primary endpoint of the clinical trials, this may not be a perfect indicator, and development of a more precise indicator of therapeutic effects is warranted.
Future perspectives
From the discussion in preclinical studies and clinical trials, it is clear that further research and development is essential for MSC-based therapy to become a widely adopted standard therapy. The issues to be solved include the improvement in cell delivery route, elucidation of the mechanism of therapeutic effects, and validation of the use of allogeneic MSCs.
Cell delivery route to the heart
Current routes for MSC delivery for the treatment of heart disease include IV injection, IC injection, and IM injection. These have their own advantages and disadvantages, but importantly all these remain suboptimal. Particularly, engraftment of donor cells by any of these methods was disappointingly poor. Freyman et al. [20] reported that donor cell presence at 14 days after MSC administration was 6, 3, and 0 % after IC, IM, and IV injection, respectively, in a swine MI model. This indicates requirement of improvement in these methods and/or development of new cell delivery technologies.
IV injection
Systemic IV injection is an easier, less invasive, and more economical approach than other methods. It has been suggested that MSCs have a unique ability to recruit (“home”) into the injured heart [44], encouraging the use of the IV route. Potential homing signals include stromal cell-derived factor (SDF)-1α, interleukins (ILs), matrix metalloproteases (MMPs), and adhesion molecules at the myocardial side and integrins, selectins, and chemokine receptors at the MSC side. It is known that MSCs express CXCR4 (for SDF-1α), IL6RA and IL6ST (for IL-6), and CCR2 (for CCL7), E-selectin ligand, VLA-4 (integrin α4/β1), integrin α6/β1, integrin α8/β1, and α9/β1 [45]. However, it is likely that such homing systems are not sufficient even when the heart is suffering acute MI. Barbash and colleagues demonstrated that very few MSCs were accumulated in the heart after IV injection of 99mTc-labeled MSCs in rats with acute MI, and the most cells were localized in the lung [46]. Development of strategies to enhance such homing signals is needed for the success of this cell delivery route.
IM injection
This method has been frequently used in animal studies and clinical trials. By the IM injection, MSC suspensions are directly delivered into the myocardium via a needle inserted. Three approaches for IM injection have been reported: epicardial, endocardial, and transvascular approaches [47]. The epicardial IM injection allows to deliver cells into the aimed area under the direct vision or under the endoscopic observation. In contrast, endocardial IM and transvascular IM injection are performed using transcatheter techniques. For the endocardial approach, the percutaneously inserted catheter is advanced to the left ventricular cavity, and MSCs are injected into left ventricle walls, while for the transvascular approach, the catheter is placed in the coronary artery or the cardiac vein, and cells are injected into the myocardium via a needle penetrating the vascular wall.
The IM injection method is advantageous in delivering a large number of cells into a targeted area selectively. This method is free from the risk of coronary embolism unlike IC injection. In addition, the epicardial method is quite easy for surgeons to add routine cardiac surgery such as coronary artery bypass grafting. However, in addition to the poor efficiency of retention and survival of donor MSCs [48], formation of islet-like donor cell clusters is a problem for this method. Such isolated clusters are consisted of injected donor cells as well as host inflammatory cells, generating physical, biological, and electrical heterogeneity in the host myocardium, potentially resulting in arrhythmia occurrence [49].
Several reasons for the poor donor cell engraftment after IM injection have been reported. Donor cells prepared using trypsinization lose the cell surface proteins, reducing the cell–cell affinity and thereby being easily flushed out [50]. Mechanical injury induced by direct needle injection may cause donor cell damage and death directly (mechanical injury) or secondarily via inducing inflammation [51, 52]. It will be important to optimize injection pressure, volume of cell suspensions, and the needle type to improve donor cell engraftment and subsequent therapeutic effect from MSC-based therapy by IM injection.
IC injection
This is infusion of MSC suspensions into the coronary circulation. Two different approaches are available to undertake IC injection of MSCs, antegrade and retrograde IC injection [53]. These techniques are usually performed by the percutaneous catheter technique. Unlike the IM injection, the IC injection method can achieve more homogenous cell distribution in the target areas without producing cell clusters and with less inflammatory response [54].
However, donor cell engraftment after IC injection is similarly poor to that after IM injection. Ly and colleagues demonstrated the poor initial retention of injected cells, with 15 % of injected MSCs engrafted at 2 min and only 5 % detected at 1 h [55]. The injected cells by IC injection have to adhere to coronary endothelial cells via adhesion molecules or to be entrapped passively in the vessel lumen. Subsequently, these cells need to undergo transendothelial migration into the myocardial interstitium or integration into the vascular walls [56]. It is likely that these processes, which are usual in myocardial accumulation of inflammatory cells, do not appropriately occur after IC injection of MSCs, resulting in poor donor cell engraftment [20, 55].
Another important issue associated with IC injection of MSCs, which are relatively larger cells in size, is the risk of coronary embolization. Vullite and colleagues reported ST-T changes in ECG, increased plasma concentrations of cardiac troponin I, and histological findings of scattered regions of dense fibroplasias, suggesting occurrence of coronary embolisms leading to MI, after IC injection of MSCs in a dog model [57]. This risk will be more critical when the cells are injected into diffusely diseased and narrowed coronary arteries.
New technologies for MSC delivery
As discussed above, IV, IM, and IC injection all result in poor donor cell engraftment. This has encouraged developing new, more effective cell delivery techniques to the heart, including tissue engineering technologies. One of the most promising technologies for MSC delivery will be the “cell sheet” technique, developed by Okano et al. [21, 22]. They have developed a culture dish, the bottom of which is coated with temperature-responsive polymer (poly-N-isopropylacrylamide). At 37 °C, the polymer is hydrophobic, and cells can adhere to and grow on the dish to become confluent. While once the temperature is dropped to below 25 °C, the polymer turns to hydrophilic and swollen, letting the cells spontaneously to detach from the dish as a scaffold-free “cell sheet.” Cells in the cell sheet are supposed to have better-preserved cell surface proteins, cell–cell communications, and the underlying extracellular matrix, compared to cells dissociated by trypsinization. We have recently reported the utility of this technology for MSC-based therapy for heart disease [48]. Epicardial placement of an MSC sheet largely increased initial retention and subsequent presence; 94.8 and 61.4 % of grafted MSCs retained on the myocardial surface at 1 h and 3 days after MSCs sheet placement, respectively. These rates were 6.4-fold and 6.1-fold increased compared to IM injection, respectively (14.9 and 10.1 % at 1 h and day 3). More importantly, this effect by MSC sheet technique was correlated with significantly improved cardiac function recovery, in association with amplified paracrine effects, compared to IM injection. The cell sheet technology has entered a clinical trial with skeletal myoblasts [58], and clinical development of MSC sheet is warranted.
Mechanism of MSC-based therapy
Mechanisms by which transplanted MSCs improve cardiac function remain uncertain. Possible major mechanisms reported include transdifferentiation of MSCs toward cardiomyocytes and/or vascular cells and “paracrine effect” due to secretion of a range of cytokines and growth factors.
Differentiation to cardiomyocytes
It is a major aim of stem cell therapy to generate new cardiomyocytes derived from donor cells compensating cardiomyocyte loss by myocardial injury. There are reports showing cardiomyogenic differentiation potency of MSCs in vitro and in vivo. Makino and colleagues demonstrated that cultured MSCs can differentiate to cardiomyocyte-like cells in response to demethylating agent, 5-azacytidine in vitro [23]. Toma and colleagues reported that human MSCs intramyocardially injected into the mice heart obtained cardiomyocyte-specific features in vivo [59]. It was reported that bone morphogenetic protein (BMP)-2, fibroblast growth factor (FGF)-4, hepatocyte growth factor (HGF), insulin-like growth factor (IGF)-1, and transforming growth factor (TGF)-1β would play a role in the mechanism of cardiomyogenic differentiation of MSCs [60–62]. In addition, importance of direct cell–cell contact in differentiation of MSCs to cardiomyocytes has been suggested [63]. However, more recently, there have been accumulating in vivo reports showing that cardiomyogenic differentiation of transplanted MSCs does not occur to such a degree that the new cardiomyocytes influence global cardiac function [24]. Taken poor donor cell survival together, it is unlikely that cardiomyogenic differentiation of MSCs is the central mechanism of cardiac function improvement by MSC-based therapy [24].
Differentiation to vascular cells
Differentiation of MSCs to endothelial cells and vascular smooth muscle cells has also been reported. Oswald and colleagues demonstrated that MSCs differentiate toward the endothelial lineage and form capillary-like structures in vitro [64]. They also identified the role of vascular endothelial growth factor (VEGF) to enhance endothelial differentiation of MSCs. In vivo, Silva et al. [65] observed differentiation of IM-injected MSCs into smooth muscle cells and endothelial cells in a dog model of chronic myocardial ischemia. We also observed MSC-derived endothelial cells after IM injection and epicardial placement of MSC sheets in rat [48]. Thus, the frequency of in vivo transdifferentiation of MSCs to endothelial or smooth muscle cells appears to be more significant compared to differentiation to cardiomyocytes. However, the functional role of the vascular differentiation in cardiac function improvement after MSC-based therapy remains unclear, requiring further investigations.
Paracrine effect
Instead of differentiation, the “paracrine” mechanism is now focused as the key mechanism of the therapeutic effects induced by MSC-based therapy. Transplanted MSCs can secrete a range of growth factors, cytokines, and chemokines, which could help repairing failing myocardium undergoing adverse remodeling in association with persistent ischemia and inflammation in heart failure. Such factors could also be secreted from recipient cardiac cells such as cardiomyocytes, fibroblasts, and endothelial cells, in response to the stimuli occurred by MSC transplantation. Targets of the paracrine effects include many cell types including cardiomyocytes, fibroblasts, endothelial cells, accumulated inflammatory cells, and endogenous stem/progenitor cells [25–30].
Inflammation underpins the pathophysiology in both acute MI and chronic heart failure [2]. MSCs may be able to attenuate such inflammation via production of anti-inflammatory cytokines including IL-10, resulting in protection of the viable myocardium [66, 67]. Neovascularization, encompassing angiogenesis and vasculogenesis, is an important process to save and repair damaged tissues. There has been extensive experimental evidence that MSCs improve neovascular formation in the heart in association with upregulation of pro-angiogenic factors including VEGF, FGF, TGF-β, tumor necrosis factor (TNF)-α, and placenta growth factor [26]. Pathological fibrosis is a typical event in chronic heart failure [68]. Transplanted MSCs modulate expression of MMPs and tissue inhibitor of metalloproteinases (TIMPs) [67, 69], leading to favorable modulation of extracellular matrix (ECM) accumulation, increased ECM stability, and consequently prevention from the left ventricle dilatation and structural disorganization. Apoptosis of cardiomyocytes plays a role in progression of heart failure, with which two kinds of pathways including caspases and Bcl-2 are involved [70]. MSCs can modulate both apoptotic mechanisms through secreted factors such as HGF, IGF, FGF-2, Ang-2, VEGF, and Sfrp2, which lead to modulation of mitogen-activated protein kinase (MAPK) and PI3K-AKT signaling pathways [71–73]. In addition, there are increasing evidence that MSCs enhance proliferation and differentiation of endogenous cardiac stem cells in a paracrine manner for myocardial regeneration [29, 30].
Use of allogeneic MSCs
As donor for cell-based therapy, autologous cells are more convenient because these cells do not require immunosuppression and do not include ethical issues. However, the use of autologous cells is associated with several concerns and limitations. Stem cells collected from aged, diseased patients may have deteriorated cellular function including the ability of in vitro expansion and the capability to repair the damaged myocardium [74]. In addition, in the case of MSCs, it usually takes 4–8 weeks to collect/expand a sufficient number of autologous MSCs for heart failure treatment [5]. This prolonged culture period will delay the treatment and is associated with a risk of contamination by bacterial, fungus, and virus [75]. The use of allogeneic MSCs will solve many of these concerns. Ultimately, it will be possible to develop a bank of allogeneic MSCs, which can supply off-the-shelf, highly competent, quality controlled/assured MSCs upon requirement for treatment without delay. Therefore, if allogeneic MSCs can survive after transplantation to a similar degree to autologous MSCs without immunosuppression, it will be a great advantage, enhancing the therapeutic effects and expanding the application of MSC-based therapy.
Immunomodulation by MSCs
Research has shown that MSCs have relatively low expression of major histocompatibility complex (MHC) class antigens and also have the ability to secrete immunosuppressive factors. The expression level of MHC class Ia, which is a component recognized by T cells and a mediated lysis target of natural killer (NK) cells, is relatively low in MSCs [76]. In addition, expression of MHC class II, which plays a role in presenting antigens for T-cell activation, is absent or extremely low in MSCs [76]. Also, co-stimulators for T-cell activation (CD40, CD80, and CD86) are not expressed in MSCs [77]. In addition, MSCs are able to secret immunosuppressive soluble factors such as TGF-β, prostaglandin E2, HGF, soluble HLA-G, nitric oxide, galectin-1, and indoleamine 2,3-dioxygenase [78]. These result in attenuation of immunological response against allogeneic cells by inhibiting T-cell proliferation [79], B-cell proliferation, and immunoglobulin [80], response of NK cells [81], and dendritic cells activity [82].
Allogeneic MSC transplantation
The specific features of MSCs in low MHC antigen expression and immunosuppressive ability may allow allogeneic MSCs to survive and work for myocardial repair in the host heart without causing significant immunorejection. In fact, allogeneic MSCs have been injected into patients for the treatment of GVHD [83], autoimmune diseases [84], heart failure [33], and so on. Although a small number of reports suggested that administrated allogeneic MSCs were associated with some graft rejection, injection of allogeneic MSCs has been proven safe in general [25].
Among 15 preclinical studies of allogeneic MSC transplantation to the heart in large animals, 12 (80 %) reports demonstrated positive therapeutic effects, either in the short term, mid-term, or long term, in terms of cardiac function recovery (Table 1). Amado and colleagues reported that IM injection of allogeneic MSCs improved cardiac function without rejection by 8 weeks in a swine acute MI model [85]. Quevedo et al. [86] also demonstrated long-term MSC survival and engraftment by 12 weeks in a swine chronic MI model, contributing to improvement in LVEF and reduction in infarct size. Hashemi et al. [87], however, showed that, in swine post-MI acute heart failure model, IM injection of allogeneic MSCs reduced the infarct size by 12 weeks but did not improve LVEF. Allogeneic MSCs have been injected into patients with heart diseases [33]. This did not appear to induce severe immunological response, while obtaining some therapeutic benefits, which appeared to be similar to those by autologous MSC injection. Further investigations into preclinical and clinical trials are needed to elucidate whether allogeneic MSCs are really useful as donor for cell therapy for heart failure.
Conclusions
MSCs have great potential to become an established standard therapy for heart failure. However, for this ultimate goal, there remain several issues to be solved. In terms of safety, there are considerable amounts of data supporting the safety of MSCs in preclinical and clinical research; however, it is also true that there are reports warning about a risk of complications after MSC injection. Jeong and colleagues have shown that MSCs injected into the mouse heart with acute MI resulted in tumor formation with features of malignant sarcoma [17]. It was also reported by Breitbach et al. [16] that the MSCs injected in the myocardium formed bone-like structures in mice. However, these observations in mice should be interpreted with caution, as it is known that small rodents have genetic/chromosomal instability in MSCs, compared to human and large animals [18, 19, 88]. There was no such a finding in large animal studies so far. Nonetheless, one clinical trial reported a case, which developed eccrine poroma, a benign tumor after MSC injection for the treatment of stroke [89]. It is of importance to keep our extreme caution on the safety of MSCs, in particular long-term tumorigenicity and unwanted differentiation, in future preclinical and clinical research.
Most of the previous clinical trials reported preliminary but encouraging results in the therapeutic efficacy of MSC injection. However, it is obvious that the effect is limited by poor donor cell retention and survival. It is important to continue our effort to improve the current injection methods or development of new, more effective, cell delivery technologies. Comparisons of the effects among different cell delivery methods in homogenous patient populations using similar competent MSCs will be needed to decide the optimal protocol for MSC-based therapy. Continuation of challenges to enhance the therapeutic efficacy of MSC-based therapy by improving the capability of MSCs by physical and genetic pre-treatment may also be useful for the future success of MSC-based therapy [90, 91].
References
Liang CS, Delehanty JD (2009) Increasing post-myocardial infarction heart failure incidence in elderly patients a call for action. J Am Coll Cardiol 53:21–23
Frangogiannis NG, Smith CW, Entman ML (2002) The inflammatory response in myocardial infarction. Cardiovasc Res 53:31–47
Gordon O, Gilon D, He Z, May D, Lazarus A, Oppenheim A, Keshet E (2012) Vascular endothelial growth factor-induced neovascularization rescues cardiac function but not adverse remodeling at advanced ischemic heart disease. Arterioscler Thromb Vasc Biol 32:1642–1651
Sutton MG, Sharpe N (2000) Left ventricular remodeling after myocardial infarction: pathophysiology and therapy. Circulation 101:2981–2988
Mosna F, Sensebe L, Krampera M (2010) Human bone marrow and adipose tissue mesenchymal stem cells: a user’s guide. Stem Cells Dev 19:1449–1470
Lazarus HM, Haynesworth SE, Gerson SL, Rosenthal NS, Caplan AI (1995) Ex vivo expansion and subsequent infusion of human bone marrow-derived stromal progenitor cells (mesenchymal progenitor cells): implications for therapeutic use. Bone Marrow Transplant 16:557–564
Lalu MM, McIntyre L, Pugliese C, Fergusson D, Winston BW, Marshall JC, Granton J, Stewart DJ (2012) Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS One 7:e47559
Imanishi Y, Saito A, Komoda H, Kitagawa-Sakakida S, Miyagawa S, Kondoh H, Ichikawa H, Sawa Y (2008) Allogenic mesenchymal stem cell transplantation has a therapeutic effect in acute myocardial infarction in rats. J Mol Cell Cardiol 44:662–671
Nagaya N, Kangawa K, Itoh T, Iwase T, Murakami S, Miyahara Y, Fujii T, Uematsu M, Ohgushi H, Yamagishi M, Tokudome T, Mori H, Miyatake K, Kitamura S (2005) Transplantation of mesenchymal stem cells improves cardiac function in a rat model of dilated cardiomyopathy. Circulation 112:1128–1135
Nauta AJ, Fibbe WE (2007) Immunomodulatory properties of mesenchymal stromal cells. Blood 110:3499–3506
Friedenstein AJ, Chailakhjan RK, Lalykina KS (1970) The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet 3:393–403
Friedenstein AJ, Gorskaja JF, Kulagina NN (1976) Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol 4:267–274
Friedenstein AJ, Petrakova KV, Kurolesova AI, Frolova GP (1968) Heterotopic of bone marrow. Analysis of precursor cells for osteogenic and hematopoietic tissues. Transplantation 6:230–247
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop D, Horwitz E (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8:315–317
Breitbach M, Bostani T, Roell W, Xia Y, Dewald O, Nygren JM, Fries JW, Tiemann K, Bohlen H, Hescheler J, Welz A, Bloch W, Jacobsen SE, Fleischmann BK (2007) Potential risks of bone marrow cell transplantation into infarcted hearts. Blood 110:1362–1369
Jeong JO, Han JW, Kim JM, Cho HJ, Park C, Lee N, Kim DW, Yoon YS (2011) Malignant tumor formation after transplantation of short-term cultured bone marrow mesenchymal stem cells in experimental myocardial infarction and diabetic neuropathy. Circ Res 108:1340–1347
Miura M, Miura Y, Padilla-Nash HM, Molinolo AA, Fu B, Patel V, Seo BM, Sonoyama W, Zheng JJ, Baker CC, Chen W, Ried T, Shi S (2006) Accumulated chromosomal instability in murine bone marrow mesenchymal stem cells leads to malignant transformation. Stem Cells 24:1095–1103
Hatzistergos KE, Blum A, Ince T, Grichnik JM, Hare JM (2011) What is the oncologic risk of stem cell treatment for heart disease? Circ Res 108:1300–1303
Freyman T, Polin G, Osman H, Crary J, Lu M, Cheng L, Palasis M, Wilensky RL (2006) A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. Eur Heart J 27:1114–1122
Elloumi-Hannachi I, Yamato M, Okano T (2010) Cell sheet engineering: a unique nanotechnology for scaffold-free tissue reconstruction with clinical applications in regenerative medicine. J Intern Med 267:54–70
Yang J, Yamato M, Kohno C, Nishimoto A, Sekine H, Fukai F, Okano T (2005) Cell sheet engineering: recreating tissues without biodegradable scaffolds. Biomaterials 26:6415–6422
Makino S, Fukuda K, Miyoshi S, Konishi F, Kodama H, Pan J, Sano M, Takahashi T, Hori S, Abe H, Hata J, Umezawa A, Ogawa S (1999) Cardiomyocytes can be generated from marrow stromal cells in vitro. J Clin Invest 103:697–705
Noiseux N, Gnecchi M, Lopez-Ilasaca M, Zhang L, Solomon SD, Deb A, Dzau VJ, Pratt RE (2006) Mesenchymal stem cells overexpressing Akt dramatically repair infarcted myocardium and improve cardiac function despite infrequent cellular fusion or differentiation. Mol Ther 14:840–850
Griffin MD, Ritter T, Mahon BP (2010) Immunological aspects of allogeneic mesenchymal stem cell therapies. Hum Gene Ther 21:1641–1655
Kinnaird T, Stabile E, Burnett MS, Lee CW, Barr S, Fuchs S, Epstein SE (2004) Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circ Res 94:678–685
Kinnaird T, Stabile E, Burnett MS, Shou M, Lee CW, Barr S, Fuchs S, Epstein SE (2004) Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation 109:1543–1549
Tang YL, Zhao Q, Qin X, Shen L, Cheng L, Ge J, Phillips MI (2005) Paracrine action enhances the effects of autologous mesenchymal stem cell transplantation on vascular regeneration in rat model of myocardial infarction. Ann Thorac Surg 80:229–236; discussion 236–227
Hatzistergos KE, Quevedo H, Oskouei BN, Hu Q, Feigenbaum GS, Margitich IS, Mazhari R, Boyle AJ, Zambrano JP, Rodriguez JE, Dulce R, Pattany PM, Valdes D, Revilla C, Heldman AW, McNiece I, Hare JM (2010) Bone marrow mesenchymal stem cells stimulate cardiac stem cell proliferation and differentiation. Circ Res 107:913–922
Linke A, Muller P, Nurzynska D, Casarsa C, Torella D, Nascimbene A, Castaldo C, Cascapera S, Bohm M, Quaini F, Urbanek K, Leri A, Hintze TH, Kajstura J, Anversa P (2005) Stem cells in the dog heart are self-renewing, clonogenic, and multipotent and regenerate infarcted myocardium, improving cardiac function. Proc Natl Acad Sci USA 102:8966–8971
http://clinicaltrials.gov/. (Accessed 20 Oct 2013)
Heldman AW, DiFede DL, Fishman JE, Zambrano JP, Trachtenberg BH, Karantalis V, Mushtaq M, Williams AR, Suncion VY, McNiece IK, Ghersin E, Soto V, Lopera G, Miki R, Willens H, Hendel R, Mitrani R, Pattany P, Feigenbaum G, Oskouei B, Byrnes J, Lowery MH, Sierra J, Pujol MV, Delgado C, Gonzalez PJ, Rodriguez JE, Bagno LL, Rouy D, Altman P, Foo CW, da Silva J, Anderson E, Schwarz R, Mendizabal A, Hare JM (2014) Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC–HFT randomized trial. JAMA 311:62–73
Hare JM, Fishman JE, Gerstenblith G, DiFede Velazquez DL, Zambrano JP, Suncion VY, Tracy M, Ghersin E, Johnston PV, Brinker JA, Breton E, Davis-Sproul J, Schulman IH, Byrnes J, Mendizabal AM, Lowery MH, Rouy D, Altman P, Wong Po Foo C, Ruiz P, Amador A, Da Silva J, McNiece IK, Heldman AW (2012) Comparison of allogeneic vs autologous bone marrow-derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. JAMA 308:2369–2379
Bartunek J, Behfar A, Dolatabadi D, Vanderheyden M, Ostojic M, Dens J, El Nakadi B, Banovic M, Beleslin B, Vrolix M, Legrand V, Vrints C, Vanoverschelde JL, Crespo-Diaz R, Homsy C, Tendera M, Waldman S, Wijns W, Terzic A (2013) Cardiopoietic stem cell therapy in heart failure: the C-CURE (cardiopoietic stem cell therapy in heart failure) multicenter randomized trial with lineage-specified biologics. J Am Coll Cardiol 61:2329–2338
Lasala GP, Silva JA, Kusnick BA, Minguell JJ (2011) Combination stem cell therapy for the treatment of medically refractory coronary ischemia: a Phase I study. Cardiovasc Revasc Med 12:29–34
Williams AR, Trachtenberg B, Velazquez DL, McNiece I, Altman P, Rouy D, Mendizabal AM, Pattany PM, Lopera GA, Fishman J, Zambrano JP, Heldman AW, Hare JM (2011) Intramyocardial stem cell injection in patients with ischemic cardiomyopathy: functional recovery and reverse remodeling. Circ Res 108:792–796
Mohyeddin-Bonab M, Mohamad-Hassani MR, Alimoghaddam K, Sanatkar M, Gasemi M, Mirkhani H, Radmehr H, Salehi M, Eslami M, Farhig-Parsa A, Emami-Razavi H, Alemohammad MG, Solimani AA, Ghavamzadeh A, Nikbin B (2007) Autologous in vitro expanded mesenchymal stem cell therapy for human old myocardial infarction. Arch Iran Med 10:467–473
Chen SL, Fang WW, Ye F, Liu YH, Qian J, Shan SJ, Zhang JJ, Chunhua RZ, Liao LM, Lin S, Sun JP (2004) Effect on left ventricular function of intracoronary transplantation of autologous bone marrow mesenchymal stem cell in patients with acute myocardial infarction. Am J Cardiol 94:92–95
Gao LR, Pei XT, Ding QA, Chen Y, Zhang NK, Chen HY, Wang ZG, Wang YF, Zhu ZM, Li TC, Liu HL, Tong ZC, Yang Y, Nan X, Guo F, Shen JL, Shen YH, Zhang JJ, Fei YX, Xu HT, Wang LH, Tian HT, Liu DQ, Yang Y (2013) A critical challenge: dosage-related efficacy and acute complication intracoronary injection of autologous bone marrow mesenchymal stem cells in acute myocardial infarction. Int J Cardiol 168:3191–3199
Katritsis DG, Sotiropoulou PA, Karvouni E, Karabinos I, Korovesis S, Perez SA, Voridis EM, Papamichail M (2005) Transcoronary transplantation of autologous mesenchymal stem cells and endothelial progenitors into infarcted human myocardium. Catheter Cardiovasc Interv 65:321–329
Hare JM, Traverse JH, Henry TD, Dib N, Strumpf RK, Schulman SP, Gerstenblith G, DeMaria AN, Denktas AE, Gammon RS, Hermiller JB Jr, Reisman MA, Schaer GL, Sherman W (2009) A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. J Am Coll Cardiol 54:2277–2286
Yang Z, Zhang F, Ma W, Chen B, Zhou F, Xu Z, Zhang Y, Zhang D, Zhu T, Wang L, Wang H, Ding Z, Zhang Y (2010) A novel approach to transplanting bone marrow stem cells to repair human myocardial infarction: delivery via a noninfarct-relative artery. Cardiovasc Ther 28:380–385
Tolar J, Le Blanc K, Keating A, Blazar BR (2010) Concise review: hitting the right spot with mesenchymal stromal cells. Stem Cells 28:1446–1455
Kang SK, Shin IS, Ko MS, Jo JY, Ra JC (2012) Journey of mesenchymal stem cells for homing: strategies to enhance efficacy and safety of stem cell therapy. Stem Cells Int 2012:342968
Ip JE, Wu Y, Huang J, Zhang L, Pratt RE, Dzau VJ (2007) Mesenchymal stem cells use integrin beta1 not CXC chemokine receptor 4 for myocardial migration and engraftment. Mol Biol Cell 18:2873–2882
Barbash IM, Chouraqui P, Baron J, Feinberg MS, Etzion S, Tessone A, Miller L, Guetta E, Zipori D, Kedes LH, Kloner RA, Leor J (2003) Systemic delivery of bone marrow-derived mesenchymal stem cells to the infarcted myocardium: feasibility, cell migration, and body distribution. Circulation 108:863–868
Williams AR, Hare JM (2011) Mesenchymal stem cells: biology, pathophysiology, translational findings, and therapeutic implications for cardiac disease. Circ Res 109:923–940
Narita T, Shintani Y, Ikebe C, Kaneko M, Campbell NG, Coppen SR, Uppal R, Sawa Y, Yashiro K, Suzuki K (2013) The use of scaffold-free cell sheet technique to refine mesenchymal stromal cell-based therapy for heart failure. Mol Ther 21:860–867
Narita T, Shintani Y, Ikebe C, Kaneko M, Harada N, Tshuma N, Takahashi K, Campbell NG, Coppen SR, Yashiro K, Sawa Y, Suzuki K (2013) The use of cell-sheet technique eliminates arrhythmogenicity of skeletal myoblast-based therapy to the heart with enhanced therapeutic effects. Int J Cardiol 168:261–269
Huang HL, Hsing HW, Lai TC, Chen YW, Lee TR, Chan HT, Lyu PC, Wu CL, Lu YC, Lin ST, Lin CW, Lai CH, Chang HT, Chou HC, Chan HL (2010) Trypsin-induced proteome alteration during cell subculture in mammalian cells. J Biomed Sci 17:36
Fukushima S, Coppen SR, Lee J, Yamahara K, Felkin LE, Terracciano CM, Barton PJ, Yacoub MH, Suzuki K (2008) Choice of cell-delivery route for skeletal myoblast transplantation for treating post-infarction chronic heart failure in rat. PLoS One 3:e3071
Suzuki K, Murtuza B, Beauchamp JR, Brand NJ, Barton PJ, Varela-Carver A, Fukushima S, Coppen SR, Partridge TA, Yacoub MH (2004) Role of interleukin-1beta in acute inflammation and graft death after cell transplantation to the heart. Circulation 110:II219–II224
Campbell NG, Suzuki K (2012) Cell delivery routes for stem cell therapy to the heart: current and future approaches. J Cardiovasc Transl Res 5:713–726
Copland IB (2011) Mesenchymal stromal cells for cardiovascular disease. J Cardiovasc Dis Res 2:3–13
Ly HQ, Hoshino K, Pomerantseva I, Kawase Y, Yoneyama R, Takewa Y, Fortier A, Gibbs-Strauss SL, Vooght C, Frangioni JV, Hajjar RJ (2009) In vivo myocardial distribution of multipotent progenitor cells following intracoronary delivery in a swine model of myocardial infarction. Eur Heart J 30:2861–2868
Ruster B, Gottig S, Ludwig RJ, Bistrian R, Muller S, Seifried E, Gille J, Henschler R (2006) Mesenchymal stem cells display coordinated rolling and adhesion behavior on endothelial cells. Blood 108:3938–3944
Vulliet PR, Greeley M, Halloran SM, MacDonald KA, Kittleson MD (2004) Intra-coronary arterial injection of mesenchymal stromal cells and microinfarction in dogs. Lancet 363:783–784
Fujita T, Sakaguchi T, Miyagawa S, Saito A, Sekiya N, Izutani H, Sawa Y (2011) Clinical impact of combined transplantation of autologous skeletal myoblasts and bone marrow mononuclear cells in patients with severely deteriorated ischemic cardiomyopathy. Surg Today 41:1029–1036
Toma C, Pittenger MF, Cahill KS, Byrne BJ, Kessler PD (2002) Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation 105:93–98
Chang SA, Lee EJ, Kang HJ, Zhang SY, Kim JH, Li L, Youn SW, Lee CS, Kim KH, Won JY, Sohn JW, Park KW, Cho HJ, Yang SE, Oh WI, Yang YS, Ho WK, Park YB, Kim HS (2008) Impact of myocardial infarct proteins and oscillating pressure on the differentiation of mesenchymal stem cells: effect of acute myocardial infarction on stem cell differentiation. Stem Cells 26:1901–1912
Duan HF, Wu CT, Wu DL, Lu Y, Liu HJ, Ha XQ, Zhang QW, Wang H, Jia XX, Wang LS (2003) Treatment of myocardial ischemia with bone marrow-derived mesenchymal stem cells overexpressing hepatocyte growth factor. Mol Ther 8:467–474
Hahn JY, Cho HJ, Kang HJ, Kim TS, Kim MH, Chung JH, Bae JW, Oh BH, Park YB, Kim HS (2008) Pre-treatment of mesenchymal stem cells with a combination of growth factors enhances gap junction formation, cytoprotective effect on cardiomyocytes, and therapeutic efficacy for myocardial infarction. J Am Coll Cardiol 51:933–943
Wang T, Xu Z, Jiang W, Ma A (2006) Cell-to-cell contact induces mesenchymal stem cell to differentiate into cardiomyocyte and smooth muscle cell. Int J Cardiol 109:74–81
Oswald J, Boxberger S, Jorgensen B, Feldmann S, Ehninger G, Bornhauser M, Werner C (2004) Mesenchymal stem cells can be differentiated into endothelial cells in vitro. Stem Cells 22:377–384
Silva GV, Litovsky S, Assad JA, Sousa AL, Martin BJ, Vela D, Coulter SC, Lin J, Ober J, Vaughn WK, Branco RV, Oliveira EM, He R, Geng YJ, Willerson JT, Perin EC (2005) Mesenchymal stem cells differentiate into an endothelial phenotype, enhance vascular density, and improve heart function in a canine chronic ischemia model. Circulation 111:150–156
Burchfield JS, Iwasaki M, Koyanagi M, Urbich C, Rosenthal N, Zeiher AM, Dimmeler S (2008) Interleukin-10 from transplanted bone marrow mononuclear cells contributes to cardiac protection after myocardial infarction. Circ Res 103:203–211
Guo J, Lin GS, Bao CY, Hu ZM, Hu MY (2007) Anti-inflammation role for mesenchymal stem cells transplantation in myocardial infarction. Inflammation 30:97–104
Tsuda T, Gao E, Evangelisti L, Markova D, Ma X, Chu ML (2003) Post-ischemic myocardial fibrosis occurs independent of hemodynamic changes. Cardiovasc Res 59:926–933
Molina EJ, Palma J, Gupta D, Torres D, Gaughan JP, Houser S, Macha M (2009) Reverse remodeling is associated with changes in extracellular matrix proteases and tissue inhibitors after mesenchymal stem cell (MSC) treatment of pressure overload hypertrophy. J Tissue Eng Regen Med 3:85–91
Krijnen PA, Nijmeijer R, Meijer CJ, Visser CA, Hack CE, Niessen HW (2002) Apoptosis in myocardial ischaemia and infarction. J Clin Pathol 55:801–811
Afzal MR, Haider H, Idris NM, Jiang S, Ahmed RP, Ashraf M (2010) Preconditioning promotes survival and angiomyogenic potential of mesenchymal stem cells in the infarcted heart via NF-kappaB signaling. Antioxid Redox Signal 12:693–702
Isele NB, Lee HS, Landshamer S, Straube A, Padovan CS, Plesnila N, Culmsee C (2007) Bone marrow stromal cells mediate protection through stimulation of PI3-K/Akt and MAPK signaling in neurons. Neurochem Int 50:243–250
Tsubokawa T, Yagi K, Nakanishi C, Zuka M, Nohara A, Ino H, Fujino N, Konno T, Kawashiri MA, Ishibashi-Ueda H, Nagaya N, Yamagishi M (2008) Impact of anti-apoptotic and anti-oxidative effects of bone marrow mesenchymal stem cells with transient overexpression of heme oxygenase-1 on myocardial ischemia. Am J Physiol Heart Circ Physiol 298:H1320–H1329
Fossett E, Khan WS (2012) Optimising human mesenchymal stem cell numbers for clinical application: a literature review. Stem Cells Int 2012:465259
Drexler HG, Uphoff CC (2002) Mycoplasma contamination of cell cultures: incidence, sources, effects, detection, elimination, prevention. Cytotechnology 39:75–90
Huang XP, Sun Z, Miyagi Y, McDonald Kinkaid H, Zhang L, Weisel RD, Li RK (2010) Differentiation of allogeneic mesenchymal stem cells induces immunogenicity and limits their long-term benefits for myocardial repair. Circulation 122:2419–2429
Tse WT, Pendleton JD, Beyer WM, Egalka MC, Guinan EC (2003) Suppression of allogeneic T-cell proliferation by human marrow stromal cells: implications in transplantation. Transplantation 75:389–397
Dazzi F, Lopes L, Weng L (2012) Mesenchymal stromal cells: a key player in ‘innate tolerance’? Immunology 137:206–213
Glennie S, Soeiro I, Dyson PJ, Lam EW, Dazzi F (2005) Bone marrow mesenchymal stem cells induce division arrest anergy of activated T cells. Blood 105:2821–2827
Corcione A, Benvenuto F, Ferretti E, Giunti D, Cappiello V, Cazzanti F, Risso M, Gualandi F, Mancardi GL, Pistoia V, Uccelli A (2006) Human mesenchymal stem cells modulate B-cell functions. Blood 107:367–372
Spaggiari GM, Capobianco A, Becchetti S, Mingari MC, Moretta L (2006) Mesenchymal stem cell-natural killer cell interactions: evidence that activated NK cells are capable of killing MSCs, whereas MSCs can inhibit IL-2-induced NK-cell proliferation. Blood 107:1484–1490
Zhang B, Liu R, Shi D, Liu X, Chen Y, Dou X, Zhu X, Lu C, Liang W, Liao L, Zenke M, Zhao RC (2009) Mesenchymal stem cells induce mature dendritic cells into a novel Jagged-2-dependent regulatory dendritic cell population. Blood 113:46–57
Le Blanc K, Frassoni F, Ball L, Locatelli F, Roelofs H, Lewis I, Lanino E, Sundberg B, Bernardo ME, Remberger M, Dini G, Egeler RM, Bacigalupo A, Fibbe W, Ringden O (2008) Mesenchymal stem cells for treatment of steroid-resistant, severe, acute graft-versus-host disease: a phase II study. Lancet 371:1579–1586
Fotino C, Ricordi C, Lauriola V, Alejandro R, Pileggi A (2010) Bone marrow-derived stem cell transplantation for the treatment of insulin-dependent diabetes. Rev Diabet Stud 7:144–157
Amado LC, Saliaris AP, Schuleri KH, St John M, Xie JS, Cattaneo S, Durand DJ, Fitton T, Kuang JQ, Stewart G, Lehrke S, Baumgartner WW, Martin BJ, Heldman AW, Hare JM (2005) Cardiac repair with intramyocardial injection of allogeneic mesenchymal stem cells after myocardial infarction. Proc Natl Acad Sci USA 102:11474–11479
Quevedo HC, Hatzistergos KE, Oskouei BN, Feigenbaum GS, Rodriguez JE, Valdes D, Pattany PM, Zambrano JP, Hu Q, McNiece I, Heldman AW, Hare JM (2009) Allogeneic mesenchymal stem cells restore cardiac function in chronic ischemic cardiomyopathy via trilineage differentiating capacity. Proc Natl Acad Sci USA 106:14022–14027
Hashemi SM, Ghods S, Kolodgie FD, Parcham-Azad K, Keane M, Hamamdzic D, Young R, Rippy MK, Virmani R, Litt H, Wilensky RL (2008) A placebo controlled, dose-ranging, safety study of allogenic mesenchymal stem cells injected by endomyocardial delivery after an acute myocardial infarction. Eur Heart J 29:251–259
Foudah D, Redaelli S, Donzelli E, Bentivegna A, Miloso M, Dalpra L, Tredici G (2009) Monitoring the genomic stability of in vitro cultured rat bone-marrow-derived mesenchymal stem cells. Chromosome Res 17:1025–1039
Lee JS, Hong JM, Moon GJ, Lee PH, Ahn YH, Bang OY (2010) A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells 28:1099–1106
Hu X, Yu SP, Fraser JL, Lu Z, Ogle ME, Wang JA, Wei L (2008) Transplantation of hypoxia-preconditioned mesenchymal stem cells improves infarcted heart function via enhanced survival of implanted cells and angiogenesis. J Thorac Cardiovasc Surg 135:799–808
Mangi AA, Noiseux N, Kong D, He H, Rezvani M, Ingwall JS, Dzau VJ (2003) Mesenchymal stem cells modified with Akt prevent remodeling and restore performance of infarcted hearts. Nat Med 9:1195–1201
Boomsma RA, Swaminathan PD, Geenen DL (2007) Intravenously injected mesenchymal stem cells home to viable myocardium after coronary occlusion and preserve systolic function without altering infarct size. Int J Cardiol 122:17–28
Van Linthout S, Savvatis K, Miteva K, Peng J, Ringe J, Warstat K, Schmidt-Lucke C, Sittinger M, Schultheiss HP, Tschope C (2011) Mesenchymal stem cells improve murine acute coxsackievirus B3-induced myocarditis. Eur Heart J 32:2168–2178
van der Bogt KE, Sheikh AY, Schrepfer S, Hoyt G, Cao F, Ransohoff KJ, Swijnenburg RJ, Pearl J, Lee A, Fischbein M, Contag CH, Robbins RC, Wu JC (2008) Comparison of different adult stem cell types for treatment of myocardial ischemia. Circulation 118:S121–S129
van der Bogt KE, Schrepfer S, Yu J, Sheikh AY, Hoyt G, Govaert JA, Velotta JB, Contag CH, Robbins RC, Wu JC (2009) Comparison of transplantation of adipose tissue- and bone marrow-derived mesenchymal stem cells in the infarcted heart. Transplantation 87:642–652
Cho J, Zhai P, Maejima Y, Sadoshima J (2011) Myocardial injection with GSK-3beta-overexpressing bone marrow-derived mesenchymal stem cells attenuates cardiac dysfunction after myocardial infarction. Circ Res 108:478–489
Buccini S, Haider KH, Ahmed RP, Jiang S, Ashraf M (2012) Cardiac progenitors derived from reprogrammed mesenchymal stem cells contribute to angiomyogenic repair of the infarcted heart. Basic Res Cardiol 107:301
Grauss RW, Winter EM, van Tuyn J, Pijnappels DA, Steijn RV, Hogers B, van der Geest RJ, de Vries AA, Steendijk P, van der Laarse A, Gittenberger-de Groot AC, Schalij MJ, Atsma DE (2007) Mesenchymal stem cells from ischemic heart disease patients improve left ventricular function after acute myocardial infarction. Am J Physiol Heart Circ Physiol 293:H2438–H2447
Li TS, Cheng K, Malliaras K, Smith RR, Zhang Y, Sun B, Matsushita N, Blusztajn A, Terrovitis J, Kusuoka H, Marban L, Marban E (2012) Direct comparison of different stem cell types and subpopulations reveals superior paracrine potency and myocardial repair efficacy with cardiosphere-derived cells. J Am Coll Cardiol 59:942–953
Derval N, Barandon L, Dufourcq P, Leroux L, Lamaziere JM, Daret D, Couffinhal T, Duplaa C (2008) Epicardial deposition of endothelial progenitor and mesenchymal stem cells in a coated muscle patch after myocardial infarction in a murine model. Eur J Cardiothorac Surg 34:248–254
Mills WR, Mal N, Kiedrowski MJ, Unger R, Forudi F, Popovic ZB, Penn MS, Laurita KR (2007) Stem cell therapy enhances electrical viability in myocardial infarction. J Mol Cell Cardiol 42:304–314
Ohnishi S, Yanagawa B, Tanaka K, Miyahara Y, Obata H, Kataoka M, Kodama M, Ishibashi-Ueda H, Kangawa K, Kitamura S, Nagaya N (2007) Transplantation of mesenchymal stem cells attenuates myocardial injury and dysfunction in a rat model of acute myocarditis. J Mol Cell Cardiol 42:88–97
Nagaya N, Fujii T, Iwase T, Ohgushi H, Itoh T, Uematsu M, Yamagishi M, Mori H, Kangawa K, Kitamura S (2004) Intravenous administration of mesenchymal stem cells improves cardiac function in rats with acute myocardial infarction through angiogenesis and myogenesis. Am J Physiol Heart Circ Physiol 287:H2670–H2676
Li Y, Yao Y, Sheng Z, Yang Y, Ma G (2011) Dual-modal tracking of transplanted mesenchymal stem cells after myocardial infarction. Int J Nanomed 6:815–823
Lopez Y, Lutjemeier B, Seshareddy K, Trevino EM, Hageman KS, Musch TI, Borgarelli M, Weiss ML (2013) Wharton’s jelly or bone marrow mesenchymal stromal cells improve cardiac function following myocardial infarction for more than 32 weeks in a rat model: a preliminary report. Curr Stem Cell Res Ther 8:46–59
Wang T, Tang W, Sun S, Wan Z, Xu T, Huang Z, Weil MH (2009) Mesenchymal stem cells improve outcomes of cardiopulmonary resuscitation in myocardial infarcted rats. J Mol Cell Cardiol 46:378–384
Khan M, Meduru S, Mohan IK, Kuppusamy ML, Wisel S, Kulkarni A, Rivera BK, Hamlin RL, Kuppusamy P (2009) Hyperbaric oxygenation enhances transplanted cell graft and functional recovery in the infarct heart. J Mol Cell Cardiol 47:275–287
Jiang S, Haider H, Idris NM, Salim A, Ashraf M (2006) Supportive interaction between cell survival signaling and angiocompetent factors enhances donor cell survival and promotes angiomyogenesis for cardiac repair. Circ Res 99:776–784
Tang J, Xie Q, Pan G, Wang J, Wang M (2006) Mesenchymal stem cells participate in angiogenesis and improve heart function in rat model of myocardial ischemia with reperfusion. Eur J Cardiothorac Surg 30:353–361
Jiang S, Kh Haider H, Ahmed RP, Idris NM, Salim A, Ashraf M (2008) Transcriptional profiling of young and old mesenchymal stem cells in response to oxygen deprivation and reparability of the infarcted myocardium. J Mol Cell Cardiol 44:582–596
Davani S, Marandin A, Mersin N, Royer B, Kantelip B, Herve P, Etievent JP, Kantelip JP (2003) Mesenchymal progenitor cells differentiate into an endothelial phenotype, enhance vascular density, and improve heart function in a rat cellular cardiomyoplasty model. Circulation 108(Suppl. 1):II253–II258
Furlani D, Li W, Pittermann E, Klopsch C, Wang L, Knopp A, Jungebluth P, Thedinga E, Havenstein C, Westien I, Ugurlucan M, Li RK, Ma N, Steinhoff G (2009) A transformed cell population derived from cultured mesenchymal stem cells has no functional effect after transplantation into the injured heart. Cell Transplant 18:319–331
Al Kindi AH, Asenjo JF, Ge Y, Chen GY, Bhathena J, Chiu RC, Prakash S, Shum-Tim D (2011) Microencapsulation to reduce mechanical loss of microspheres: implications in myocardial cell therapy. Eur J Cardiothorac Surg 39:241–247
Wang W, Jin P, Wang L, Yang Z, Hu S, Gao B, Zhang H (2010) Impact of escaped bone marrow mesenchymal stromal cells on extracardiac organs after intramyocardial implantation in a rat myocardial infarction model. Cell Transplant 19:1599–1607
Zeng B, Chen H, Zhu C, Ren X, Lin G, Cao F (2008) Effects of combined mesenchymal stem cells and heme oxygenase-1 therapy on cardiac performance. Eur J Cardiothorac Surg 34:850–856
Dai W, Hale SL, Martin BJ, Kuang JQ, Dow JS, Wold LE, Kloner RA (2005) Allogeneic mesenchymal stem cell transplantation in postinfarcted rat myocardium: short- and long-term effects. Circulation 112:214–223
Guarita-Souza LC, Carvalho KA, Rebelatto C, Senegaglia A, Hansen P, Furuta M, Miyague N, Francisco JC, Olandoski M, Faria-Neto JR, Oliveira SA, Brofman PR (2006) Cell transplantation: differential effects of myoblasts and mesenchymal stem cells. Int J Cardiol 111:423–429
Amsalem Y, Mardor Y, Feinberg MS, Landa N, Miller L, Daniels D, Ocherashvilli A, Holbova R, Yosef O, Barbash IM, Leor J (2007) Iron-oxide labeling and outcome of transplanted mesenchymal stem cells in the infarcted myocardium. Circulation 116:I38–I45
Gao LR, Zhang NK, Bai J, Ding QA, Wang ZG, Zhu ZM, Fei YX, Yang Y, Xu RY, Chen Y (2010) The apelin-APJ pathway exists in cardiomyogenic cells derived from mesenchymal stem cells in vitro and in vivo. Cell Transplant 19:949–958
Wang A, Shen F, Liang Y, Wang J (2011) Marrow-derived MSCs and atorvastatin improve cardiac function in rat model of AMI. Int J Cardiol 150:28–32
Flynn A, Chen X, O’Connell E, O’Brien T (2012) A comparison of the efficacy of transplantation of bone marrow-derived mesenchymal stem cells and unrestricted somatic stem cells on outcome after acute myocardial infarction. Stem Cell Res Ther 3:36
Wang T, Sun S, Wan Z, Weil MH, Tang W (2012) Effects of bone marrow mesenchymal stem cells in a rat model of myocardial infarction. Resuscitation 83:1391–1396
Enoki C, Otani H, Sato D, Okada T, Hattori R, Imamura H (2010) Enhanced mesenchymal cell engraftment by IGF-1 improves left ventricular function in rats undergoing myocardial infarction. Int J Cardiol 138:9–18
Hou M, Yang KM, Zhang H, Zhu WQ, Duan FJ, Wang H, Song YH, Wei YJ, Hu SS (2007) Transplantation of mesenchymal stem cells from human bone marrow improves damaged heart function in rats. Int J Cardiol 115:220–228
Wang M, Tan J, Wang Y, Meldrum KK, Dinarello CA, Meldrum DR (2009) IL-18 binding protein-expressing mesenchymal stem cells improve myocardial protection after ischemia or infarction. Proc Natl Acad Sci USA 106:17499–17504
Bayes-Genis A, Soler-Botija C, Farre J, Sepulveda P, Raya A, Roura S, Prat-Vidal C, Galvez-Monton C, Montero JA, Buscher D, Izpisua Belmonte JC (2010) Human progenitor cells derived from cardiac adipose tissue ameliorate myocardial infarction in rodents. J Mol Cell Cardiol 49:771–780
Arminan A, Gandia C, Garcia-Verdugo JM, Lledo E, Trigueros C, Ruiz-Sauri A, Minana MD, Solves P, Paya R, Montero JA, Sepulveda P (2010) Mesenchymal stem cells provide better results than hematopoietic precursors for the treatment of myocardial infarction. J Am Coll Cardiol 55:2244–2253
Herrmann JL, Abarbanell AM, Wang Y, Weil BR, Poynter JA, Manukyan MC, Meldrum DR (2011) Transforming growth factor-alpha enhances stem cell-mediated postischemic myocardial protection. Ann Thorac Surg 92:1719–1725
Rasmussen JG, Frobert O, Holst-Hansen C, Kastrup J, Baandrup U, Zachar V, Fink T, Simonsen U (2012) Comparison of human adipose-derived stem cells and bone marrow-derived stem cells in a myocardial infarction model. Cell Transplant 23:195–206
Molina EJ, Palma J, Gupta D, Torres D, Gaughan JP, Houser S, Macha M (2008) Improvement in hemodynamic performance, exercise capacity, inflammatory profile, and left ventricular reverse remodeling after intracoronary delivery of mesenchymal stem cells in an experimental model of pressure overload hypertrophy. J Thorac Cardiovasc Surg 135:292–299
Mokashi SA, Guan J, Wang D, Tchantchaleishvili V, Brigham M, Lipsitz S, Lee LS, Schmitto JD, Bolman RM 3rd, Khademhosseini A, Liao R, Chen FY (2010) Preventing cardiac remodeling: the combination of cell-based therapy and cardiac support therapy preserves left ventricular function in rodent model of myocardial ischemia. J Thorac Cardiovasc Surg 140:1374–1380
Kang K, Sun L, Xiao Y, Li SH, Wu J, Guo J, Jiang SL, Yang L, Yau TM, Weisel RD, Radisic M, Li RK (2012) Aged human cells rejuvenated by cytokine enhancement of biomaterials for surgical ventricular restoration. J Am Coll Cardiol 60:2237–2249
Xu YL, Gao YH, Liu Z, Tan KB, Hua X, Fang ZQ, Wang YL, Wang YJ, Xia HM, Zhuo ZX (2010) Myocardium-targeted transplantation of mesenchymal stem cells by diagnostic ultrasound-mediated microbubble destruction improves cardiac function in myocardial infarction of New Zealand rabbits. Int J Cardiol 138:182–195
Price MJ, Chou CC, Frantzen M, Miyamoto T, Kar S, Lee S, Shah PK, Martin BJ, Lill M, Forrester JS, Chen PS, Makkar RR (2006) Intravenous mesenchymal stem cell therapy early after reperfused acute myocardial infarction improves left ventricular function and alters electrophysiologic properties. Int J Cardiol 111:231–239
Halkos ME, Zhao ZQ, Kerendi F, Wang NP, Jiang R, Schmarkey LS, Martin BJ, Quyyumi AA, Few WL, Kin H, Guyton RA, Vinten-Johansen J (2008) Intravenous infusion of mesenchymal stem cells enhances regional perfusion and improves ventricular function in a porcine model of myocardial infarction. Basic Res Cardiol 103:525–536
Schuleri KH, Centola M, Choi SH, Evers KS, Dawoud F, George RT, Lima JA, Lardo AC (2011) Multi-detector computed tomography for evaluation of myocardial cell therapy in heart failure: a comparison with CMR imaging. JACC Cardiovasc Imaging 4:1284–1293
Yang YJ, Qian HY, Huang J, Geng YJ, Gao RL, Dou KF, Yang GS, Li JJ, Shen R, He ZX, Lu MJ, Zhao SH (2008) Atorvastatin treatment improves survival and effects of implanted mesenchymal stem cells in post-infarct swine hearts. Eur Heart J 29:1578–1590
Huang SD, Lu FL, Xu XY, Liu XH, Zhao XX, Zhao BZ, Wang L, Gong DJ, Yuan Y, Xu ZY (2006) Transplantation of angiogenin-overexpressing mesenchymal stem cells synergistically augments cardiac function in a porcine model of chronic ischemia. J Thorac Cardiovasc Surg 132:1329–1338
Schuleri KH, Feigenbaum GS, Centola M, Weiss ES, Zimmet JM, Turney J, Kellner J, Zviman MM, Hatzistergos KE, Detrick B, Conte JV, McNiece I, Steenbergen C, Lardo AC, Hare JM (2009) Autologous mesenchymal stem cells produce reverse remodelling in chronic ischaemic cardiomyopathy. Eur Heart J 30:2722–2732
Wang X, Jameel MN, Li Q, Mansoor A, Qiang X, Swingen C, Panetta C, Zhang J (2009) Stem cells for myocardial repair with use of a transarterial catheter. Circulation 120:S238–S246
Amado LC, Schuleri KH, Saliaris AP, Boyle AJ, Helm R, Oskouei B, Centola M, Eneboe V, Young R, Lima JA, Lardo AC, Heldman AW, Hare JM (2006) Multimodality noninvasive imaging demonstrates in vivo cardiac regeneration after mesenchymal stem cell therapy. J Am Coll Cardiol 48:2116–2124
Schuleri KH, Amado LC, Boyle AJ, Centola M, Saliaris AP, Gutman MR, Hatzistergos KE, Oskouei BN, Zimmet JM, Young RG, Heldman AW, Lardo AC, Hare JM (2008) Early improvement in cardiac tissue perfusion due to mesenchymal stem cells. Am J Physiol Heart Circ Physiol 294:H2002–H2011
Williams AR, Hatzistergos KE, Addicott B, McCall F, Carvalho D, Suncion V, Morales AR, Da Silva J, Sussman MA, Heldman AW, Hare JM (2013) Enhanced effect of combining human cardiac stem cells and bone marrow mesenchymal stem cells to reduce infarct size and to restore cardiac function after myocardial infarction. Circulation 127:213–223
Valina C, Pinkernell K, Song YH, Bai X, Sadat S, Campeau RJ, Le Jemtel TH, Alt E (2007) Intracoronary administration of autologous adipose tissue-derived stem cells improves left ventricular function, perfusion, and remodelling after acute myocardial infarction. Eur Heart J 28:2667–2677
Peng C, Yang K, Xiang P, Zhang C, Zou L, Wu X, Gao Y, Kang Z, He K, Liu J, Cheng M, Wang J, Chen L (2013) Effect of transplantation with autologous bone marrow stem cells on acute myocardial infarction. Int J Cardiol 162:158–165
Dubois C, Liu X, Claus P, Marsboom G, Pokreisz P, Vandenwijngaert S, Depelteau H, Streb W, Chaothawee L, Maes F, Gheysens O, Debyser Z, Gillijns H, Pellens M, Vandendriessche T, Chuah M, Collen D, Verbeken E, Belmans A, Van de Werf F, Bogaert J, Janssens S (2010) Differential effects of progenitor cell populations on left ventricular remodeling and myocardial neovascularization after myocardial infarction. J Am Coll Cardiol 55:2232–2243
Dixon JA, Gorman RC, Stroud RE, Bouges S, Hirotsugu H, Gorman JH 3rd, Martens TP, Itescu S, Schuster MD, Plappert T, St John-Sutton MG, Spinale FG (2009) Mesenchymal cell transplantation and myocardial remodeling after myocardial infarction. Circulation 120:S220–S229
Houtgraaf JH, de Jong R, Kazemi K, de Groot D, van der Spoel TI, Arslan F, Hoefer I, Pasterkamp G, Itescu S, Zijlstra F, Geleijnse ML, Serruys PW, Duckers HJ (2013) Intracoronary infusion of allogeneic mesenchymal precursor cells directly after experimental acute myocardial infarction reduces infarct size, abrogates adverse remodeling, and improves cardiac function. Circ Res 113:153–166
Perin EC, Silva GV, Assad JA, Vela D, Buja LM, Sousa AL, Litovsky S, Lin J, Vaughn WK, Coulter S, Fernandes MR, Willerson JT (2008) Comparison of intracoronary and transendocardial delivery of allogeneic mesenchymal cells in a canine model of acute myocardial infarction. J Mol Cell Cardiol 44:486–495
Acknowledgments
This work was supported by the National Institute of Health Research-funded Barts Cardiovascular Biomedical Research Unit, British Heart Foundation and Heart Research UK.
Conflict of interest
Drs. Ken Suzuki and Takuya Narita have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narita, T., Suzuki, K. Bone marrow-derived mesenchymal stem cells for the treatment of heart failure. Heart Fail Rev 20, 53–68 (2015). https://doi.org/10.1007/s10741-014-9435-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-014-9435-x