Abstract
Multiple endocrine neoplasia type 2A (MEN2A) may be rarely associated with cutaneous lichen amyloidosis (CLA), a skin lesion located in the interescapular region. Here, we describe 3 MEN2A-related CLA kindred and perform a systematic review (SR) of the literature on clinical, biochemical and molecular characteristics of MEN2A-related CLA patients. Thirty-eight patients with MEN2A-related CLA followed at our institution were evaluated. The median age at MEN2A diagnosis in our cohort was 25 (13–41) years, 68 % were women and all harbored codon 634 RET mutations. The literature search resulted in 20 publications that contributed with 25 MEN2A families and 214 individuals. The mean age of MEN2A diagnosis was 31 ± 17 years, with 77 % women. The mean age reported by patients to initial skin lesion suggestive to CLA was 20 ± 13 years. All but two kindred harbored mutations at codon 634: C634R 7 kindred (35 %), C634Y 5 kindred (25 %), C634W 3 kindred (15 %), C634G 1 kindred (5 %), V804M 1 kindred (5 %) and S891A 1 kindred (5 %). Most interesting, the standardized CLA prevalence was higher in women (2.3/1.0, P < 0.005). The overall reported prevalence of medullary thyroid carcinoma, CLA, pheochromocytoma and hyperparathyroidism was 94, 51, 30 and 16 %, respectively. SR of literature indicates that MEN2A-related CLA is more frequent in women and presents a high penetrance, being the second most frequent manifestation of the syndrome, preceded only by MTC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medullary thyroid carcinoma (MTC) is a rare calcitonin-producing tumor of the parafollicular or C cells of the thyroid gland. It accounts for 4 % of all thyroid cancers and may occur sporadically or as a manifestation of an autosomal-dominant inherited syndrome, multiple endocrine neoplasia type 2 (MEN2) [1].
The MEN2 syndrome includes two clinically distinct forms: MEN type 2A (MEN2A) and MEN type 2B (MEN2B). MEN2A accounts for over 95 % of MEN2 cases and includes classical MEN2A, familial MTC (FMTC), MEN2A with CLA, and MEN2A with Hirschsprung’s disease (HD) [2]. Classical MEN2A is characterized by presence of MTC in 95 % of cases, unilateral or bilateral PHEO in 30–50 %, and primary hyperparathyroidism (HPT) in 20–30 %. In patients with FMTC, only the thyroid is affected. MEN2B syndrome presents a specific phenotype that includes/encompasses MTC, PHEO, ganglioneuromas of the digestive tract, mucosal neuromas, and/or skeletal abnormalities. MTC is the first neoplasic manifestation in the vast majority of MEN2 patients [3, 4]. Germline mutations in the RET (REarranged during Transfection) proto-oncogene, which result in a constitutive activation of the transmembrane tyrosine kinase receptor, are responsible for MEN2 phenotype [5]. The most frequent RET mutations in MEN2A occur in codons 609, 611, 618, or 620 (exon 10) or codon 634 (exon 11) [2, 6, 7]. Currently, the molecular testing for the RET proto-oncogene has become widely available and composes the basis for MTC screening strategies [8–10].
MEN2A is rarely associated with cutaneous lichen amyloidosis (CLA), a rare skin condition usually located in the interescapular region or on the extensor surfaces of the extremities, and described as pruritic, scaly, papular, and pigmented [11–13]. The CLA is characterized by deposits of amorphous amyloid-like material immediately beneath and in contiguity with the dermoepidermal junction. The amyloids are the result of filamentous degeneration of cells. In the cutaneous amyloidosis, the keratinocytes degenerate and/or show apoptosis. Large areas of filamentous degeneration continuously connected to dermal islands of amyloid have been observed, displaying the point of cascade like steps at molecular level resulting in amyloid formation and deposition. The pruritus improves with sun exposure and worsens during periods of stress. The cutaneous manifestations are the consequence of repeated scratching of the pruritic zone. This causes epidermal hyperplasia, pigmentation and damages the keratinocytes which then undergo apoptosis. The residues derived from cell damage are deposited in the upper dermis as amyloid. CLA hereditary forms are a rare autosomal dominant diseases, a sporadic variety of this lesion is more frequently observed [14–16]. Interestingly, MEN2A-related CLA and familial CLA seem to be distinct diseases. The reason why only a small percentage of MEN2A kindred develop this manifestation is still unknown.
Despite the fact that the association of CLA with MEN2A has long been established, a comprehensive clinical and oncologic characterization of the MEN2A-related CLA kindred has not yet been done. Thus, the aim of this study is to describe 3 kindred with MEN2A syndrome, and to perform a systematic literature review (SR) of clinical, biochemical and molecular features about the MEN2A-related CLA.
Materials and methods
Our cohort
Patients
From a cohort of MTC patients attending the Thyroid Outpatient Clinic of the Endocrine Division of Hospital de Clínicas de Porto Alegre (HCPA), a tertiary care, university-teaching hospital in southern Brazil, a large family and 2 other kindred with MEN2A-related CLA were selected for this study.
All patients with MEN2A underwent a complete clinical examination and laboratorial evaluation following the current MTC guidelines [4, 9]. The data collected for each individual included the clinical and oncological features of family members (association of other endocrine neoplasias), the type of RET mutations, and information on atypical features noted, such as HD or CLA. The family relatives of each index cases were evaluated by screening of RET mutation.
Total thyroidectomy was performed in all patients with varying cervical neck dissection procedures. The diagnosis of lymph node metastases was based on histological examination. Patients with suspicious distant metastases (i.e. the presence of local metastases and/or serum calcitonin >150 pg/ml) underwent imaging exams [cervical, thoracic and abdomen CT (or liver magnetic resonance imaging), and bone scintigraphy]. Patients with undetectable calcitonin levels were considered free of disease. Patients with PHEO or HPT underwent specific surgery. Tumor staging was performed according to the current International Union against Cancer TNM classification [17].
Laboratory tests were performed at baseline and every 3–6 months thereafter. Levels of basal calcitonin [Until December 2003, Calcitonin IRMA-DSL7700, Diagnostic Systems Laboratories, Inc., Webster, TX, USA, reference range <10 pg/ml and, after January 2004, Immulite 2000, Diagnostic Products Corporation, Los Angeles, CA, USA; reference value (RV) male <12.0 pg/ml and female <6.0 pg/ml], plasma parathyroid hormone (PTH; Immulite 2000 Intact PTH, Diagnostic Products), urinary fractionated metanephrines (HPLC). Whenever indicated, diagnostic imaging investigation [cervical ultrasonography, thorax and abdominal computed tomography (CT)] was performed. Selected patients were submitted to whole-body metaiodobenzylguanidine scintigraphy to rule out PHEO and/or distant metastases.
This study has been approved by the institutional Ethics Committee and all patients and/or their legal guardians had given written consent.
Genetic screening analysis
Genomic DNA was prepared from peripheral blood leukocytes by standard procedures. RET exons 8, 11, 13, 14, 15 and 16 were analyzed. Oligonucleotide primers for amplification of different RET exons were as following: 8(5′AGCTGGTGCTGTTCCCTGTCC3′/5′CCACCGGTGCCATCGCCCCT3′) 10(5′TTGCGACACCAGTTGGGGAG3′/5′CAGCAATTTCCTCCCTTGTTG3′), 11(5′GAGCCATGAGGCAGAGCATA3′/5′CCCTCACCAGGATCTTGAAGG3′), 13(5′TGAACTTGGGCAAGGCGATG3′/5′GGGAGAACAGGGCTGTATGGAG3′), 14(5′AAGACCCAAGCTGCCTGAC3′/5′GCTGGGTGCAGAGCCATAT3′), 15(5′CTCTGCTGGTCACACCAGGC3′/5′GGTATCTTTCCTAGGCTTCCC3′) and 16(5′AGGGATAGGGCCTGGG*CTTC3′/5′TAACCTCCACCCCAAGAGAG3′). PCRs were run in a final volume of 50ul, using 300–500 ng of genomic DNA, 1.5 mM MgCl2, 0.2 mM dNTPs, 0.2 mM of each primer, and 2.5U Platinum Taq DNA Polymerase (Ludwig Biotec, Porto Alegre, RS, Brazil). Genomic DNA was denatured for 5 min at 94 °C before 35 cycles at 94 °C 30 s, 60 °C 30 s, and 72 °C 30 s, followed by a 5 min 72 °C step in a programmable thermal controller (MJ Research, Inc., Waltham, MA).
For sequencing, PCR products were purified using the GFX PCR DNA purification kit (GE Healthcare, Buckinghamshire, UK), and submitted to direct sequencing using the Big Dye™ Terminator Cycle Sequencing Ready Reaction Kit (Applied Biosystems, Foster City, CA, USA).
Pedigrees analysis
The families pedigrees design on the version 8 of Progeny© (1996–2013 Progeny Software LLC, Delray Beach, Florida, USA), a Genetic Pedigree Software.
Dermatopathological study and pathological examination
Biopsy specimens were obtained from the cutaneous lesions of some patients presenting skin abnormalities suggestive of CLA. The biopsy material was fixed in 10 % formalin and stained with hematoxylin and eosin, crystal violet, and congo red and then observed in light microscopy by a pathologist.
Immunohistochemistry analysis
Immunohistochemistry analysis (IHC) was performed on thin sections. (3 μm) of previously formalin-fixed and paraffin-embedded tissues. The antibodies used were polyclonal rabbit anti-human calcitonin (229A-16, CellMarque, Rocklin, CA, USA) and monoclonal rabbit anti-human RET (ab134100; Abcam Inc., Cambridge, MA, USA), Sections representing CLA were submitted to routine immunohistochemical technique, which comprises deparaffination and rehydration, antigenic recovery, inactivation of endogenous peroxidase, and blockage of unspecific reactions. Primary antibodies were incubated overnight at a temperature of 4 °C, at dilutions of 1:400 followed by application of streptavidin horseradish peroxidase conjugate (LSAB; DakoCytomation, Via Real Carpinteria, CA, USA), and diaminobenzidine tetrahydrochloride (Kit DAB; DakoCytomation). Absence of the primary antibody was used as a negative control.
Statistical analysis
Results are expressed as frequencies, mean ± SD, median (IQ 25–75) unless otherwise specified. Baseline characteristics were compared using x 2 tests or Fisher’s exact test for qualitative variables. Quantitative variables were compared between groups using Student’s t test or Mann–Whitney tests. Hardy–Weinberg equilibrium for each polymorphism was assessed by x 2 tests.
Systematic literature review
We performed a SR about MEN2A-related CLA. Relevant articles were identified by searching the electronic databases EMBASE and MEDLINE, in June 2015, using the search terms “Amyloidosis, Familial Cutaneous Lichen” AND “Multiple Endocrine Neoplasia Type 2A”, with no additional filters. The reference list of all identified articles was searched for additional studies on the subject. Study eligibility was double assessed by Scapineli JO and Dora JM, with all data abstracted in a standardized abstraction form.
Results
Patients
From a cohort of 337 MTC patients followed at our institution, 179 (40 kindred) have the hereditary form of disease (MEN2). Out of them, 3 kindred have MEN2A-related CLA. The clinical and biochemical features of the 38 patients of the 3 affected kindred with MEN2A-related CLA are summarized in Table 1. The mean age at MEN2A diagnosis was 25 (13–41) years, 68 % (26/38) were women and all patients had codon 634 RET mutations [1 family C634Y (33 %) with 30 patients (78.9 %); 1 family C634W (33 %) with 6 patients (15.8 %); 1 family C634R (33 %) with 2 patients (5.3 %)]. CLA was found in 50 % (18/36) of the patients. Information was missing for 2 individuals.
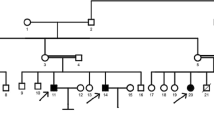
The overall reported prevalence of PHEO and HPT was 31 and 19 %, respectively. The median basal pre-operative levels of serum calcitonin and CEA were 251 pg/ml (35–1113) and 6.0 ng/ml (1.8–44.6), respectively. The median tumor size was 1.0 cm (1.0–2.8). Twelve patients (36 %) presented lymph node and 3 (9 %) distant metastases at diagnosis. The median follow-up period was 10 years (9–11). The pedigrees of these families are briefly described below and shown in Fig. 1.
Family 1A
Patients developed MTC, 6 PHEO (II-5, III-3, III-10, III-16, III-22 and IV-20) and 6 HPT (II-9, III-9, III-16, III-21, IV-1 and IV-20). CLA was present in 14 individuals (50 %). Follow-up data of 2 patients (I-4 and II-4) are missing.
Family 2A
Five patients had MTC while one gene carrier presented C cell hyperplasia (IV-1). Two patients presented PHEO (III-5 and III-7) and none HPT. CLA was present in 2 patients of this family (III-5 and III-7).
Family 3A
Two patients developed MTC and CLA (II-2 and III-1) and one of them also developed PHEO (III-1).
There was no significant differences between patients with or without CLA, regarding the tumor size [1.7 (1.0–3.0) vs 1.0 (1.0–2.0), P = 0.38], presence of lymph node [7 (41 %) vs 4 (27 %), P = 0.39] or distant metastases [2 (12 %) vs 0 (0 %), P = 0.48] and basal calcitonin levels [930 (35–2215) vs 118 (31–491), P = 0.12] (Table 1).
The frequency of CLA was 50 % (13/26) in women and 41.6 % (5/12) in men, resulting in a standardized CLA prevalence in women/men (1.2/1.0, P = 0.87).
There were no differences in the frequency of most common RET polymorphisms: G691S/S904S [4 (66.7 %) vs. 2 (33.3 %), P = 0.83], L769L [6 (54.5 %) vs. 5 (45.5 %), P = 1.00] and S836S [2 (66.7 %) vs. 1 (33.3 %), P = 1.00] in patients with or without CLA, respectively.
CLA manifestations
All patients had clinical and physical examination to CLA. Eighteen subjects who presented with physical signs compatible with CLA (pruritic and maculopapular skin lesion, either unilaterally or bilaterally) were considered as presenting clinical disease. Interestingly, all but 3 patients (15/18, 83 %) already presented the CLA lesion at MEN2A diagnosis. CLA was observed at the interescapular region, with pruritus being the initial manifestation, usually appearing 11 ± 10 years before the diagnostic of the first neoplasia.
Eight patients with CLA clinical manifestations underwent skin biopsy. The diagnosis was confirmed in all of them. The histologic pattern demonstrated characteristic features of the disorder, including mild acanthosis, hyperkeratosis and hyperpigmentation of basal keratinocytes, elongation of the rete ridges. There were amorphous material eosinophilic deposits within the superficial papillary dermis, immediately beneath the dermal–epidermal junction, and numerous scattered melanophages. The exam also revealed small globular deposits of amyloid in the papillary dermis (Fig. 2). Immunohistochemical analysis showed no expression of RET or calcitonin in the CLA tissue (results not shown).
Light microscopy of a cutaneous lesion biopsy. a First skin biopsy ×100 magnification portrays light hyperkeratosis, acanthosis and hyperpigmentation of basal keratinocytes, elongation of the rete ridges. Within the superficial papillary dermis, immediately beneath the dermal–epidermal junction, there were amorphous material eosinophilic deposits. There were also numerous scattered melanophages. b Second biopsy ×200 magnification, stained with hematoxylin and eosin, revealing small globular deposits of amyloid in the papillary dermis (arrow)
Systematic literature review
All publications about MEN2A with patient data on RET proto-oncogene mutation and CLA were considered for inclusion. All data were independently abstracted in duplicate, using a standardized abstraction form.
A total of 31 potentially relevant articles were retrieved from MEDLINE and EMBASE databases. Seven references were duplicates. Thus, 24 articles were identified using our search strategy. Nine articles were excluded because lack of data (clinical, biochemical and molecular characteristics) on MEN2A-related CLA. Five additional articles were identified by review of references, resulting in 20 papers that contributed to our SR (Fig. 3).
The SR comprised data of 214 MEN2A patients, 108 (51 %) with skin manifestations characteristics of CLA. The mean age at MEN2A diagnosis was 31 ± 17 years and 77 % (55/71) were women. The mean age reported by patients to initial skin lesion suggestive to CLA was 20 ± 13 years. The frequency of CLA was higher in women than in men [51 % (51/100) vs. 22 % (14/64)], with a standardized CLA prevalence in women/men of 2.3/1.0 (P < 0.005; Table 2).
All but 2 kindred harbored mutations at codon 634 (23 out of 25; 92 %): C634R 7 (35 %), C634Y 5 (25 %), C634W 3 (15 %), C634G 1 (5 %). The information about the amino acid substitutions at codon 634 was missing for 2 kindred. One kindred harbor the V804 M RET mutation and other the S891A mutation. CLA was the second most frequent manifestation of the syndrome (51 %), preceded only by MTC (94 %). PHEO and HPT were diagnosed in 30 and 16 % of the MEN2A patients, respectively.
Interestingly, patients with MEN2A-related CLA were older [34 (20–47) vs 23 (13–40); P = 0.024] and have higher basal preoperative serum calcitonin levels [883 (43–1723) vs 58 (28–438); P = 0.032] as compared to those without CLA, respectively. The analysis of disease status was precluded because data about metastatic disease was missing in the majority of the studies.
Discussion and conclusion
In this study we present a comprehensive clinical, biochemical and molecular characterization of the MEN2A-related CLA and a systematic literature review comprising 25 MEN2A families and 108 CLA individuals.
Lichen amyloidosis is the most common form of primary localized cutaneous amyloidosis. It is a cutaneous type of amyloidosis that is not associated with systemic amyloidosis but may be associated with other systemic conditions such as systemic lupus erythromatosis, Sjögren’s Syndrome, dermatomyositis, primary biliary cirrhosis and scleroderma [18]. Although LCA is sporadic in the vast majority of cases, some individuals do show evidence for genetic susceptibility and up to 10 % of individuals may have an autosomal dominant family history [19].
MEN2A-related CLA was first described by Gagel et al. [11]. The distribution of the skin lesions in all reported cases of MEN2A-related CLA was restricted to the interescapular area and pruritus can pre-date the development of MTC in years, usually during childhood [11, 20, 21]. In MEN2A-related CLA, amyloid deposition secondary to repeated scratching triggers the inflammatory response—a phenomenon not related to calcitonin deposition. This results in epidermal hyperplasia, pigmentation and damages the keratinocytes which then undergo apoptosis. The residues derived from cell damage are deposited in the upper dermis as amyloid. The rash occurs in the area of repeated scratching and is located in the upper back at either or both interscapular regions. MEN2A-related CLA is a phenotypic marker for members of the MEN 2A families. Symptomatic patients may be treated with topical Capsaicin 0.025 %, an agent known to release neuropeptides from C-fibres and prevent their deposition. Some patients refer amelioration of itching during treatment, but the symptoms usually return after cessation of therapy [22]. In our cohort, 83 % (15/18) of the patients already presented the CLA lesion at MTC diagnosis, with pruritus being the initial manifestation, present in an average of 11 years before MEN2A diagnosis. The overall prevalence of MTC, CLA, PHEO and HPT in our population was 97, 50, 31 and 19 %, respectively. Similarly, data from our SR displayed prevalence for MTC, CLA, PHEO, and HPT of 94, 51, 30, and 16 %, respectively.
The MEN2A-related occurs almost exclusively in patients with C634 RET mutation, it has been estimated that more than 30 % of patients with C634 mutation will develop CLA during their lifetime [23]. In our cohort, all cases of MEN2A-related CLA harbor RET mutations at codon 634. In accordance, the SR shows that the most common mutations in MEN2A-related CLA occur in codon 634, with the C634R mutation being the most prevalent (7 kindred, 35 %). Rothberg et al. [24] reported a patient with CLA not associated with mutation in codon 634. This case report a single patient with a novel genotype–phenotype relationship involved V804M mutation and MEN2A-related CLA. Recently, Qi et al. [25] reported a kindred (3 patients) with MEN2A-related CLA associated to S891A/G513D mutations.
The genetic basis for MEN2A-related CLA remains obscure as well as the reason why just only a small percentage of kindred develop this manifestation. It has been suggested that the primary cause is neurogenic and the skin lesions are a secondary phenomenon due to chronic pruritus and repeated scratching [20, 26]. The mechanism by which these mutations induce CLA may be related to and effect in the peripheral nervous system development, since the RET gene is expressed in this tissue during embryogenesis [15]. Gagel et al. [11] proposed that the lack of a demonstrable skin lesion in some kindred of MEN2A could be explained by a delayed onset of the skin lesion or incomplete penetrance. However, post embryogenesis, RET expression has been demonstrated in cells derived from the neural crest: thyroid parafollicular cells, parathyroid cells, chromaffin cells of the adrenal medulla and enteric autonomic plexus. [27]. Of interest, different activated sites of the RET can trigger several signaling pathways (RAS/MEK/ERK and PI3K/AKT/mTOR) that regulate cell survival, differentiation, proliferation, and chemotaxis in thyroid carcinoma [28, 29]. The fact of the majority of patients with MEN2A-related CLA have mutations at codon 634 suggests an involvement of this specific cysteine residue in both disorders, which may imply the possibility of additional mechanisms in the pathogenesis of the MEN2A-related CLA syndrome [30]. Another explanation could be the interaction of apparently benign polymorphism and a mutation in the disease causing gene modifying disease phenotype. However, extensive search for co-segregation of several common synonymous nucleotide changes in the RET gene sequence with MEN2A-related CLA phenotype has failed to demonstrate this association [16, 31].
In our population, no differences between patients with or without CLA were found in the frequency of RET G691S/S904S, L769L and S836S polymorphisms. Indeed, the possible association between LCA and the RET gene was previously addressed by genetic linkage studies focused on the RET locus on chromosome 10, but no linkage was demonstrated in Chinese kindred [32]. Further evaluations by genome wide association studies (GWAS) might help clarify this intriguing disorder.
One interesting and unexpected finding of this study was the higher prevalence of MEN2A-related CLA in women. In the SR we show that the frequency of CLA was 77 % in women contrasting with only 23 % in men, resulting in a standardized CLA prevalence of 2.3/1.0 in women/men (P < 0.005). To date, we found no explanation for this intriguing observation.
In summary, we show that all but two reported cases of MEN2A-related CLA harbored RET codon 634 mutations. Moreover, MEN2A-related CLA presents a high penetrance, being the second most frequent manifestation of the syndrome, preceded only by MTC. These observations indicate that CLA could be an early marker of MEN2A, especially in women, and that clinicians should be aware of this finding, particularly in patients with thyroid nodules or family history of thyroid carcinoma.
References
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295(18):2164–2167. doi:10.1001/jama.295.18.2164
Wells SA Jr, Asa SL, Dralle H et al (2015) Revised american thyroid association guidelines for the management of medullary thyroid carcinoma. Thyroid Off J Am Thyroid Assoc 25(6):567–610. doi:10.1089/thy.2014.0335
Wells SA Jr, Pacini F, Robinson BG, Santoro M (2013) Multiple endocrine neoplasia type 2 and familial medullary thyroid carcinoma: an update. J Clin Endocrinol Metab 98(8):3149–3164. doi:10.1210/jc.2013-1204
Maia AL, Siqueira DR, Kulcsar MA, Tincani AJ, Mazeto GM, Maciel LM (2014) Diagnosis, treatment, and follow-up of medullary thyroid carcinoma: recommendations by the Thyroid Department of the Brazilian Society of Endocrinology and Metabolism. Arquivos brasileiros de endocrinologia e metabologia 58(7):667–700
Mathew CG, Chin KS, Easton DF et al (1987) A linked genetic marker for multiple endocrine neoplasia type 2A on chromosome 10. Nature 328(6130):527–528. doi:10.1038/328527a0
Donis-Keller H, Dou S, Chi D et al (1993) Mutations in the RET proto-oncogene are associated with MEN 2A and FMTC. Hum Mol Genet 2(7):851–856
Mulligan LM, Kwok JB, Healey CS et al (1993) Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature 363(6428):458–460. doi:10.1038/363458a0
Punales MK, Graf H, Gross JL, Maia AL (2003) RET codon 634 mutations in multiple endocrine neoplasia type 2: variable clinical features and clinical outcome. J Clin Endocrinol Metab 88(6):2644–2649. doi:10.1210/jc.2002-021422
Wells SA Jr, Asa SL, Dralle H et al (2015) Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 25(6):567–610. doi:10.1089/thy.2014.0335
Maia AL, Gross JL, Puñales MK (2005) Neoplasia Endócrina Múltipla Tipo 2. Arq Bras Endocrinol Metab 49(5):725–734. doi:10.1590/S0004-27302005000500013
Gagel RF, Levy ML, Donovan DT, Alford BR, Wheeler T, Tschen JA (1989) Multiple endocrine neoplasia type 2a associated with cutaneous lichen amyloidosis. Ann Intern Med 111(10):802–806
Kousseff BG, Espinoza C, Zamore GA (1991) Sipple syndrome with lichen amyloidosis as a paracrinopathy: pleiotropy, heterogeneity, or a continuous gene? J Am Acad Dermatol 25:651–657
de Groot JWB, Links TP, Plukker JTM, Lips CJM, Hofstra RMW (2006) RET as a diagnostic and therapeutic target in sporadic and hereditary Endocrine tumors. Endocr Rev 27(5):535–560. doi:10.1210/er.2006-0017
Ferrer JP, Halperin I, Conget JI et al (1991) Primary localized cutaneous amyloidosis and familial medullary thyroid carcinoma. Clin Endocrinol 34(6):435–439
Lemos MC, Carrilho F, Rodrigues FJ, Carvalheiro M, Regateiro FJ, Ruas MMA (2003) Caracterização Molecular de uma Família com NEM2A e suas Implicações Clínicas. Acta Méd Port 16:245–250
Gullu S, Gursoy A, Erdogan MF, Dizbaysak S, Erdogan G, Kamel N (2005) Multiple endocrine neoplasia type 2A/localized cutaneous lichen amyloidosis associated with malignant pheochromocytoma and ganglioneuroma. J Endocrinol Invest 28(8):734–737
Osada D, Viegas SF, Shah MA, Morris RP, Patterson RM (2003) Comparison of different distal radius dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg 28(1):94–104. doi:10.1053/jhsu.2003.50016
Tanaka A, Arita K, Lai-Cheong JE, Palisson F, Hide M, McGrath JA (2009) New insight into mechanisms of pruritus from molecular studies on familial primary localized cutaneous amyloidosis. Br J Dermatol 161(6):1217–1224. doi:10.1111/j.1365-2133.2009.09311.x
Breathnach SM (1988) Amyloid and amyloidosis. J Am Acad Dermatol 18(1 Pt 1):1–16
Pacini F, Fugazzola L, Bevilacqua G, Viacava P, Nardini V, Martino E (1993) Multiple endocrine neoplasia type 2A and cutaneous lichen amyloidosis: description of a new family. J Endocrinol Invest 16(4):295–296
Verga U, Fugazzola L, Cambiaghi S et al (2003) Frequent association between MEN 2A and cutaneous lichen amyloidosis. Clin Endocrinol 59(2):156–161
Hong J, Buddenkotte J, Berger TG, Steinhoff M (2011) Management of itch in atopic dermatitis. Semin Cutan Med Surg 30(2):71–86. doi:10.1016/j.sder.2011.05.002
Singh DN, Gupta S, Agarwal A (2012) Cutaneous lichen amyloidosis associated with multiple endocrine neoplasia type 2A: an early clinical marker. World J Endocr Surg 4(1):41. doi:10.5005/jp-journals-10002-1092
Rothberg AE, Raymond VM, Gruber SB, Sisson J (2009) Familial medullary thyroid carcinoma associated with cutaneous lichen amyloidosis. Thyroid Off J Am Thyroid Assoc 19(6):651–655. doi:10.1089/thy.2009.0021
Qi XP, Zhao JQ, Chen ZG et al (2015) RET mutation p.S891A in a Chinese family with familial medullary thyroid carcinoma and associated cutaneous amyloidosis binding OSMR variant p.G513D. Oncotarget 6(32):33993–34003. doi:10.18632/oncotarget.499
Robinson MF, Furst EJ, Nunziata V et al (1992) Characterization of the clinical features of five families with hereditary primary cutaneous lichen amyloidosis and multiple endocrine neoplasia type 2. Henry Ford Hosp Med J 40(3–4):249–252
Takahashi M, Asai N, Iwashita T, Isomura T, Miyazaki K, Matsuyama M (1993) Characterization of the ret proto-oncogene products expressed in mouse L cells. Oncogene 8(11):2925–2929
Lin SF, Huang YY, Lin JD, Chou TC, Hsueh C, Wong RJ (2012) Utility of a PI3K/mTOR inhibitor (NVP-BEZ235) for thyroid cancer therapy. PLoS One 7(10):e46726. doi:10.1371/journal.pone.0046726
Tamburrino A, Molinolo AA, Salerno P et al (2012) Activation of the mTOR pathway in primary medullary thyroid carcinoma and lymph node metastases. Clin Cancer Res 18(13):3532–3540. doi:10.1158/1078-0432.CCR-11-2700
Seri M, Celli I, Betsos N, Claudiani F, Camera G, Romeo G (1997) A Cys634Gly substitution of the RET proto-oncogene in a family with recurrence of multiple endocrine neoplasia type 2A and cutaneous lichen amyloidosis. Clin Genet 51(2):86–90
Hofstra RM, Sijmons RH, Stelwagen T et al (1996) RET mutation screening in familial cutaneous lichen amyloidosis and in skin amyloidosis associated with multiple endocrine neoplasia. J Invest Dermatol 107(2):215–218
Lee DD, Huang JY, Wong CK, Gagel RF, Tsai SF (1996) Genetic heterogeneity of familial primary cutaneous amyloidosis: lack of evidence for linkage with the chromosome 10 pericentromeric region in Chinese families. J Invest Dermatol 107(1):30–33
Birla S, Singla R, Sharma A, Tandon N (2014) Rare manifestation of multiple endocrine neoplasia type 2A & cutaneous lichen amyloidosis in a family with RET gene mutation. Indian J Med Res 139(5):779–781
Abdullah F, Udelsman R (2004) Cutaneous lichen amyloidosis in a family with familial medullary thyroid cancer. Surgery 135(5):563–564. doi:10.1016/S0039
Vieira AE, Mello MP, Elias LL et al (2002) Molecular and biochemical screening for the diagnosis and management of medullary thyroid carcinoma in multiple endocrine neoplasia type 2A. Horm Metab Res 34(4):202–206. doi:10.1055/s-2002-26712
Karga HJ, Karayianni MK, Linos DA, Tseleni SC, Karaiskos KD, Papapetrou PD (1998) Germ line mutation analysis in families with multiple endocrine neoplasia type 2A or familial medullary thyroid carcinoma. Eur J Endocrinol 139(4):410–415
Ceccherini I, Romei C, Barone V et al (1994) Identification of the Cys634– > Tyr mutation of the RET proto-oncogene in a pedigree with multiple endocrine neoplasia type 2A and localized cutaneous lichen amyloidosis. J Endocrinol Invest 17(3):201–204
Nunziata V, Giannattasio R, Di Giovanni G, D’Armiento MR, Mancini M (1989) Hereditary localized pruritus in affected members of a kindred with multiple endocrine neoplasia type 2A (Sipple’s syndrome). Clin Endocrinol 30(1):57–63
Donovan DT, Levy ML, Furst EJ et al (1989) Familial cutaneous lichen amyloidosis in association with multiple endocrine neoplasia type 2A: a new variant. Henry Ford Hosp Med J 37(3–4):147–150
Acknowledgments
This work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundacão de Amparo Pesquisa do Estado do Rio Grande do Sul (FAPERGS) and Fundo de Incentivo à Pesquisa do Hospital de Clínicas de Porto Alegre (FIPE).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests exist that could be perceived as prejudicing the impartiality of the research reported.
Additional information
Jessica Oliboni Scapineli and Lucieli Ceolin have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Scapineli, J.O., Ceolin, L., Puñales, M.K. et al. MEN 2A-related cutaneous lichen amyloidosis: report of three kindred and systematic literature review of clinical, biochemical and molecular characteristics. Familial Cancer 15, 625–633 (2016). https://doi.org/10.1007/s10689-016-9892-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-016-9892-6