Abstract
Members of families affected by hereditary cancer are often concerned about passing on risk to offspring. Preimplantation genetic diagnosis is a procedure performed to identify embryos that inherit mutations placing them at risk for hereditary conditions. Little is known about attitudes toward the use of this technology among individuals at risk for hereditary breast and ovarian cancer. We sought to determine high risk women’s attitudes. This study is a qualitative examination of comments from women who participated in an online survey regarding knowledge and attitudes of preimplantation genetic diagnosis among individuals affected by hereditary breast and ovarian cancer. More than half the respondents held less favorable attitudes about the use of preimplantation genetic diagnosis for hereditary breast and ovarian cancer for both themselves and others. However, among the women who felt favorable about its usage, the majority said it became a new option for them to pursue parenthood whereas previously they had opted to not have a biological child. The high percentage of respondents who have never heard of preimplantation genetic diagnosis and who were in favor of this technology for hereditary breast and ovarian cancer indicates the need for educational campaigns to increase awareness and provide information about the procedure, access and affordability. Further research is needed to determine how this population would like this information presented to them and how best to instruct health care professionals to present this topic to women who do not know to ask about it.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The majority of hereditary breast cancers are associated with mutations in BRCA1 and BRCA2 (BRCA1/2) tumor suppressor genes [1, 2]. Women who carry a BRCA1/2 mutation face up to an 80% lifetime risk of developing breast cancer and up to a 40% lifetime risk of developing ovarian cancer. This risk far exceeds the risks in the general population (13% for breast cancer and 1.5% for ovarian cancer) [3–8] and the age of diagnosis for carriers of this predisposing gene mutation is about 10–20 years earlier than for sporadic breast cancer [3]. These genes follow an autosomal dominant inheritance pattern, usually affecting every generation of a family [3, 8].
Based on this inheritance pattern, BRCA1/2 mutation carriers have a 50% probability of passing this mutation to their children [7, 9]. Thus, women who carry BRCA1/2 mutations who are interested in having children face many difficult psychosocial issues surrounding the decision to become a biological parent [6, 7, 10]. Passing hereditary cancer risk to future offspring may be a major concern for some families affected by hereditary breast ovarian cancer (HBOC) and some may choose not to have children for fear of passing on the high risk of cancer [4, 6–8]. In a survey of 213 women of reproductive age affected by HBOC, Stanton et al. [7] found that almost 90% reported intense concern about passing the mutation to their children.
Technologies exist that allow families to avoid passing on genetic cancer risk to offspring [6, 11, 12]. Prenatal diagnosis, a general term used to describe any invasive medical procedure done to determine if a fetus has a genetic disorder, is offered to families at risk for having children with genetic disease, with the option to terminate the pregnancy to avoid offspring who carry genetic disease [3, 8, 13]. Prenatal diagnosis includes amniocentesis and chorionic villous sampling (CVS), both of which pose a small risk of miscarriage of the pregnancy.
Preimplantation genetic diagnosis (PGD) is an alternative to prenatal diagnoses that allows parents to avoid the possibility of terminating a pregnancy and/or damaging the fetus or the mother [14, 15]. This medical procedure allows fertilized embryos, created through in vitro fertilization (IVF), to be tested for genetic disorders before implantation into a women’s uterus [10, 15, 16] allowing parents the option to choose which embryos are selected for transfer to the mother [10]. During PGD, an egg is fertilized and allowed to grow for approximately three days until it reaches the eight-cell stage [10]. To test the embryo, one or two cells are removed and examined using polymerase chain reaction (PCR) or fluorescence in situ hybridization (FISH) [10]. Once the genetic status of the embryo is determined, parents can make decision about transfer [10]. PGD was first reported in medical journals in 1990 [15, 17] and almost 2,000 babies evaluated with PGD have been born since its creation [18].
PGD was initially used to allow parents to avoid having a child with a severe or deadly genetic disease [15], such as monogenic and chromosomal disorders like hemophilia, neuromuscular dystrophy, cystic fibrosis, sickle cell anemia, Huntington’s disease, and Down’s syndrome [15, 16]. Most of these diseases occur at an early age and can lead to death or severe morbidity by early adulthood [4, 19]. The applications of PGD have expanded to include cancer predisposition syndromes, a class of disorders in which having a gene mutation increases a person’s chance of developing cancer, with HBOC falling under this class of syndromes [13].
The earliest use of PGD for cancer predisposition syndromes was in 1998 with Familial Adenomatous Polyposis Coli (FAPC), a hereditary disease in which individuals develop hundreds of thousands of colon polyps throughout their lifetime, with untreated polyps developing into colon cancer [13]. Concerns have been raised about the ethics of using PGD for cancer predisposition among researchers, clinicians and the general public due to relatively late onsets and multifactorial causes of cancer, the risk of developing the disease not being absolute, the improved accuracy of prevention and early detection methods and the efficacy of risk reducing surgeries and effective treatments [3, 6, 20, 21]. While no governmental regulations exist for PGD in the US, the Human Fertilization and Embryology Authority (HFEA) in the UK approved PGD for BRCA1/2 carriers in 2006, given the lifetime risk of breast and ovarian cancer for mutation carriers is at least three times greater than those without a mutation [3]. In the absence of PGD, carriers of BRCA1/2 mutations are faced with making exceptionally difficult decisions, such as choosing whether or not to have children. PGD, in some cases, can reassure parents their offspring will be safe from the psychological trauma of living with a high risk of cancer [21, 22] and prevent further perpetuating of the hereditary cancer burden in families where a mutation is present [3].
A few studies have been conducted that assess the public’s view of PGD in general and for BRCA specifically [3, 23, 24]. As is often the case with medical technologies, reproductive technologies often outpace society’s ability to assess the psychosocial and informational needs of users and potential users [8, 25]. An article published in the New England Journal of Medicine (2006) in response to the approval of PGD for HBOC by the HFEA [3, 26], explained that a member of the British Parliament was responsible for creating the HFEA. The HFEA was formed to give protection to embryos and requires clinics to apply for a license to test for any new disease using PGD [26]. After garnering opinions from the general public on this change in policy, the HFEA approved PGD for use with cancer susceptibility genes that were less than fully penetrant. Physicians, professional societies, and patient groups welcomed the decision as it recognized it as an opportunity to reduce the likelihood of cancer and contributed to preventive medicine [26].
However, very few studies have been conducted on the attitudes and knowledge of women for whom PGD may be a consideration [4, 7, 8]. Following the approval by the HFEA of PGD for HBOC, BRCA carriers in the UK were surveyed on their views toward PGD for HBOC [4]. This quantitative study showed that women affected by HBOC were concerned about passing the mutation on to their children and felt PGD was an acceptable option for BRCA1/2 carriers [4].
Recently, two quantitative studies have been conducted on BRCA carriers in the US [7, 8]. The first study focused on overall reproductive concerns among this population, finding that few respondents would likely use PGD [7]. The second study, which focused specifically on PGD, found that respondents believe PGD is an acceptable option for individuals affected by HBOC and high risk individuals should be given information about PGD [8]. However, no study conducted to date has provided an in depth assessment of high risk women’s attitudes related to PGD. This study seeks to explore the attitudes and opinions of PGD among women in the US who have been personally affected by HBOC, including women who carry a BRCA1/2 mutation, have a strong family history of breast and/or ovarian cancer, have had cancer, or have family members with cancer.
Methods
Recruitment and data collection
This study is a qualitative examination of comments from the 446 respondents who chose to make a comment while participating in an online survey regarding knowledge, attitudes, and behaviors related to PGD among women affected by HBOC (n = 964). The online survey was conducted with FORCE (Facing Our Risk of Cancer Empowered), an organization devoted to empowering women whose family history or genetic status puts them at high risk for developing breast or ovarian cancer. This organization has a large online community that frequently posts and seeks information regarding HBOC on its website www.facingourrisk.org. We received permission from the director of FORCE to survey the online community via the listserve. The study was approved by the institutional review board and a waiver of informed consent was obtained. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and consistent with the principles of the Helsinki Declaration of the World Medical Association.
A description of the survey and instructions, along with a link to the website of the survey was forwarded to all FORCE members via email. At the end of the survey, participants had an opportunity to enter their names into a drawing for one $50 gift certificate. The survey was posted online on November 8, 2007 and remained available until January 8, 2008. Altogether, 975 members of the FORCE online community completed our survey, 446 chose to enter comments. The majority of the survey participants, (94%), were white. Forty-nine percent of the women carried a BRCA1/2 mutation or gene variant. Eighty-eight percent were over the age of 34 and 36% considered themselves Christian, 28% Catholic and 18% Jewish. Seventy-five percent were married and 71% were college graduates.
Study instrument
The study team developed a 33-question web-based survey to assess the knowledge and attitudes of women affected by HBOC towards PGD. It included seven demographic questions followed by several questions to determine BRCA1/2 carrier status. Additional questions included the use of prenatal diagnosis and other assisted reproductive technologies, and attitudes about PGD. Four questions were adapted from a telephone survey on the public’s attitudes toward reproductive technology conducted by the Genetics and Public Policy Center [23], and others were created by the study team. The survey also provided respondents with the following brief definition of PGD: Preimplantation Genetic Diagnosis (PGD) is a genetic test performed on embryos produced through in vitro fertilization and is used to determine if they are with or without gene mutation. Test results are used to inform prospective parents about the status of the embryos before transfer to a woman’s uterus [23].
For this paper, we report the results of the two sections where respondents were asked open ended questions. For the first comment section, respondents were asked if they would like to provide any additional comments after the following question: Do you think some women who have a strong personal or family history of breast or ovarian cancer may choose not to have children for fear of passing on a hereditary cancer gene mutation? The second comment section was at the end of the survey and was not in response to any specific question on the survey.
Data analysis
The qualitative comments were separated from the quantitative survey data and analyzed using a combination of hand-coding methods. Hand-coding is an established term in qualitative research signifying that coding was performed by in-depth review and re-review of qualitative data by study team members and not via a computer program [27, 28]. The content was first analyzed by placing each response in broad categories using the constant comparative method. Similar themes were organized together, dissimilar themes formed new groups for categorization and labeling [29]. From there, the research team identified new categories of themes and went through several rounds of thematic validation [28].
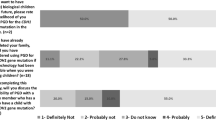
The responses under each key theme were quantified and are shown in Table 1. The research team truncated the very broad range of responses into four themes and then grouped them as favorable or unfavorable. These themes are described in the results section below. Two themes are included at the end of the section that do not fit under the Favorable or Less Favorable label. All comments were then edited so that none contained identifiable information.
Results
Favorable attitudes about PGD use for others
Among those women who had a positive or hopeful comment about PGD, the majority were focused on the possibility of this technology as being useful for others.
PGD would be a nice [option] for others, I no longer have ovaries but all the women in my family have had cancer at least twice.
I want this for my children (ages 5 & 7), I want them to have as many choices as possible.
I may be the surrogate for my sister; I would love to use PGD on the embryos.
This information just provides more options and as an ovarian cancer survivor, I believe women should be given as much information as possible. It’s a personal choice how you use the information, but we all should have it.
Favorable about PGD for self
Although only 33% of the population sample was interested in personally using PGD, the majority of this sub-population’s comments focused on a desire to take control over personal health.
This is a personal choice for me and not to judge others.
I believe this is certainly a possibility. As a BRCA carrier who underwent prophylactic surgeries at a very young age, and someone who lost female relatives at a young age, I have considered this risk and struggled to make a decision regarding children that I will feel comfortable with… I would be interested if it were affordable and available.
With a strong family history for cancer, I would seek the PGD testing. Our daughter passed away at age 13 (from a childhood cancer)… I wondered at the time of her diagnosis what right did I have to bring a child into the world to suffer as she did? I would have liked to not have passed on these genetic markers.
To have the options to prevent the suffering of my child while it is an embryo is wonderful. Praise modern medicine!
Favorable about educational aspects of informing people about PGD
Seventy-four percent (n = 154) of the comments were positive and focused on the benefits of emerging technology and the need for high risk women to be able to make their own choices about their reproductive health.
I feel like education is really key with regard to this issue. I think some individuals may or may not choose to have children for fear of passing on a hereditary cancer gene, especially if they have lost family members to cancer. It is our right to know and our choice what to do.
It is important to know that PGD is available and that we have options, it is also important to receive counseling on these issues. Education is important but dealing with diagnoses often requires counseling too.
This is something I believe to be critical. With proper information and a good estimate of the probabilities… I believe an informed choice and freedom of choice is power and affects quality of life of individual and prospective progeny.
Until this is a 100% cure with no side effects, not passing these diseases down may be a reasonable alternative. It is certainly our right to at least know about this technology.
Favorable about PGD in relation to cure
Of the 208 women who responded with a comment about PGD, 38 saw PGD as having the potential to “wipe out cancer” or reduce the familial risk within their kinship. This was represented by quite similar comments among all women in this category.
I’m not exactly sure how I feel about PGD but if it can wipe out breast and ovarian cancer than I say, go for it!!!
If I had known I carried this gene I would have had the risk reduction surgeries and would never have had children to pass this onto. The more of us that know our genetic status and use PGD, the quicker we can eliminate this gene from our pool.
I feel very, very strongly that this gene must stop being passed on, if my boys test positive and there be no cure at the time, I would like them to consider PGD.
If I had the chance to erase this mutation from my bloodline would I do it? I believe if someone who really wanted children made a decision not to have them based on their positive status PGD would be a wonderful alternative.
Unfavorable about PGD for self
Among those women who wrote unfavorable comments relating to PGD, their responses also fell into the four categories related to self, others, education, and cure. The majority of women who had an unfavorable reaction to learning about PGD were highly focused on what this option may have meant for their own mothers or for the children they already had. These women also felt strongly that HBOC was a treatable disease and not in the category of other genetic diseases with no options for prevention or treatment (e.g., Huntington’s).
These things (breast/ovarian cancer) can be diagnosed and treated early. I would hate to think my parents would have chosen not to have me if they knew I carried the gene for breast cancer.
I consider breast cancer to be curable and controllable. Thank God PGD was not around when my mother was pregnant with me and my sisters or we may not be here.
I had prenatal genetic testing when I was pregnant, if I had tested positive for a syndrome, I would have had an abortion. I would not screen for BRCA–this mutation is not a death sentence.
All humans have some form of genetic deficit; I can’t imagine life without my beautiful children… I can’t imagine they would not be allowed to live because a test when they were embryos declared them unfit.
Unfavorable about PGD for others
The majority of women who felt disapprovingly about PGD also voiced concerns in relation to others.
I do not think a woman should avoid having children if she is BRCA positive. Everyone has genetic mutations, those of us who are BRCA positive just happen to know what ours means.
I think PGD testing is sickening… I wish this technology did not exist and that no woman ever had to think about it.
Testing leads to living in fear and living in fear is a terrible thing. I understand the fear, but young women do not need more fear by knowing PGD is an option. Some things are better not known.
Unfavorable about educational aspects of informing people about PGD
Across the whole population of respondents, those who felt both favorable and unfavorable about PGD for themselves or others, there were concerns about the process of educating women. The greater part of these concerns was focused on health care professionals and the current healthcare system.
No matter what, this is a woman’s choice that must be protected by law and not influenced by a health care provider.
I think we are overly scared by Myriad labs and health care professionals–women need to be given the true facts by an unbiased, educated professional who has no agenda.
I would hate to see women reading about PGD and making decisions on their own. Everyone should get this information from a genetic counselor.
Who shall be the educators for this? Our physicians do not prevent disease, they treat it. Many physicians are reactionary and blow risk and odds ratios out of proportion.
Unfavorable about PGD in relation to future cures
About 50% of the women who wrote any comment about PGD were apprehensive about a focus on the technology in relation to a cure for breast and ovarian cancer. Some feared this technology would reduce scientific attention to cures, while others felt hopeful a cure may be found within their own children’s lifetime.
With modern technologies we may soon be able to circumvent cancer. Will focusing on this in embryos detract from a cure?
Who knows where medicine will be in 30 years when these children grow up? There may be a cure.
This is a very personal decision. I would not want to pass on the gene but I don’t know that by the time a child would have to worry about genetic heritage, a cure may have been found.
Feelings of guilt
Another theme across the comments written in the survey is one of guilt related to passing along the genetic mutation. This was manifested in terms of perceived guilt that women suspected their own parents may have had as well as their own guilt in relation to their offspring. Due to the highly personal nature of these comments we elected not to separate these comments into a category of favorable or unfavorable.
I know my mom feels guilty for having passed the gene on to me… however, I don’t think that would prevent me from having children… I have to believe that science will be significantly improved…
I worry my children may carry the mutation. I hope I gave them good genes and not BRCA but this is too tough… having cancer was hard… I do not want them to ever experience what I did… I may have been selfish to have had children.
There is a lot of guilt in our family about this. Parental guilt when passing on a mutation to children… sibling guilt when one has it and the other doesn’t… I have a relative who chose not to have children because of her fear of passing on the BRCA gene… she was determined to let it end with her.
It will break my heart to pass this to my own daughter, my hope would be that by the time she is an adult there is cure… but you can’t help feeling incredibly guilty.
Perception of irresponsibility
A few other women offered their perceptions of the “irresponsibility” of women who have children knowing there are genetic mutations in their family.
I am continually stunned when I see news programs about women who go ahead with pregnancies despite the high probability of substantial deformity or disease… they so desperately want a child… this is selfish.
I chose to be responsible. We adopted our children so the genetic mutations would not be an issue. I am amazed by the vanity of some women who have to have a biological child and know the crapshoot they are playing with the gene pool.
I think not having children if you are a carrier is a valid reason that should be honored. More women should choose this option of PGD and we should be supported, not condemned. It is irresponsible to bring a child into this world knowing you are perpetuating this terrible cancer.
One woman’s comments seemed to summarize what the majority of respondents felt:
Of course some may choose PGD, some may choose not to have children–the important thing is having the education from a qualified person–it’s all about choice. One thing we learn as cancer survivors is that life may be fleeting so hopefully it is rich. All of us could die tomorrow from a car accident and many of us will live a long time. I got this from my mother and I don’t blame her. I don’t think my children will blame me… Life is what you make of it.
Discussion
This study explored attitudes and opinions of PGD among a population of women who have a personal or family history suggestive of HBOC. Results showed more than half the respondents who commented held unfavorable attitudes and opinions about the use of PGD for HBOC for both themselves and others. Most women felt strongly PGD should not be used to eliminate embryos. However, among the women who felt favorable about the use of PGD, the majority said it provided options for them to pursue parenthood, whereas previously they had opted to refrain from having a biological child due to fear of transmitting the mutation. In addition, Shahine et al. [30], in a survey conducted among women seeking treatment for infertility, found a high rate of interest (72%) in PGD among this population.
Most of the women in our survey focused their comment on others including their family members and other women in the HBOC population. A UK survey of 52 BRCA carriers’ views on PGD for HBOC found that 75% of the women felt PGD should be offered to others with HBOC [4].
However, despite this general support, the majority of the comments from women who would consider using PGD personally focused on taking control over their health. A survey conducted by the HFEA found that, of those that agreed with PGD, the reasons for doing so were because it prevented further suffering within families where the condition is present and was a preferable technology to prenatal diagnosis [3]. Studies of the US general public, including PGD users, stress the importance of individual decision making regarding reproductive genetic technologies [19, 31, 32].
Only 20% of those surveyed were aware of PGD prior to participation. Because respondents were only provided with a short definition of PGD, it is possible they did not have a full understanding of the technique. Women were favorable about educational and counseling aspects of PGD, commenting on the need to provide education on this emerging technology for high risk women so they can make their own decisions. Offit et al. [19] explained that once individuals become aware of PGD, they should be referred for full discussion at specialized centers. Irrespective of their decision to use PGD, discussion of the option can empower members with strong family histories of cancer [19]. Women were also positive in relation to a cure for cancer, commenting they are in favor of this technology because they perceive it may stop this mutation from passing to future generations and thereby reducing cancer. A survey conducted by Staton et al. [7] on a population of women concerned about HBOC found comments from responders also focused on eliminating this mutation for future generations.
Many of the women who commented in our survey wrote unfavorable comments about PGD relating to their self and others. Most women in this category expressed anger that if this technology were available to their parents, they may have never been born. They also felt strongly that PGD should not be used for HBOC since it is treatable, unlike other diseases with no options for prevention or treatment. Menon [4] and Staton [7] also had similar comments on their surveys with respondents commenting that people affected by HBOC’s lives are not less valuable then other’s lives and they are not sorry they exist. Comments were also made suggesting PGD is not appropriate for BRCA1/2 carriers, but may be appropriate for carriers of disorders with imminent death, such as Trisomy 13 [4, 7]. A study conducted by the HFEA also found some respondents perceived PGD was acceptable for very serious genetic conditions but not for trivial reasons, however these reasons were not specified and likely vary from person to person [3]. Respondents in the HFEA survey who disagreed with PGD for any condition, typically disagreed because they did not believe in discarding embryos for any reason, perceiving it diminishes the lives of people already living in society with disabilities and genetic conditions and sends a message that people with these conditions lives may not be worth living [3].
Respondents also had strong opinions about the process of educating women on PGD, with concerns that women should not make these decisions on their own. Respondents wanted to ensure information was given by unbiased, educated health care professionals such as genetic counselors [33]. This is a realistic sentiment, especially within this population who, due to their high risk status, had likely experienced discussions with a variety of health care providers offering conflicting points of view. Several studies have reported on high risk populations perceptions of the inconsistency and complex ways in which risk and statistics have been portrayed. These studies also highlight patients/consumers questioning of the credibility and true intent of health care professionals [34–36]. Some respondents in our survey also felt apprehension toward PGD for HBOC because they thought it would detract from finding a cure for breast and ovarian cancer. Others felt hopeful that a cure would be found in their children’s lifetime. The HFEA [3] also found respondents disagreed with PGD because focusing on this technology was taking research money away from finding a treatment to make the lives of BRCA carriers easier.
Many respondents in this study expressed feelings related to guilt in terms of inheriting or passing along the mutation to their children or future children. Menon [4] also found respondents were concerned their children were carriers. Some respondents to this survey felt women who choose to have children knowing their future child is at risk for inheriting a BRCA mutation present in their family are “irresponsible”. Offit suggests guidelines and regulations need to be established for the use of PGD for cancer predisposition syndromes [19]. Because hereditary cancer is such a complex family experience, providing discussion, education, and counseling to individuals affected by HBOC can decrease the psychological burden these families experience [19].
Limitations
The results of the study should be interpreted with caution due to certain limitations. The majority of females were white, over the age of 34, college educated and considered themselves Christian. HBOC affects women of many different races, religions, and educational backgrounds, so these data may not be a representative sample of the population of women affected by HBOC. Further research is needed to explore this issue in more ethnically, religious, educational and age diverse populations. As in all qualitative research, it is difficult to generalize our results to other women who are concerned or personally affected about HBOC. It is also possible that women who are part of a single organization may have underlying characteristics that draw them to a particular community. Self-selection bias may also have been a factor because those women who chose to participate may have more of an interest in PGD than those who chose not to participate. All of the respondents were female which excluded the male perspective. Although the proportion of men who experience breast cancer is relatively low, males are carriers of BRCA mutations and may have similar feelings of guilt and concerns about the hereditary aspect of cancer. Despite the limitations, this is among the first qualitative studies to explore the attitudes and opinions of PGD among HBOC-affected individuals.
Conclusion
While many women who participated in this study had an unfavorable opinion of the use of PGD for individuals affected by HBOC, some women with a favorable opinion considered PGD as a new option for high risk women who may have previously opted to refrain from having a biological child due to fear of transmitting the mutation, whereas. Quinn et al. [8] referred to women in this population who decided not to have children as silent sufferers because they did not discuss their concerns about family history and childbearing with a health care professional and therefore were not likely aware of the technology of PGD.
The high percentage of respondents who have never heard of PGD and the high percentage who are in favor of this technology for HBOC indicates a great need for patient education to be developed regarding the mechanics and ethics of PGD. The need for educational campaigns to increase PGD awareness and provide information about the procedure, access and affordability, is high within this population.
Further research is needed to determine how this population would like this information presented to them. There is also a need to explore attitudes of PGD among health care professionals, including genetic counselors and physicians, who will most likely be the professionals discussing these issues with high risk women. Future research is needed to determine how best to instruct health care professionals to present this topic to women who do not know to ask about it. Shahine et al. [30], in a survey conducted among women seeking treatment for infertility, found a high rate of interest (72%) in PGD and participating in PGD clinical trials among IVF patients. They suggest randomized trials should be conducted on PGD before widespread application [30]. Finally, the opinion of males should also be incorporated into the development of future strategies and interventions.
Abbreviations
- BRCA1/2 :
-
Breast cancer 1 and 2 genes
- HBOC:
-
Hereditary breast and ovarian cancer
- PGD:
-
Preimplantation genetic diagnosis
- IVF:
-
In vitro fertilization
- CVS:
-
Chorionic villous sampling
- FISH:
-
Fluorescence in situ hybridization
- FAPC:
-
Familial adenomatous polyposis coli
- HFEA:
-
Human fertilization and embryology authority
- FORCE:
-
Facing our risk of cancer empowered
References
Miki Y, Swensen J, Shattuck-Eidens D et al (1994) A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science 266(5182):66–71. doi:10.1126/science.7545954
Wooster R, Bignell G, Lancaster J et al (1995) Identification of the breast cancer susceptibility gene BRCA2. Nature 378(6559):789–792. doi:10.1038/378789a0
HFEA Choices and Boundaries Report (2006) [cited Sept 15, 2007]; Available from: http://www.hfea.gov.uk/docs/Choices_and_boundaries_Report_2006.pdf
Menon U, Harper J, Sharma A, Fraser L, Burnell M, ElMasry K, Rodeck C, Jacobs I (2007) Views of BRCA gene mutation carriers on preimplantation genetic diagnosis as a reproductive option for hereditary breast and ovarian cancer. Hum Reprod 22(6):1573–1577. doi:10.1093/humrep/dem055
Weitzel J, McCaffrey S, Nedelcu R, MacDonald D, Blazer K, Cullinane C (2003) Effect of genetic cancer risk assessment on surgical decisions at breast cancer diagnosis. Arch Surg 138:1323–1328. doi:10.1001/archsurg.138.12.1323
Friedman LC, Kramer RM (2005) Reproductive issues for women with BRCA mutations. J Natl Cancer Inst Monogr 34:83–86. doi:10.1093/jncimonographs/lgi012
Staton AD, Kurian AW, Cobb K, Mills MA, Ford JM (2007) Cancer risk reduction and reproductive concerns in female BRCA1/2 mutation carriers. Fam Cancer 7:179–186
Quinn G, Vadaparampil S, Wilson C et al (2009) Attitudes of high-risk women toward preimplantation genetic diagnosis. Fertil Steril 91:2361–2368
Miki Y, Swensen J, Shattuck-Eidens D et al (1994) A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science 266:66–71. doi:10.1126/science.7545954
Ogilvie C, Braude P, Scriven P (2005) Preimplantation genetic diagnosis- an overview. J Histochem Cytochem 53:255–260. doi:10.1369/jhc.4B6395.2005
Lancaster JM, Wiseman RW, Berchuck A (1995) An inevitable dilemma: prenatal testing mutations in the BRCA1 breast-ovarian cancer susceptibility gene. Obstet Gynecol 87:306–309
Smith KR, Ellington L, Chan AY, Croyle RT, Botkin JR (2004) Fertility intentions following testing for a BRCA1 gene mutation. Cancer Epidemiol Biomarkers Prev 13(5):733–740
Ao A, Wells D, Handyside AJ, Winston RML, Delhanty JDA (1998) Preimplantation genetic diagnosis of inherited cancer: familial adenomatous polyposis coli. Genetics 15(3):140–144
Paek B (2003) Prenatal diagnosis. World J Surg 27(1):27–37. doi:10.1007/s00268-002-6734-5
Handyside AH, Kontogianni EH, Hardy K, Winston RML (1990) Pregnancies from biopsied human preimplantation embryos sexed by Y-specific DNA amplification. Nature 344:768–770
Marik JJ Preimplantation Genetic Diagnosis. E-Medicine (2005) [cited Nov 26, 2007]; Available from: http://www.emedicine.com/med/topic3520.htm#section~bibliography
Verlinsky Y, Ginsburg N, Lifchez A, Valle J, Moise J, Strom C (1990) Analysis of the first polar body: preconception genetic diagnosis. Hum Reprod 5:826–829
Zitner A (2002) The nation: cloning receives a makeover politics: nuances of language helped reframe the debate and derail an all-out ban in congress. LA Times, p A1
Offit K, Sagi M, Hurley K (2006) Preimplantation genetic diagnosis for cancer syndromes. JAMA 296:2727–2730. doi:10.1001/jama.296.22.2727
Testart J, Sele B (1995) Towards an efficient medical eugenics: is the desirable always the feasible? Hum Reprod 10(12):3086–3090
(2006) Editorial, the leading edge. Ethics of preimplantation genetic diagnosis for cancer. Lancet Oncol 7(8):611. doi:10.1016/S1470-2045(06)70768-9
Simpson JL (2001) Celebrating preimplantation genetic diagnosis of p53 mutations in Li-Fraumeni syndrome. Reprod Biomed Online 3:2–3
Hudson K (2002) Public awareness and attitudes about reproductive genetic technology. Genetics and Public Policy Center, Washington, DC
Hudson KL (2006) Preimplantation genetic diagnosis: public policy and public attitudes. Fertil Steril 85:1638–1645. doi:10.1016/j.fertnstert.2006.01.014
Woodsong C, Severy LJ (2005) Generation of knowledge for reproductive health technologies: constraints on social and behavioral research. J Soc Issues 61(1):193–205. doi:10.1111/j.0022-4537.2005.00401.x
Braude P (2006) Preimplantation diagnosis for genetic susceptibility. N Engl J Med 355:541–543. doi:10.1056/NEJMp068139
Guba EG (1978) Toward a methodology of naturalistic inquiry in educational evaluation. University of California, Los Angeles
Patton MQ (2002) Qualitative research and evaluation methods. Thousand Oaks, Sage Publications
Dye JF, Schatz IM, Rosenberg BA, Coleman ST (2000) Constant comparison method: a kaleidoscope of data. Qual Rep 4:1–2
Shahine LK, Kuppermann M, Davis G, Creasman J, Cedars MI (2008) Patient willingness to participate in a clinical trial with preimplantation genetic diagnosis. Fertil Steril 89(4):879–884
Kalfoglou AL, Doksum T et al (2005) Opinions about new reproductive genetic technologies. Fertil Steril 83:1612–1621. doi:10.1016/j.fertnstert.2005.01.090
Kalfoglou AL, Scott J, Hudson K (2005) PGD patients’ and providers’ attitudes to the use and regulation of preimplantation genetic diagnosis. Reprod Biomed Online 11:486–496
Greendale K, Pyeritz RE (2001) Empowering primary care health professionals in medical genetics: How soon? How fast? How far? Am J Med Genet C Semin Med Genet 106(3):223–232. doi:10.1002/ajmg.10010
Olsen S (2002) Cancer genetics: information source for patients and families. Cancer Pract 2:323–326. doi:10.1046/j.1523-5394.2002.106004.x
Wonderlick AL, Fine BA (1997) Knowledge of breast cancer genetics among breast cancer patients and first-degree relatives of affected individuals. J Genet Couns 6(2):111–130
Donelle L, Loffman-Goetz L, Clarke JN (2004) Portrayal of genetic risk for breast cancer. Women Health 49(4):93–111
Acknowledgments
This work is supported in part by the American Cancer Society, Atlanta, GA, RSGPB-07-019-01-CPPB. The work contained within this publication was supported in part by the Survey Methods Core Facility at the Moffitt Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Quinn, G.P., Vadaparampil, S.T., King, L.M. et al. Conflict between values and technology: perceptions of preimplantation genetic diagnosis among women at increased risk for hereditary breast and ovarian cancer. Familial Cancer 8, 441–449 (2009). https://doi.org/10.1007/s10689-009-9263-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-009-9263-7