Abstract
We investigate the issue of patient readmission at a large academic hospital in the U.S. Specifically, we look for evidence that patients discharged when post-operative unit utilization is high are more likely to be readmitted. After examining data from 7,800 surgeries performed in 2007, we conclude that patients who are discharged from a highly utilized post-operative unit are more likely to be readmitted within 72 h. Each additional bed utilized at time of discharge increases the odds of readmission on average by 0.35% (Odds Ratio = 1.008, 95% CI [1.003, 1.012]). We propose that this effect is due to an increased discharge rate when the unit is highly utilized.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The current structure of the U.S. healthcare system rewards hospitals based on the volume of specialty services they can provide. Surgical volume is often the primary driver of hospitals’ revenues and profits. The income from surgeries is used to subsidize other less profitable, but vital hospital operations. Surgeons derive a large portion of their income on a per-operation basis. The more surgeries a surgeon can perform, the more money the surgeon will earn. Both surgeons and the hospital want to ensure that as many surgeries as possible are performed each day.
Many resources are required to perform a surgery. In addition to an operating room, nurses, and a surgeon, there must be an available bed in a downstream recovery unit such as an intensive care unit, an intermediate care unit, or an acute care unit. Often, the limiting factor in how many surgeries can be performed is the number of available beds in the post-operative path. If there is no bed available for the patient, the surgery must be cancelled or postponed.
In previous work, Anderson et al. [2] showed that both higher post-operative bed utilization and higher demand for beds (more incoming surgeries) lead to increases in the discharge rate. They offered two explanations for this increase: either patients were being held longer than needed when beds were available, or they were being discharged early when beds were needed for incoming patients. While they showed that the discharge rate was increased by higher utilization, they were not able to reach a conclusion that explained this increase.
In this paper, we examine how the utilization of beds on the post-operative path at the time of discharge affects the readmission rate among surgery patients. By looking at readmission rates, we try to determine which of the two explanations for the higher discharge rate is applicable. If patients are discharged too soon when utilization is high, we would expect to see an increase in the readmission rate. A patient who is still recovering will be more likely to return to the hospital than one who is ready to be discharged. However, if patients are simply being held longer until space is needed, we should not see any effect on readmissions. Figure 1 illustrates the hypothesis that we test in this paper. We are confident in the direction of the causal arrows, because utilization precedes readmissions. When patients are readmitted to the hospital, they are not sent back to the post-operative unit, so they do not affect the utilization rate. Instead, they are either treated through the emergency department, or in a bed elsewhere in the hospital. In this paper, we examine surgical data from a large urban teaching hospital in the U.S.
In Section 2, we review the relevant literature with respect to hospital readmission. In Section 3, we describe our data, explain the methodology, and present our results. In Section 4, we mention the limitations of our work. In Section 5, we discuss the implication of our results and provide conclusions.
2 Literature review
Our work focuses on studying post-operative readmission. We seek to show a connection between decreased length of stay due to early discharge and increased likelihood of readmission. We hypothesize that higher utilization leads to inappropriately shorter length of stay and, thus, increased readmissions. In doing so, we summarize the literature on length of stay because we are not aware of any work that has connected utilization to readmission. While some studies have shown a relationship between length of stay and readmission, others have found no evidence for such a link. Hasan [11] provides a short survey of work studying hospital readmissions. He concludes that while premature discharge has been proposed as a cause for readmission, no causal link has been shown. We focus on the effect of length of stay on readmission in this section for two reasons. First, we are not aware of any papers that study the effect of utilization on readmission. Secondly, we hypothesize that high utilization causes a decrease in length of stay.
As already mentioned, the literature is split on whether or not length of stay has an effect on readmission rate. It seems that length of stay does not have an effect on readmission rate, unless the length of stay is artificially shortened. Bohmer et al. [3] studied the readmission rate after coronary bypass surgery and found that there was no relationship between length of stay and readmission rate. However, they showed that cost savings from shorter stays were offset by increased use of post-acute services. Cowper et al. [6] found that patients discharged early after coronary bypass graft surgeries did not have a higher readmission rate, and had an average cumulative savings of over $6,000. Delaney et al. [7] observed that patients selected for a “fast track” discharge protocol were no more likely to be readmitted. In addition, these patients had shorter lengths of stay and lower costs.
However, there is evidence that early discharge leads to higher rates of readmission. Niehaus et al. [13] concluded that patients discharged because of bed shortages in psychiatric hospitals were significantly more likely to be readmitted. Campbell et al. [4] used length of stay as a significant predictor of readmission after discharge from an intensive care unit. Hwang et al. [12] found that patients who disregarded medical advice and left the hospital early were significantly more likely to be readmitted within 15 days. Dobson et al. [8] proposed a model of ICU bumping. They modeled physicians’ decisions on which patients to discharge early when bed space in the ICU is limited. They found that the surgical schedule influences physicians’ decisions to bump patients. They concluded that under some circumstances it is optimal, in terms of throughput, for surgeons to discharge patients before it would be medically advisable.
3 Data and analysis
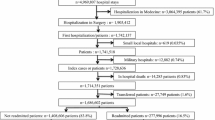
We were provided surgical data by a large urban east coast U.S. academic hospital on every surgery patient during the first half of 2007 (January 1, 2007 to June 1, 2007). During that time period, there were no major changes in operating room procedures or scheduling. The dataset contains information on patient age, surgical schedule type (emergency vs. elective), and the surgical specialty group that performed the surgery. Our data contains a total of 5,265 (adult) patients admitted as inpatients. We also have available the date and time of the surgery, the dates when the patient was admitted to and discharged from the hospital, and the dates when the patient was readmitted, if any. Using this dataset, we calculated the number of post-operative beds that were utilized at the start of each day during the fiscal year. The hospital has a dedicated post-operative unit that has surgical ICU beds, acute care beds, and intermediate care beds.
We focus our analysis on differences in readmission rates within 72 h because we expect the effect that utilization has on readmission to be most prominent in the first few days. The 72-hour cutoff is important because a patient readmitted within 72 h of discharge must be treated as part of inpatient services and billed as one claim, thereby reducing the amount the hospital makes from the procedure. If a patient is discharged before he/she is ready to be sent home, we expect that he/she will be more likely to be readmitted sooner rather than later. While an early discharge might lead to more complications down the road, it might particularly lead to more complications in the short term. We will examine readmission rates in every time frame up to 30 days after discharge, but our main focus is on rates within 72 h. In this study, we only address readmission after discharge from the hospital, not “bounce backs” when patients move back to an ICU from a step-down unit.
We examine how the percent of patients who were readmitted within 72 h varies with changes in bed utilization upon discharge. When utilization was high (above 94%), 15.4% of patients were readmitted within 72 h, compared to just 10% of those discharged when utilization was below 94%. A chi-square test comparing these two rates found that they were statistically different (p < .0001). After 30 days, 55% of patients discharged from a full (utilization >94%) post-operative unit were readmitted, while only 50% were readmitted of those discharged when utilization was lower. We initially choose 94% as the cutoff for high utilization because previous work (Anderson et al. [2]) found an increased discharge rate when utilization crossed that threshold. Table 1 shows the average readmission rates within 72 h for different ranges of downstream bed utilization. As utilization increases, the readmission rate increases, especially at the highest range of utilization. Figure 2 shows the relationship between discharge rate and readmission. As utilization increases, the discharge rate (shown by triangles) and the readmission rate (shown by squares) both increase. The discharge rate shown here is the percent of patients discharged each day.
We construct four logistic regression models to study the relationship between readmission rate and occupancy level at the time of discharge. We use a dichotomous dependent variable, i.e., whether or not a patient is readmitted within 72 h of discharge from the hospital. To determine if increased utilization of post-operative beds at the time of discharge increases the readmission rate, we need to define a suitable measure for increased utilization. We use two different variables: an indicator variable (called FULL) that is 1 if utilization is above a certain threshold when the patient is discharged and 0 otherwise, and a continuous variable (called BEDS) that gives the number of filled beds when the patient was discharged. We use four models because we have two different utilization metrics (continuous and discrete), and we examine readmission in the entire post-operative ward as well as just in the trauma surgical line. Using these four models allows us to study the relationship between utilization and readmission rates in more depth. Table 2 summarizes the variables used in our models.
In our first model (Model 1), we regress readmission within 72 h on FULL. We control for the patient’s age, race, gender, and the type of surgery. Age, race, and gender have previously been shown to be important factors of readmission (see Hannan et al. [10]). In addition, type of surgery has an important effect on readmissions (see Goodney et al. [9]). By controlling for other determinants of readmission, we are able to isolate the effect of being discharged from a full unit. Our control variables are relevant, not only practically but also statistically, since each variable lowers the Akaike Information Criterion (AIC) (see [1]) when added to the model.
The equation for this logistic regression model is given by
The baseline case, in which all dummy variables are 0, is a white, female patient in the general surgery line. The results from this model are presented in Table 3. We do not exclude any insignificant predictors since our sample size is very large and our overall goal is to measure the varying degrees of relationship between response and predictors. The effect of FULL is statistically significant at the 1% level and indicates that a patient discharged from a full unit is more likely to be readmitted within 72 h. When FULL is 1, it increases the odds by a factor of 2.341. This implies that for a baseline patient of average age (i.e., 46 years), the probability of readmission increases from 10% to 20%.
We observe expected results from the control variables. For example, trauma and transplant patients are significantly more likely to be readmitted compared to the (baseline) general surgery patients. On the other hand, elective patients are less likely to be readmitted pointing to the lesser severity of elected surgeries. We control for a patient’s demographics (age, race and gender). We find that male patients are more likely to be readmitted and that readmissions are significantly higher for black patients.
The second model (Model 2) tests readmission within 72 h, using the continuous utilization variable, BEDS. We regress the readmission variable on the number of beds in use at the time of discharge (BEDS). This model allows us to quantify the effect of each additional occupied bed on the likelihood of readmission, as opposed to the effect of crossing a particular threshold. The hypothesized regression equation is given by:
In this regression, BEDS measures the number of utilized beds at the time the patient was discharged. The results of this model are given in Table 4. The effect of BEDS is positive and significant at the 1% level. This tells us that an increase in utilization at discharge leads to an increased readmission rate. The magnitude of the BEDS coefficient (.00797) is smaller than that of FULL in the previous model (.851) because the range of BEDS is over 100. Each additional bed in use at the time of discharge increases the odds of readmission by a factor of 1.008. Table 5 shows the effect of increasing the number of beds in use at the time of discharge on the odds of readmission, and on the probability that a baseline patient will be readmitted. The probability of readmission is calculated at the mean age of a patient and with all dummy variables set to 0 (i.e., a 46-year-old, white female patient in general surgery).
To further investigate the effect over time, we construct six additional models (all similar to Model 1), with readmission within 5, 10, 15, 20, 25, and 30 days as the dependent variable. For example, if a patient was readmitted after 13 days, the indicator variable would have a value of 0 for 5 and 10 days and a value of 1 for the other day variables. We recorded the magnitude of the coefficient of FULL for each model. In Fig. 3, we show the magnitude of the coefficient of FULL as the definition of readmission changes. The error bars for each point show one standard error above and below each value. The utilization at discharge has the strongest effect on readmission within 72 h, and it slowly diminishes over time. Patients who are discharged too soon are more likely to be readmitted quickly, instead of later in the month.
Next, we were interested in determining the effect when only one surgical line is considered. By isolating the surgical line, we can more precisely measure the effect of utilization. Concentrating on one surgical line only allows us to eliminate any variation between the discharge procedures of different surgical lines, the differences in case severity, and the potential for future complications. The trauma surgery line is one of the largest units in our dataset, and has patients who are similar demographically to the general surgery population at the hospital. The percentage of each racial group is nearly the same as the percentage in the general population. The mean and median ages for trauma patients are both within 1 year of the mean and median ages in the general population, as well. There are 248 patients admitted as inpatients after having trauma surgery. Of those, 18% were readmitted within 72 h. The results are given in Tables 6 and 7.
Table 6 shows that high utilization upon discharge has a statistically significant effect on readmission rates within 72 h. While FULL is statistically significant, its p-value is higher compared to Model 1 (Table 3). The reason is the reduced sample size (since we are only focusing on a single surgical line, the sample size is reduced by 95%), which reduces the power of the test. However, the magnitude of the odds ratio is increased dramatically (from 2.3 in the first model to over 25).Footnote 1 This implies that for a baseline patient (a 46-year-old, white female) the probability of readmission increases by 63% (from 10% to 73%)—compared to an increase of only 10% (10% to 20%) when averaging over all surgical lines (Model 1). The insight from this analysis is that the impact of utilization on readmission changes from one surgical line to another. We observe a much stronger effect for trauma patients because surgeries in this line are typically more severe and, thus, more sensitive to variations in length of stay and thoroughness of treatment. Lower acuity patients might be less sensitive to premature discharge, and, therefore, exhibit less of an increased risk for readmission.
The same conclusions hold when measuring utilization on a continuous scale (BEDS; see Table 7). In fact, we see that the odds ratio of BEDS is 1.027, which is more than three times larger than its effect in Model 2 (which averages over all surgical lines). In other words, regardless of how utilization is measured, increased utilization at the time of discharge increases the readmission rate for trauma surgery patients.
Finally, we use survival analysis to determine what affects the rate at which patients return to the hospital after being discharged. While logistic regression estimates the probability that a patient will be readmitted in a certain time frame, survival analysis models the fraction of patients who have been readmitted over time. In this model, our dependent variable is whether or not the patient was readmitted on a given day. We create one observation for each day, for each patient, until the patient is readmitted, up to 30 days. If the patient is readmitted on that day, the variable is 1, if he/she is not, it is 0. A patient who is readmitted on the 10th day after discharge will have nine observations where the dependent variable is 0. For the 10th observation, the dependent variable will be 1, because the patient was readmitted on that day. We also create 30 dummy variables to account for the baseline hazard on each day (D1, D2, …, D30). DN is 1 on the Nth day after discharge, and 0 otherwise. In the first observation, D1 is 1, and the remaining DN variables are 0. In the 10th observation, D10 is 1, the remaining DN variables are 0. When FULL is 1, the odds that a patient will be readmitted on any given day increase by a factor of 1.32. This means that when a patient was discharged from a highly utilized unit, the patient is readmitted at a higher rate. FULL has a larger effect on the odds of readmission than age, race, or gender. Figure 4 shows the percent of each type of patient who is readmitted as a function of time. Table 8 shows the results of this model.
Patients discharged when the post-operative unit was full are more likely to return the first day, and the gap grows as the month progresses. These results are similar to the logistic regression models, in that patients dismissed from a full unit are more likely to return, and that the effect is observable immediately. In this model, the effect that utilization has on readmission rates is statistically significant throughout the entire month. When compared to the logistic regression models, we see a stronger effect later in the month in this model. The difference between the two models comes from a restriction of the survival analysis model. Survival analysis assumes that the effect of each variable is constant over time. However, by varying the readmission window in the logistic regression models, we can examine how the effect changes over time. The survival analysis model gives the effect of FULL averaged over the entire month. The coefficients on the DN variables are decreasing with time. This means that as the month progresses, patients are less likely to be readmitted. While many readmissions that occur after 72 h are unavoidable, it is still interesting to note that the effect of utilization at time of discharge has a lingering effect on readmission rates that lasts up to 30 days.
4 Limitations
While our results shed new light on hospital readmissions, one should use caution in generalizing from them. Since our data pertain to one particular hospital only, our results don’t immediately generalize to all hospitals. While we suspect that similar phenomena occur at other hospitals, since incentives in other U.S. hospitals are essentially the same, our study can only address one hospital. In addition, we have very little data on patient acuity levels. We only have information on whether or not the surgery was elective or emergency. While this captures some of the variance in patient severity, we cannot control for all aspects of patient acuity levels. Also, we do not have the cause for patient readmission, which would allow us to examine in more depth the effect that ICU utilization has on readmission. We also investigated flexible nonparametric regressions via smoothing splines in order to relax the linearity assumption of our model. However, the results were not distinguishable from the linear approach. One reason for the lack of power of the nonparametric model may be the small sample size; a larger sample size might lead to a more nuanced understanding of the relationship between utilization and readmission rates.
5 Conclusions
In previous work, Anderson et al. [2] showed that the discharge rate of patients in the post-operative unit increased when utilization was high. In this paper, we show that these patients are more likely to be readmitted within 72 h than patients discharged when utilization is lower. This effect prevails regardless of the utilization measurement or the chosen timeframe for readmission. Our results indicate that an additional day of recovery would help some patients who are being discharged when there are few available beds.
The systematic early discharge of patients is problematic because readmissions are costly and could lead to an inefficient use of healthcare resources. In addition, early discharge with readmission is a potential public relations problem for a hospital. We propose four solutions for lowering readmission rates. A first solution is to add more flexibility to the post-operative path for patients. While there is a standard post-operative ICU for each service line, there might be other beds in the hospital that would be able to take a patient and allow the patient to recover more fully. Making it easier to match patients with beds might help to reduce readmission rates. A second solution would be the creation of a discharge checklist with objective criteria. Patients must satisfy the criteria before they can be discharged. This checklist can be used at all times, or only when the unit is operating at high levels of utilization. By standardizing the discharge process, it becomes more likely that each patient is fully ready to be transitioned out of the hospital at the time of discharge. Third, the hospital might consider using transition coaches, especially for patients at high risk of readmission. Hiring social workers to check on patients and to coach them on treatment and rehabilitation has been shown to lower the readmission rate (Coleman et al. [5]). A fourth solution would be to align a surgeon’s compensation with a patient’s health outcome. Currently, surgeons are paid for performing surgeries and having high operating room utilizations. By incorporating readmission rate into the compensation formula, we might impact the discharge decision process in a way that would lower the readmission rate.
Our work has identified a class of patients for whom the readmission rate is shown to be demonstrably higher. Patients discharged from a highly utilized unit are more likely to be readmitted to the hospital after surgery. Because the discharge rate increases when utilization is high, extra time in the post-operative unit for these patients might help lower the probability that they are readmitted.
In future work, we plan to address questions on the total length of stay for each type of patient. For example, do patients who are discharged from a highly utilized unit come back and stay longer than those who are discharged under normal circumstances? What effect do these early discharges and extra readmissions have on the overall efficiency of the hospital? In terms of throughput, there is a tradeoff to be considered when deciding to discharge a patient a day early. By discharging a patient early, a bed is freed up to allow a surgery to be performed. However, this discharged patient is now more likely to be readmitted. If the patient comes back, he/she might cause future surgeries to be postponed. There is a delicate tradeoff between rushing to discharge patients, which comes with the risk of higher readmission rates, and taking the time to treat patients fully in order to lower future readmission rates.
Notes
Note that the confidence interval is very wide (1.085, 594.979). The decrease in sample size, combined with the dichotomization of a continuous variable, leads to larger standard errors, and, hence, less precision in the confidence interval.
References
Akaike H (1974) A new look at the statistical model identification. IEEE Trans Autom Control 19:716–723
Anderson D, Golden B, Jank W, Price C, Wasil E (2011) Examining the discharge practices of surgeons at a large medical center. Health Care Management Science (Forthcoming)
Bohmer RMJ, Newell J, Torchiana DF (2002) The effect of decreasing length of stay on hospital discharge destination and readmission after coronary bypass operation. Surgery 132:10–11
Campbell AJ, Cook JA, Adey G, Cuthbertson BH (2008) Predicting death and readmission after intensive care discharge. Br J Anaesth 100:656–662
Coleman EA, Parry C, Chalmers S, Min SJ (2006) The care transitions intervention: results of a randomized controlled trial. Arch Intern Med 166:1822–1828
Cowper PA, DeLong ER, Hannan EL, Muhlbaier LH, Lytle BL, Jones RH, Holman WL, Pokorny JJ, Stafford JA, Mark DB, Peterson ED (2007) Is early too early? Effect of shorter stays after bypass surgery. Ann Thorac Surg 83:100–107
Delaney CP, Fazio VW, Senagore AJ, Robinson B, Halverson AL, Remzi FH (2001) ‘Fast track’ postoperative management protocol for patients with high co-morbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg 88:1533–1538
Dobson G, Lee H-H, Pinker E (2011) A model of ICU bumping. Working Paper. University of Rochester
Goodney PP, Stukel TA, Lucas FL, Finlayson EV, Birkmeyer JD (2003) Hospital volume, length of stay, and readmission rates in high-risk surgery. Ann Surg 238:161–167
Hannan EL, Racz MJ, Walford G et al (2003) Predictors of readmission for complications of coronary artery bypass graft surgery. JAMA 290(6):773–780
Hasan M (2001) Readmission of patients to hospital: still ill-defined and poorly understood. Int J Qual Health Care 13:177–179
Hwang SW, Li J, Gupta R, Chien V, Martin RE (2003) What happens to patients who leave hospital against medical advice? Can Med Assoc J 168:417–420
Niehaus D, Koen L, Galal U, Dhansay K, Oosthuizen P, Emsley R, Jordan E (2008) Crisis discharges and readmission risk in acute psychiatric male inpatients. BMC Psychiatry 1:8–44
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderson, D., Golden, B., Jank, W. et al. The impact of hospital utilization on patient readmission rate. Health Care Manag Sci 15, 29–36 (2012). https://doi.org/10.1007/s10729-011-9178-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10729-011-9178-3