Abstract
Diet is one of the modifiable risk factors for cognitive decline. However, human studies on total energy intake and cognitive function have remained limited and studies on fat intake and cognitive decline have been inconclusive. We aimed to examine prospectively the associations between long-term intakes of total energy and fat with subsequent subjective cognitive decline (SCD). A total of 49,493 women from the Nurses’ Health Study and 27,842 men from the Health Professionals Follow-up Study were followed for over 20 years. Average dietary intake was calculated based on repeated food frequency questionnaires (SFFQs), and Poisson regression was used to evaluate associations. Higher total energy intake was significantly associated with greater odds of SCD in both cohorts. Comparing the highest with lowest quintiles of total energy intake, the pooled multivariable-adjusted ORs (95% CIs) for a 3-unit increment in SCD, corresponding to poor versus normal SCD, was 2.77 (2.53, 2.94). Each 500 kcal/day greater intake of total energy was associated with 48% higher odds of SCD. Intakes of both total fat and total carbohydrate appeared to contribute to the positive association between total energy intake and SCD although for the same percent of energy, the association was stronger for total fat. In conclusion, higher intakes of total energy, total fat, and total carbohydrate were adversely associated with SCD. Whether these associations are causal is unclear and deserves further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia has become a leading disease burden in many countries, impacting the rapidly aging world population with enormous healthcare costs [1, 2]. To date, there are no effective treatments for dementia [3], and identification of modifiable risk factors to prevent or delay the onset and progression of this disease is of utmost importance. Subjective cognitive decline (SCD)—a state of self-perceived cognitive decline without detectable cognitive impairments by objective measures—can precede clinically apparent mild cognitive impairment and dementia [4]. Dementia-associated brain pathologies may be found on brain MRI even years before SCD is detectable [5], suggesting a long window for potential prevention [6]. Available evidence has suggested that diet is one of the modifiable risk factors for cognitive decline [7].
Calorie restriction has been used frequently to understand the mechanisms in age-related diseases [8]. In numerous animal studies, calorie restriction has increased longevity [9], delayed or prevented many chronic diseases, and improved cognitive function and late-life health [10,11,12]. However, human data on total energy intake and cognitive function remain sparse. Of the three macronutrients, fat, carbohydrates, and proteins, contributing to total energy intake, dietary fat has been of research interest because of the relationship with cholesterol metabolism, which is related to APOE ε4, the strongest genetic risk factor for Alzheimer’s disease [13]. To date, results of studies on the relationship between dietary fat and cognitive function have been inconclusive: some studies found that higher intakes of total fat, trans-fat, and saturated fats were associated with higher risk of cognitive decline and that higher intakes of unsaturated fats were associated with lower risk [14, 15], whereas other studies found null results [16] or inverse findings [17, 18]. Different methods of exposure and outcome assessment, as well as differences in the geographical locations and populations, might contribute to the discrepancies of the aforementioned study findings. Thus, in the current study, we used multiple dietary assessments from over 20 years of follow-up in two large prospective cohorts of US men and women to examine the associations between long-term total energy and fat intake with SCD.
Methods
Study design
The Nurses’ Health Study (NHS) started in 1976. Questionnaires have been distributed to the participants biennially inquiring about newly diagnosed diseases and risk factors. A semi-quantitative food frequency questionnaire (SFFQ), which has been validated in multiple studies [19], has been used to collect dietary information in 1980, 1984, 1986, and every 4 years thereafter. The Health Professionals Follow-up Study (HPFS) began in 1986. Questionnaires on lifestyle risk factors and medical history have been sent to participants every 2 years [20], and dietary assessments using the SFFQ have been collected from 1986 and every 4 years thereafter. This study was approved by the Human Subjects Committees of the Harvard T.H. Chan School of Public Health and Brigham and Women’s Hospital.
Assessment of dietary intake
Dietary information was assessed by the SFFQs (available at www.nurseshealthstudy.org and sites.sph.harvard.edu/hpfs/hpfs-questionnaires). The total intake amount of nutrients and energy intake were calculated based on the product of consumption frequency of each item and its nutrient and energy composition, summed across all items. For the NHS, an expanded SFFQ with 131 items was first distributed in 1984, and repeated in 1986 and then every four years. Average intakes of percentage of energy from fat, other nutrients/foods, and total energy were calculated based on the seven repeated SFFQs from 1984 until 2006 to best represent long-term diet and minimize within-subject variation [21]. Updating of intake was stopped in 2006 to provide a lag before the assessment of cognitive decline and thus minimize the effect of cognitive function on diet. Similarly, for the HPFS, the average intake from five repeated dietary assessments (starting from 1986 and then every four years until 2002) was used. In both cohorts, intakes assessed by SFFQs correlated well with those assessed by multiple dietary records for total and specific types of fat: the correlations for energy-adjusted intakes were 0.67 for total fat, 0.70 for saturated fatty acids (SFAs), 0.69 for monounsaturated fatty acids (MUFA), and 0.64 for polyunsaturated fatty acids (PUFA) [22, 23]. Correlations further increased when the means of multiple SFFQs were used (e.g., correlations were 0.83 for total fat and 0.95 for SFAs) [22, 23].
Assessment of subjective cognitive decline (SCD)
In both cohorts, SCD was assessed twice by either mail or online questionnaires (2012 and 2014 for NHS; 2008 and 2012 for HPFS). In our previous publications, the term subjective cognitive function (SCF) was used [24, 25], but we have updated the terminology to SCD in line with changes in the field [26]. For the HPFS, there were 6 yes/no questions assessing recent changes in general memory, executive function, attention, and visuospatial skills: (1) “Do you have more trouble than usual remembering recent events?”; (2) “Do you have more trouble than usual remembering a short list of items, such as a shopping list?”; (3) “Do you have trouble remembering things from one second to the next?”; (4) “Do you have any difficulty in understanding things or following spoken instructions?”; (5) “Do you have more trouble than usual following a group conversation or a plot in a TV program due to your memory?”; and (6) “Do you have trouble finding your way around familiar streets?” There was one additional question for the NHS: “Have you recently experienced any change in your ability to remember things?” [27] For scoring, one point was given to each positive response for these questions. Two SCD scores were then averaged to minimize random errors [25, 28, 29], except for participants with only one documented response from the two SCD questionnaires.
Strong associations have been shown between SCD with both concurrent objective cognitive function [27, 30] and subsequent cognitive decline [27], notably for individuals with higher education [31], SCD was also strongly associated with homozygous APOE ℇ4 genotype in both the NHS and HPFS [25]. Also, numerous risk factors for dementia, such as high blood pressure, depression, CVD, type 2 diabetes, heavy smoking, and high blood cholesterol, were all associated with SCD [25], which further supports validity.
Covariates
Information on covariates was prospectively collected in the NHS and HPFS at baseline and on follow-up questionnaires. These included: age, body mass index (BMI), height, physical activity, race, the use of multivitamins, smoking status, amount of alcohol consumption, cancer, diabetes, high blood pressure, elevated cholesterol, history of CVD, family history of dementia, and depression. For the NHS, additional information on menopausal status, use of hormone replacement therapy, parity, education, husband’s education, census tract income was obtained. For the HPFS, information on profession was also collected.
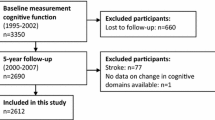
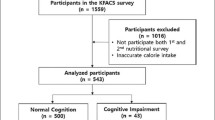
Population for analysis
For both NHS and HPFS, we excluded participants with > 70 food items blank and those with extreme energy intakes (< 600 or > 3,500 kcal/day for women and < 800 or > 4200 kcal/day for men). Individuals who developed Parkinson’s disease (PD) prior to SCD assessments were also excluded because PD patients may present with cognitive impairment. The final analysis included 49,493 women with a mean age of 48 years at baseline in 1984 and 27,842 men with a mean age of 51 years at enrollment in 1986 (Supplementary Fig. 1).
Statistical analysis
Average daily total energy intake was calculated from repeated SFFQs. The percentage of energy from fat was calculated by dividing the energy intake from fat by total energy intake for each SFFQ, and then we calculated the average percentage of energy from fat from repeated SFFQs. Intakes of total energy, total fat, and specific fatty acids were divided into quintiles. Poisson regression models were used due to the distribution and nature of the SCD scores. ORs and 95% CIs of 3-unit increments in SCD were calculated because three or more positive SCD questions was the definition of poor cognitive function [27]. The associations between total energy, total fat, and specific fatty acid intakes with SCD were estimated by comparing each quintile of intake with the lowest quintile. Due to a non-linear relationship between age and SCD, both a linear and a quadratic term for age were included in all models. Because hypertension, diabetes, elevated cholesterol, and CVD were potential mediators on a causal pathway, we did not adjust for these variables in our primary analysis, although similar results were observed with or without these variables in the models. For analyses of total energy intake, we also adjusted for intakes of fruit juice, fruits, and vegetable in the final model because these are the dietary variables most strongly associated with the risk of SCD in our cohorts. To further investigate what sources of energy were associated with SCD, we conducted additional analysis where we include separate terms for energy from fat, carbohydrates, and protein, and all other covariates, without controlling for total energy intake. For primary fatty acid analyses, all models were mutually adjusted for remaining fatty acid intakes; and protein intake, which had an inverse association with SCD in our cohorts [32], was also adjusted in the models. In the fully adjusted model, intakes of carotenoids, anthocyanins, vitamin C, D, and E were also included. In addition to being categorized as quintiles, total fat and specific fatty acids were also treated as continuous variables. We used isocaloric substitution models, which simultaneously included total energy intake, percentage of energy intake from protein, and percentage of energy intake from fatty acids; the coefficients in these models can be interpreted as the associations when substituting the percentage of energy from fat for the same percentage of energy from total carbohydrates. In the sensitivity analyses we adjusted for baseline BMI [33], individual carotenoids (β-carotene, α-carotene, lycopene, lutein/zeaxanthin, and β-cryptoxanthin) instead of total carotenoids, and for flavonoid subclasses (including flavones and flavanones), which had significant inverse associations with SCD in our cohorts [34]. Because body size is one of the major determinants of between-person variation in total energy intake, we further adjusted for height when evaluating the association between total energy intake and SCD. We also performed a sensitivity analysis among only the participants with both SCD assessments.
In addition to the aforementioned traditional isocaloric substitution with carbohydrates, we modeled each specific fatty acid as percentage of total fat (fat quality index), also adjusting for total fat and total energy intakes in the same model. The coefficients from these models can be interpreted as the effect when substituting the specific fatty acid for all other fatty acids.
For all analyses, testing for linear trends was conducted by assigning median values within each quintile and modeling these values as continuous variables.
To investigate whether the associations between total energy and fat intake were modified by variables of interests, additional analyses were conducted by stratifying participants by baseline age (< 50 years, ≥ 50 years), smoking status (never smokers, past smokers, and current smokers), BMI (underweight, normal weight, overweight, and obese), disease status (self-reported CVD, type 2 diabetes, and depression), and APOE ℇ4 allele carrier status (yes/no).
To evaluate the temporal relationship between total energy and fat intakes with SCD, the associations between dietary intake at each of the individual years with SCD were estimated. We also mutually included both recent (average intake from 2002 to 2006 in NHS and average intake from 1998 to 2002 for HPFS) and remote (average intake from 1984 to 1990 in NHS and average intake from 1986 to 1990 for HPFS) intakes in the same model to examine whether these associations were independent of each other. In these analyses, we used covariate information closest in time to the dietary assessments [25, 34, 35].
Analyses were first performed separately for each cohort, and an inverse-variance-weighted, fixed-effect meta-analysis was used to combine the results across the NHS and HPFS studies. Because our analyses included multiple comparisons, we considered the interpretation of our findings using the conservative Bonferroni correction. All analyses were performed using SAS software, version 9.2 (SAS Institute Inc., Cary, NC).
Results
Population characteristics
Participants with higher total energy intake were younger, had higher alcohol and percentage of energy from total fat intakes, lower percentage of energy from protein, carotenoid, and anthocyanin intakes, higher level of physical activity, and higher prevalence of depression in both the NHS and HPFS (Table 1). Characteristics by quintiles of total fat intake (as percentage of energy) are shown in Supplementary Table 1.
Total energy
In both the NHS and HPFS, higher total energy intake was significantly associated with higher odds of SCD after adjusting for age and major non-dietary factors (Table 2). The positive associations further strengthened after additionally adjusting for fruit, vegetable, and fruit juice intakes. In the fully adjusted model, when comparing the highest with the lowest quintiles of total energy intake, the pooled OR of a 3 unit-increment in SCD was 2.77 (95% CI 2.53, 2.94), P trend < 0.0001; each 500 kcal/day greater intake was associated with a 48% higher odds of SCD. In the sensitivity analysis when height was additionally adjusted, the positive associations were strengthened. Subgroup analysis by BMI did not show significant differences in the associations (Supplementary Table 2). In the additional analysis investigating what sources of energy were associated with SCD, positive associations were observed for total fat and carbohydrate intakes, whereas an inverse association was observed for protein intake (Supplementary Table 3).
Fatty acid analysis
Comparing the highest with the lowest quintiles of total fat intake, the pooled OR was 1.39 (1.29, 1.50) (Table 3). When substituting each 5% of energy intake from total fat for the same amount of energy from total carbohydrates, the pooled OR was 1.14 (1.11, 1.17).
For both trans-fat and SFA, although positive associations with SCD were observed in the age-adjusted and age-and-calorie-adjusted models, associations became null in the fully-adjusted models. For MUFA intake, positive associations with SCD were only found in the NHS; for PUFA intake, positive associations were observed in both the NHS and HPFS. Results were similar across strata of baseline age, smoking status, disease status, and APOE ℇ4 allele carrier status. Similar results were observed in the sensitivity analysis when we only included participants with both SCD assessments, and when we adjusted for baseline BMI, individual carotenoids instead of total carotenoids, or for flavonoid subclasses.
Secondary analysis for specific fatty acids
When modeling specific fatty acids as the percentage of total fat and also adjusting for total fat in the same model, results for trans-fat, SFA, MUFA, and PUFA had similar trends as the aforementioned substitution for total carbohydrates.
For ω-3 PUFA intake (including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA)), although inverse associations with SCD were observed when adjusting for age and total energy intake, the associations generally became null after further adjusting for dietary factors (Supplementary Table 4).
Temporal relationships
In both the NHS and HPFS, higher total energy intake was significantly associated with higher odds of SCD at all time points during follow-up (Fig. 1); both recent and remote intakes had positive associations with SCD when being mutually adjusted in the model; the average of all dietary assessments had the strongest associations. Similar findings were observed for total fat (Fig. 2). For trans-fat and SFA intakes, associations with SCD were mostly null in both cohorts. For MUFA and PUFA intakes, temporal relationships were relatively inconsistent over time and across cohorts: associations were null at most of the time points in the HPFS, whereas null associations were found in more recent years in the NHS (Supplementary Fig. 2).
Total energy intake at each year of dietary assessment and ORa of 3-unit increments in SCD. aComparing the highest versus the lowest quintiles of intake. Multivariate model: NHS: adjusted for age, census tract income, education (registered nursing degrees, bachelors degree, masters or doctorate degree), husband’s education (high school or lower education, college, graduate school), race (white, black, other), smoking history (never, ≤ 4 pack-years, 5–24 pack-years, 24 + pack-years), depression, physical activity level (METs-hr/week, quintiles), BMI, family history of dementia, multivitamin use (yes/no), intakes of alcohol (g/d), postmenopausal status and hormone replacement therapy use, missing indicator for SCD measurement at 2012 or 2014, number of dietary assessments during 1984–2006, parity (nulliparous, 1–2, > 2), fruit intake (quintiles), vegetable intake (quintiles), and fruit juice intake (quintiles). HPFS: adjusted for age, smoking history (never, ≤ 24 pack-years, 25–44 pack-years, 45 + pack-years), cancer (yes/no), depression, physical activity level (METs-h/week, quintiles), BMI, multivitamin use (yes/no), intake of alcohol (g/day), family history of dementia, profession (dentist, pharmacist, optometrist, osteopath, podiatrist, veterinarian), missing indicator for SCD measurement at 2008 or 2012, and number of dietary assessments during 1986–2002, fruit intake (quintiles), vegetable intake (quintiles), and fruit juice intake (quintiles)
Intake of total fat at each year of dietary assessment and ORa of 3-unit increment in SCD. aSubstituting every 5% of energy intake from total fat for the same amount of energy from total carbohydrates. Multivariate model: NHS: adjusted for percentage of energy intake from dietary total protein (quintiles), age, total energy intake, census tract income, education (registered nursing degrees, bachelors degree, masters or doctorate degree), husband’s education (high school or lower education, college, graduate school), race (white, black, other), smoking history (never, ≤ 4 pack-years, 5–24 pack-years, 24 + pack-years), depression, physical activity level (METs-h/week, quintiles), BMI, family history of dementia, multivitamin use (yes/no), intakes of alcohol (g/d), postmenopausal status and hormone replacement therapy use, missing indicator for SCD measurement at 2012 or 2014, number of dietary assessments during 1984–2006, parity (nulliparous, 1–2, > 2), intakes of vitamin c, d, e (quintiles), carotenoids (quintiles), and anthocyanins (quintiles). HPFS: adjusted for percentage of energy intake from dietary total protein (quintiles), age, total energy intake, smoking history (never, ≤ 24 pack-years, 25–44 pack-years, 45 + pack-years), cancer (yes/no), depression, physical activity level (METs-hr/week, quintiles), BMI, multivitamin use from 1986 to 2002 (yes/no), intake of alcohol (g/d), family history of dementia, profession (dentist, pharmacist, optometrist, osteopath, podiatrist, veterinarian), missing indicator for SCD measurement at 2008 or 2012, and number of dietary assessments during 1986–2002, intakes of vitamin c, d, e (quintiles), carotenoids (quintiles), and anthocyanins (quintiles)
Discussion
Higher total energy intake was significantly associated with greater odds of SCD in two large prospective cohort studies of US men and women. Each 500 kcal increase in daily total energy intake was associated with 48% higher odds of SCD, and the positive associations persisted across more than 20 years of follow-up. Intakes of both total fat and total carbohydrate appeared to contribute to the positive association of total energy intake with SCD although for the same percent of energy, the association was stronger for total fat.
Lower total energy intake was related to increased life span and more favorable aging-related outcomes in numerous experimental animal studies [10,11,12, 36, 37]. Lower calorie intake reversed the accumulation of pro-inflammatory cells across various tissues, dampening aging-associated cell–cell interaction [37]. Although similar experiments have been hard to conduct in humans, a study on the Okinawan diet suggested a link between lower calorie intake and longer lifespan as well as better later-life outcomes [38]. To date, human studies on total energy intake and cognitive function remain limited. In a study with 980 participants followed up for 4 years, higher calorie intake was associated with a higher risk of Alzheimer’s disease among APOE ε4 carriers [39]. In a case–control study, high caloric intake was associated with an increased risk of having mild cognitive impairment (MCI) compared with the reference group, whereas moderate caloric intake was not associated with MCI [40]. One randomized controlled trial with 50 participants concluded that caloric restriction over a period of 3 months had beneficial effects on memory performance in healthy elderly subjects [41]. The results of the current study support and strengthen the hypothesis that lower total energy intake could be related to better cognitive function. Major determinants of between-person variation in total energy intake include physical activity, body size, and metabolic efficiency [28]. Many studies have indicated improvement of energy efficiency in those who practice calorie restriction. In an 11-year follow-up study of rhesus monkeys, caloric restriction led to a reduction of total energy expenditure and resting energy expenditure, but no change in nonbasal energy expenditure [42]. In the CALERIE study, non-obese humans who were calorie-restricted did not have a reduction in daily activity, indicating the reduction in the activity energy expenditure was most likely attributed to increased metabolic efficiency [43]. Metabolic slowing likely benefits those under caloric restriction by reducing oxidative stress [44], which has been one of the major mechanisms proposed for the association between lower calorie intake and better age-related outcomes [45]. Lower calorie intake increased neurotrophic factor expression and decreased neuronal death in the brain of rats [46], and may improve brain plasticity in older humans [41]. Calorie restriction also changed body composition, including weight loss (especially fat mass) and waist circumference reduction; such changes can be seen within the first two years of dietary intervention [47]. These changes in body composition and reduction in central obesity also partly contribute to a reduced risk of dementia with energy restriction [48]. In aging monkeys, continuous calorie restriction for more than 10 years did not result in continued weight loss, suggesting adaption to a new steady-state [49]. In the current analysis, we adjusted for BMI, physical activity, body size (height), and intakes of fruit juice, fruits, and vegetable, therefore, the association between total energy intake and SCD was independent of these factors. The findings for total energy are consistent with the positive association for waist circumference with SCD in our cohorts, which suggests the importance of maintaining a healthy energy balance throughout life.
As for total fat intake, the findings from an animal study have suggested that a high-fat diet may lead to detrimental neuroinflammation in the brain [50]. However, the findings of epidemiologic studies have been mixed. In the Rotterdam study, higher total fat intake was associated with a greater risk of dementia with a 2.1 year of follow-up [51], but the association became null after extending the follow-up period to 6 years [16]. Higher fat intake was related to a higher risk of AD only among APOE ε4 carriers [39], and higher fat intake was related to reduced risk of MCI or dementia in a cohort study from the Mayo Clinic [52]. In the current study, compared with total carbohydrate, higher total fat intake was positively associated with SCD throughout the follow-up period in both cohorts. The differences in the study population characteristics, geographical locations, dietary patterns, and the length of follow-up period might contribute to the different study findings. Also, different data analytic methods were used in different studies: many did not use substitution models or specify the reference of comparison, and some studies did not adjust for potential confounders such as physical activity, BMI, smoking, alcohol consumption, depression, socioeconomic status, or intakes of fruits and vegetables. The positive association of total fat intake with worse SCD when compared isocalorically with carbohydrate intake would suggest that replacing dietary fat with carbohydrate might reduce cognitive decline. However, this finding should be interpreted cautiously as the results of studies on the association between dietary fat and cognitive decline are inconsistent. Also, a previous study showed that total fat intake was inversely associated with total mortality, and intakes of PUFA and MUFA were inversely associated with total mortality and deaths due to neurodegenerative conditions [53]. In the current study, although fat quality improved over the period of follow-up, including a shift from animal and partially hydrogenated fats to relatively unsaturated plant oils [53], the potential long-term impact of less healthy fats consumed many years ago on health, such as atherosclerosis and systemic inflammation, may still have important influences on subsequent cognitive function.
Regarding specific fatty acid intakes, higher trans-fat and SFA intakes were associated with worse cognitive trajectory among participants with type 2 diabetes [14], and in the Women’s Health Study, higher SFA and lower MUFA intakes were associated with worse cognitive function [15]. However, in the Rotterdam study, higher intakes of trans-fat and SFA were related to lower risk of AD, whereas no associations were found for MUFA and PUFA intakes; no association was observed for trans-fat, SFA, MUFA, and PUFA when the outcome was total dementia [16]. In contrast, one prospective cohort study found MUFA was associated with higher odds of mild cognitive impairment [17] and another study found MUFA intake may be related to poorer memory in women [18]. The inconsistencies across studies may arise from different definitions of cognitive impairment, various lengths of study follow-up and different time points of dietary assessment, as intakes of specific dietary fatty acids changed over time. Also, many studies did not mutually adjust for intakes of specific fatty acids, and most had only one single dietary assessment, which may not adequately represent long-term diet.
One major difference between the current study and previous studies was that we additionally adjusted for carotenoids and flavonoids, two dietary variables with strong inverse associations with SCD in our cohorts [34] and also significantly related to fat intakes. After adjusting for these two dietary variables, the inverse associations between intakes of ω-3 PUFA and risk of SCD, and the positive associations between trans-fat and SFA with SCD became null. Although null results for these specific fatty acids have been reported in other epidemiological studies [14,15,16, 51] and intervention trials for ω-3 PUFA [54], future studies are warranted to further examine these relationships. Notably, the sources of MUFA changed from margarine, steak, roast, other red meat, and hamburger in the remote years to olive oil, nuts, and peanut butter in the recent years; the sources of PUFA changed from mayonnaise, margarine, and pure butter in the remote years to walnuts, other nuts, and peanut butter in the recent years [53]. The cooking methods and other nutrients related to the aforementioned food sources may have contributed to the positive associations observed for MUFA and PUFA in the remote years. Overall, interpreting findings for fatty acids in the current study is difficult because of inconsistencies of the associations observed over time and between cohorts.
Two major strengths of the current study are more than 20 years of long-term follow-up and large sample sizes in both cohorts, allowing for the capture of potentially critical exposure windows, reducing reverse causation, and providing great statistical power for analysis. Averaged dietary information from multiple dietary assessments over time best represents long-term diet, and reduces errors in assessing diet. Dietary data were updated only to 6 years before SCD assessments to minimize the impact of reverse causation, i.e., the effect of altered cognitive function on diet. To minimize confounding, we adjusted for a comprehensive list of variables collected from our biannual questionnaires. However, there are some limitations in the present study. First, baseline assessment of the cognitive function of our study participants was not available. However, a general high baseline cognitive function can be assumed in these participants during their early adulthood to be able to enter professional schools and pass board exams. Also, these highly educated participants generally have better health awareness and better insights to report subtle cognitive changes [55]. Second, no objective cognitive assessment was included in either cohort, and differential reporting of SCD related to dietary exposures could have occurred. However, the validity of SCD has been repeatedly evaluated and was strongly related to both concurrent objective cognitive function [27, 30] and subsequent cognitive decline [27]. The clear association between APOE ε4 genotype and SCD provides additional strong evidence of validity [25]. Moreover, SCD can be used to detect more subtle cognitive changes [56], especially in higher educated participants [31]. Third, our dietary data was based on self-reporting, which may be subject to errors. However, the SFFQ has been repeatedly validated and has been widely used in epidemiological studies [19] and we averaged the multiple dietary assessments over the long-term follow-up period to reduce possible errors. Fourth, although we adjusted for total energy intake in all analyses of specific nutrients, residual confounding could still have existed because of a strong positive association between total energy and SCD. Finally, our study results could have limited generalizability, because the study populations were mainly Caucasian, relatively highly educated healthcare professionals with better health awareness. However, the relatively high and uniform cognitive function in our study participants during early adulthood should have reduced residual confounding.
In conclusion, the results from the current study support the hypothesis that lower total energy intake could be beneficial for subsequent cognitive function. Intakes of both total fat and total carbohydrate appeared to contribute to the positive association between total energy intake and SCD although for the same amount of energy, the association was stronger for total fat. Future studies are needed to further examine these relationships.
Data availability
Data will be shared at the request of other qualified investigators for purposes of replicating procedures and results. Our NHS and HPFS websites (www.nurseshealthstudy.org and sites.sph.harvard.edu/hpfs/) include guidelines for external users and links to all questionnaires.
Code availability
Analytic code will be made available upon request.
Abbreviations
- SCD:
-
Subjective cognitive decline
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- NHS:
-
Nurses’ Health Study
- HPFS:
-
Health Professionals Follow-up Study
- SFFQ:
-
Food frequency questionnaires
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- FA:
-
Fatty acids
- SFA:
-
Saturated fatty acid
- MUFA:
-
Monounsaturated fatty acids
- PUFA:
-
Polyunsaturated fatty acids
- ALA:
-
Alpha-linolenic acid
- EPA:
-
Eicosapentaenoic acid
- DHA:
-
Docosahexaenoic acid
References
Ahmadi-Abhari S, Guzman-Castillo M, Bandosz P, et al. Temporal trend in dementia incidence since 2002 and projections for prevalence in England and Wales to 2040: modelling study. BMJ. 2017. https://doi.org/10.1136/bmj.j2856.
Yeh TS, Wang JD, Ku LE. Estimating life expectancy and lifetime healthcare costs for Alzheimer’s disease in Taiwan: does the age of disease onset matter? JAD. 2020;73(1):307–15. https://doi.org/10.3233/jad-181060.
Wessels AM, Tariot PN, Zimmer JA, et al. Efficacy and safety of lanabecestat for treatment of early and mild Alzheimer disease: the AMARANTH and DAYBREAK-ALZ randomized clinical trials. JAMA Neurol. 2019. https://doi.org/10.1001/jamaneurol.2019.3988.
Rabin LA, Smart CM, Amariglio RE. Subjective cognitive decline in preclinical Alzheimer’s disease. Annu Rev Clin Psychol. 2017;13:369–96. https://doi.org/10.1146/annurev-clinpsy-032816-045136.
Galluzzi S, Frisoni GB. Imaging, subjective complaints, and MCI: 30 years before. J Nutr Health Aging. 2008;12(1):80s-s83. https://doi.org/10.1007/bf02982592.
Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s Dementia. 2011;7(3):280–92. https://doi.org/10.1016/j.jalz.2011.03.003.
Tucker KL. Nutrient intake, nutritional status, and cognitive function with aging. Ann N Y Acad Sci. 2016;1367(1):38–49. https://doi.org/10.1111/nyas.13062.
Mattison JA, Roth GS, Beasley TM, et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489:318. https://doi.org/10.1038/nature11432.
Colman RJ, Beasley TM, Kemnitz JW, Johnson SC, Weindruch R, Anderson RM. Caloric restriction reduces age-related and all-cause mortality in rhesus monkeys. Nat Commun. 2014;5:3557. https://doi.org/10.1038/ncomms4557.
Parikh I, Guo J, Chuang KH, et al. Caloric restriction preserves memory and reduces anxiety of aging mice with early enhancement of neurovascular functions. Aging. 2016;8(11):2814–26. https://doi.org/10.18632/aging.101094.
Wahl D, Cogger VC, Solon-Biet SM, et al. Nutritional strategies to optimise cognitive function in the aging brain. Ageing Res Rev. 2016;31:80–92. https://doi.org/10.1016/j.arr.2016.06.006.
Dal-Pan A, Pifferi F, Marchal J, Picq JL, Aujard F. Cognitive performances are selectively enhanced during chronic caloric restriction or resveratrol supplementation in a primate. PLoS ONE. 2011;6(1):e16581. https://doi.org/10.1371/journal.pone.0016581.
Harold D, Abraham R, Hollingworth P, et al. Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat Genet. 2009;41(10):1088–93. https://doi.org/10.1038/ng.440.
Devore EE, Stampfer MJ, Breteler MM, et al. Dietary fat intake and cognitive decline in women with type 2 diabetes. Diabetes Care. 2009;32(4):635–40. https://doi.org/10.2337/dc08-1741.
Okereke OI, Rosner BA, Kim DH, et al. Dietary fat types and 4-year cognitive change in community-dwelling older women. Ann Neurol. 2012;72(1):124–34. https://doi.org/10.1002/ana.23593.
Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Diet and risk of dementia: does fat matter? The Rotterdam Study. Neurology. 2002;59(12):1915–21.
Cherbuin N, Anstey KJ. The Mediterranean diet is not related to cognitive change in a large prospective investigation: the PATH Through Life study. Am J Geriatr Psychiatry. 2012;20(7):635–9. https://doi.org/10.1097/JGP.0b013e31823032a9.
Gibson EL, Barr S, Jeanes YM. Habitual fat intake predicts memory function in younger women. Front Hum Neurosci. 2013;7:838. https://doi.org/10.3389/fnhum.2013.00838.
Klipstein-Grobusch K, den Breeijen JH, Goldbohm RA, et al. Dietary assessment in the elderly: validation of a semiquantitative food frequency questionnaire. Eur J Clin Nutr. 1998;52(8):588–96. https://doi.org/10.1038/sj.ejcn.1600611.
Rimm EB, Giovannucci EL, Willett WC, et al. Prospective study of alcohol consumption and risk of coronary disease in men. Lancet (London, England). 1991;338(8765):464–8.
Bernstein AM, Rosner BA, Willett WC. Cereal fiber and coronary heart disease: a comparison of modeling approaches for repeated dietary measurements, intermediate outcomes, and long follow-up. Eur J Epidemiol. 2011;26(11):877–86. https://doi.org/10.1007/s10654-011-9626-x.
Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135(10):1114–26 (discussion 27–36).
Willett W. Nutritional epidemiology. 3rd ed. Oxford: Oxford University Press; 2012.
Fondell E, Townsend MK, Unger LD, et al. Physical activity across adulthood and subjective cognitive function in older men. Eur J Epidemiol. 2018;33(1):79–87. https://doi.org/10.1007/s10654-017-0331-2.
Yuan C, Fondell E, Bhushan A, et al. Long-term intake of vegetables and fruits and subjective cognitive function in US men. Neurology. 2019;92(1):e63–75. https://doi.org/10.1212/wnl.0000000000006684.
Molinuevo JL, Rabin LA, Amariglio R, et al. Implementation of subjective cognitive decline criteria in research studies. Alzheimer’s Dementia. 2017;13(3):296–311. https://doi.org/10.1016/j.jalz.2016.09.012.
Samieri C, Proust-Lima C, M MG, et al. Subjective cognitive concerns, episodic memory, and the APOE epsilon4 allele. Alzheimer's Dementia 2014;10(6):752-9.e1. https://doi.org/10.1016/j.jalz.2014.06.012.
Willett W. Nutritional epidemiology. New York: Oxford University Press; 2017.
Fleiss JL. Chapter 13. The measurement of interrater agreement. In: Statistical methods for rates and proportions, 2nd edition, John Wiley, New York, p. 212–236 (1981).
Amariglio RE, Townsend MK, Grodstein F, Sperling RA, Rentz DM. Specific subjective memory complaints in older persons may indicate poor cognitive function. J Am Geriatr Soc. 2011;59(9):1612–7. https://doi.org/10.1111/j.1532-5415.2011.03543.x.
van Oijen M, de Jong FJ, Hofman A, Koudstaal PJ, Breteler MM. Subjective memory complaints, education, and risk of Alzheimer’s disease. Alzheimer’s Dementia. 2007;3(2):92–7. https://doi.org/10.1016/j.jalz.2007.01.011.
Yeh TS, Yuan C, Ascherio A, Rosner BA, Blacker D, Willett WC. Long-term dietary protein intake and subjective cognitive decline in US men and women. Am J Clin Nutr. 2021. https://doi.org/10.1093/ajcn/nqab236.
Rothman KJ. Epidemiology: an introduction. New York: Oxford University Press; 2012.
Yeh TS, Yuan C, Ascherio A, Rosner BA, Willett WC, Blacker D. Long-term dietary flavonoid intake and subjective cognitive decline in US men and women. Neurology. 2021;97(10):e1041–56. https://doi.org/10.1212/wnl.0000000000012454.
Bhushan A, Fondell E, Ascherio A, Yuan C, Grodstein F, Willett W. Adherence to Mediterranean diet and subjective cognitive function in men. Eur J Epidemiol. 2018;33(2):223–34. https://doi.org/10.1007/s10654-017-0330-3.
Colman RJ, Anderson RM, Johnson SC, et al. Caloric restriction delays disease onset and mortality in rhesus monkeys. Science. 2009;325(5937):201–4. https://doi.org/10.1126/science.1173635.
Mattison JA, Roth GS, Beasley TM, et al. Impact of caloric restriction on health and survival in rhesus monkeys from the NIA study. Nature. 2012;489(7415):318–21. https://doi.org/10.1038/nature11432.
Willcox BJ, Willcox DC, Todoriki H, et al. Caloric restriction, the traditional Okinawan diet, and healthy aging: the diet of the world’s longest-lived people and its potential impact on morbidity and life span. Ann N Y Acad Sci. 2007;1114:434–55. https://doi.org/10.1196/annals.1396.037.
Luchsinger JA, Tang MX, Shea S, Mayeux R. Caloric intake and the risk of Alzheimer disease. Arch Neurol. 2002;59(8):1258–63. https://doi.org/10.1001/archneur.59.8.1258.
Geda YE, Ragossnig M, Roberts LA, et al. Caloric intake, aging, and mild cognitive impairment: a population-based study. JAD. 2013;34(2):501–7. https://doi.org/10.3233/jad-121270.
Witte AV, Fobker M, Gellner R, Knecht S, Floel A. Caloric restriction improves memory in elderly humans. Proc Natl Acad Sci USA. 2009;106(4):1255–60. https://doi.org/10.1073/pnas.0808587106.
Blanc S, Schoeller D, Kemnitz J, et al. Energy expenditure of rhesus monkeys subjected to 11 years of dietary restriction. J Clin Endocrinol Metab. 2003;88(1):16–23. https://doi.org/10.1210/jc.2002-020405.
Martin CK, Das SK, Lindblad L, et al. Effect of calorie restriction on the free-living physical activity levels of nonobese humans: results of three randomized trials. Journal of applied physiology (Bethesda, Md. : 1985). 2011;110(4):956–63. https://doi.org/10.1152/japplphysiol.00846.2009.
Redman LM, Smith SR, Burton JH, Martin CK, Il'yasova D, Ravussin E. Metabolic slowing and reduced oxidative damage with sustained caloric restriction support the rate of living and oxidative damage theories of aging. Cell Metab. 2018;27(4):805-15 e4. https://doi.org/10.1016/j.cmet.2018.02.019.
Calabrese V, Cornelius C, Cuzzocrea S, Iavicoli I, Rizzarelli E, Calabrese EJ. Hormesis, cellular stress response and vitagenes as critical determinants in aging and longevity. Mol Aspects Med. 2011;32(4–6):279–304. https://doi.org/10.1016/j.mam.2011.10.007.
Lee J, Duan W, Long JM, Ingram DK, Mattson MP. Dietary restriction increases the number of newly generated neural cells, and induces BDNF expression, in the dentate gyrus of rats. J Mol Neurosci. 2000;15(2):99–108. https://doi.org/10.1385/jmn:15:2:99.
Das SK, Roberts SB, Bhapkar MV, et al. Body-composition changes in the Comprehensive Assessment of Long-term Effects of Reducing Intake of Energy (CALERIE)-2 study: a 2-y randomized controlled trial of calorie restriction in nonobese humans. Am J Clin Nutr. 2017;105(4):913–27. https://doi.org/10.3945/ajcn.116.137232.
Fitzpatrick AL, Kuller LH, Lopez OL, et al. Midlife and late-life obesity and the risk of dementia: cardiovascular health study. Arch Neurol. 2009;66(3):336–42. https://doi.org/10.1001/archneurol.2008.582.
DeLany JP, Hansen BC, Bodkin NL, Hannah J, Bray GA. Long-term calorie restriction reduces energy expenditure in aging monkeys. J Gerontol Ser A Biol Sci Med Sci. 1999;54(1):B5-11; (discussion B2–3). https://doi.org/10.1093/gerona/54.1.b5.
Yin Z, Raj DD, Schaafsma W, et al. Low-fat diet with caloric restriction reduces white matter microglia activation during aging. Front Mol Neurosci. 2018;11:65. https://doi.org/10.3389/fnmol.2018.00065.
Kalmijn S, Launer LJ, Ott A, Witteman JC, Hofman A, Breteler MM. Dietary fat intake and the risk of incident dementia in the Rotterdam Study. Ann Neurol. 1997;42(5):776–82. https://doi.org/10.1002/ana.410420514.
Roberts RO, Roberts LA, Geda YE, et al. Relative intake of macronutrients impacts risk of mild cognitive impairment or dementia. JAD. 2012;32(2):329–39. https://doi.org/10.3233/jad-2012-120862.
Wang DD, Li Y, Chiuve SE, et al. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 2016;176(8):1134–45. https://doi.org/10.1001/jamainternmed.2016.2417.
Burckhardt M, Herke M, Wustmann T, Watzke S, Langer G, Fink A. Omega-3 fatty acids for the treatment of dementia. Cochrane Database Syst Rev. 2016;4:CD009002. https://doi.org/10.1002/14651858.CD009002.pub3.
Li Y, Schoufour J, Wang DD, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ (Clinical Research ed.). 2020;368:l6669. https://doi.org/10.1136/bmj.l6669.
Jessen F, Wiese B, Bachmann C, et al. Prediction of dementia by subjective memory impairment: effects of severity and temporal association with cognitive impairment. Arch Gen Psychiatry. 2010;67(4):414–22. https://doi.org/10.1001/archgenpsychiatry.2010.30.
Funding
This work was supported by grants from the National Institutes of Health (UM1 CA186107, U01 167552).
Author information
Authors and Affiliations
Contributions
TSY designed and conducted the analysis, interpreted the data, and wrote the manuscript. CY contributed to data analysis and completed the technical review of the results. AA, BAR, DB contributed to the interpretation of the results, provided critical feedback, and revision of the manuscript for important intellectual content. WCW designed the analysis, interpretation of the results, revision of the manuscript for important intellectual content, and supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yeh, TS., Yuan, C., Ascherio, A. et al. Long-term intake of total energy and fat in relation to subjective cognitive decline. Eur J Epidemiol 37, 133–146 (2022). https://doi.org/10.1007/s10654-021-00814-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-021-00814-9