Abstract
The prognostic significance of O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation on Glioblastoma multiforme (GBM) remains controversial. A meta-analysis of published studies investigating the effects of MGMT promoter methylation on both progression-free survival (PFS) and overall survival (OS) among GBM patients was performed. A total of 2,986 patients from 30 studies were included in the meta-analysis. In all, the frequency of MGMT promoter methylation was 44.27 %. Five studies undertook univariate analyses and nine undertook multivariate analyses of MGMT promoter methylation on PFS. The pooled hazard ratio (HR) estimate for PFS was 0.72 (95 % CI 0.55–0.95) by univariate analysis and 0.51 (95 % CI 0.38–0.69) by multivariate analysis. The effect of MGMT promoter methylation on OS was evaluated in 15 studies by univariate analysis and 14 studies by multivariate analysis. The combined HR was 0.67 (95 % CI 0.58–0.78) and 0.49 (95 % CI 0.38–0.64), respectively. For GBM patients treated with Alkylating agent, the meta-risk remained highly significant by both univariate (HR = 0.58; 95 % CI 0.42–0.79) and multivariate analysis (HR = 0.42; 95 % CI 0.29–0.60). This study showed that MGMT promoter methylation was associated with better PFS and OS in patients with GBM regardless of therapeutic intervention, and associated with longer OS in GBM patients treated with alkylating agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM, WHO grade 4) is one of the most frequently occurring brain tumors with an annual incidence of 3–4/100,000[1] in the primary central nervous system of adults and is highly malignant. The current WHO classification recognizes three variants, including conventional glioblastoma, giant cell glioblastoma, and gliosarcoma. GBM is a morphologically diverse and genetically instable neoplasm usually with rapidly fatal prognosis. After the trial by Stupp et al. [2, 3], the current standard of care for newly diagnosed GBM is surgical resection to the extent feasible followed by radiotherapy plus an oral cytotoxic chemotherapy with the alkylating agent temozolomide (TMZ), given concomitantly with and after radiotherapy (RT). The median survival time is only 14 months from diagnosis, despite the use of aggressive treatment, surgery, postoperative radiotherapy, and adjuvant temozolomide (TMZ)-based chemotherapy [2, 4, 5]. The necessity of tumor markers that explain their biology is becoming increasingly important, mainly to recognize a potential molecular target of therapy.
The O6-methylguanine-DNA methyltransferase (MGMT) gene encodes a ubiquitously expressed suicide DNA repair enzyme that counteracts the normally lethal effects of alkylating agents by removing alkyl adducts from the O6-position of guanine [6]. O6-Alkylated guanine causes base mispairing and double-strand breaks, thus inducing apoptosis and cell death [7]. The assessment of MGMT promoter methylation is currently considered as mandatory for patient selection in clinical trials [8]. The results of the European Organisation for Research and Treatment of Cancer (EORTC) and the National Cancer Institute of Canada (NCIC) trial, in which methylation of the MGMT promoter was the strongest predictor for outcome and benefit from TMZ treatment [3, 8].
However, the prognostic significance of MGMT promoter methylation on GBM regardless of therapeutic intervention remains controversial [9, 10]. Based on the discordant results obtained by a large number of studies, we performed this meta-analysis with accumulated data from different studies to quantify the prognostic impacts of MGMT promoter methylation on both progression-free survival (PFS) and overall survival (OS) among patients with GBM.
Materials and methods
Publication selection
We searched the PubMed and CNKI (China National Knowledge Infrastructure) databases for all articles within a range of published years from 2000 to 2012 on the association between MGMT promoter methylation and GBM (last search was update 20st June 2012). The following terms were used in this search: “MGMT promoter methylation” and “glioblastoma” and “survival analysis”. The meta-analysis gathered complete databases from published cohort studies dealing with the prognostic value of MGMT promoter methylation in patients with GBM who underwent surgical resection of a tumor. The language in which the papers were written was not restricted. Abstracts were excluded because of insufficient data for meta-analysis. In order to identify the relevant publications, the references cited in the research papers were also scanned. To avoid duplication of data, we carefully noted the author names and the different research centres involved. We evaluated the eligible studies if all the following conditions were met: (1) MGMT promoter methylation status were measured by using methylation-specific polymerase chain reaction (MSP); (2) surgically resected tumor tissue but not body fluids such as sputum, peritoneal fluid and serum were used; (3) inclusion of sufficient data to calculate HR and 95 % CI or inclusion of the HR and 95 % CI; and (4) full paper investigated the relationship between MGMT promoter methylation and PFS or OS.
Data extraction
Two authors (Kui Zhang and Bin Zhou) independently reviewed and extracted the data needed. Disagreements were resolved through discussion among the authors to achieve a consensus. Publications were read by Kui Zhang in order to check original data extraction. The following information was recorded for each study: first author, year of publication, region, HR form, and sample size (all of the data are shown in Table 1).
Statistical analysis
In some studies, HR and 95 % CI were directly obtained from published literature by using univariate or multivariate survival analysis. For studies in which the HR corresponding to the 95 % CI were not given directly, published data and figures from original papers were used to calculate the HR according to the methods described by Parmar et al. [11]. The pooled HR corresponding to the 95 % CI was used to assess the prognostic value of MGMT promoter methylation in patients with GBM. The statistical heterogeneity among studies was assessed with the Q-test and I2 statistics [12]. If there was no obvious heterogeneity, the fixed-effects model (the Mantel–Haenszel method) was used to estimate the pooled HR [13]; otherwise, the random-effects model (the DerSimonian and Laird method) was used [14]. The pejorative impact of MGMT promoter methylation on PFS and OS was considered to be statistically significant if the 95 % CI for the HR did not overlap 1. Publication bias was evaluated with funnel plot and Begg’s rank correlation method [15]. The statistical analyses were performed by STATA 12.0 software (Stata Corp., College Station, TX).
Results
Characteristics of studies
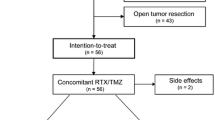
Out of a total of 109 articles were screened, 76 articles concerned topics not relevant to this study, 3 studies were excluded for determination of MGMT promoter methylation by Pyrosequencing [16–18], and finally 30 studies were available for this study. All the included studies were in English. The individual characteristics of the eligible studies are reported in Table 1. The total number of patients was 2,986, and the frequency of MGMT promoter methylation was 44.27 %. Of the 30 publications eligible for systematic review, 17 studies reported the HR corresponding to 95 % CI directly [19–35], the other 13 studies only contain survival curve [36–48] available to calculate the HR.
Meta-analysis
Five studies [24, 36, 37, 44, 47], including 462 patients, reported the effect of MGMT promoter methylation on PFS using analyses unadjusted for other factors. As shown in Fig. 1, MGMT promoter methylation was significantly correlated with better PFS according to univariate analysis, with a combined HR of 0.72 (95 % CI 0.55–0.95). The random-effects model (the DerSimonian and Laird method) was used [14] because of significant heterogeneity was detected among these studies (p = 0.002, I2 = 76.0 %). The effect of MGMT promoter methylation on PFS adjusted for other variables was evaluated in nine studies [19–23, 25, 27, 28, 34], including 957 patients. As shown in Fig. 1, MGMT promoter methylation was significantly correlated with better PFS according to multivariate analysis, with a combined HR of 0.51 (95 % CI 0.38–0.69). The random-effects model (the DerSimonian and Laird method) was used [14] because of significant heterogeneity was detected among these studies (p = 0.001, I2 = 68.6 %).
The effect of MGMT promoter methylation on OS unadjusted for other variables was evaluated in 15 studies [24, 29, 32, 37–48], including 1,409 patients. As shown in Fig. 2, MGMT promoter methylation was significantly correlated with better OS according to univariate analysis, with a combined HR of 0.67 (95 % CI 0.58–0.78). The random-effects model (the DerSimonian and Laird method) was used [14] because of significant heterogeneity was detected among these studies (p = 0.010, I2 = 52.0 %). 14 studies [19–23, 26–31, 33–35], including 1,507 patients, reported the effect of MGMT promoter methylation on OS using analyses adjusted for other factors. As shown in Fig. 2, MGMT promoter methylation was significantly correlated with better OS according to multivariate analysis, with a combined HR of 0.49 (95 % CI 0.38–0.64). The random-effects model (the DerSimonian and Laird method) was used [14] because of significant heterogeneity was detected among these studies (p < 0.001, I2 = 68.6 %).
Among 13 studies, which reported the prognostic value of MGMT promoter methylation on OS in GBM patients treated with alkylating agent, nine studies, including 653 patients, reported the effect of MGMT promoter methylation on OS using analyses unadjusted for other factors. Six studies, including 371 patients, reported the effect on OS using analyses adjusted for other factors. As shown in Fig. 3, MGMT promoter methylation were significantly correlated with better OS according to both univariate analysis and multivariate analysis, with combined HR of 0.58 (95 % CI 0.42–0.79) for univariate analysis, and combined HR of 0.42 (95 % CI 0.29–0.60) for multivariate analysis. The random-effects model (the DerSimonian and Laird method) was used [14] because of significant heterogeneity was detected among these studies (p < 0.001, I2 = 75.2 % for univariate analysis and p = 0.125, I2 = 42.1 % for multivariate analysis).
Publication bias statistics were determined, no publication bias (Begg’s test, p > 0.05) was found. Sensitivity analysis was performed to investigate the influence of a single study on the overall meta-analysis by omitting one study at a time, and the omission of any study made no significant difference, indicating that our results were statistically reliable.
Discussion
The prognostic role of a specific molecular marker is more powerful when used to help make therapeutic decisions. Despite progress in our understanding of the genetic alterations in GBM, clinically useful molecular markers predictive of the therapeutic response and prognosis are still rare. Usually, meta-analysis is used to evaluate pooled results from different randomized controlled trials.
Our meta-analysis focuses on MGMT promoter methylation in patients with GBM. Although the findings of two studies [21, 37] which reported the status of MGMT promoter methylation on PFS, and the results of nine studies [21, 29, 31, 32, 35, 37, 38, 40, 41] which reported the status of MGMT promoter methylation on OS were in the opposite direction to those observed in the meta-analysis, our meta-analysis with accumulated data suggested MGMT promoter methylation was associated with longer PFS and OS according to both univariate analyses and multivariate analyses.
MGMT protects cells against the potentially deleterious effects of alkylating agents, which include mutations, sister chromatid exchanges, recombination, and chromosomal aberrations [49, 50]. It has been shown that glial brain tumors are characterized by a low expression of MGMT, however, the activity of MGMT is commonly increased in relation to surrounding normal tissue [51, 52]. MGMT activity is partly mediated through methylation of the MGMT promoter region; this epigenetic mechanism contributes to a loss of MGMT expression [49]. Epigenetic MGMT gene silencing by promoter methylation associated with loss of MGMT expression may contribute to diminished DNA repair [53], which may be the potential mechanism that results in longer PFS and OS.
Esteller et al. [9] first determined that MGMT promoter methylation is related to the responsiveness of gliomas to carmustine (BCNU). Alkylating agents are the currently leading chemotherapeutic agents for GBM patients [2, 54]. Evaluation of prognostic factors is vital to improve research pursuing new therapies for GBM. Although 4 previous studies [29, 32, 37, 41] failed to find significant association of MGMT promoter methylation on OS in GBM patients treated with alkylating agents, our meta-analysis with pooled data suggested that MGMT promoter methylation was associated with prolonged OS in GBM patients treated with alkylating agents according to both univariate analysis and multivariate analysis. Indeed, it was demonstrated that MGMT-hypermethylated tumors were more sensitive to the killing effects of alkylating drugs, because tumor cells with low MGMT expression were unable to repair such DNA lesions and, thus, were prone to apoptosis [55].
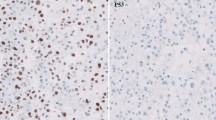
The various methods of measurement of MGMT promoter methylation sometimes show discrepant results. It is generally accepted that a methylation-specific polymerase chain reaction (MSP) evaluating the methylation status of the MGMT promoter is the best way to predict the MGMT expression of the tumor in a manner that also correlates with clinical outcome [56]. The vast majority of previous studies of MGMT promoter methylation in GBM have used MSP, which is a qualitative method. Our meta-analysis was performed under the bases of the same methods of measurement of MGMT promoter methylation, which eliminated the disparity from the method differences.
Publication bias statistics were determined, no publication bias (Begg’s test, p > 0.05) was found. Sensitivity analysis was also performed to investigate the influence of a single study on the overall meta-analysis by omitting one study at a time, and the omission of any study made no significant difference, indicating that our results were statistically reliable.
In conclusion, MGMT promoter methylation was associated with better PFS and OS in patients with GBM regardless of therapeutic intervention, and associated with longer OS in GBM patients treated with alkylating agents. Our results suggested that MGMT promoter methylation was an independent indicator of better prognosis for GBM. The presence of a methylated MGMT promoter may be a marker for response to therapy with alkylating agents.
References
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114(2):97–109. doi:10.1007/s00401-007-0243-4
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996. doi:10.1056/NEJMoa043330
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10(5):459–466. doi:10.1016/S1470-2045(09)70025-7
Parsons DW, Jones S, Zhang X et al (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321(5897):1807–1812. doi:10.1126/science.1164382
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359(5):492–507. doi:10.1056/NEJMra0708126
Pegg AE (2000) Repair of O(6)-alkylguanine by alkyltransferases. Mutat Res 462(2–3):83–100
Karran P, Bignami M (1994) DNA damage tolerance, mismatch repair and genome instability. BioEssays 16(11):833–839. doi:10.1002/bies.950161110
Gorlia T, van den Bent MJ, Hegi ME et al (2008) Nomograms for predicting survival of patients with newly diagnosed glioblastoma: prognostic factor analysis of EORTC and NCIC trial 26981–22981/CE.3. Lancet Oncol 9(1):29–38. doi:10.1016/S1470-2045(07)70384-4
Esteller M, Garcia-Foncillas J, Andion E et al (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343(19):1350–1354. doi:10.1056/NEJM200011093431901
Brell M, Tortosa A, Verger E et al (2005) Prognostic significance of O6-methylguanine-DNA methyltransferase determined by promoter hypermethylation and immunohistochemical expression in anaplastic gliomas. Clin Cancer Res 11(14):5167–5174. doi:10.1158/1078-0432.CCR-05-0230
Parmar MK, Torri V, Stewart L (1998) Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 17(24):2815–2834
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. doi:10.1002/sim.1186
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22(4):719–748
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Tang K, Jin Q, Yan W et al (2012) Clinical correlation of MGMT protein expression and promoter methylation in Chinese glioblastoma patients. Med Oncol 29(2):1292–1296. doi:10.1007/s12032-011-9901-4
Motomura K, Natsume A, Kishida Y et al (2011) Benefits of interferon-beta and temozolomide combination therapy for newly diagnosed primary glioblastoma with the unmethylated MGMT promoter: a multicenter study. Cancer 117(8):1721–1730. doi:10.1002/cncr.25637
Etcheverry A, Aubry M, de Tayrac M et al (2010) DNA methylation in glioblastoma: impact on gene expression and clinical outcome. BMC Genomics 11:701. doi:10.1186/1471-2164-11-701
Kim YS, Kim SH, Cho J et al (2012) MGMT gene promoter methylation as a potent prognostic factor in glioblastoma treated with temozolomide-based chemoradiotherapy: a Single-Institution Study. Int J Radiat Oncol Biol Phys. doi:10.1016/j.ijrobp.2011.12.086
Lechapt-Zalcman E, Levallet G, Dugue AE, et al (2012) O(6)-Methylguanine-DNA methyltransferase (MGMT) promoter methylation and low MGMT-encoded protein expression as prognostic markers in glioblastoma patients treated with biodegradable carmustine wafer implants after initial surgery followed by radiotherapy with concomitant and adjuvant temozolomide. Cancer. doi:10.1002/cncr.27441
Reifenberger G, Hentschel B, Felsberg J, et al (2011) Predictive impact of MGMT promoter methylation in glioblastoma of the elderly. Int J Cancer. doi:10.1002/ijc.27385
Felsberg J, Thon N, Eigenbrod S et al (2011) Promoter methylation and expression of MGMT and the DNA mismatch repair genes MLH1, MSH2, MSH6 and PMS2 in paired primary and recurrent glioblastomas. Int J Cancer 129(3):659–670. doi:10.1002/ijc.26083
Balana C, Carrato C, Ramirez JL et al (2011) Tumour and serum MGMT promoter methylation and protein expression in glioblastoma patients. Clin Transl Oncol 13(9):677–685
Lakomy R, Sana J, Hankeova S et al (2011) MiR-195, miR-196b, miR-181c, miR-21 expression levels and O-6-methylguanine-DNA methyltransferase methylation status are associated with clinical outcome in glioblastoma patients. Cancer Sci 102(12):2186–2190. doi:10.1111/j.1349-7006.2011.02092.x
Sonoda Y, Yokosawa M, Saito R et al (2010) O(6)-Methylguanine DNA methyltransferase determined by promoter hypermethylation and immunohistochemical expression is correlated with progression-free survival in patients with glioblastoma. Int J Clin Oncol 15(4):352–358. doi:10.1007/s10147-010-0065-6
Minniti G, Salvati M, Arcella A et al (2011) Correlation between O6-methylguanine-DNA methyltransferase and survival in elderly patients with glioblastoma treated with radiotherapy plus concomitant and adjuvant temozolomide. J Neurooncol 102(2):311–316. doi:10.1007/s11060-010-0324-4
Thon N, Eigenbrod S, Grasbon-Frodl EM et al (2011) Predominant influence of MGMT methylation in non-resectable glioblastoma after radiotherapy plus temozolomide. J Neurol Neurosurg Psychiatry 82(4):441–446. doi:10.1136/jnnp.2010.214593
Weller M, Felsberg J, Hartmann C et al (2009) Molecular predictors of progression-free and overall survival in patients with newly diagnosed glioblastoma: a prospective translational study of the German Glioma Network. J Clin Oncol 27(34):5743–5750. doi:10.1200/JCO.2009.23.0805
Wemmert S, Bettscheider M, Alt S et al (2009) p15 promoter methylation—a novel prognostic marker in glioblastoma patients. Int J Oncol 34(6):1743–1748
Hegi ME, Diserens AC, Godard S et al (2004) Clinical trial substantiates the predictive value of O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated with temozolomide. Clin Cancer Res 10(6):1871–1874
Zawlik I, Vaccarella S, Kita D, Mittelbronn M, Franceschi S, Ohgaki H (2009) Promoter methylation and polymorphisms of the MGMT gene in glioblastomas: a population-based study. Neuroepidemiology 32(1):21–29. doi:10.1159/000170088
Park CK, Park SH, Lee SH et al (2009) Methylation status of the MGMT gene promoter fails to predict the clinical outcome of glioblastoma patients treated with ACNU plus cisplatin. Neuropathology 29(4):443–449. doi:10.1111/j.1440-1789.2008.00998.x
Sonoda Y, Kumabe T, Watanabe M et al (2009) Long-term survivors of glioblastoma: clinical features and molecular analysis. Acta Neurochir 151(11):1349–1358. doi:10.1007/s00701-009-0387-1
Metellus P, Coulibaly B, Nanni I et al (2009) Prognostic impact of O6-methylguanine-DNA methyltransferase silencing in patients with recurrent glioblastoma multiforme who undergo surgery and carmustine wafer implantation: a prospective patient cohort. Cancer 115(20):4783–4794. doi:10.1002/cncr.24546
Cao VT, Jung TY, Jung S et al (2009) The correlation and prognostic significance of MGMT promoter methylation and MGMT protein in glioblastomas. Neurosurgery 65(5):866–75; discussion 75. doi:10.1227/01.NEU.0000357325.90347.A1
Christians A, Hartmann C, Benner A et al (2012) Prognostic value of three different methods of MGMT promoter methylation analysis in a prospective trial on newly diagnosed glioblastoma. PLoS One 7(3):e33449. doi:10.1371/journal.pone.0033449
Combs SE, Rieken S, Wick W et al (2011) Prognostic significance of IDH-1 and MGMT in patients with glioblastoma: one step forward and one step back? Radiat Oncol 6:115. doi:10.1186/1748-717X-6-115
Yang SH, Lee KS, Yang HJ et al (2012) O(6)-Methylguanine-DNA-methyltransferase promoter methylation assessment by microdissection-assisted methylation-specific PCR and high resolution melting analysis in patients with glioblastomas. J Neurooncol 106(2):243–250. doi:10.1007/s11060-011-0668-4
Ellingson BM, Cloughesy TF, Pope WB et al (2012) Anatomic localization of O6-methylguanine DNA methyltransferase (MGMT) promoter methylated and unmethylated tumors: a radiographic study in 358 de novo human glioblastomas. NeuroImage 59(2):908–916. doi:10.1016/j.neuroimage.2011.09.076
Park CK, Kim J, Yim SY et al (2011) Usefulness of MS-MLPA for detection of MGMT promoter methylation in the evaluation of pseudoprogression in glioblastoma patients. Neuro-oncology 13(2):195–202. doi:10.1093/neuonc/noq162
Costa BM, Caeiro C, Guimaraes I et al (2010) Prognostic value of MGMT promoter methylation in glioblastoma patients treated with temozolomide-based chemoradiation: a Portuguese multicentre study. Oncol Rep 23(6):1655–1662
Brandes AA, Franceschi E, Tosoni A et al (2010) O(6)-Methylguanine DNA-methyltransferase methylation status can change between first surgery for newly diagnosed glioblastoma and second surgery for recurrence: clinical implications. Neuro-oncology 12(3):283–288. doi:10.1093/neuonc/nop050
Morandi L, Franceschi E, de Biase D et al (2010) Promoter methylation analysis of O6-methylguanine-DNA methyltransferase in glioblastoma: detection by locked nucleic acid based quantitative PCR using an imprinted gene (SNURF) as a reference. BMC Cancer 10:48. doi:10.1186/1471-2407-10-48
Rivera AL, Pelloski CE, Gilbert MR et al (2010) MGMT promoter methylation is predictive of response to radiotherapy and prognostic in the absence of adjuvant alkylating chemotherapy for glioblastoma. Neuro-oncology 12(2):116–121. doi:10.1093/neuonc/nop020
Zunarelli E, Bigiani N, Sartori G, Migaldi M, Sgambato A, Maiorana A (2011) INI1 immunohistochemical expression in glioblastoma: correlation with MGMT gene promoter methylation status and patient survival. Pathology 43(1):17–23. doi:10.1097/PAT.0b013e328340bb26
Karayan-Tapon L, Quillien V, Guilhot J et al (2010) Prognostic value of O6-methylguanine-DNA methyltransferase status in glioblastoma patients, assessed by five different methods. J Neurooncol 97(3):311–322. doi:10.1007/s11060-009-0031-1
Brandes AA, Franceschi E, Tosoni A et al (2009) Temozolomide concomitant and adjuvant to radiotherapy in elderly patients with glioblastoma: correlation with MGMT promoter methylation status. Cancer 115(15):3512–3518. doi:10.1002/cncr.24406
Smith KA, Ashby LS, Gonzalez LF et al (2008) Prospective trial of gross-total resection with Gliadel wafers followed by early postoperative Gamma Knife radiosurgery and conformal fractionated radiotherapy as the initial treatment for patients with radiographically suspected, newly diagnosed glioblastoma multiforme. J Neurosurg 109(Suppl):106–117. doi:10.3171/JNS/2008/109/12/S17
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG (1999) Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59(4):793–797
Kim JI, Suh JT, Choi KU et al (2009) Inactivation of O6-methylguanine-DNA methyltransferase in soft tissue sarcomas: association with K-ras mutations. Hum Pathol 40(7):934–941. doi:10.1016/j.humpath.2009.01.005
Citron M, Decker R, Chen S et al (1991) O6-Methylguanine-DNA methyltransferase in human normal and tumor tissue from brain, lung, and ovary. Cancer Res 51(16):4131–4134
Silber JR, Mueller BA, Ewers TG, Berger MS (1993) Comparison of O6-methylguanine-DNA methyltransferase activity in brain tumors and adjacent normal brain. Cancer Res 53(14):3416–3420
Chakravarti A, Erkkinen MG, Nestler U et al (2006) Temozolomide-mediated radiation enhancement in glioblastoma: a report on underlying mechanisms. Clin Cancer Res 12(15):4738–4746. doi:10.1158/1078-0432.CCR-06-0596
Nishikawa R (2010) Standard therapy for glioblastoma—a review of where we are. Neurol Med Chir 50(9):713–719
Hegi ME, Diserens AC, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352(10):997–1003. doi:10.1056/NEJMoa043331
Idbaih A, Omuro A, Ducray F, Hoang-Xuan K (2007) Molecular genetic markers as predictors of response to chemotherapy in gliomas. Curr Opin Oncol 19(6):606–611. doi:10.1097/CCO.0b013e3282f075f3
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Kui Zhang, Xiao-qin Wang and Bin Zhou contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, K., Wang, Xq., Zhou, B. et al. The prognostic value of MGMT promoter methylation in Glioblastoma multiforme: a meta-analysis. Familial Cancer 12, 449–458 (2013). https://doi.org/10.1007/s10689-013-9607-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-013-9607-1