Abstract
The aetiology of pericardial effusion has been generally assessed by clinical work-up only, which leaves a large cohort of patients with “idiopathic” effusions virtually undiagnosed. In accordance with the ESC guidelines, this contribution intends to change this attitude. After therapeutic or diagnostic pericardiocentesis of 259 patients with large to moderate pericardial effusions, pericardial fluid, epicardial and pericardial biopsies, and blood samples were analysed by PCR for cardiotropic microbial agents. Cytology, histology, immunohistology of tissue and fluids and laboratory tests were performed. Of the 259 patients, 35 % suffered from an autoreactive aetiology, 28 % suffered from a malignant and 14 % from an infectious cause. Investigating all samples by PCR, we identified viral genomes in 51 (19.7 %) patients, parvovirus B19 (B19 V) being identified in 25 and Epstein–Barr virus (EBV) in 19 cases. In patients with a sole infectious aetiology (n = 36), B19 V was detected in 21 and EBV in 10 cases. When differentiating with regard to the material investigated for the presence of cardiotropic viruses, parvovirus B19 was most often detected in the epicardium and EBV was most frequently detected in the pericardial fluid independent from the final diagnostic categorisation. Bacterial cultures including tests for tuberculosis were all negative. Molecular techniques improve sensitivity, specificity and diagnostic accuracy for the underlying aetiology in pericarditis patients with effusion. The identification of specific viral signatures will help to understand pathogenetic mechanisms in pericarditis and allow to tailor an adequate therapy beyond antiphlogistic treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pericarditis is defined as a condition, in which the pericardium or the pericardial sac surrounding the heart is inflamed [1–3]. Pericarditis may affect only the pericardium or may occur in association with a number of systemic diseases. In most cases not only the pericardial but also the epicardial layer is affected, which is referred to by the term myopericarditis or perimyocarditis describing pericarditis associated with myocardial damage. Major causes for acute or chronic pericarditis include viral or bacterial infections, myocardial infarction (postinfarction syndrome), cardiac surgery (postpericardiotomy syndrome), chest trauma, malignancies, diagnostic or interventional cardiac procedures, drugs and toxins, metabolic disorders, mediastinal radiation and systemic inflammatory diseases. The minimum clinical diagnostic procedures in patients with pericardial diseases include first the physical evaluation of patients reporting chest pain and pericardial friction rub, typical ECG findings such as low QRS voltage, ST-changes or a bundle brunch block, chest X-ray and the evaluation of markers of inflammation and myocardial lesion. The detection and quantification of a pericardial effusion (PE) by echocardiography confirms the suspicion of pericarditis [1, 4]. If a specific cause using traditional diagnostic tests to exclude tuberculosis, neoplastic aetiology or systemic autoimmune diseases is not identifiable, the disease is often named idiopathic pericarditis [1–5] with the consequence of an empiric anti-inflammatory treatment. This may depend on the respective patient population investigated and also in part on demographics, but most often it is the result of the inadequate diagnostic procedures and methods used [6–8].
Very often the yield of a standard diagnostic evaluation to determine the aetiology of pericarditis is relatively low. For example, it has been shown that in countries with a high prevalence of both poverty and HIV, a dramatic increase in tuberculous pericarditis is detectable [7, 8]. On the other hand, in patients with an acute pericarditis in Europe, in whom no cause is identified, the aetiology is frequently just presumed to be viral, but viral aetiology has never been established correctly [1–6]. Viral infections that may cause pericarditis include viruses often associated with inflammatory heart disease, for example, coxsackieviruses A and B, echovirus, adenovirus, herpes viruses, influenza viruses, parvovirus B19 and HHV6 [5–9]. The infectious organism in patients with pericarditis may induce direct damage or cause it by the immune response, which initially started to resolve the infection but lead to recurrence of the inflammation by an autoreactive process.
Since the aetiology of pericardial effusions is difficult to assess on the basis of clinical assessment only, the accurate evaluation of the pericardial effusion and the tissue samples from the pericardium and epicardium is of paramount interest [7–9]. For that reason, we investigated in accordance with the 2004 Guidelines on the Diagnosis and Management of Pericardial Diseases [9] 259 consecutive patients with moderate or large pericardial effusion to diagnose the underlying aetiology by cytology, immunohistochemistry and molecular methods to determine whether a viral or bacterial infection is involved by the evaluation of the pericardial effusion and/or pericardial/epicardial tissue, which we used in addition to antimicrobial serology in the circulating blood and the effusion. Once the infectious aetiology of the pericardial disease is established, this enables the selection of an appropriate causative treatment in a given patient, which will be reported in a subsequent publication.
Methods
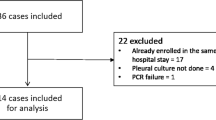
A total of 259 consecutive patients with moderate to large pericardial effusions undergoing pericardiocentesis with pericardioscopy-guided pericardial and epicardial biopsy for therapeutic and/or diagnostic reasons were included in this evaluation after written informed consent. Age, sex, type of effusion according to the Horowitz classification [10] and NYHA class of the patients are given in Table 1. Pericardial fluid and tissue samples retrieved from the pericardial and epicardial layers by targeted epi- and pericardial biopsy under pericardioscopical control [11, 12] were collected at the time of therapeutic or diagnostic pericardiocentesis as described elsewhere [9, 11–14]. Pericardial fluid samples were divided for laboratory analyses including biochemical parameters, cytology, bacterial cultures and polymerase chain reaction (PCR) for identification of cardiotropic viruses (influenza A, parvovirus B19, cytomegalovirus, enterovirus, adenovirus, human herpes virus 6, Epstein–Barr virus), as well as Borrelia burgdorferi, Chlamydia pneumoniae and Mycobacterium tuberculosis. To exclude systemic viral or bacterial infection, peripheral blood was investigated in parallel by PCR for all patients. Samples of pericardial fluid and of the serum of each patient were also analysed for tuberculosis by a routine Ziehl Neelsen stain and for antibodies against the above-mentioned cardiotropic viruses and bacteria including HIV and Hepatitis C. The analyses of epicardial biopsies included the histopathological examination by two independent pathologists. Immunohistochemistry and PCR for the identification of cardiotropic viruses and bacteria were carried out as previously described [9, 11–14].
In brief, immunohistochemistry was performed with the epicardial or pericardial biopsies. For demonstration of infiltrating cells antibodies specific for activated T and B cells, macrophages, major histocompatibility class 1 and class 2 antigens, adhesion molecules and endothelial cells were used. Specific binding of the antibodies indicating an inflammatory reaction was demonstrated by peroxidase double-staining procedure. For the demonstration of cardiotropic viruses in the epicardial and pericardial biopsies or the pericardial effusion, the QIAamp Blood Mini Kit and the QIAamp Tissue Kit (Qiagen, Hilden, Germany) were used to extract total DNA and RNA from the samples. Conditions for PCR and primers have been described elsewhere [9, 11–14]. Ten microlitres of extracted DNA/RNA was incubated with 25 pmol of the appropriate primer, 5 μl 10× PCR buffer (1.5 mmol MgCl2), 10 mmol dNTP’s and 2.5 U Taq polymerase gold (Applied Biosystems, USA) and deionised H2O in a 50 μl final reaction volume [5, 15, 16]. After an initial incubation at 94 °C for 12 min, 40 rounds of amplification were performed under the following conditions: 94 °C (denaturation) for 45 s, appropriate temperature for each primer pair between 45 and 60 °C for 45 s, 72 °C (extension) for 1 min. A final cycle of 72 °C for 5 min for complete polymerisation followed. For the detection of the RNA viruses, influenza virus A and coxsackievirus B, an initial reverse transcription using the RT-One-step-PCR-KIT (Qiagen, Hilden, Germany) was performed. Ten microlitres of each reaction were analysed on a 1.5 % agarose gel (Sigma, Deisenhofen, Germany) containing 0.5 μg/ml ethidium bromide (σ). All samples were run together with an appropriate positive control and two negative controls (Fig. 1). In addition to conventional PCR, real-time PCR for the quantification of parvovirus B19 and EBV in the pericardial fluid and the tissue samples was used. A TaqMan probe labelled with 6-carboxyfluorescein-phosphoramidite (FAM) enables the real-time detection of the target amplicons. All samples prepared using the above-mentioned conditions were run simultaneously with a dilution series of parvovirus B19/EBV-positive controls ranging from 108 to 104 genome equivalents (GE) per microgram of isolated nucleic acids and were amplified together with the FAM 490 labelled TaqMan probe. The quantification of the viral DNA concentrations of unknown samples is based on the calibration curve with the external viral standards (Fig. 2a, b).
Detection of EBV in the pericardial fluid of a patient with infectious pericarditis using agarose gel electrophoresis (left side) and Southern blot hybridisation (right side) for confirmation of the result. The positive patient sample is indicated by the triangle; the positive controls are indicated with arrows. The size of the amplificate was measured in comparison with the basepair marker shown
a Dilution series of the B19 V-positive control (positive plasma with a concentration of 108–104 genome equivalents per microgram of isolated nucleic acids) using real-time PCR and a FAM labelled TaqMan probe. b Positive patient sample derived from an epicardial biopsy with a concentration of 3.3 × 104 genome equivalents/μg DNA)
The causes for the respective pericardial effusions were diagnosed according to the results of epicardial and pericardial tissue and the pericardial fluid analysis. The nomenclature followed the criteria defined by the Task Force on Pericardial Diseases of the European Society of Cardiology published in 2004 [9]. In brief, the diagnosis of malignant pericardial effusion was based on either the presence of malignant cells in pericardial fluid or the presence of an invasive tumour in pericardioscopy-guided pericardial biopsy specimens [5, 9, 17–20]. In case of an autoreactive pericarditis, the patients met the following criteria (1) pericardial fluid revealing >5,000/mm3 mononuclear cells or the detection of antisarcolemmal antibodies, (2) the inflammation in epicardial, pericardial or endomyocardial biopsies by >14 lymphocytes/mm2 or an infiltrate of lymphocytes using immunohistochemistry, (3) the exclusion of an active viral infection by PCR, (4) the exclusion of tuberculosis and other bacterial infections by PCR and/or bacterial cultures, (5) the absence of neoplastic infiltrations, and (6) the exclusion of systemic and metabolic disorders including uraemia. Infectious pericarditis was diagnosed by the presence of cardiotropic viruses [coxsackievirus B, parvovirus B19 (B19 V), cytomegalovirus (CMV), adenovirus type 2 (ADV), human herpesvirus 6 (HHV6) and Epstein–Barr virus (EBV)] shown by PCR in all samples of pericardial fluid and/or in the tissue collected from peri-, epi- or endomyocardial biopsies or a positive result for bacterial agents isolated by fluid cultures [5, 9, 17–23].
Statistical analyses
Results are given as mean ± standard deviation, and p values < 0.05 were considered statistically significant (two-sided test). Comparison of parametric variables was made by a two-tailed Student’s t test. Nonparametric variables were compared using the Mann–Whitney test, and categorical parameters were compared using the chi-square or Fisher`s exact test as appropriate. The software packages SigmaPlot version 11.0 were used.
Results
A total of 259 patients investigated were diagnosed according to the results of epicardial tissue and pericardial fluid analysis (Table 2). Most often patients with PE suffered from an autoreactive aetiology (35 %), followed by patients with a malignant (28 %) and an infectious (14 %) aetiology. The group of patients classified as traumatic/iatrogenic (15 %) comprised patients with direct chest trauma (n = 4), after myocardial infarction (n = 6), pericardial haemorrhage after pacemaker implantation (n = 15) or other interventional procedures (heart catherisation with percutaneous transluminal coronary angioplasty or endomyocardial biopsy n = 15). The group of patients with other causes (8 %) comprised patients with systemic inflammatory pneumonia, sepsis (n = 11), uraemia (n = 4) or metabolic diseases (n = 5).
By investigating samples from 259 patients with pericardial effusions using PCR for the detection of cardiotropic viral and bacterial genomes, we were able to identify the underlying viral causes in 51 patients (19.7 %); no bacterial genomes were detected in this investigation. The most often detected virus was parvovirus B19 in 49 % of cases (n = 25) followed by EBV in 37 % of cases (n = 19) (Table 3). A total of 34 of these patients (13 %) could be classified as patients with a viral aetiology only without a concomitant systemic, metabolic or malignant disorder. Interestingly, in 12 patients with proven malignant pericardial effusion, a viral genome was also detected. The type of viral genome detected in those patients differed considerably from the type of virus detected in patients with a pure viral aetiology (Fig. 3a, b). In patients with malignant disorders, EBV in 59 % of cases (7 patients) was the most often detected virus followed by a double viral infection with EBV and parvovirus B19 in two cases, and the single detection of parvovirus B19, influenza virus and CMV in one case, each (Fig. 3a). In contrast, in patients with an isolated PCR-positive viral aetiology, parvovirus B19 was the most often detected virus (62 %) followed by EBV in 10 patients (29 %) (Fig. 3b). Remarkably in 5 patients from the group of patients with trauma or iatrogenically induced pericardial effusion viral genome was also detectable: parvovirus B19 genome was found in the epicardial biopsy of three (7.5 %) and EBV in the pericardial fluid of two patients(5 %).
Viral loads were determined for all parvovirus B19-positive patients ranging from 4.1 × 102 GE/μg DNA lowest to 7 × 106 GE/μg DNA highest in epicardial biopsies. The mean value over all samples was 8.2 × 104 GE/μg DNA with no significant difference between patients with infectious or malignant aetiology. With regard to the quantification of EBV in pericardial effusion and epicardial biopsies viral loads vary considerably lower ranging from 0.2 × 101 GE/μg DNA lowest to 9.5 × 103 GE/μg DNA highest with a mean value of 9.5 × 102 GE/μg DNA, there was no significant difference between the viral loads of EBV in the epicardial biopsies or the pericardial fluid in patients with infectious versus malignant aetiology.
With regard to the determination of antiviral antibodies in the pericardial effusion and serum of the patients, we were able to identify one patient with an infectious pericardial effusion due to an active and systemic Hepatitis C infection by the presence of HepC-specific IgM antibodies in the effusion and the serum. With regard to IgG antibodies specific for the most often detected viruses, EBV IgG antibodies were detected in 178 patients, parvovirus B19 IgG antibodies were detected in 129 patients, and HHV6 IgG antibodies were detected in 107 patients with no significant differences between the patient subgroups. IgM antibodies specific for EBV were positive for one patient with an autoreactive aetiology, IgM antibodies specific for parvovirus B19 were positive for one patient with a viral aetiology (PCR for B19 V positive) and two patients with an malignant aetiology. IgM antibodies specific for HHV6 were detected in 26 patients suffering from infectious pericarditis (9 patients), autoreactive pericarditis (6 patients) and malignant pericarditis (8 patients). When analysing the presence of the genome of cardiotropic viruses in the different samples, we were able to show that parvovirus B19 DNA was most often detected in the epicardial tissue samples, whereas EBV DNA was most often detected in the pericardial fluid, irrespective of the underlying aetiology be it infectious or malignant. Figure 4 illustrates that parvovirus B19 was detected in epicardial biopsies of patients with infectious aetiology in 64 % of cases and in the epicardial biopsies of patients with a proven malignant effusion in only 25 % of cases. On the other hand, EBV was detectable in 29 % of the effusions from patients with an infectious aetiology and in 66 % of the effusions from patients with a malignant effusion. In the case of a metastatic pericardial effusion associated with the presence of a viral genome in the cardiac samples, we consider this to be of a mixed aetiology. Of note, in this cohort of consecutive patients, all patients were tested negative for HIV and tuberculosis.
Discussion
Methods
All PCR investigations including the real-time experiments were performed twice to confirm the results in every sample. The peripheral blood of all patients was investigated to exclude systemic viral infection or contamination of pericardial effusion/pericardial tissue by blood cells. These tests were negative in all cases. Since in each set of PCRs performed, all negative controls were negative; no artificial background due to contamination was found. Efficacy of quantitative real-time PCR was comparable between all runs and reproducible with a value of 97.4 %.
Findings
By the consecutive investigation of 259 patients with pericardial effusion after pericardiocentesis and pericardioscopy-guided peri- and epicardial biopsy with all methods available following the criteria defined by the Task Force on Pericardial Diseases of the European Society of Cardiology published in 2004 [9], we were able to establish a specific diagnosis with regard to an infectious, autoreactive or malignant aetiology in 73 % of cases. In particular, the use of molecular tools like PCR helped to detect the persistence of specific viral genomes in epicardial tissue samples or pericardial fluid in 51 patients. As the intrapericardial triamcinolone therapy has been shown to be effective in preventing short-term and probably also long-term recurrences in radiogenic or autoimmune effusions [13], it is most important to exclude a possible viral infection in those patients and to demonstrate an autoreactive process instead.
In general, the treatment of chronic or acute pericardial effusions should be targeted to the cause, but it often remains empirical without a thorough examination of the underlying aetiology [24, 25]. The current treatment regimens with non-steroidal anti-inflammatory drugs (NSAIDs) or colchicine in “idiopathic” cases [26–28] may hide our diagnostic failures and are in addition symptomatic treatment only. Whether there is a possibility for a specific antiviral treatment in patients with viral-positive pericardial effusion cannot be derived from this investigation, nevertheless, we should keep in mind that in a significant proportion of patients with a viral aetiology, additional treatment options are available. From our data, it can be derived that in patients with a viral aetiology, neither a systemic nor an intrapericardial application of corticosteroids is justified. Corticosteroids should be used only in patients with an autoreactive, viral-negative pericardial effusions and tissue or in patients with systemic autoimmune disease [5, 9, 13]. Secondly, the higher prevalence for the detection of parvovirus B19 preferentially in epicardial biopsies and EBV preferentially in pericardial effusion may reflect different pathogenetic mechanisms, which have to be investigated further.
Samples of all patients were also tested for the detection of antiviral IgM or IgA antibodies in the pericardial fluid and in the serum. By this approach, we were able to identify one patient with an infectious pericardial effusion due to an active, systemic Hepatitis C infection by the presence of specific IgM antibodies coexisting in the pericardial fluid and in the serum. There was no correlation between the multitude of antiviral IgG antibodies in the serum and the pericardial fluid, on the one hand, and the molecular PCR analyses for cardiotropic viruses in the patients with pericarditis, but obviously patients with a positive PCR for microbial agents in the samples were also positive for the respective serum antibodies. IgG antibodies to cardiotropic viruses in the serum and to a lesser extend also in the pericardial fluid just reflect the infectious biography of a patient as it has been shown recently in patients with myocarditis [29]. We propose, however, to investigate viral antibodies specific for Hepatitis C, HIV, Rickettsia burnetii and B. burgdorferi in endemic regions further on in all patients with suspected pericarditis as well as in myocarditis.
Molecular techniques such as PCR provide an accurate aetiological diagnosis with an excellent sensitivity, specificity and diagnostic accuracy. This also applies to patients with pericardial diseases. We were able to show that with regard to the different tissues investigated, the most frequently detected viral genomes were parvovirus B19 and Epstein–Barr virus, with a differential distribution, however. We still know very little about the role and distribution of these viruses in inflammatory pericardial diseases. Parvovirus B19 has been discussed as a possible aetiologic agent in myocarditis and DCM with inflammation (DCMi) and without inflammation [16, 30, 31], but was not yet appreciated in peri(myocardial) disease. This is the first larger cross-sectional study to demonstrate parvovirus B19 in patients with moderate to large pericardial effusions, although an infection with parvovirus B19 in myopericarditis has already been reported in single cases previously [32]. The predominant detection of parvovirus B19 in epicardial tissue in contrast to the pericardial fluid indicates myocardial involvement in these patients as well. Whether a myocardial injury secondary to parvovirus B19 infection of the pericardium is linked to a cellular immune response leading to myocarditis in these patients is not unlikely but this hypothesis has to be investigated by clinically following parvovirus B19-positive patients with moderate to large pericardial effusions.
EBV infections are rarely reported to induce cardiac symptoms. EBV-linked acute pericarditis or perimyocarditis was only reported in few immunocompetent patients or in immunocompromised individuals [33, 34]. The frequent detection of EBV especially in the pericardial fluid of patients as the only source of viral aetiology or in patients with a malignant aetiology of their pericardial effusion gives rise to the assumption that there is a role for EBV in co-inducing pericardial effusion particularly in immunocompromised patients. Interestingly, EBV persistence has been discussed as a marker of biological aggressiveness in patients with breast cancer [35]. Our own cohort of patients with malignant pericardial effusion included only 3 patients with breast cancer, two of whom were positive for EBV. We will follow all EBV-positive patients without tumours to elaborate, whether the detection of EBV may serve as a hint for a later manifestation of malignant disease.
Study limitations
There are some study limitations which should be acknowledged: most of the patients were referred to our hospital as a tertiary referral center especially in cases of a non-malignant origin, which may cause some unavoidable selection bias. In addition, the patients investigated here presented with moderate to large pericardial effusion since only in them pericardiocentesis and targeted epi- and pericardial biopsy could be carried out safely. Of note, no severe complication requiring cardiac surgery was experienced from our procedures. The aim of the investigation was to provide a recent update of the prevalence of different aetiologies in a German cohort of patients with moderate to large pericardial effusion. We think that this investigation may provide a stronger evidence base for future diagnostic recommendations and clinical research in the field.
Conclusions
Molecular techniques such as PCR provide an accurate diagnosis which improves sensitivity, specificity and diagnostic accuracy in patients with pericardial diseases. The identification of specific viruses in subgroups of patients or in different tissue compartments will help to understand the complex pathogenetic mechanisms in pericardial diseases. Although there is no straight correlation between the serology and the molecular analyses for most cardiotropic viruses in patients with pericarditis, the determination of viral antibodies specific for Hepatitis C, HIV, R. burnetii and the assessment of B. burgdorferi in endemic areas in all patients with suspected pericarditis appears to be helpful.
References
Troughton RW, Asher CR, Klein AL (2004) Pericarditis. Lancet 363:717–727
Spodick DH (1997) The pericardium: a comprehensive textbook, 1st edn. Marcel Dekker, New York, p 260
LeWinter MM, Tischler MD (2012) Pericardial disease. In: Braunwald E, Bonow RO, Mann DL, Zipes D, Libby P (eds) Heart disease: a textbook of cardiovascular medicine, 9th edn. W.B. Saunders Company, Philadelphia PA, pp 1651–1671
Spodick DH (2001) Pericardial disease. In: Braunwald E, Zipes D, Libby P (eds) Heart disease: a textbook of cardiovascular medicine. W.B. Saunders Company, New York
Maisch B, Ristic A, Seferovic P (2011) Tsang TSM. Interventional Pericardiology, Springer Medizin, Verlag Heidelberg
Corey GR, Campbell PT, Van Trigt P, Kenney RT, O’Connor CM, Sheikh KH, Kisslo JA, Wall TC (1993) Etiology of large pericardial effusions. Am J Med 95(2):209
Mayosi BM, Burgess LJ, Doubell AF (2005) Tuberculous pericarditis. Circulation 112:3608–3616
Sagrista-Sauleda J, Mercé J, Permanyer-Miralda G, Soler–Soler J (2000) Clinical clues to the causes of large pericardial effusions. Am J Med 109(2):95–101
Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH (2004) Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases executive summary. Eur Heart J 25(7):587–610
Horowitz MDS, Schultz CS, Stinson EB, Harrison DC, Popp RL (1974) Sensitivity and specificity of echocardiographic diagnosis in pericardial effusion. Circulation 50:239–245
Maisch B, Ristić AD (2003) Practical aspects of the management of pericardial disease. Heart 89(9):1096–1103
Maisch B, Drude L (1991) Pericardioscopy—a new diagnostic tool in inflammatory diseases of the pericardium. Eur Heart J 12(Suppl B):2–7
Maisch B, Ristic AD, Pankuweit S (2002) Intrapericardial treatment of autoreactive pericardial effusion with triamcinolone; the way to avoid side effects of systemic corticosteroid therapy. Eur Heart J 23:1503–1508
Maisch B, Ristic AD, Pankuweit S, Neubauer A, Moll R (2002) Neoplastic pericardial effusion. efficacy and safety of intrapericardial treatment with cisplatin. Eur Heart J 23(20):1625–1631
Pankuweit S, Portig I, Eckhardt H, Crombach M, Hufnagel G, Maisch B (2000) Prevalence of viral genome in endomyocardial biopsies from patients with inflammatory heart muscle disease. Herz 25(3):221–226
Pankuweit S, Moll R, Baantrup U, Portig I, Hufnagel G, Maisch B (2003) Prevalence of the parvovirus B19 genome in endomyocardial biopsy specimens. Hum Pathol 34:497–500
Pankuweit S, Wädlich A, Meyer E, Portig I, Hufnagel G, Maisch B (2000) Cytokine activation in pericardial fluids in different forms of pericarditis. Herz 25(8):748–754
Dalla Pozza R, Hartl D, Bechtold S, Urschel S, Kozlik-Feldmann R, Pankuweit S, Belohradsky B, Netz H (2007) Recurrent pericarditis in children: elevated cardiac autoantibodies. Clin Res Cardiol 96:1–8
Karatolios K, Pankuweit S, Goettsch C, Hofbauer LC, Timmesfeld N, Al-Fakhri N, Maisch B, Schoppet M (2012) Osteoprotegerin (OPG) and TNF-related apoptosis-inducing ligand (TRAIL) levels in malignant and benign pericardial effusions. Clin Biochem 45(3):237–242
Karatolios K, Pankuweit S, Moosdorf RG, Maisch B (2012) Vascular endothelial growth factor in malignant and benign pericardial effusion. Clin Cardiol 35(6):377–378
Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, Martin I, Nordet P (1996) Report of the 1995 World Health Organization/International society and federation of cardiology task force on the definition and classification of cardiomyopathies. Circulation 93:841–842
Maisch B, Bültman B, Factor S, Gröne HJ, Hufnagel, Kawamura K, Kühl U, Olsen EJ, Pankuweit S, Virmani R (1999) World Heart Federation consensus conference’s definition of inflammatory cardiomyopathy (myocarditis): report from two expert committees on histology and viral cardiomyopathy. Heartbeat 4:3–4
Maisch B, Portig I, Ristic A, Hufnagel G, Pankuweit S (2000) Definition of inflammatory cardiomyopathy (myocarditis): on the way to consensus. Herz 25(3):200–209
Imazio M, Mayosi BM, Brucato A, Markel G, Trinchero R, Spodick DH, Adler Y (2010) Triage and management of pericardial effusion. J Cardiovasc Med (Hagerstown) 11:928–935
Imazio M (2012) Contemporary management of pericardial diseases. Curr Opin Cardiol 27(3):308–317
Sagrista`-Sauleda J, Merce′ AS, Soler-Soler J (2011) Diagnosis and management of pericardial effusion. World J Cardiol 3:135–143
Imazio M, Spodick DH, Brucato A, Trinchero R, Adler Y (2010) Controversial issues in the management of pericardial diseases. Circulation 121:916–928
Imazio M (2011) Evaluation and management of pericarditis. Expert Rev Cardiovasc Ther 9(9):1221–1233
Mahfoud F, Gärtner B, Kindermann M, Ukena C, Gadomski K, Klingel K, Kandolf R, Böhm M, Kindermann I (2011) Virus serology in patients with suspected myocarditis: utility or futility? Eur Heart J 32(7):897–903
Rohayem J, Dinger J, Fischer R, Klingel K, Kandolf R, Rethwilm A (2001) Fatal myocarditis associated with acute parvovirus B19 and human herpesvirus 6 coinfection. J Clin Microbiol 39:4585–4587
Heegaard ED, Eiskjaer H, Baandrup U, Hornsleth A (1998) Case report: parvovirus B19 infection associated with myocarditis following adult cardiac transplantation. Scand J Infect Dis 30:607–610
Chia JKS (1996) Myopericarditis due to parvovirus B19 in an adult. Clin Infect Dis 23:200–201
Zafrir B, Aviv A, Reichman N, Flatau E (2005) Epstein-Barr virus associated pericarditis and pericardial effusion: case report and diagnostic aspects. Eur J Intern Med 16:528–530
Roubille F, Gahide G, Moore-Morris T, Granier M, Davy JM, Vernhet H, Piot C (2008) Epstein Barr virus (EBV) and acute myopericarditis in an immunocompetent patient: first demonstrated case and discussion. Intern Med 47(7):627–629
Mazouni C, Fina F, Romain S, Ouafik L, Bonnier P, Brandone J, Martin P (2011) Epstein-Barr virus as a marker of biological aggressiveness in breast cancer. Br J Cancer 18; 104(2):332–7
Acknowledgments
This work was partially funded by the Federal Ministry of Education and Research 01GI 0205-TP9a to BM and SP and by the Cardiac Promotion Society Marburg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pankuweit, S., Stein, A., Karatolios, K. et al. Viral genomes in the pericardial fluid and in peri- and epicardial biopsies from a German cohort of patients with large to moderate pericardial effusions. Heart Fail Rev 18, 329–336 (2013). https://doi.org/10.1007/s10741-013-9375-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-013-9375-x