Abstract
The programmed cell death 6 (PDCD6), discovered as a proapoptotic calcium-binding protein, has recently been found dysregulated in tumors of various origin and contributed to cancer cell viability. The aim of this study was to determine whether SNPs in PDCD6 are associated with cervical squamous cell carcinoma (CSCC). Polymerase chain reaction-restriction fragment length polymorphism method was used to genotype two tag SNPs (rs3756712 and rs4957014) of PDCD6 in 328 CSCC patients and 541 controls. Significantly increased CSCC risks were found to be associated with T allele of rs3756712 and G allele of rs4957014 (P = 0.017, OR = 1.320, and P = 0.007, OR = 1.321, respectively). CSCC risks were associated with these two SNPs in different genetic model (P = 0.04, OR = 1.78 for rs3756712 in a recessive model, and P = 0.006, OR = 2.01 for rs4957014 in a codominant model, respectively). Results of stratified analyses revealed that rs4957014 is associated with parametrial invasion of CSCC (P = 0.044, OR = 1.414). Our results suggest that these two tag SNPs of PDCD6 are associated with CSCC, indicating that PDCD6 may play an important role in the pathogenesis of CSCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer has long been recognized as an important reproductive health problem for women in developing and developed countries. The global incidence increased from 378,000 cases per year in 1980 to 454,000 cases per year in 2010—a 0.6 % annual rate of increase. Cervical cancer death rates have been decreasing but this disease still killed 200,000 women in 2010, of whom 46,000 were aged 15–49 years in developing countries [1]. In China, incidence rates of cervical cancer ranged from 2.4 per 100,000 women in Jiashan to 4.6 per 100,000 women in Guangzhou [2]. Although it is well-recognized that specific high-risk types of human papillomavirus (HPV) are primary etiologic factors in cervical cancer, the majority of infected women do not develop the cancer, suggesting that other factors including host genetic factors appear to contribute to the susceptibility and development of malignancy [3, 4]. Genetic-epidemiological studies on the heritability of cervical cancer have shown a familial aggregation of cervical intraepithelial neoplasia and cervical cancer in first-degree relatives [5–7]. The evidence of genetic inheritance and susceptibility to cervical cancer were also supported in twin studies that investigated smear abnormalities and cervical cancer [5, 8, 9]. Although these genetic-epidemiological studies strongly suggest that host genetics play a role in susceptibility to cervical cancer, the genes involved in this process are still unknown.
Programmed cell death 6 (PDCD6), also well-known as apoptosis-linked gene-2 (ALG-2), is a calcium-binding modulator protein associated with cell proliferation and death. It is first described as a pro-apoptotic protein in a functional screen of T cell hybridoma cells [10]. PDCD6 gene encodes a 22 kDa Ca2+-binding protein containing five serially repetitive EF-hand structures. This protein is one of the prototypic members of the penta EF-hand protein family, participating in T cell receptor-, Fas-, and glucocorticoid-induced programmed cell death [11, 12]. However, apoptosis was not blocked in PDCD6-deficient mice, suggesting that PDCD6 is functionally redundant [13]. It has also been reported that PDCD6 play a role in modulation of endoplasmic reticulum (ER)-stress-stimulated cell death and neuronal apoptosis during organ formation [14, 15].
Programmed cell death 6 (PDCD6) is widely expressed in tissues and cell lines, including various tumor types, as shown by transcript analyses and Western blot analyses [16–18]. PDCD6 was found to be up-regulated in a variety of tumors compared to normal tissues of the breast, liver, lung, and colon, especially in metastatic tissues, suggesting that in addition to its known pro-apoptotic function PDCD6 may play a role in cell survival [17, 18]. In contrast, down-regulation of PDCD6 expression was also observed in gastric cancer and HeLa cells [19, 20]. In addition, recent studies found that lower mRNA expression levels of PDCD6 were significantly with a poor overall survival in endoscopic biopsy samples of gastric cancer and that PDCD6 may be a molecular marker for the prognosis of advanced gastric cancer [19, 21]. Epithelial ovarian cancer patients with medium or high levels of PDCD6 mRNA were at higher risk for disease progression, but no association was found between PDCD6 expression and overall survival [22]. Thus, these findings indicate that alteration of PDCD6 expression may contribute to the development and/or progression of cancers and that PDCD6 may be a useful molecular marker for the prognosis of cancers.
To investigate whether the PDCD6 gene contributes to the development and/or progression of cervical squamous cell carcinoma (CSCC), we genotyped two tag SNPs (rs3756712 and rs4957014) of PDCD6 gene in 328 CSCC patients and 541 control subjects and analyzed the association between these two SNPs and CSCC risk.
Materials and methods
Study subjects
This study was approved by the hospital ethics committee and all subjects gave written informed consent to participate. A hospital-based case–control study was conducted including 328 unrelated patients ranging in age from 20 to 77 years (mean ± SD, 43.92 ± 8.51) with CSCC between July 2007 and April 2012 at the second university Hospital of Sichuan University. The diagnosis of CSCC was confirmed in all cases by histological examination of tissue from biopsy or resected specimens. A group of control subjects consisted of 541 healthy subjects ranging in age from 29 to 70 years (mean ± SD, 44.49 ± 5.98) was selected randomly from a routine health survey in the same hospital. Subjects with any personal or family history of CSCC or other serious disease were intentionally excluded. All subjects were Han population living in Sichuan province of southwest China. Medical records were reviewed for patients’ characteristics, including age at diagnosis, clinical stage, tumor differentiation, lymph node status, and parametrial invasion.
PDCD6 genotyping
Genomic DNA of each individual was extracted from 200 μL EDTA-anticoagulated peripheral blood samples by a DNA isolation kit from Bioteke (Peking, China) and the procedure was performed according to the manufacturer’s instructions. The polymerase chain reaction (PCR)-restriction fragment length polymorphism (RFLP) method was used to genotype these two SNPs (rs3756712 and rs4957014) of PDCD6 gene. Primers were established with the PIRA PCR designer (http://cedar.genetics.soton.ac.uk/public_html/primer2.html) [23]. In brief, the primer sequences were: F: 5′-TACAGTGGCAAAGGACCACA-3′ and R: 5′-CACATTCCAGCACTCACCAC-3′ for rs3756712. The primers used for amplification of the rs4957017 were F: 5′-TGGTGTTTCATACCATTGACACTTGC-3′ and R: 5′-CTCAGAACCAAGCAGGTTCCTTCA-3′.
DNA fragments containing the polymorphism were amplified in a total volume of 25 μL, including 2.5 μL 10 × PCR buffer, 1.5 mmol/L MgCl2, 0.15 mmol/L dNTPs, 0.5 μmol/L each primer, 100 ng of genomic DNA and 1 U of Taq DNA polymerase. Both of the PCR conditions were 94 °C for 4 min, followed by 32 cycles of 30 s at 94 °C, 30 s at 62 °C and 30 s at 72 °C, with a final elongation at 72 °C for 10 min. PCR products were digested overnight with specific restriction enzyme and the digested PCR products were separated by a 6 % polyacrylamide gel and stained with 1.5 g/L argent nitrate: RsaI for rs3756712, allele G is cuttable, yielding two fragments of 66 and 99 bp, allele T is uncuttable and the fragment is still 165 bp; and HphI for rs4957014, allele G is cuttable, yielding two fragments of 13 and 100 bp, allele T is uncuttable and the fragment is still 113 bp. The genotypes were confirmed by the DNA sequencing analysis. About 10 % of the samples were randomly selected to perform the repeated assays and the results were 100 % concordant.
Statistical analysis
Data were analyzed using SPSS for Windows software package version 13.0 (SPSS Inc., Chicago, IL, USA). Genotype frequencies of these two SNPs were obtained by directed counting and Hardy–Weinberg equilibrium were evaluated by Chi square test. Genotypic association tests in a case–control pattern assuming codominant, dominant, recessive, overdominant, or log-additive genetic models were performed using SNPstats [24]. Odds ratio (OR) and respective 95 % confidence intervals were reported to evaluate the effects of any difference between alleles, genotypes. Probability values of 0.05 or less were regarded as statistically significant in CSCC patients compared to controls.
Results
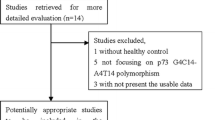
These two SNPs of PDCD6 were successfully genotyped in 328 CSCC patients and 541 control subjects. Three genotypes of these two SNPs were identified and the genotypes were confirmed by the DNA sequencing analysis (Fig. 1). Genotype distributions of these two SNPs in control subjects and CSCC patients were in agreement with that expected under the Hardy–Weinberg equilibrium. Allele frequencies of these two SNPs for CSCC patients and control subjects are shown in Table 1. As shown in Table 1, significantly increased CSCC risk was found to be associated with T allele of SNP rs3756712 (P = 0.017, OR = 1.320, 95 % CI = 1.050–1.659), and with G allele of SNP rs4957014 (P = 0.007, OR = 1.321, 95 % CI = 1.079–1.618), respectively.
a Determination of SNP rs3756712 by PCR–polyacrylamide gel electrophoresis. M 100-bp ladder; lanes 1, 4, 5, 6, 7, 8, and 11 the TT homozygotes; lanes 2, 9, and 10 the GT heterozygotes; lane 3 the GG homozygote. b Sequencing analysis for SNP rs3756712. c Determination of SNP rs4957014 by PCR–polyacrylamide gel electrophoresis. M 100-bp ladder; lanes 1, 2, and 4 the GG homozygotes; lanes 3, 8, and 9, the GT heterozygotes; lanes 5, 6, 7, and 10 the TT homozygotes. d. Sequencing analysis for SNP rs4957014
As shown in Table 2, significant associations were observed with genotypes of SNP rs3756712 and rs4957014 in different genetic model. Compared with TT homozygous carriers, a significant decreased CSCC risk was associated with GG homozygous carriers of rs3756712 in a codominant model (OR = 1.91, 95 % CI = 1.07–3.42). Subjects without allele T (GG genotype) of rs3756712 had a significantly decreased risk for CSCC compared with that carrying allele T (TT/GT genotypes) in a recessive model (P = 0.04, OR = 1.78, 95 % CI = 1.01–3.15). For SNP rs4957014, a significant increased CSCC risk was associated with GG homozygous carriers compared with TT homozygous carriers in a codominant model (OR = 2.01, 95 % CI = 1.30–3.13). Subjects without allele T (GG genotype) of rs4957014 also had a significantly increased risk for CSCC compared with those carrying allele T (TT/GT genotypes) in a recessive model (P = 0.001, OR = 1.92, 95 % CI = 1.30–2.94).
Results of stratified analyses by age, clinical stage, tumor differentiation, lymph node status, and parametrial invasion with these two SNPs are presented in Table 3 and 4, respectively. Table 3 shows that rs3756712 is associated with tumor differentiation, although not statistically significant (P = 0.066, OR = 1.497, 95 % CI = 0.972–2.305, adjusted by age, clinical stage, lymph node status, and parametrial invasion). As shown in Table 4, rs4957014 was found to be associated with parametrial invasion (P = 0.044, OR = 1.414, 95 % CI = 1.009–1.983, adjusted by age, clinical stage, tumor differentiation, and lymph node status). No statistically significant difference in the genotype or allele distribution of rs3756712 between different CSCC patients stratified by age, clinical stage, lymph node status, or parametrial invasion, and that of rs4957014 between age, clinical stage, tumor differentiation, or lymph node status, was observed.
Discussion
In the present study, for the first time, we identified the associations between tag SNPs of PDCD6 gene and CSCC, as well as the association between these two SNPs and CSCC patients’ characteristics. Our findings suggest that the T allele of rs3756712 and G allele of rs4957014 may increase CSCC risk. In addition, rs4957014 is associated with parametrial invasion of CSCC. This study provided the first evidence that PDCD6 may be used as candidate biomarker for CSCC susceptibility.
PDCD6 was one of the six apoptosis-linked genes whose cDNA clones were isolated by the “death-trap” method in which a cDNA library constructed in a mammalian expression vector was used to transfect mouse T cell hybridoma 3DO cells in order to protect them from death induced by T cell receptor stimulation [10, 25]. Although the length of N-terminal tails of PDCD6 protein are variable, its relative conserved in animals (69 and 89 % identities between human and fruit fly and between human and zebra fish, respectively, in the PEF domain of human PDCD6, residues No. 24–191) [25]. PDCD6 protein exists predominantly in a dimer form at higher concentrations (5–20 µmol/L) but in equilibrium between a monomer and a dimer at concentration <1 µmol/L [26]. Analyses of PDCD6 amino acid-substituted mutants of Ca2+-coordinating residues revealed strong Ca2+-binding sites located at EF1 and EF3, and that binding to Ca2+ induces conformational changes and exposure of hydrophobic surfaces at a micromolar Ca2+ concentration [26–28]. The conformational change enables PDCD6 to interact with various proteins. An isoform of PDCD6 (designated ALG-2,1) was shorter in six nucleotides corresponding to the two amino acids Gly121Phe122 in comparison with the full-length cDNA clone (designated ALG-2,5), and the shorter protein isoform has a lower Ca2+-sensitivity [16].
PDCD6IP (programmed cell death 6 interacting protein), also known as Alix (ALG-2-interacting protein X), was the first identified protein that interacts with PDCD6 in a Ca2+-dependent fashion [29, 30]. PDCD6IP is an adaptor protein involved in the regulation of the endolysosomal system through binding to endophilins and to proteins of ESCRT (endosomal sorting complexes required for transport), TSG101 (tumor susceptibility gene 101) and CHMP4b (chromatin-modifying protein; charged multivesicular body protein). Overexpression of PDCD6IP is sufficient to induce cell death of neuroepithelial cells, while this effect is strictly dependent on its capacity to bind to PDCD6 and the interaction of the PDCD6/PDCD6IP complex with ESCRT proteins is necessary for naturally occurring death of motoneurons [15]. Expression of the C-terminal half of PDCD6IP blocked apoptosis depending on its capacity to bind PDCD6, suggesting that it acts by titrating out of PDCD6 [15, 31]. PDCD6 and PDCD6IP interact with pro-caspase-8 and that PDCD6IP forms a complex with the TNF-R1 (TNFα receptor-1), depending on its capacity to bind ESCRT proteins. The death domain (DD) of TNF-R1 and the death effector domain (DED) containing pro-domain of pro-caspase 8 are obligatory for binding to PDCD6IP and PDCD6, respectively, and that Fas-associated protein with death domain (FADD) is present in the PDCD6/PDCD6IP/pro-caspase-8 complex [32]. The human death-associated protein kinase 1 (DAPk1), a protein that functions as a positive mediator of apoptosis, has been identified interacts with PDCD6, and thus accelerate apoptotic cell death by increasing caspase-3 activity [33].
Constitutive and alternative splicing of pre-mRNAs are complex processes which must be accomplished with high precision that is reflected by the complex machinery involved in splicing. Impaired splicing can lead to severe cell damage and many diseases, including cancer [34]. RBM22 is an RNA-binding protein of unknown function. Duo to the presence of RBM22, the cytosolic protein PDCD6 becomes translocated to the nucleus, suggesting that the formation of PDCD6/RBM22 complexes may thus play an important role in Ca2+-dependent signaling influencing alternative splicing and cell division during development [35]. The human embryonic ectoderm development protein (HEED), a transcriptional repressor involved in the regulation of homeotic genes during mouse development, has also been reported to interact with PDCD6, and that the interaction between HEED and the third EF-hand motif of PDCD6 is stronger than that of others [36]. These may provide a link between PDCD6 and the regulation of alternative splicing influencing basic cellular processes during development, including the development of cancer.
PDCD6 has recently been found dysregulated in tumors of various origin and contributed to cancer cell viability, indicating that it may play an important role in the pathology of cancer cells and may be a tumor marker [18]. Beside its known proapoptotic functions, PDCD6 has also been shown to be upregulated in a variety of human tumors, suggesting that PDCD6 may be also a player in survival pathways in cancers [17, 18, 37]. The prospect of the opposing function of PDCD6 may be that PDCD6 function is species or cell-type dependent. PDCD6 knockdown in HeLa cells induces accumulation of cells in the G2/M cell cycle phase and increases the amount of early apoptotic and dead cells, indicating that PDCD6 has an anti-apoptotic function in HeLa cells by facilitating the passage through checkpoints in the G2/M cell cycle phase [20]. In pulmonary adenocarcinomas, PDCD6 gene is amplified and upregulated, and it has been identified as a prognostic marker for early stage adenocarcinoma with poor prognosis [37]. In epithelial ovarian cancer, PDCD6 is highly expressed in metastatic ovarian cancer cells and positively regulates cell migration and invasion. Although no association was found between PDCD6 expression and overall survival, patients with medium or high levels of PDCD6 expression were at higher risk for disease progression [22]. PDCD6 may be also a molecular biomarker for the prognosis of gastric cancer, as the protein expression is closely associated with the prognosis of advanced gastric cancer patients and it accelerates apoptotic cell death by activating the mitochondrial pathway [21]. Recently, it has been identified that PDCD6 may be a new candidate marker for advanced-stage oral cancer [38]. Most recently, two studies reported the possible molecular mechanism for PDCD6 as a pro-apoptotic protein [39, 40]. PDCD6 can regulate phosphorylation of PI3K/AKt through targeting NF-κB signaling pathways, and PDCD6 can mediate the pro-apoptotic activity of cisplatin or TNFα through the down-regulation of NF-κB expression [40]. Angiogenesis is essential in early development, tissue repair, tumor metastasis, and is a key step in tumor growth. PDCD6 can inhibit tumor growth via suppression of tumor angiogenesis in the cellular physiological condition through targeting PI3K/mTOR (mammalian target of rapamycin)/p70S6K (p70 ribosomal protein S6 kinase) signaling pathway [39].
Although PDCD6 has been widely studied in various cancers and cell lines, our study is the first report demonstrated that both rs3756712 and rs4957014 of PDCD6 gene were associated with the development of CSCC, as well as with parametrial invasion of CSCC, suggesting an important role for PDCD6 in the pathogenesis of CSCC. Nevertheless, the present study may have some limitations because of study design. In this study, only 328 CSCC patients and 541 controls have been genotyped, which may limit the statistical power of our analysis. Further studies genotyping more genetic polymorphisms in PDCD6 gene in different population could help to establish the true significance of the associations between these SNPs and severity, and susceptibility to CSCC. The impact of these SNPs on pro-tumorigenicity of CSCC, as well as the expression of PDCD6, the molecular mechanism for PDCD6 involved in the development of CSCC, and so on, are needed to further study.
References
Forouzanfar MH, Foreman KJ, Delossantos AM et al (2011) Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis. Lancet 378(9801):1461–1484
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB (2008) Cancer incidence in five continents. Volume IX. IARC scientific publications (160):1–837
Ko SM, Kua EH, Fones CS (1999) Stress and the undergraduates. Singapore Med J 40(10):627–630
Walboomers JM, Jacobs MV, Manos MM et al (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1):12–19
Vink JM, van Kemenade FJ, Meijer CJ, Casparie MK, Meijer GA, Boomsma DI (2011) Cervix smear abnormalities: linking pathology data in female twins, their mothers and sisters. Eur J Hum Genet : EJHG 19(1):108–111
Magnusson PK, Sparen P, Gyllensten UB (1999) Genetic link to cervical tumours. Nature 400(6739):29–30
Couto E, Hemminki K (2006) Heritable and environmental components in cervical tumors. Int J Cancer 119(11):2699–2701
Ahlbom A, Lichtenstein P, Malmstrom H, Feychting M, Hemminki K, Pedersen NL (1997) Cancer in twins: genetic and nongenetic familial risk factors. J Natl Cancer Inst 89(4):287–293
de Freitas AC, Gurgel AP, Chagas BS, Coimbra EC, do Amaral CM (2012) Susceptibility to cervical cancer: an overview. Gynecol Oncol 126(2):304–311
Vito P, Lacana E, D’Adamio L (1996) Interfering with apoptosis: Ca2+-binding protein ALG-2 and Alzheimer’s disease gene ALG-3. Science 271(5248):521–525
Shibata H, Yamada K, Mizuno T et al (2004) The penta-EF-hand protein ALG-2 interacts with a region containing PxY repeats in Alix/AIP1, which is required for the subcellular punctate distribution of the amino-terminal truncation form of Alix/AIP1. J Biochem 135(1):117–128
Jung YS, Kim KS, Kim KD, Lim JS, Kim JW, Kim E (2001) Apoptosis-linked gene 2 binds to the death domain of Fas and dissociates from Fas during Fas-mediated apoptosis in Jurkat cells. Biochem Biophys Res Commun 288(2):420–426
Jang IK, Hu R, Lacana E, D’Adamio L, Gu H (2002) Apoptosis-linked gene 2-deficient mice exhibit normal T-cell development and function. Mol Cell Biol 22(12):4094–4100
Rao RV, Poksay KS, Castro-Obregon S et al (2004) Molecular components of a cell death pathway activated by endoplasmic reticulum stress. J Biol Chem 279(1):177–187
Mahul-Mellier AL, Hemming FJ, Blot B, Fraboulet S, Sadoul R (2006) Alix, making a link between apoptosis-linked gene-2, the endosomal sorting complexes required for transport, and neuronal death in vivo. J Neuroscience: Off J Soc Neurosci 26(2):542–549
Tarabykina S, Moller AL, Durussel I, Cox J, Berchtold MW (2000) Two forms of the apoptosis-linked protein ALG-2 with different Ca2+ affinities and target recognition. J Biol Chem 275(14):10514–10518
la Cour JM, Mollerup J, Winding P, Tarabykina S, Sehested M, Berchtold MW (2003) Up-regulation of ALG-2 in hepatomas and lung cancer tissue. Am J Pathol 163(1):81–89
la Cour JM, Hoj BR, Mollerup J, Simon R, Sauter G, Berchtold MW (2008) The apoptosis linked gene ALG-2 is dysregulated in tumors of various origin and contributes to cancer cell viability. Mol Oncol 1(4):431–439
Yamada Y, Arao T, Gotoda T et al (2008) Identification of prognostic biomarkers in gastric cancer using endoscopic biopsy samples. Cancer Sci 99(11):2193–2199
Hoj BR, la Cour JM, Mollerup J, Berchtold MW (2009) ALG-2 knockdown in HeLa cells results in G2/M cell cycle phase accumulation and cell death. Biochem Biophys Res Commun 378(1):145–148
Yoon JH, Choi YJ, Kim SG, Nam SW, Lee JY, Park WS (2012) Programmed cell death 6 (PDCD6) as a prognostic marker for gastric cancers. Tumour Biol 33(2):485–494
Su D, Xu H, Feng J et al (2012) PDCD6 is an independent predictor of progression free survival in epithelial ovarian cancer. J Transl Med 10:31
Ke X, Collins A, Ye S (2001) PIRA PCR designer for restriction analysis of single nucleotide polymorphisms. Bioinformatics 17(9):838–839
Sole X, Guino E, Valls J, Iniesta R, Moreno V (2006) SNPStats: a web tool for the analysis of association studies. Bioinformatics 22(15):1928–1929
Maki M, Suzuki H, Shibata H (2011) Structure and function of ALG-2, a penta-EF-hand calcium-dependent adaptor protein. Sci China Life Sci 54(8):770–779
Subramanian L, Crabb JW, Cox J et al (2004) Ca2+ binding to EF hands 1 and 3 is essential for the interaction of apoptosis-linked gene-2 with Alix/AIP1 in ocular melanoma. Biochemistry 43(35):11175–11186
Lo KW, Zhang Q, Li M, Zhang M (1999) Apoptosis-linked gene product ALG-2 is a new member of the calpain small subunit subfamily of Ca2+-binding proteins. Biochemistry 38(23):7498–7508
Maki M, Yamaguchi K, Kitaura Y, Satoh H, Hitomi K (1998) Calcium-induced exposure of a hydrophobic surface of mouse ALG-2, which is a member of the penta-EF-hand protein family. J Biochem 124(6):1170–1177
Missotten M, Nichols A, Rieger K, Sadoul R (1999) Alix, a novel mouse protein undergoing calcium-dependent interaction with the apoptosis-linked-gene 2 (ALG-2) protein. Cell Death Differ 6(2):124–129
Vito P, Pellegrini L, Guiet C, D’Adamio L (1999) Cloning of AIP1, a novel protein that associates with the apoptosis-linked gene ALG-2 in a Ca2+-dependent reaction. J Biol Chem 274(3):1533–1540
Trioulier Y, Torch S, Blot B et al (2004) Alix, a protein regulating endosomal trafficking, is involved in neuronal death. J Biol Chem 279(3):2046–2052
Mahul-Mellier AL, Strappazzon F, Petiot A et al (2008) Alix and ALG-2 are involved in tumor necrosis factor receptor 1-induced cell death. J Biol Chem 283(50):34954–34965
Lee JH, Rho SB, Chun T (2005) Programmed cell death 6 (PDCD6) protein interacts with death-associated protein kinase 1 (DAPk1): additive effect on apoptosis via caspase-3 dependent pathway. Biotechnol Lett 27(14):1011–1015
Venables JP (2004) Aberrant and alternative splicing in cancer. Cancer Res 64(21):7647–7654
Montaville P, Dai Y, Cheung CY et al (2006) Nuclear translocation of the calcium-binding protein ALG-2 induced by the RNA-binding protein RBM22. Biochim Biophys Acta 1763(11):1335–1343
Lee KH, Kim E, Lee JS, Lee KS, Kim JW (2001) Mapping of the interaction sites between apoptosis linked gene ALG-2 and HEED. Mol Cells 12(3):298–303
Aviel-Ronen S, Coe BP, Lau SK et al (2008) Genomic markers for malignant progression in pulmonary adenocarcinoma with bronchioloalveolar features. Proc Natl Acad Sci USA 105(29):10155–10160
Ambatipudi S, Gerstung M, Gowda R et al (2011) Genomic profiling of advanced-stage oral cancers reveals chromosome 11q alterations as markers of poor clinical outcome. PLoS One 6(2):e17250
Rho SB, Song YJ, Lim MC, Lee SH, Kim BR, Park SY (2012) Programmed cell death 6 (PDCD6) inhibits angiogenesis through PI3K/mTOR/p70S6K pathway by interacting of VEGFR-2. Cell Signal 24(1):131–139
Park SH, Lee JH, Lee GB et al (2012) PDCD6 additively cooperates with anti-cancer drugs through activation of NF-κB pathways. Cell Signal 24(3):726–733
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No. 81172440, No. 81272821, No. 81172494 and No. 30901596); the Applied Basic Research Programs of Science and Technology Commission Foundation of Sichuan Province (No. 2013JY0008 and No. 2013JY0013); and Program for Changjiang Scholars and Innovative Research Team in University (PCSIRT0935).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Bin Zhou and Peng Bai have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhou, B., Bai, P., Xue, H. et al. Single nucleotide polymorphisms in PDCD6 gene are associated with the development of cervical squamous cell carcinoma. Familial Cancer 14, 1–8 (2015). https://doi.org/10.1007/s10689-014-9767-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-014-9767-7