Abstract
An increasing demand for genetic testing has moved the procedure from highly selected at-risk individuals, now also including cancer patients for treatment associated testing. The heritable fraction of ovarian cancer is more than 10 %, and our department has offered BRCA testing to such patients irrespective of family history since 2002. This study examined potential psychosocial distress associated with this procedure using The Multidimensional Impact of Cancer Risk Assessment (MICRA) questionnaire and other patient-rated generic distress instruments. Patients were divided into four groups according to cancer risk: mutation carriers, own history of breast cancer and ovarian cancer, family history of breast cancer and/or ovarian cancer, and patients without family history. In a postal survey, 354 patients responded. Good acceptance of the MICRA was observed, and previously described good psychometric properties were confirmed. A significant association between MICRA total score and receiving a positive BRCA test result was found. No significant between-group differences were observed with generic distress instruments. Time since cancer diagnosis, test result, and survey showed no significant associations with MICRA scores. Internal consistencies of instruments were adequate. Exploratory and confirmatory factor analyses showed adequate fit indices for a three factor solution of the MICRA, but further refinement of the items should be considered. In conclusion, the specific types of worry and distress most relevant to receiving genetic testing irrespective of family history were not captured by the generic distress instruments. The MICRA was supported as a useful tool for detection of mental distress related to genetic testing and risk evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 10 % of ovarian cancer (OC) cases are due to hereditary predisposition, and the high carrier frequency makes genetic testing for BRCA mutations in OC patients an efficient way to identify mutation carriers and their families, as well as identifying those who will benefit of BRCA associated targeted cancer treatment. Genetic testing can confirm, disconfirm or leave the individual’s carrier status inconclusive. The risk of OC is on average 39–40 % in BRCA1 mutation carriers and 11–18 % in BRCA2 mutation carriers [1, 2]. The corresponding risk of breast cancer (BC) in BRCA1 mutation carriers is on average 57–65 % and for BRCA2 mutation carriers 45–49 %. Thus knowledge of BRCA carrier status may be a personal burden, as well as it is valuable for risk assessment and cancer prevention in the individual and in healthy family members at risk.
From the start of genetic testing, experts in the field have feared that the procedure should trigger mental distress in the cancer patients, and particularly so in healthy women receiving confirmation of BRCA carrier status with all its personal and familial mental and physical consequences. Mental distress was initially examined using established generic distress questionnaires, and no long-term distress was observed with such instruments independent of cancer and mutation status [3, 4].
However, in the meta-analytic review of 20 such distress studies, Hamilton et al. [4] argued that generic distress instruments did not capture the worries and distress specific to individuals exposed to genetic testing. However, several years earlier, Cella et al. [5] reasoned accordingly and developed “The Multidimensional Impact of Cancer Risk Assessment” (MICRA) questionnaire to assess worries and distress considered specific to genetic testing for cancer risk.
Cella et al. [5] tested the MICRA in a sample of 158 women, identifying three factors of the general part of the questionnaire (21 items). They documented good psychometric properties, and that all three subscales of the MICRA differentiated the BRCA mutation carriers from other three groups of non-carriers, while that was not the case for the comparative generic distress instruments.
The feasibility and the internal consistencies of subscales of the MICRA have been confirmed in several studies related to genetic testing of the BRCA genes [6–13]. However, among them only Lynch et al. [6] have examined the psychometric properties of the MICRA further. Their sample comprised 295 women and 100 men, and they also identified three factors of the general part of the MICRA. The MICRA have been used in several studies comprising a wide variety of issues related to genetic testing and risk assessment [7–13]. These studies include self-selected samples at high risk of being mutation carriers, and they include individuals both with and without cancer. To our knowledge, our study is the first using the MICRA in a sample consisting solely of cancer patients with a minimum of self-selection.
Since 2002, our department has offered BRCA testing to all OC patients, irrespective of a family history of cancer. In order to investigate specific worries and distress related to genetic testing, we made an official Norwegian translation of the MICRA. We then tested the translation in a postal survey of OC patients. The study had four aims: (1) to identify the women most vulnerable to experience psychological distress related to receiving genetic testing and the test result; (2) to explore the psychometric properties of the Norwegian MICRA; (3) to examine the MICRA scorings versus the scorings of two generic distress instruments, and (4) to examine the MICRA scoring patterns in mutation carriers versus non-carriers.
Patients and methods
Patients’ recruitment
Treatment of OC patients is centralized in Norway, and the Department of Gynecologic Oncology, Oslo University Hospital, Norwegian Radium Hospital, covers half of the Norwegian population (approx. 2.6 million inhabitants). Since 2002, all OC patients consecutively admitted to the Department have been offered genetic counseling and testing in the BRCA genes irrespective of their family history of cancer.
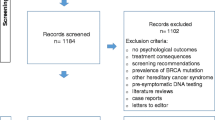
By the end of 2009, 1032 patients had been enrolled in this program. In January 2010, 530 of these patients were still alive, and they were mailed a questionnaire containing the MICRA and two generic distress instruments. One reminder was sent to non-responders after 4 weeks. Altogether 354 delivered valid questionnaires (67 % response rate). We performed an attrition analysis comparing the 176 non-respondents with the respondents.
Study groups
In contrast to the samples of Cella et al. [5] and Lynch et al. [6], our sample consisted exclusively of women with OC. Based on the result from genetic testing combined with patients’ own and family history of both BC and OC, we defined four groups representing a spectrum of genetic risk used by Cella et al. [5].
Group 1: 32 women (9 %) with a demonstrable BRCA mutation; and three groups of non-carriers: Group 2: 23 (6 %) women having both BC and OC; Group 3: 104 women (29 %) with a family history of BC and/or OC; Group 4: 195 women (56 %) without a family history of BC and/or OC. These groups are mutually exclusive, and like those of Cella et al. [5], our groups represented a continuum of cancer risk from group 1 with the highest to group 4 with the lowest risk.
Measurements
The Multidimensional Impact of Cancer Risk Assessment questionnaire (MICRA)
Based on agreement with Cella et al. [5], an official Norwegian translation of the MICRA was developed by professional translators through forward and back translations according to the procedure designed and approved by the Functional Assessment of Chronic Illness Therapy (FACIT) Organization of the developers (FACIT.org).
The MICRA measures distress related to genetic testing and contains 25 items that are scored on Likert scales, from 0 (never) to 5 (often). Of these, the 21 items in “Introduction” section are rated by all respondents and relate to worries and distress concerning the test procedure and test result, and their social and familial consequences. The total score on these general items vary between 0 and 105 with a higher score indicating more specific test-related distress. No studies have indicated any cut-off value defining high genetic distress on the MICRA. Taking a reasonable statistical view, we defined a high MICRA general score as above the mean + 1 standard deviation.
Four items concern defined subgroups only; two items for respondents having children (“Patients and methods”section), and two items for respondents with cancer (“Results” section). For items #5–6, #13, and #18–19 the scores are reversed. The MICRA questionnaire is to be found in the Appendix of Cella et al. [5].
Concerning psychometric testing, Cella et al. [5] used an extension of the Rasch model to identify the underlying factor structure of the first 21 items among 158 women having at least a 10–20 % prior probability of having a deleterious BRCA mutation, and 62 % of them having BC and/or OC. By this model three subscales emerged: Distress with six items (internal consistency of Cronbach’s coefficient α = 0.86); Uncertainty with 9 items (α = 0.77); and Positive Experiences with four items (α = 0.75). From the Positive Experiences subscale item #13 was omitted due to poor factor loading and item #21 due to reduction of internal consistency.
In a study of 295 women and 100 men from high-risk families with identified BRCA mutations, among which 98 (25 %) had cancer, Lynch et al. [6] identified four subscales by Rasch measurement from the same 21 items: Potential Distress; Laden Emotions, Worries and Concerns; Attitude Toward Genetic Testing; and Positive Emotions. However, they concluded that the MICRA contained three conceptually coherent subscales: Distress with four items, Emotions and Concerns with ten items, and Attitude Toward Genetic Testing with seven items.
The Hospital Anxiety and Depression Scale (HADS)
The HADS measures anxiety and depression (emotional distress) for the last 7 days and contains 14 items, seven regarding anxiety and seven regarding depression with a time frame of last week [14]. The HADS is scored on a four-point Likert scale from 0 (not present) to 3 (highly present), and is commonly used in psychosocial cancer research [15]. We used the HADS total score (range 0–42), which showed Cronbach’s coefficient α = 0.91 in our sample.
The Impact of Event Scale (IES)
The IES is a widely used measure of mental trauma symptoms in relation to specific negative life events which in our sample was defined as presence of OC. The IES comprises two sub-scales: Intrusion with seven items, and Avoidance with eight items [16]. The time frame is the past week, and each item is scored from 0 (never) to 5 (often), so the intrusion sum score ranges from 0 to 35, and the avoidance sum from 0 to 40. Cronbach’s α was 0.94 for intrusion and 0.84 for avoidance in our sample.
Data from medical records
Data on age at OC diagnosis, FIGO stage (The International Federation of Gynecology and Obstetrics; staging system for OC), childbearing, and patients’ own history of BC were collected from their medical records. Information concerning family history of BC and/or OC, time from diagnosis to survey, the duration of time from blood sampling to test result disclosure, and the time from test result to survey were obtained from the patients self-report or retrieved from their medical records.
Statistical considerations
All statistical analyses, except the confirmatory factor analysis, were performed on IBM SPSS software package (version 20). All tests were two sided, and the significance level was set at p ≤ 0.05.
The characteristics of the four groups were analyzed with descriptive statistics, using one way analysis of variance with Bonferroni corrections for continuous variables and 2 × 4 Chi square tests for categorical variables. When two groups were compared on categorical variables, we used 2 × 2 Chi square tests. Internal consistency of scales and subscales was tested with Cronbach’s coefficient α. Univariate and multivariable linear regression analyses were performed of the MICRA total score and independent variables, and the strength of associations were reported as B and standardized B values (β).
For exploratory and confirmatory factor analyses, the total sample was randomly split into two halves (n = 177) allowing each type of analysis in separate samples. The procedure for comparing the identified factor structures from Cella et al. [5] and Lynch et al. [6] with our factor structure was as follows:
Exploratory factor analysis Both Cella et al. [5] and Lynch et al. [6] generated a three dimensional factor structure, we therefore decided to constrain our measurement model to three dimensions. Accordingly, the number of dimensions was pre-defined, but each of the 21 general MICRA items was not pre-specified to any particular of these three dimensions. Maximum Likelihood with Direct Oblimin rotation was utilized to generate a factor structure based on the first part of the divided sample.
Confirmatory factor analysis To compare the measurement model from Cella et al. [5] and Lynch et al. [6] with our SPSS generated factor structure we decided to perform structural equation modeling (i.e. Maximum Likelihood estimation) using LISREL (version 8.80) on the other half of the split sample. The fit of each model was evaluated through examination of the sizes of the factor loadings and fit indices values. Acceptable fit was shown by: (1) Root Mean Square Error of Approximation (RMSEA) ≤0.08; (2) Normed Fit Index (NFI) >0.90; (3) Non-Normed Fit Index (NNFI) >0.90; (4) Comparative Fit Index (CFI) >0.90; and (5) Goodness of Fit Index (GFI) >0.90.
Results
Attrition analysis
Of the 530 OC patients invited to the study, 368 (69 %) returned the questionnaire, 39 (8 %) declined and 123 (23 %) did not respond. Among the participants, 12 (2 %) did not complete the MICRA (rated only 0–18 of the 21 general items) and were omitted. Two women were excluded due to being in terminal phase of OC since they died less than 2 months after completing the questionnaire. The final sample therefore consisted of 354 women.
The attrition analysis showed no significant differences between participants and non-participants regarding clinical variables, age at diagnosis, FIGO stage, number of children, or proportion of BRCA mutation carriers.
Findings of the total sample
Findings concerning age at OC diagnosis and survey, time from diagnosis to survey, and time from test result to survey are displayed in Table 1. The mean total score of the 21 items in “Introduction” section of the MICRA was 17.7 and 1 standard deviation was 14.2. According to our previous mentioned definition, high MICRA score was defined as a total score ≥32. With this cut-off, 51 OC patients (14.4 %, 95 % CI 10.7–18.1 %) of the sample had high MICRA scores.
Feasibility of the MICRA
Among the 354 participants, 319 (90 %) rated all the 21 general items of the MICRA, while 25 (7 %) had rated 20 items and 10 (3 %) had rated 19 items. For these 35 women (10 %) the one or two missing values were substituted by the mean of the rated items. Eighteen of the individual items had between 0 and 3 missed ratings; item #14 (“Feeling frustrated that there are no definite cancer prevention guidelines for me”) had 4, item #18 (“Feeling that my family has been supportive during the genetic counseling and testing process”) had 7, and item #13 (“Understanding clearly my choices for cancer prevention or early detection”) had 13 missed ratings.
Items #22 (“Worrying about the possibility of my children getting cancer”) and #23 (“Feeling guilty about possibly passing on the disease to my child(ren)”) should be answered by women who had children. Among the participants, 310 women responded to these two items, while 44 women did not. These rates were in accordance to information concerning number of children given in the patients’ medical records.
Since all our participants had OC, they should all respond to item #24 (“Feeling that the genetic test result has made it harder to cope with my cancer”) and #25 (“Feeling that the genetic test result has made it easier to cope with my cancer”), but only 95 % did so (336 and 335, respectively).
Group characteristics
Characteristics of the study groups are given in Table 1. Significant differences between groups were observed for mean age at diagnosis, age at survey as well as for level of education. No significant differences were observed between groups concerning time from diagnosis to survey, time from diagnosis to test result, time from test result to survey, or FIGO stage (local or advanced disease).
High MICRA score was observed in 66 % of Group 1, 9 % of Group 2, 11 % of Group 3, and 9 % of Group 4 (p < 0.001). The distribution of high MICRA scores between the groups were: 41 % in Group 1, 4 % in group 2, 22 % in Group 3, and 33 % in Group 4.
Psychometric findings
Internal Consistencies of Scales
We obtained good internal consistency of the MICRA and its subscales with marginally better Cronbach’s coefficient α than reported by Cella et al. [5] (their results are given in parentheses): MICRA Total α = 0.84 (0.77), and its subscales: Distress α = 0.90 (0.86), Uncertainty α = 0.81 (0.77), and Positive Experiences α = 0.81 (0.75). Good internal consistencies were also observed for the HADS Total and the IES (data shown under scale descriptions).
Factor analyses
The exploratory analysis generated a solution were the pattern of the factor loadings were closest to the measurement model generated by Cella et al. [5]. Approximately 80 % of the pattern was equal to the model generated by Cella et al. [5], while approximately 60 % were equal to the model generated by Lynch et al. [6].
These three factor solutions was tested in a confirmatory factor analyses, the solutions by Cella et al. [5] and Lynch et al. [6], and our three factor solution generated through the exploratory factor analysis (Table 2). Items #13 and #21 were removed from all three solutions due to a poor factor loading and high-standardized residuals, respectively. By removing the same items from all measurement model and having the same pool of items in each model, LISREL fit indices can be compared. The five fit indices showed strongest values for the model of Cella et al. [5], but the indices did not differ significantly from our model. The weakest fit values were found for the model by Lynch et al. [6] (Table 2).
MICRA and other scale scores
Between group differences
The MICRA and its three subscales all had significantly higher mean scores among mutation carriers (Group 1) as compared with the other non-carriers groups (Groups 2–4) (Table 3). The three non-carrier groups did not show any significant between-group differences on the MICRA or its subscales.
For all four groups, no significant between-group differences were observed on the HADS-Total, IES-Avoidance, or the IES-Intrusion (Table 3).
Regression analysis
As expected, there were a statistically significant association between MICRA total score and receiving a positive BRCA test result (Table 4). Further, age both at diagnosis and at survey, and a family history of OC were also significantly associated with a high MICRA score in univariate analyses. In addition, a high score on the HADS and the IES were associated with high MICRA score. Due to correlations >0.64 between the distress scales scores, only the IES total score was entered into the multivariable analysis, and correspondingly only age at survey entered that analysis.
The associations between receiving a positive BRCA test result and higher scores on HADS and IES remained significant in the multivariable analysis with MICRA total score as dependent variable.
Item analysis of the MICRA
We dichotomized MICRA items #1 to #21 into infrequent (never and rarely) and frequent (sometimes and often) scores. Table 5 displays the proportions of frequent score in the group of mutation carriers versus the groups of non-carriers. Items #9, #12–14, and #18–19 do not significantly discriminate between the groups, and thereby could be considered as independent of mutation status in our sample. Items #2–3, #7, and #10–11 are endorsed by ≥50 % of the mutation carriers, and with significantly higher proportions as compared to the non-carrier groups. These items could then be considered as the most discriminative ones between carriers and non-carriers. Items #17 and #20–21 are all endorsed by <20 % of any group, and could perhaps be considered as superfluous.
Discussion
Summary of main findings
In our sample of women with OC, 14.4 % had high MICRA score according to our definition. These women should be considered the most vulnerable to the stress related to genetic testing (Aim 1). The MICRA showed good psychometric properties with high internal consistencies of the total scale and its subscales. The exploratory factor analysis supported a three factor solution where 80 % of the factor loading pattern was similar to the model generated by Cella et al. [5]. In addition, the fit indices from the confirmatory factor analysis indicated marginally differences between the model by Cella et al. [5] and our exploratory factor model (Aim 2). We confirmed the finding of Cella et al. [5] with significantly higher MICRA total and subscale scores in the group with a demonstrable BRCA mutation as compared to the other three groups of non-carriers. This difference did not emerge in the generic distress instruments (Aim 3). Comparison of the MICRA scoring patterns in mutation carriers versus non-carriers showed a variable frequency of positive responses and discriminating ability (Aim 4).
New findings
We are the first to define a high general MICRA score, identifying patients with high vulnerability and to explore that further. The highest proportion of women with high score was observed among mutation carriers (Group 1), but such women were observed in all four groups. The correlation between high score and group affiliation was −0.26 giving an explained variance of only 7 %. So obviously high MICRA total scores were hardly explained by group affiliation based on cancer risk in our sample of woman with OC.
Other new findings is that receiving a positive BRCA test result and high level of cancer-related distress showed the strongest association with the MICRA total score in multivariable analyses. In addition, the item analyses showed that a number of item scores hardly discriminated between mutation carriers and non-carriers, as well as three items that were endorsed by <20 % of the group samples, and should be considered for omission due to lack of informative value.
Interestingly, in spite of significant differences in sample composition, our exploratory factor structure supported that observed by Cella et al. [5] and Lynch et al. [6] In spite of samples of different sexes, cancer composition and languages, convergent factor solutions were observed.
Confirmatory factor analysis revealed somewhat weaker fit for the solution by Lynch et al. [6] with all fit indices below recommended values. Comparison showed marginally overall better fit for the solution by Cella et al. [5] over our factor solution. We assume that the different factor structure between our model and the one by Cella et al. [5] does not reflect a difference of significance, but further research is needed to confirm this assumption.
Of considerable interest is our findings that neither the time from diagnosis to survey, the time from receiving the test result to survey, nor the duration of time from taking the test to disclosure of test result were significantly related to the mean group scores or the total MICRA score. These findings support the view that genetic testing and the test result are of specific and long-term concern, also among women with a personal history of OC.
Clinical relevance
Our results support the assumption that specific distress related to genetic testing should be addressed with tailor-made instruments like the MICRA. In order to identify the specific concerns related to receiving a positive test result with its severe implications for the patients and their families.
Like the study by Cella et al. [5], Lynch et al. [6] and the few other studies using the MICRA questionnaire [7–13], we have detected significant and specific distress related to receiving a positive test result. These previous studies have all dealt with individuals from high-risk populations both affected and unaffected with cancer. To our knowledge, ours is the only MICRA study performed in individuals unselected for family history of disease. It is of particular interest that neither the duration of time from disclosure of test result to survey nor duration of time from diagnosis to survey was significantly related to the mean group scores or to the total MICRA score. This indicates that genetic testing and the test result are of specific and long-term concern in mutation carriers. However, we also found high MICRA score in nearly 10 % of non-carriers,
We have made a first attempt to define patients with high mental vulnerability to genetic testing based on the MICRA. This work should be continued in order to identify patients in need of counseling or therapy due to the negative life event of getting the bad news of a demonstrable mutation. Genetic counseling is time and labor intensive, the oncogenic approach to genetic testing implies that busy clinicians may not have the time necessary to provide adequate information about consequences of receiving a positive or inconclusive test result.
In the era of personalized medicine genetic testing becomes more available and widespread, and it moves from highly selected at-risk individuals to less self-selected population samples. With new targeted therapies, routine genetic testing of patients makes sense, but the increasing demand for genetic testing with time constraints regarding cancer treatment decisions dependent on test results pose a challenge for genetic counselors.
Since the development of the MICRA, several new instruments aimed at being more specific than the generic distress instruments have been developed [17–20]. The primary objective is to identify specifically a broad range of psychosocial issues experienced by individuals undergoing genetic counseling and testing in the oncology setting. All these instruments have been used in fewer studies than the MICRA, and more studies are needed in order to state whether they represent any improvements as compared to the MICRA.
Strengths and limitations
We consider it strength of our study that the translations and back-translations of the MICRA followed a predefined pattern established by the FACIT organization of the developers.
Hitherto, studies using the MICRA only comprise populations from the United States and Canada with North Americans and African Americans, with the majority from the clinical research program at the Lombardi Comprehensive Cancer Center by the developers of the questionnaire [5, 7–13]. In contrast, we tested the MICRA in another language, and in a population consisting solely of cancer patients. Additionally, in Norway health care is close to free of charge for everyone, and there are no restrictions of uptake to genetic testing when considered indicated by relevant medical specialists.
Although two of our study groups were small (n = 23 and n = 32), we still observed significant differences between the groups. The MICRA mean scores were significantly different from the scores of the other anxiety instruments, even at low statistical power. However, with larger group sizes more significant differences in group characteristics (Table 1) could have emerged.
Conclusions
Our study, of OC patients receiving genetic testing to disclose inherent cause of disease caused by mutations in the BRCA genes, supported good acceptance of the MICRA and confirmed the good psychometric properties previously described by Cella et al. [5]. Exploratory and confirmatory factor analyses in our sample identified a three-factor solution close to that observed by Cella et al. We defined high mental vulnerability to the genetic test procedure based on total MICRA score, and observed a rate of 14.4 %. The MICRA in Norwegian translation is a valuable tool for research and clinical work investigating specific mental distress related to the procedures of genetic testing.
References
Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL et al (2003) Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 72:1117–1130
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25:1329–1333
Reichelt JG, Moller P, Heimdal K, Dahl AA (2008) Psychological and cancer-specific distress at 18 months post-testing in women with demonstrated BRCA1 mutations for hereditary breast/ovarian cancer. Fam Cancer 7:245–254
Hamilton JG, Lobel M, Moyer A (2009) Emotional distress following genetic testing for hereditary breast and ovarian cancer: a meta-analytic review. Health Psychol 28:510–518
Cella D, Hughes C, Peterman A, Chang CH, Peshkin BN, Schwartz MD et al (2002) A brief assessment of concerns associated with genetic testing for cancer: the multidimensional impact of cancer risk assessment (MICRA) questionnaire. Health Psychol 21:564–572
Lynch HT, Snyder C, Lynch JF, Karatoprakli P, Trowonou A, Metcalfe K et al (2006) Patient responses to the disclosure of BRCA mutation tests in hereditary breast-ovarian cancer families. Cancer Genet Cytogenet 165:91–97
O’Neill SC, Demarco T, Peshkin BN, Rogers S, Rispoli J, Brown K et al (2006) Tolerance for uncertainty and perceived risk among women receiving uninformative BRCA1/2 test results. Am J Med Genet C Semin Med Genet 142C:251–259
Tercyak KP, Peshkin BN, Brogan BM, Demarco T, Pennanen MF, Willey SC et al (2007) Quality of life after contralateral prophylactic mastectomy in newly diagnosed high-risk breast cancer patients who underwent BRCA1/2 gene testing. J Clin Oncol 25:285–291
Rini C, O’Neill SC, Valdimarsdottir H, Goldsmith RE, Jandorf L, Brown K et al (2009) Cognitive and emotional factors predicting decisional conflict among high-risk breast cancer survivors who receive uninformative BRCA1/2 results. Health Psychol 28:569–578
O’Neill SC, Rini C, Goldsmith RE, Valdimarsdottir H, Cohen LH, Schwartz MD (2009) Distress among women receiving uninformative BRCA1/2 results: 12-month outcomes. Psychooncology 18:1088–1096
Graves KD, Gatammah R, Peshkin BN, Krieger A, Gell C, Valdimarsdottir HB et al (2011) BRCA1/2 genetic testing uptake and psychosocial outcomes in men. Fam Cancer 10:213–223
Halbert CH, Stopfer JE, McDonald J, Weathers B, Collier A, Troxel AB et al (2011) Long-term reactions to genetic testing for BRCA1 and BRCA2 mutations: does time heal women’s concerns? J Clin Oncol 29:4302–4306
Graves KD, Vegella P, Poggi EA, Peshkin BN, Tong A, Isaacs C et al (2012) Long-term psychosocial outcomes of BRCA1/BRCA2 testing: differences across affected status and risk-reducing surgery choice. Cancer Epidemiol Biomarkers Prev 21:445–455
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 52:69–77
Horowitz MJ, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective distress. Psychosom Med 41:209–218
Read CY, Perry DJ, Duffy ME (2005) Design and psychometric evaluation of the psychological adaptation to genetic information scale. J Nurs Scholarsh 37:203–208
Phelps C, Bennett P, Jones H, Hood K, Brain K, Murray A (2010) The development of a cancer genetic-specific measure of coping: the GRACE. Psychooncology 19:847–854
Eijzenga W, Bleiker EM, Hahn DE, Kluijt I, Sidharta GN, Gundy C et al (2014) Psychosocial aspects of hereditary cancer (PAHC) questionnaire: development and testing of a screening questionnaire for use in clinical cancer genetics. Psychooncology 23:862–869
Eijzenga W, Aaronson NK, Kluijt I, Sidharta GN, Hahn DE, Ausems MG et al (2014) The efficacy of a standardized questionnaire in facilitating personalized communication about problems encountered in cancer genetic counseling: design of a randomized controlled trial. BMC Cancer 14:26
Acknowledgments
Alv A. Dahl, MD, PhD holds a grant from The Norwegian Radium Hospital Foundation. This work was supported by the Inger and John Fredriksen Foundation for Ovarian Cancer Research.
Conflict of interest
The authors declare no conflict of interest.
Ethical standard
The study protocol was approved by The Institutional Review Board and The Regional Committee for Medicine and Health Research Ethics of South-East Norway. All patients gave written informed consent when they returned the questionnaire.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bjørnslett, M., Dahl, A.A., Sørebø, Ø. et al. Psychological distress related to BRCA testing in ovarian cancer patients. Familial Cancer 14, 495–504 (2015). https://doi.org/10.1007/s10689-015-9811-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-015-9811-2