Abstract
Identifying new methods to deliver cancer genetic counseling (GC) are needed to meet the growing interest in BRCA1/2 testing. The goal of this pilot feasibility study was designed to test the initial acceptability of group GC on selected patient outcomes (satisfaction, distress, perceived control) in a breast/ovarian cancer genetics clinic setting. Sixty-five participants at increased risk for hereditary breast/ovarian cancer (HBOC) agreed to participate in self-selected individual or group GC appointments. Forty-nine participants completed all study questionnaires and were included in the analyses. There were significant improvements for participants in both the individual and group GC formats with regard to perceived personal control, general psychological distress and cancer-specific psychological distress scores. Participants in both the individual and group formats reported high satisfaction scores on the Genetic Counseling Satisfaction Scale. Study results suggest that group GC may be feasible and acceptable to high-risk women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 209,060 new cases of breast cancer and 21,880 new cases of ovarian cancer will occur in the US in 2010 [1]. Breast cancer is the most commonly occurring cancer and second leading cause of death in women in the US, and ovarian cancer is among the top 10 most common cancers in women and the 4th leading cause of cancer deaths [1]. The US Preventative Task Force recommends genetic counseling (GC) for women with specific family history patterns suggesting an increased risk for developing breast cancer (40–66% lifetime risk) or ovarian cancer (13–40% lifetime risk) associated with BRCA1 or BRCA2 mutations [2, 3]. Consensus-approved guidelines recommend that these women would benefit from genetic counseling that allows informed decision-making about genetic testing and further screening and risk reducing surgery.
GC is a communication process that assists in helping individuals understand, assess, and use risk information to enhance decision-making for health care [4]. The current standard of care is for GC to be completed in-person using an individual format (with the option to allow other family members to attend) to provide psychosocial education and counseling to facilitate autonomous decision making [5]. However, this can be appreciably time intensive. Additionally, in some areas, there is limited access to genetic healthcare professionals and specialized multidisciplinary risk evaluation clinics and as such, more efficient methods of delivering GC are needed [6–8].
Individual GC in the cancer genetics setting is the current standard of care and well supported as an effective modality in terms of satisfaction, patient knowledge, changes in risk perception, reduced anxiety, and promoting early detection and primary prevention behaviors [9–12], which are often used as indictors of healthcare quality and effectiveness of cancer GC services [13]. Individual GC allows tailoring of information based on individual risk factors and psychosocial needs [14, 15]. However, there is limited evidence to support the notion that the needs of individuals who seek cancer GC can only be met through an individual counseling approach [16].
Other strategies for improving access and efficiency of genetic services have been investigated. For example, providing educational materials, videos, and computer-assisted learning before the cancer GC appointment have demonstrated increased knowledge and risk recall among counselees and a reduction in genetic counseling session length [17–20]. Telephone counseling has also been successfully used as an alternative to in-person cancer GC to increase access to services; however, its equivalency or non-inferiority to in-person counseling has not been established in high-risk populations [17]. In addition, research indicates that some women still prefer in-person interactions over other methods such as telephone counseling [17, 20]. Alternative models to individual cancer GC that address the growing interest in these services are needed [11].
Research supporting the use of groups for counseling and psychotherapy has provided convincing evidence for achieving positive individual outcomes [21]. One of the most cited reasons for the effectiveness of groups in counseling is due to the group-level influences [22]. The group format offers additional benefits when compared to individual counseling [23, 24]. The opportunities for listening to others and sharing personal experiences, concerns and/or questions may not only allow others to feel supported, but may also allow individuals to think more about their decisions and future courses of action [25, 26]. In addition, the group environment provides additional opportunities for disclosure, bonding, and therapeutic support that lead to positive patient outcomes [27]. Unlike other types of clinical counseling, a group approach has not been widely implemented as a means to deliver cancer GC services.
To our knowledge, only two studies have assessed the impact of group GC and found similar results when compared to individual sessions [6, 16]. Calzone et al. [6] randomly assigned 142 women who were considered to be at increased for hereditary breast/ovarian cancer (HBOC) to group or individual education and counseling sessions. The group education included brief individual counseling immediately following the session. Group sizes ranged from two to 10 patients with a mean of 4.82 patients. Results indicated that participants were equally satisfied with either method even though significantly less time per patient was spent with the group sessions (1.25 h for individual sessions and .74 h for group sessions for total counseling time) [6]. A pilot study analyzed seven group GC sessions (group sizes ranged from 2 to 4 participants) in which participants self-selected the type of counseling format (individual or group) [16]. Similar to the Calzone et al. study, patient satisfaction scores for groups were similar to the individual GC sessions, but a significant proportion chose individual counseling when given the option. In addition, some groups were small (n = 2) and may not be representative of an actual group format. Both studies indicated that there may be additional benefits available to patients through the group format such as social support but these factors were not measured [6, 16].
Cancer genetic counseling formats that meet the growing interest of genetic testing while still promoting discussion and informed decision-making are needed in this rapidly changing medical environment [8]. Therefore, the purpose of this study was to conduct an assessment of cognitive and affective outcomes with group and individual cancer GC participants on knowledge, perceived personal control, cancer specific and general distress as well as feasibility data (recruitment, adherence, attrition, logistical problems).
Methods
Study design
A modified patient preference design was employed instead of randomization for this study because the authors did want to employ a control group until more data on the acceptability of group GC was collected in this setting [16]. Seeking GC and/or testing among women with a family or personal history of breast and ovarian cancer can be an emotional and stressful event. Incorporating a pure or a wait list control group could add to these stressors. Therefore, participants were given the option for their preferred format for GC. The goal of this pilot feasibility study was to test the initial acceptability of group GC on patient outcomes. Information about why a participant chose one format over another was not collected. It is important to note, that it is not possible to conclude that the two delivery formats are equivalent in efficacy because of the wide variation for both individual and group formats, and the study was not designed to test equivalency. Although the outcomes from group and individual sessions cannot be directly compared, our findings provide feasibility data on acceptability of the group format and give impetus for further examination of group GC as a potential method for providing GC services. We hypothesized that participants in the group sessions will report similar results as participants in the individual GC sessions.
Sample and recruitment
The study was approved by the University of Utah Institutional Review Board. Participants were recruited through the Family Cancer Assessment Clinic (FCAC) at Huntsman Cancer Institute in Salt Lake City, Utah. Cancer patients and at-risk relatives were either self or physician referred. New referrals to FCAC were screened for study eligibility by the clinic coordinator, with additional review available by the genetic counselors as needed. Women with breast and/or ovarian cancer who met a modified version of the National Comprehensive Cancer Network guidelines (Table 1) for BRCA1/2 testing and women without a personal history of breast or ovarian cancer who were considered have a 25 or 50% a priori risk for having a familial BRCA1/2 mutation were included. Additional criteria for eligibility were female, English speaking and at least 18 years of age. As part of routine clinical services, the FCAC offers both the group and individual GC formats for discussions regarding cancer risk and BRCA1/2 genetic testing. Study participants were offered both counseling options and allowed to schedule an appointment in the setting they preferred. Newly diagnosed patients who were seeking testing to facilitate urgent treatment planning were excluded.
Participants were mailed information about the study, the consent form, baseline study questionnaire, and the clinic’s new patient documents that contained family and medical history questionnaires. The scripted letter explained that there were two available genetic counseling formats through this study (i.e., group and individual) and that we were interested in assessing patient responses to these two formats. The letter also explained what was required of them if they chose to enroll in the study and that participation would not change or alter the clinical services as they normally occur. Individuals interested in participating were asked to return the consent form and baseline study questionnaire prior to their appointment. The information was completed and returned approximately 2 weeks before the GC appointment. Participants were then asked to complete a post-session questionnaire immediately following the GC appointment. Only individuals who signed the consent form and completed the pre-session and post-session questionnaires were included in this study. Seventy-four recruitment packets were sent out between November 2007 and October 2008, and 65 were returned (44 participated in the individual sessions and 21 participated in the group session). This resulted in an 87% response rate. However, of the 65 participants that returned pre-session questionnaires, 49 (75%) completed all the post-session questionnaires and were included in the analysis. This resulted in a sample size of 32 for the individual GC sessions and 17 for the group GC sessions (group sizes ranged from 3 to 5 participants). There were no significant differences in attrition across groups in this study (P = .35; Fisher’s exact test).
Outcome measures
Socio-demographics
Information on the following variables was elicited on the baseline questionnaire: sex, age, marital status, race, ethnicity, religion, occupation, income, highest level of education, and any previous medical training.
Knowledge
Knowledge of breast cancer and genetic susceptibility were assessed at baseline and immediately following the counseling session using the Breast Cancer Genetics Knowledge Scale [28, 29]. This measure consists of nine items that use a true–false response format.
Cancer-specific distress
The impact of event scale (IES) is a 15-item measure of psychological distress measuring both intrusive and avoidant thoughts related to a stressful life event (in this study, GC process) [30–32]. In this study, the overall measure demonstrated excellent internal consistency (α = .93) as well as the two subscales (avoidance α = .93 and intrusion α = .85).
Perceived control
The perceived personal control (PPC) scale was used to measure an individual’s beliefs about being in control over genetic susceptibility to hereditary breast and ovarian cancer [33]. There are nine items ranked on a scale of 0–2. This survey has demonstrated reliability and validity [33, 34]. In the present study, reliability for the PPC demonstrated acceptable internal consistency (α = .79).
General psychological distress
The hospital anxiety and depression scale (HADS) is a 14-item scale that measures emotional distress, anxiety, and depression [35]. Scale items are rated on a four point likert-type scale (0–4). This scale has demonstrated internal consistency reliability for GC patients [36–38]. Cronbach’s alpha for the subscales were: depression subscale (α = .87) and anxiety subscale (α = .89).
Satisfaction
The six item genetic counseling satisfaction scale (GCSS) was used to measure patient satisfaction with the GC sessions [4]. The response format uses a five-item Likert scale ranging from strongly disagree (1) to strongly agree (5) [4, 39]. In this study, Cronbach’s alpha was .91.
BRCA1/2 testing
The number of participants who received genetic testing within 2 weeks of the GC appointment for both group and individual GC was documented by clinic staff. Reasons for not pursuing testing were also recorded.
Genetic counseling protocols
Participants in both the group and individual sessions completed medical, family history and psychosocial questionnaires prior to their appointment. These were reviewed by the genetic counseling team prior to the sessions to facilitate risk assessment preparation and to assess for continued study eligibility in light of potential changes to medical/family history information. Both individual and group sessions were developed to provide participants with similar information about BRCA1/2 genetic testing. Each session was delivered by one of three licensed genetic counselors certified by the American Board of Genetic Counseling who were trained in the counseling protocol. The standardized information content of the group and individual sessions included explanation of cancer risk categories including average, moderate, and high, BRCA1/2 associated cancer risks, inheritance of BRCA1/2 mutations, common cancer patterns seen in families with BRCA1/2 mutations, genetic testing logistics, potential outcomes of genetic testing and associated management recommendations, implications for relatives, and potential psychosocial responses to pursuing genetic/cancer risk knowledge.
The individual format provided risk assessment and management information that was specific to the patient’s family and personal medical history, while group participants were presented with general risk assessment information in which representative pedigrees were shown to illustrate the features common to moderate and high risk family and an overall summary of NCCN management guidelines for moderate and BRCA1/2 families. The duration of individualized counseling time in both study groups included a discussion of personal and medical history, personalized risk assessment, a description of management options based on possible genetic test results tailored to the patient’s situation, and the facilitation of the participant’s informed decision-making about BRCA1/2 testing. While these areas were covered during the one-on-one meetings with both the individual and group session participants, those in the group study arm had a limited personalized discussion of their medical/family history, risk assessment, and management options.
The individual counseling sessions were held in patient examination or consultation rooms in Huntsman Cancer Institute during business hours and did not include visual aides as with the group sessions. The group sessions were held in the evenings in a conference room located in the Huntsman Cancer Institute. Participants only attended one group session, and similar to the participants in the individual sessions, they were allowed to bring support individuals to the groups. (Support individuals were not included when reporting the group size.) Group counseling participants sat around a large central table and the visual aids were projected onto a screen. Group participants were provided with folders including paper copies of the information presented on the projected visual aides and pens so they could take notes during the presentation if desired. Participants were encouraged to ask questions during the session. One of the genetic counselors moderated the group and an additional counselor also attended the group. After the presentation, group participants had an opportunity to meet with one of the genetic counselors individually for approximately 10–15 min to answer any questions, briefly clarify/discuss the items outlined above (e.g., personal/family history, risk assessment, management options), discuss whether or not they wished to pursue testing, review and sign the genetic testing consent form (if applicable), and to make a plan for disclosing results. Phlebotomy services were available for both group and individual participants who decided to proceed with testing following their counseling appointment.
Participants in both the group and individual sessions were encouraged by the genetic counselors to ask questions throughout the session and participants were asked if they had any additional questions at the end of each session. At the end of the both individual and group sessions, the participants were offered the option to proceed with genetic testing. The average duration of the individual sessions was 63.2 min (SD = 20.39). This included the time for the counseling session. The average duration of the group presentations was 34.9 min (SD = 14.96). This calculation does not include the additional time that group participants may have spent with a genetic counselor.
Statistical analysis
Data were analyzed using SPSS Version 14.0 software. Univariate statistics were employed to test for differences (paired and independent t tests) between pre- and post-session questionnaires and if these scores differed significantly between group participants’ scores and individual participants’ scores. The two study groups were not directly compared because of the significantly different approach used for individual and group formats. It is recognized that conducting multiple t tests may inflate type I error, and produce spurious results. However, because of the exploratory nature of this study, the alpha was set at .05 for all analyses.
Results
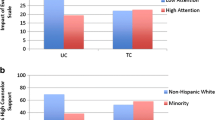
Data were initially examined for outliers and deviations from normal distribution and there were none. There were no significant differences between demographics for participants between these two groups but it is important to note that the sample size may be too small to detect statistically significant differences (Table 2). However, participants with higher income and education, and those affected with cancer and at high risk appeared to prefer individual GC. Univariate tests among the outcome measures of this study were conducted to assess if differences between pre-and post-session scores existed for participants in the group versus individual sessions. There were no significant differences between the two study groups with regard to pre-test and post-test scores.
As shown in Table 3, there were significant increases in perceived personal control for both study groups. There were also significant reductions in cancer-specific distress as measured by the IES for both study groups. However, there were no significant changes among the group GC participants on the IES avoidance subscale (P = .172), but significant reductions in avoidant thoughts among the individual GC participants were reported (P < .001; see Table 3). There were also significant reductions in the frequency of intrusive thoughts as measured by the IES Intrusion subscale for participants in both study groups. With regard to general psychological distress, there were significant improvements for the HADS total score and HADS depression subscale for both individual and group GC, and no significant improvements on the HADS anxiety subscale in either study group.
In terms of knowledge, there were no appreciable improvements in either study group (Table 4), but pre-tests scores indicated that knowledge was relatively high before counseling sessions. Regarding only post-GC satisfaction both study groups reported similarly high satisfaction scores (individual GC = 4.54/5.0 and group GC = 4.55/5.0).
Genetic testing rates differed across groups (P = .03; Fisher’s exact test). Seventy-eight percent of women who received individual GC and 47% who received group GC had BRCA1/2 gene testing. Lack of adequate insurance coverage was the most common reason for declining testing in both groups (see Table 5).
Discussion
The study’s design did not allow for a direct comparison of the outcomes of interest across the two groups examined. The two counseling formats differ in the delivery of information and amount of emphasis on the counseling components. For example, in the group GC sessions, more time was allocated to provision of information (i.e., education) with less time allotted to the personalized counseling component and included a visual presentation with handouts. However, the study’s purpose was to test feasibility and acceptability of the group format among individuals seeking genetic counseling. Participants who attended individual GC sessions around the same time period as the group GC participants were included to allow comparison of patient outcomes with the literature.
Our study examined patient outcomes in women presenting for genetic counseling for HBOC who attended group or individual GC sessions. Consistent with the study by Calzone et al. [6] that randomly assigned participants to group or individual GC sessions, this study found no differences in outcomes on psychological sequelae, preferred method of GC and satisfaction between study group, but the results did differ in that there were significant differences between the two groups in genetic testing uptake [6]. Our study also reinforced results from Ridge et al. [16] that most women, when give the option, preferred individual GC. Contrary to theses two studies, the results in this study did not demonstrate significant improvements on knowledge for participants in both groups [6, 16]. In the present study, participants who attended a group or individual session were highly satisfied and levels of satisfaction were similar between the two groups. Hass [40] has termed satisfaction as what is expected compared to what was received during the counseling process. If expectations of the GC session are concordant with services received then the GC process can be characterized as effective [40]. Participants also reported significant improvements in perceptions of personal control after attending either session. Clients who gain a greater sense of control to use genetic information in a personal meaningful way are more satisfied with the process of GC which can minimizes psychological distress [41].
Decreases in cancer-specific distress on the IES overall scale and the IES intrusion subscale were also observed among the participants in both GC formats in this study. However, on the IES avoidance subscale, there was a significant decrease on the IES avoidance subscale for participants in the individual GC format, but not for participants in the group GC format. The reason for this is unclear. Prior research supports that individuals who choose the group format may feel more comfortable addressing concerns in the presence of other individuals and this may translate into less avoidance of stressful thoughts associated with genetic testing for HBOC [33]. However, this needs to be further explored in future research.
Several studies have shown that on average women who seek GC for hereditary breast or ovarian cancer have low or moderate clinically significant levels of anxiety and depression and this study’s findings were similar to other studies with patients seeking GC in that both the anxiety and depression scores were low before counseling and showed significant improvements following GC [42, 43]. A cut-off score of eight or higher on each sub-scale is an indication of depression or anxiety disorder [44]. In a study that compared mean scores on the HADS subscales for women with and without cancer seeking GC to population data, our findings report higher mean scores, but still below the cut-off score. Normative mean scores for women with cancer for anxiety and depression were 4.7 and 3.5 and for women without cancer they were 4.6 and 3.1 respectively [45]. A reason for the higher scores in this study may have been that the participants were not self-referred for GC and therefore, may have less motivation or feelings of lack control over their situation which are common symptoms related to depression and anxiety [45, 46]. It is still important to note that there is still a small portion of women with moderate to high levels and these levels decline following genetic counseling [36].
Interestingly, participants in the group sessions demonstrated a decreasing trend on the HADS anxiety subscale. The reason for this is unclear but one possible explanation is those in the group sessions had the opportunity to interact with others going through a similar process. According to Uncertainty Reduction Theory, small group formats are theorized to reduce uncertainty through mechanisms of social support such as conversing with each other, sharing personal information and discussing future plans [47]. A prior study found that reduction in uncertainty was associated with improvements on other psychosocial variables such as anxiety and stress as observed in prostate cancer support groups [48]. However, future studies may wish to examine how levels of anxiety and depression may change after receiving the genetic test result. Calzone et al. [6] found increased IES scores for women with positive mutations who attended either individual or group GC.
There were no significant improvements in knowledge for participants who participated in this study. This in part may be due to the high knowledge levels found in pre-session scores. The pre-session questionnaires were mailed with the clinic’s new patient documents that contained some information about genetic counseling for HBOC. This may have influenced participants’ responses to the pre-session questionnaire. Future research may wish to collect pre-session questionnaires separately or use a different knowledge measure with this population.
Although the results of this study are consistent with prior research on group GC for familial breast and ovarian cancer, future research should include process measures of the counseling experience [49]. There may be other factors within the group or individual setting that influence outcomes. Research on small groups involving counseling and psychotherapy has advanced from assessment of effectiveness and efficacy to more complex research examining communication processes and group-level factors for improving clinical outcomes. Group-level factors (group climate, cohesion, therapeutic alliance) and impact of leader behaviors have been found to have a significant influence on patient outcomes [21]. For example, group conflict was highlighted as an issue in another study on group GC [16]. In two of the groups, one participant was verbal about their frustration with the testing process and the genetic counselors leading the groups found it difficult to address these individual needs and the rest of the group. Another influence from the group setting that may need to be considered is the influence of the group on individual decision making. One of the main goals of GC is to facilitate autonomous decision-making [50]. Within therapeutic groups, group influence is viewed as a benefit of the group [51]. In the context of GC, this may be problematic and identifying ways to help genetic healthcare professionals moderate groups without the group influencing autonomous decision-making may be needed [16]. Including process measures may capture some of these dynamics during the GC session.
Other ways to measure the process of GC may stem from qualitative methodologies. Both group and individual GC sessions could be recorded and analyzed using content analyses or coding systems to understand how the genetic healthcare professional may influence the process based on their communication style. For example, despite the format utilized for providing GC (individual or group), outcomes may be more influenced by the degree of patient-centered communication occurring between the genetic healthcare professional and counselee(s) during the session. Patient-centered communication is associated with improved satisfaction, health status and adherence from health care encounters [52–54]. Perceptions of patient-centered communication may be a more significant factor on outcomes related to the GC process than the format type and might be important process outcome in future research. Finally, it would be interesting for future research to assess the impact of group GC on the development of social networks and support, and how they may influence patient outcomes and testing decisions.
Conclusions
The demand for genetic counseling and testing continues to increase in all areas of health care. Only providing one format for GC may not be sufficient to meet the ever changing demands of personalized medicine and increasing demand for clinical cancer genetic services [17]. Continuously monitoring and improving the quality of GC services is a high priority [49]. An understanding of the process and format of service delivery is important for effective counseling [6]. Comparative effectiveness studies are needed to make sure alternate formats are not inferior and are safe and effective as individual GC.
Study limitations
This study has several limitations; foremost is the study design. The participants in this study self-selected which group they would attend and thus lacked randomization. In addition, the group sessions were offered in the evening while individual appointments were offered during the day. Preference for an evening versus daytime appointment may have also contributed to participants’ choices of group versus individual GC rather than a preference or avoidance of a particular counseling format. Reasons why participants choose a specific format over another were not collected. However, a study conducted by Ridge et al. [16] identified reasons for not attending a group GC session: the need for confidentiality, too old for a group experience, a private person, intimidated by strangers, and too emotional or anxious about risk of cancer. In addition, the two formats of GC are substantially different in the delivery of information and emphasis on counseling components thereby making it difficult to directly compare these two formats. It could also be argued that the group GC participants received both group GC and individual GC because of the opportunity for a one-on-one 15 min session with the counselor after the group component. Similarly, greater availability of appointment options may have contributed to participants overall satisfaction. A portion of the clinic volume is newly diagnosed breast cancer patients who are seeking GC and genetic testing to make urgent surgical decisions. These patients were excluded from the study because they were frequently offered the next available appointment slot or an appointment slot outside of regular clinic times. This limited the number of patients available for recruitment within the timeframe for this study. The small sample size also limited statistical power and multiple t tests were conducted that could have inflated type I error. Most of the women in this study were non-Latina white and were recruited from one university-based high-risk clinic; thereby limiting the generalizability of the study’s findings. Finally, there are other possible confounding variables that could distort the results such as the differences in socio-economic status between the participants, only one group was provided visual information (group GC), evening sessions for one group (group GC) versus day sessions for the other group (individual GC), and the influence of a particularly verbal patient in the group GC that was not present in the individual GC. More research is warranted with larger samples and random assignment to validate these initial findings. However, despite these limitations, this study draws attention to the acceptability of group GC based on the similar outcomes on perceived control, satisfaction, general and cancer-specific distress between participants in the individual or group GC among the participants in this study, and extends previous findings on the use of group GC by incorporation of the measures of perceived personal control and HADS.
Practice implications
Our study’s findings suggest that a group GC approach with brief individual follow-up counseling (10–15 min) is feasible and acceptable format that may be considered for the delivery of genetic counseling in clinical cancer genetics clinics. Group counseling is a highly utilized and recognized approach to counseling within a variety of disciplines. Findings from prior research [6, 16] suggest that group GC, may serve as a safe and effective approach to GC for BRCA1/2 testing. However, additional research on groups in counseling and psychotherapy is needed. Future work should employ randomized design and stringent quality control methods to assess intervention fidelity [49]. In addition, inclusion of communication process measures in such research will increase knowledge about ways to improve and refine the delivery of group GC.
Abbreviations
- GC:
-
Genetic counseling
- HBOC:
-
Hereditary breast/ovarian cancer
- FCAC:
-
Family cancer assessment clinic
- IES:
-
Impact of event scale
- PPC:
-
Perceived personal control
- HADS:
-
Hospital anxiety and depression scale
- GCSS:
-
Genetic counseling satisfaction scale
References
ACS (2010) American cancer society: cancer facts and figures 2010. Author, Atlanta
USPSTF (2005) U.S. preventative services task force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Ann Intern Med 143:355–361
Chen S, Parmigiani G (2007) Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 25:1329–1333
DeMarco TA et al (2004) Patient satisfaction with genetic counseling: a psychometric analysis of the genetic counseling satisfaction scale. J Genet Couns 13(4):292–304
Bennet RL et al (2003) Genetic counselors: translating genomic science into practice. J Clin Invest 112:1274–1279
Calzone KA et al (2005) Randomized comparison of group versus individual genetic education and counseling for familial breast and/or ovarian cancer. J Clin Oncol 23(15):3455–3464
Freedman AN et al (2003) US physicians’ attitudes toward genetic testing for cancer susceptability. Am J Med Genet A 120:63–71
Lea DH (2006) Expanding nurses’ roles in telemedicine and genetic services. Am J Matern Child Nurs 31(3):185–189
Braithwaite D et al (2006) Psychological impact of genetic counseling for familial cancer: a systematic review and meta-analysis. Fam Cancer 5(1):61–75
Miller S et al (2005) Enhanced counseling for women undergoing BRCA1/2 testing: impact on subsequent decision making about risk reduction behaviors. Health Educ Behav 32(5):654–667
Pieterse A et al (2005) Initial cancer genetic counseling consultation: change in counselees’ cognitions and anxiety, and association with addressing their needs and preferences. Am J Med Genet 137(1):27–35
Matloff ET et al (2006) Healthy women with a family history of breast cancer: impact of tailored genetic counseling intervention on risk perception, knowledge, and menopausal therapy decision making. J Women’s Health 15(7):843–856
Nordin K et al (2002) Coping style, psychological distress, risk perception, and satisfaction in subjects attending genetic counseling for hereditary cancer. J Med Gen 39:689–694
den Heijer M et al. (2010) The contribution of self-esteem and self-concept in psychological distress in women at risk of hereditary breast cancer. Psycho-oncology. doi:10.1002/pon.1824
Lerman C et al (1997) Controlled trial of pretest education approaches to enhance informed decision-making for BRCa1 genet testing. J Natl Cancer Inst 89:148–157
Ridge Y et al (2009) Evaluation of group genetic counseling for hereditary breast and ovarian cancer. J Genet Couns 18:87–100
Helmes AW, Culver JO, Bowen DJ (2006) Results of a randomized study of telephone versus in-person breast cancer risk counseling. Patient Educ Couns 64:96–103
Skinner CS et al (2002) Pre-counseling education materials for BRCA testing: does tailoring make a difference? Genet Test 6:93–105
Cull A et al (1998) The use of videotaped information in cancer genetic counseling: a randomized evaluation study. Br J Cancer 77:830–837
Green MJ et al (2001) Education about genetic testing for breast cancer susceptibility: patient preferences for a computer program or genetic counselor. Am J Med Genet 103:24–31
Burlingame GM, Fuhriman AJ, Johnson J (2004) Process and outcome in group counseling and psychotherapy: a perspective. In: DeLucia-Waack J et al (eds) Handbook of group counseling and psychotherapy. Sage, Thousand Oaks, pp 49–61
Lieberman MA, Golant M, Altman T (2004) Therapeutic norms and patient benefit: cancer patients in professionally directed support groups. Group Dyn 8(4):265–276
Beck AP, Lewis CM (eds) (2000) The process of group psychotherapy. American Psychologcial Association, Washington
Spiegel D, Classen C (2000) Group therapy for cancer patients: a research-based handbook of psychosocial care. Basic Books Inc Publishers, New York
Shaw ME (1981) Group dynamics: the psychology of small group behavior. McGraw-Hill College, New York
Wilson SR (1997) Individual versus group education: is one better? Patient Educ Couns 21(1):67–75
Shechtman Z, Toren Z (2010) The association of personal, process, and outcome variables in group counseling: testing an exploratory model. Group Dyn Theory Res Pract 14:292–303
Lerman C et al (1996) BRCA1 testing in families with hereditary breast-ovarian cancer. JAMA 275:1885–1892
Meiser B et al (2001) Long term outcomes of genetic counseling in women at increased risk of developing hereditary breast cancer. Patient Educ Couns 44:215–225
Horowitz M, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective stress. J Psychosom Med 41:209–218
Zilberg N, Weiss D, Horowitz M (1982) Impact of event scale: a cross validation study and some empirical evidence supporting a conceptual model of stress response syndromes. J Consult Clin Psychol 50(3):409–414
Spiegel D et al (1999) Group psychotherapy for recently diagnosed breast cancer patients: a multicenter feasibility study. Psycho-Oncology 8:482–493
Smets EMA et al (2006) The perceived personal control questionnaire as an outcome of genetic counseling: reliability and validity of the instrument. Am J Med Genet 140A:843–850
Berkenstadt M et al (1999) Perceived personal control (PPC): a new concept for measuring outcome of genetic counseling. Am J Med Genet 94:189–197
Johnston M, Pollard B, Hennessey P (2000) Construct validation of the hospital anxiety and depression scale with clinical populations. J Psychosom Res 48:579–584
Bjorvatn C et al (2008) Anxiety and depression among subjects attending genetic counseling for hereditary cancer. Patient Educ Couns 71:234–243
Mikkelsen J et al (2008) Psychosocial conditions of women awaiting genetic counseling: a population based study. J Genet Couns 17(3):242–251
Wakefield CE et al (2008) A randomized trial of a breast/ovarian cancer genetic testing decision aid used as a communication aid during genetic counseling. Psycho-Oncology 17:844–854
Tercyak KP et al (2001) Psychological response to prenatal genetic counseling and amniocentesis. Patient Educ Couns 43:73–84
Haas M (1999) A critique of patient satisfaction. Health Inf Manag 29:9–13
Shiloh S et al (1997) Mediating effects of perceived personal control: the case of genetic counseling. J Appl Soc Psychol 27:1146–1174
Tercyak KP et al (2004) Women’s satisfaction with genetic counseling for hereditary breast-ovarian cancer: psychological aspects. Am J Med Genet 131:36–41
Schwartz MD et al (2002) Impact of BRCA1/BRCA2 mutation testing on psychologic distress in a clinic-based sample. J Clin Oncol 20:514–520
Bjelland I et al (2002) The validity of the hospital anxiety and depression scale; an updated literature. J Psychosom Med 52:69–77
Reichelt JG et al (2004) BRCA1 testing with definitive results: a prospective study of psychological distress in a large clinic-based sample. Familial Cancer 3:21–28
Lerman C et al (2002) Genetic testing: psychological aspects and implications. J Consult Clin Psychol 70:784–797
Berger CR (1979) Beyond initial interaction: uncertainty, understanding, and the development of interpersonal relationships. In: Giles H, St.Clair RN (eds) Language and social psychology. Lawrence Erlbaum, Hillsdale, pp 41–67
Arrington MI (2010) Theorizing about social support and health communication in a prostate cancer support group. J Psychosoc Oncol 28:260–268
Biesecker BB, Peters KF (2001) Process studies in genetic counseling: peering into the black box. Am J Med Genet 106:191–198
Wang C, Gonzales R, Merajver DS (2004) Assessment of genetic testing and related counseling services: current research and future directions. Soc Sci Med 58:1427–1442
Lepore SJ et al (2003) Improving quality of life in men with prostate cancer: a randomized controlled trial of group education interventions. Health Psychol 22:443–452
Derkx HP et al (2009) Quality of communication during telephone triage at Dutch out of hours centres. Patient Educ Couns 74:174–178
DiMatteo MR (2003) Future directions in research on consumer-provider communication and adherence to cancer prevention and treatment. Patient Educ Couns 50(1):23–26
Stewert M et al (2000) The impact of patient-centered care on outcomes. J Fam Pract 49(9):796–804
Acknowledgments
We acknowledge the support from the Huntsman Cancer Foundation and the use of core facilities supported by the P30 CA0421014 awarded to the Huntsman Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rothwell, E., Kohlmann, W., Jasperson, K. et al. Patient outcomes associated with group and individual genetic counseling formats. Familial Cancer 11, 97–106 (2012). https://doi.org/10.1007/s10689-011-9486-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-011-9486-2