Abstract
Low fat dairy products are part of dietary guidelines to prevent stroke. However, epidemiological evidence is inconclusive with regard to the association between dairy products and stroke. We therefore investigated associations for substitutions between dairy product subgroups and risk of total stroke and stroke subtypes. We included 55,211 Danish men and women aged 50–64 years without previous stroke. Baseline diet was assessed by a food frequency questionnaire. Cases were identified through a national register and subsequently verified. The associations were analyzed using Cox proportional hazard regression. During a median follow-up of 13.4 years, we identified 2272 strokes, of which 1870 were ischemic (318 large artery atherosclerotic, 839 lacunar, 102 cardioembolic, 98 other determined types, 513 of unknown type), 389 were hemorrhages (273 intracerebral, 116 subarachnoid) and 13 of unknown etiology. Substitution of semi-skimmed fermented milk or cheese for whole-fat fermented milk was associated with a higher rate of ischemic stroke [semi-skimmed fermented milk: hazard ratio (HR) = 1.20 (95% confidence interval (CI) 0.99–1.45), cheese: HR = 1.14 (95% CI 0.98–1.31) per serving/day substituted] and substitutions of whole-fat fermented milk for low-fat milk, whole-fat milk or buttermilk were associated with a lower rate [low-fat milk: HR = 0.85 (95% CI 0.74–0.99), whole-fat milk: HR = 0.84 (95% CI 0.71–0.98) and buttermilk: HR = 0.83 (95% CI 0.70–0.99)]. We observed no associations for substitutions between dairy products and hemorrhagic stroke. Our results suggest that intake of whole-fat fermented milk as a substitution for semi-skimmed fermented milk, cheese, buttermilk or milk, regardless of fat content, is associated with a lower rate of ischemic stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Dietary Approaches to Stop Hypertension (DASH) [1] diet is recommended for stroke prevention [2] and has recently been associated with a lower risk of ischemic stroke [3]. Intake of low-fat dairy products is a principal component of the DASH-diet. However, since dairy products differ from each other with respect to the content of nutrients which, in addition to fat, may also be related to stroke risk, for instance calcium, potassium, magnesium and sodium [4,5,6,7], a more detailed distinction between dairy products is called for.
Previous cohort studies have failed to associate intake of total dairy products with stroke [8,9,10,11,12,13], while intake of low-fat dairy products [10] as well as intake of whole-fat dairy products [11] have been associated with a lower risk of stroke, although most studies found no association with either product type [8, 13, 14]. Studies investigating milk with different fat contents have found an association between low-fat milk and a lower [12] or no risk of stroke [9, 14] and an association between whole-fat milk and a higher [9] or no risk of stroke [12, 14] suggesting that the fat content may be of importance. Intake of fermented dairy products, to which probiotics have been added during production, has been associated with a lower risk of stroke [8, 12, 14]. Intake of cheese has been associated with a lower or no risk of stroke [8,9,10,11,12, 14].
To date, the most widely applied analytical approach when investigating the association between dairy products and stroke has been to compare individuals with a different intake of e.g. milk but with a similar total energy intake. This implies that these individuals differ in intake of other non-specified energy-providing foods. Thus, results from such studies represent a joint effect of the investigated food and the substituted foods. Consequently, the inconsistent findings from studies on dairy products and stroke could stem from a lack of specification of the substituted foods, as people within and between populations may substitute dairy products differently. By specifying the substitution, the studies would offer a more detailed and clear interpretation of the results. Further, stroke is a collective term for several vascular diseases of the brain which have different etiology and do not necessarily share risk factors [15,16,17], which necessitates a distinction between stroke subtypes. We therefore assessed the associations for specified substitutions between different subgroups of dairy products and the risk of any type of stroke as well as the risk of specific stroke subtypes.
Methods
Study population
The participants in this study were part of the Danish cohort Diet, Cancer and Health, as described elsewhere [18]. Briefly, they were recruited from December 1993 through May 1997 where 160,725 men and women aged 50–64 years, with no previous cancer diagnosis registered in the Danish Cancer Registry and residing in the greater Copenhagen or Aarhus areas were invited, of whom 57,053 (27,190 men and 29,863 women) gave informed consent to participate [18]. We excluded 569 participants with an existing cancer diagnosis at baseline (due to a delayed entry in the Danish Cancer Registry) and those with stroke before baseline (n = 582) or with incomplete information on any variable to be included in the statistical analyses (n = 723), leaving 55,211 participants for analysis (Supplementary Figure 1). The baseline assessment included self-administered questionnaires on diet and lifestyle as well as anthropometrical measurements taken by trained personnel [18]. The questionnaires were scanned and checked for completeness by the study personnel.
Diet assessment
The participants completed a 192-item semi-quantitative food frequency questionnaire (FFQ), specifically developed for the Diet, Cancer and Health cohort [19] and designed to reflect the average food intake during the previous year. The FFQ included pre-specified frequencies ranging from never to 8 times or more per day, and the recorded information was converted to daily intakes of foods and nutrients using FoodCalc version 1.3. The FFQ was validated against two 7-day food records [20]. The agreement between the two instruments for classification of subjects into quintiles of intakes of saturated fat and calcium, for which dairy products are major sources, was 64% for saturated fat and 81% for calcium among men and 71% for saturated fat and 61% for calcium among women (same quintile ± 1) [20]. Dairy products include all products made from cow’s milk, i.e. milk, milk derivatives, cheese, butter, cream and ice cream. The questions specifically addressing dairy product intake included milk (skimmed milk, 0.3% fat, semi-skimmed milk, 1.5% fat, whole-fat milk, 3.5% fat), buttermilk, 0.5% fat, fermented milk products (yoghurt-type products with 1.5 or 3.5% fat, with and without added fruit), cheese (semi-hard cheese, soft matured cheese, blue cheese, cottage cheese and cream cheese) and butter. In addition to these items, dairy product intake was also derived from standard recipes for dishes addressed in the questionnaire and other food items containing dairy products. However, in this study, only dairy products which were specifically addressed in the FFQ were investigated.
Dairy product intake was operationalized as follows: (1) low-fat milk (sum of skimmed and semi-skimmed milk), (2) whole-fat milk, (3) buttermilk, (4) semi-skimmed fermented milk products, (5) whole-fat fermented milk products, (6) cheese and (7) butter. All dairy product variables were expressed as servings per day. For milk and fermented milk products, the serving size was 200 g/day, for cheese and butter it was 20 and 6 g/day, respectively.
Stroke ascertainment
The participants were followed-up for stroke incidence (fatal and non-fatal) by linkage of each participant’s civil registration number to the Danish National Patient Registry, which covers discharge records from Danish hospitals since 1977 [21]. Possible stroke cases were identified through the register as first-ever hospital discharge diagnosis according to the International Classification of Diseases (ICD-8 codes: 430, 431, 433, 434, 436.01, or 436.90; ICD-10 codes: I60 I61 I63 or I64). The identified cases were verified by review of each individual medical record and/or hospital discharge letter.
The identified strokes were classified as ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage or unspecified type of stroke. Ischemic strokes were further classified according to the TOAST-criteria [22] as large artery atherosclerosis, lacunar stroke (small-vessel occlusion), cardioembolism, stroke of other etiology or stroke of unknown etiology. Participants were followed from the time of inclusion into the study until the date of a stroke diagnosis, death, emigration or 30 November 2009, whichever came first.
Assessment of covariates
Information about length of elementary and secondary education, smoking habits, physical activity, hypertension, hypercholesterolemia and diabetes was collected using a self-administered questionnaire. The total length of elementary and secondary education was expressed as short (≤7 years), medium (8–10 years) or long (≥10 years). Smoking status was categorized as never, former, current <15 g tobacco/day, current 15–25 g tobacco/day, current >25 g tobacco/day. Physical activity included both participation in planned activity as well as active transportation and was expressed as being active <30 or ≥30 min/day. Hypertension was defined as a history of hypertension or use of antihypertensive medication. Hypercholesterolemia was defined as a history of hypercholesterolemia or use of lipid-lowering medication. Diabetes was defined as a history of diabetes or use of insulin. These conditions were reported as yes, no or unknown. Weight, height and waist circumference were measured by trained technicians at the study centers. Body mass index (BMI) was calculated as the weight divided by the height squared (kg/m2). Information about prevalent myocardial infarction was obtained from the Danish National Patient Registry.
Statistical analysis
We evaluated the associations for substitutions between subgroups of dairy products with the rate of total stroke, ischemic stroke, sub-types of ischemic stroke (large artery atherosclerosis, lacunar stroke and cardioembolic stroke) and sub-types of hemorrhagic stroke (intracerebral hemorrhage and subarachnoid hemorrhage) using sex- and date of inclusion-stratified Cox proportional hazards regression models with age as time scale.
The basic model (Model 1a) included intake of all subgroups of dairy products (servings/day), except for the dairy product subgroup to be replaced, and a variable representing the total number of servings of dairy products per day. Thus, hazard ratios for each of the dairy product subgroups in the model can be interpreted as the estimated difference in rate of stroke associated with a one serving higher intake of the subgroups included in the model and a concomitant lower intake of the subgroup left out of the model. Model 1a was adjusted for total energy intake (excluding energy from alcohol, continuous, kJ/day) and age at inclusion (continuous), the latter used as a proxy for the “age” of the exposure and covariate information. Additional adjustments included BMI, residuals of waist circumference regressed on BMI (continuous), education (categorical), smoking status (categorical) physical activity (binary), alcohol intake (spline with 4 knots) (Model 1b) and intakes of fruit, vegetables, red meat, processed red meat and fish (all continuous, servings/day) (Model 2). In order to assess the influence of the potential mediating variables hypertension, hypercholesterolemia, diabetes and myocardial infarction at baseline, we adjusted for these separately (Model 3). We also tested for effect modification by sex by means of likelihood ratio tests between models with and without interaction terms of sex and exposure variables. We found no indication of effect modification by sex, thus the results are presented for the whole sample.
The individual dairy product subgroups were only weakly correlated (Supplementary Table 1), thus justifying the simultaneous inclusion of them in the substitution analyses. The assumption of independent delayed entry was met once the analyses were stratified by date of inclusion in tertiles. The proportional hazards assumption tested with Schoenfeld residuals was satisfied. We plotted martingale residuals against the exposure variables and included a lowess smooth in order to determine departures from linearity in the associations between substitutions of dairy products and stroke and found no departure from linearity.
To evaluate the robustness of the results, sensitivity analyses were performed. Since people diagnosed with diabetes, hypertension, hypercholesterolemia or myocardial infarction are likely to change their diets, analyses were repeated without participants reporting these conditions at baseline. All analyses were performed using STATA 13.1 (College Station, Texas, USA).
Results
During a median follow-up of 13.4 years, we identified 2272 incident stroke cases, of which 1870 were ischemic, 273 were intracerebral hemorrhages, 116 were subarachnoid hemorrhages and 13 were of unknown etiology. Of the 1870 ischemic stroke cases, 318 were large artery atherosclerotic, 839 were lacunar, 102 were cardioembolic, 98 were of other determined types of ischemic stroke, and 513 were of an unknown type of ischemic stroke (Supplementary Figure 2).
The characteristics of the cohort are presented in Table 1. Intake of cheese and butter contributed the most to the total number of servings per day of dairy products, and intake of whole-fat milk, buttermilk and semi-skimmed fermented milk contributed the least. Across quintiles of low-fat milk, those with the highest intake compared to those with the lowest were more likely to be men, be more physically active and have a history of diabetes or myocardial infarction. Across quintiles of whole-fat milk, those with the highest intake compared to the lowest were older, had a shorter education and were less likely to have a history of hypertension, hypercholesterolemia, diabetes or myocardial infarction. Those with the highest intake of whole-fat milk also had a higher intake of butter and processed meat. The participant characteristics across quintiles of buttermilk, semi-skimmed and whole-fat fermented milk, cheese and butter are presented in Supplementary Tables 2–6.
The results for total stroke are presented in Table 2 and Supplemental Table 7.
For total ischemic stroke, substitutions of whole-fat fermented milk for low-fat milk, whole-fat milk or buttermilk were associated with a lower rate [low-fat milk: HR = 0.85 (95% CI 0.74–0.99), whole-fat milk: HR = 0.84 (95% CI 0.71–0.98) and buttermilk: HR = 0.83 (95% CI 0.70–0.99) per 1 serving/day substituted] when adjusted for lifestyle and dietary risk factors (Table 3, Model 2). Furthermore, substitutions of semi-skimmed fermented milk or cheese for whole-fat fermented milk were associated with a higher rate [semi-skimmed fermented milk: HR = 1.20 (95% CI 0.99–1.45) and cheese: HR = 1.14 (95% CI 0.98–1.31) per 1 serving/day substituted] (Table 3, Model 2). When excluding participants with hypertension, hypercholesterolemia, diabetes or myocardial infarction, the pattern of associations was similar (Supplementary Table 8).
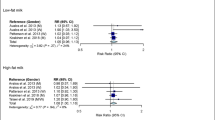
For large artery atherosclerotic stroke, we observed a lower rate of stroke for substitutions of whole-fat fermented milk for low-fat milk [HR = 0.63 (95% CI 0.43–0.94)], whole-fat milk [HR = 0.59 (95% CI 0.39–0.89)] and for buttermilk [HR = 0.59 (95% CI 0.38–0.92)] (Fig. 1). Additionally, we observed a higher rate of large artery atherosclerotic stroke for substitution of semi-skimmed fermented milk for whole-fat fermented milk [HR = 1.59 (95% CI 0.97–2.58)] and for substitution of cheese for whole-fat fermented milk [HR = 1.49 (95% CI 1.01–2.20)] (Fig. 1). For lacunar stroke, the pattern of associations was roughly similar to that for large artery atherosclerosis (Fig. 2). In contrast, for cardioembolic stroke, semi-skimmed fermented milk appeared to be beneficial when substituting low-fat milk, whole-fat milk, buttermilk or cheese (Fig. 3).
The association between a 1 serving/day difference in dairy product intake and risk of large artery atherosclerotic stroke in the Danish Diet, Cancer and Health cohort (318 cases). Adjusted for total energy intake, age at inclusion, education, waist circumference adjusted for body mass index, smoking, alcohol intake, physical activity and intakes of fruit, vegetables, red meat, processed meat and fish. The circles indicate hazard ratios and the whiskers indicate 95% CIs
The association between a 1 serving/day difference in dairy product intake and risk of lacunar stroke in the Danish Diet, Cancer and Health cohort (839 cases). Adjusted for total energy intake, age at inclusion, education, waist circumference adjusted for body mass index, smoking, alcohol intake, physical activity and intakes of fruit, vegetables, red meat, processed meat and fish. The circles indicate hazard ratios and the whiskers indicate 95% CIs
The association between a 1 serving/day difference in dairy product intake and risk of cardioembolic stroke in the Danish Diet, Cancer and Health cohort (102 cases). Adjusted for total energy intake, age at inclusion, education, waist circumference adjusted for body mass index, smoking, alcohol intake, physical activity and intakes of fruit, vegetables, red meat, processed meat and fish. The circles indicate hazard ratios and the whiskers indicate 95% CIs
We observed no statistically significant associations between substitutions of dairy products and risk of intracerebral hemorrhagic stroke (Table 4) or subarachnoid hemorrhagic stroke (Table 5), but the pattern of associations for intracerebral hemorrhage resembled those of large artery atherosclerosis and lacunar stroke.
Discussion
In this large population-based cohort study of middle-aged and older adults, we found that substitutions of whole-fat fermented milk for low-fat milk, whole-fat milk or buttermilk, regardless of fat content, were associated with a lower risk of ischemic stroke. Moreover, substitution of semi-skimmed fermented milk or cheese for whole-fat fermented milk was associated with a higher risk of ischemic stroke.
Strengths of this study include: the prospective cohort design, the nearly complete follow-up, the use of a validated FFQ and the large number of validated and classified stroke cases. In this study, loss to follow-up was solely due to emigration, and less than 1% of the participants emigrated during follow-up, rendering selection bias due to attrition unlikely to have affected our results. We invited all residents aged 50–64 years without a registered cancer diagnosis and living in two defined urban and suburban areas of Denmark. While participants generally were of higher socioeconomic position compared to non-participants [18], the direction of the associations is believed to be applicable across socioeconomic position. Moreover, the Diet, Cancer and Health cohort was established to investigate overall diet in relation to cancer and therefore it is unlikely that intake of subgroups of dairy products as well as one’s perceived future risk of stroke have been determinants for participation, thus we expect the associations for substitutions between dairy products and stroke to be similar in participants and non-participants, which limits the concern for selection bias. The detailed information about subgroups of dairy product intake, which was specifically addressed in the FFQ, enabled us to distinguish between milk and fermented milk with different fat contents, buttermilk, cheese and butter. Finally, information on diet intake was collected by an FFQ, which may reflect habitual diet intake. This makes an FFQ a suitable assessment method when investigating long-term exposure. However, the use of a single diet measurement and the long follow-up as well as diet intake being self-reported may have given rise to some non-differential misclassification of diet. The large number of verified stroke cases enabled us to investigate subtypes of ischemic stroke. The stroke diagnoses were established independently of the information from the FFQs and information bias is thus unlikely to have affected our results.
Despite thorough adjustment for lifestyle and dietary risk factors, residual confounding cannot be ruled out. However, given the strength of the observed associations after adjustment, potential unknown confounders must be strongly associated with stroke incidence to fully explain our results. Substitution of one food group with another such as fish for meat may be followed by changes in intake of other foods. Accordingly, the findings from substitution analyses adjusted for other foods may not easily be applied for dietary recommendations. However, this may be of less concern when substituting between dairy products, as we do not expect the choice of for instance type of milk to be followed by a difference in the accompanying foods.
We applied an analytical approach with specification of the substituting foods. Most previous studies have compared individuals with different intake of a single dietary exposure but similar intake of total energy, thus introducing a non-specified substitution model. Adjustment for total energy intake is a means to account for potential confounding of the diet-disease association by energy. However, without a specification of the food substitution, the interpretation of the results is unclear because the substituted foods may be neutral, harmful or beneficial in relation to the investigated disease, and people within and between populations may substitute foods differently. Data were therefore modelled using the following approach: We compared e.g. one individual with a reported intake of 2 servings of low-fat milk per day and 1 serving of whole-fat milk per day with another individual with a reported intake of 1 serving of low-fat milk per day and 2 servings of whole-fat milk per day. In other words, we investigated the rate of stroke associated with a 1 serving/day higher intake of one specified dairy product subgroup and a 1 serving/day lower intake of another specified dairy product subgroup. With this approach, the only unexplained part of the model is the difference in energy intake from other non-specified foods when equal serving sizes of products differing in energy are compared, or energy intake and amount of other non-specified foods when different serving sizes are compared.
Two other studies investigated food substitutions including dairy products in relation to stroke [23, 24]. Bernstein and colleagues investigated substitutions of low-fat or whole-fat dairy products for red meat [23] as well as substitution of skimmed milk for low-calorie or sugar-sweetened soda [24] and observed lower risks of total stroke associated with replacement of red meat and low-calorie soda, but not sugar-sweetened soda. These results support our theory that the associations between dairy products and stroke depend on which food is substituted and suggest that low-fat and whole-fat dairy products may be equally associated with stroke when substituting red meat. Similarly, our study underlines the importance of specifying substitutions. We observed that different types of dairy products are differently associated with stroke and that the associations depend on the specified substitutions, implying that dairy products are too complex to be evaluated based on their fat content alone. Furthermore, our results suggest that substitutions of dairy products may be differently associated with different stroke subtypes, as we found associations for ischemic stroke but not for hemorrhagic stroke. In particular, we observed a lower rate of large artery atherosclerotic stroke with substitutions of whole-fat fermented milk for low-fat milk, whole-fat milk or buttermilk, suggesting that whole-fat fermented milk intake may influence atherosclerotic plaque development. For cardioembolic stroke, unlike other subtypes of ischemic stroke, semi-skimmed fermented milk as a substitution for low-fat milk, whole-fat milk or buttermilk was associated with a lower risk. Atrial fibrillation is a major risk factor for cardioembolic stroke [2], thus the observed differences could reflect a different influence of dairy products on atrial fibrillation than atherosclerosis, but research is needed to confirm this. However, the results for semi-skimmed fermented milk as a substitution for other dairy product subgroups in relation to cardioembolic stroke should be interpreted with caution, as the analyses are based only on 102 cases.
Our findings suggest that whole-fat fermented milk products are preferable compared to other dairy products, which is in contrast to the DASH-diet [1], which includes a high intake of low-fat dairy products and is recommended for stroke prevention. Additional observational studies on substitutions between dairy product subgroups and risk of stroke as well as randomized trials investigating substitutions between dairy product subgroups in relation to intermediary end points are needed to further ascertain our findings. Plausible biological mechanisms for our findings may be found in the unique composition of dairy fat. Dairy fat contains conjugated linoleic acid originating from isomerization and biohydrogenation of unsaturated fatty acids in the rumen as well as conversion of vaccenic acid in the mammary gland of the cow [25]. Despite the conversion of vaccenic acid into conjugated linoleic acid by the cow, dairy fat also contains a considerable amount of vaccenic acid, which can be converted to conjugated linoleic acid endogenously by humans [26, 27]. Fermented milk products, unlike milk, contain probiotic cultures, such as lactobacilli and bifidobacteria, that may further increase the product content of conjugated linoleic acid through conversion of linoleic acid [28]. Conjugated linoleic acid has been proposed to have a number of health effects related to atherosclerosis, such as changes in body fat, lipid profile and blood pressure [29, 30]. In addition to this, different probiotic cultures may also individually exert anti-atherosclerotic effects [30]. Moreover, milk intake has been positively associated with urinary 8-iso-PGF2α, a biomarker of oxidative stress, whereas fermented milk intake has been negatively associated with 8-iso-PGF2α [31], offering another potential explanation as to why fermented milk products seem more favorable than milk.
In conclusion, this study suggests that intake of whole-fat fermented milk as a substitution for semi-skimmed fermented milk, cheese, buttermilk or milk, regardless of fat content, is associated with a lower rate of ischemic stroke.
References
Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–24. doi:10.1056/nejm199704173361601.
Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(2):517–84. doi:10.1161/STR.0b013e3181fcb238.
Larsson SC, Wallin A, Wolk A. Dietary approaches to stop hypertension diet and incidence of stroke: results from 2 prospective cohorts. Stroke. 2016;47(4):986–90. doi:10.1161/strokeaha.116.012675.
Gaucheron F. Milk and dairy products: a unique micronutrient combination. J Am Coll Nutr. 2011;30(5 Suppl 1):400s–9s.
Larsson SC, Orsini N, Wolk A. Dietary potassium intake and risk of stroke: a dose-response meta-analysis of prospective studies. Stroke. 2011;42(10):2746–50. doi:10.1161/STROKEAHA.111.622142.
Larsson SC, Orsini N, Wolk A. Dietary magnesium intake and risk of stroke: a meta-analysis of prospective studies. Am J Clin Nutr. 2012;95(2):362–6. doi:10.3945/ajcn.111.022376.
Larsson SC, Orsini N, Wolk A. Dietary calcium intake and risk of stroke: a dose-response meta-analysis. Am J Clin Nutr. 2013;97(5):951–7. doi:10.3945/ajcn.112.052449.
Dalmeijer GW, Struijk EA, van der Schouw YT, et al. Dairy intake and coronary heart disease or stroke—a population-based cohort study. Int J Cardiol. 2013;167(3):925–9. doi:10.1016/j.ijcard.2012.03.094.
Larsson SC, Mannisto S, Virtanen MJ, Kontto J, Albanes D, Virtamo J. Dairy foods and risk of stroke. Epidemiology. 2009;20(3):355–60. doi:10.1097/EDE.0b013e3181935dd5.
Larsson SC, Virtamo J, Wolk A. Dairy consumption and risk of stroke in Swedish women and men. Stroke. 2012;43(7):1775–80. doi:10.1161/STROKEAHA.111.641944.
Praagman J, Franco OH, Ikram MA, et al. Dairy products and the risk of stroke and coronary heart disease: the Rotterdam Study. Eur J Nutr. 2014;. doi:10.1007/s00394-014-0774-0.
Sonestedt E, Wirfalt E, Wallstrom P, Gullberg B, Orho-Melander M, Hedblad B. Dairy products and its association with incidence of cardiovascular disease: the Malmo diet and cancer cohort. Eur J Epidemiol. 2011;26(8):609–18. doi:10.1007/s10654-011-9589-y.
Louie JC, Flood VM, Burlutsky G, Rangan AM, Gill TP, Mitchell P. Dairy consumption and the risk of 15-year cardiovascular disease mortality in a cohort of older Australians. Nutrients. 2013;5(2):441–54. doi:10.3390/nu5020441.
Goldbohm RA, Chorus AM, Galindo Garre F, Schouten LJ, van den Brandt PA. Dairy consumption and 10-y total and cardiovascular mortality: a prospective cohort study in the Netherlands. Am J Clin Nutr. 2011;93(3):615–27. doi:10.3945/ajcn.110.000430.
Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH Jr, Folsom AR. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke. 2006;37(10):2493–8. doi:10.1161/01.STR.0000239694.19359.88.
Feigin VL, Rinkel GJ, Lawes CM, et al. Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies. Stroke. 2005;36(12):2773–80. doi:10.1161/01.STR.0000190838.02954.e8.
Hu G, Tuomilehto J, Silventoinen K, Sarti C, Mannisto S, Jousilahti P. Body mass index, waist circumference, and waist-hip ratio on the risk of total and type-specific stroke. Arch Intern Med. 2007;167(13):1420–7. doi:10.1001/archinte.167.13.1420.
Tjonneland A, Olsen A, Boll K, et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health. 2007;35(4):432–41. doi:10.1080/14034940601047986.
Overvad K, Tjonneland A, Haraldsdottir J, Ewertz M, Jensen OM. Development of a semiquantitative food frequency questionnaire to assess food, energy and nutrient intake in Denmark. Int J Epidemiol. 1991;20(4):900–5.
Tjonneland A, Overvad K, Haraldsdottir J, Bang S, Ewertz M, Jensen OM. Validation of a semiquantitative food frequency questionnaire developed in Denmark. Int J Epidemiol. 1991;20(4):906–12.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90. doi:10.2147/clep.s91125.
Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41. doi:10.1161/01.str.24.1.35.
Bernstein AM, Pan A, Rexrode KM, et al. Dietary protein sources and the risk of stroke in men and women. Stroke. 2012;43(3):637–44. doi:10.1161/STROKEAHA.111.633404.
Bernstein AM, de Koning L, Flint AJ, Rexrode KM, Willett WC. Soda consumption and the risk of stroke in men and women. Am J Clin Nutr. 2012;95(5):1190–9. doi:10.3945/ajcn.111.030205.
Collomb M, Schmid A, Sieber R, Wechsler D, Ryhänen E-L. Conjugated linoleic acids in milk fat: variation and physiological effects. Int Dairy J. 2006;16(11):1347–61. doi:10.1016/j.idairyj.2006.06.021.
Jakobsen MU, Bysted A, Andersen NL, et al. Intake of ruminant trans fatty acids in the Danish population aged 1–80 years. Eur J Clin Nutr. 2006;60(3):312–8. doi:10.1038/sj.ejcn.1602316.
Turpeinen AM, Mutanen M, Aro A, et al. Bioconversion of vaccenic acid to conjugated linoleic acid in humans. Am J Clin Nutr. 2002;76(3):504–10.
Andrade JC, AscenÇÃO K, GullÓN P, et al. Production of conjugated linoleic acid by food-grade bacteria: a review. Int J Dairy Technol. 2012;65(4):467–81. doi:10.1111/j.1471-0307.2012.00871.x.
Dilzer A, Park Y. Implication of conjugated linoleic acid (CLA) in human health. Crit Rev Food Sci Nutr. 2012;52(6):488–513. doi:10.1080/10408398.2010.501409.
DiRienzo DB. Effect of probiotics on biomarkers of cardiovascular disease: implications for heart-healthy diets. Nutr Rev. 2014;72(1):18–29. doi:10.1111/nure.12084.
Michaelsson K, Wolk A, Langenskiold S, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. 2014;349:g6015. doi:10.1136/bmj.g6015.
Acknowledgements
We wish to thank the Danish Cancer Society and the study personnel of the Diet, Cancer and Health cohort for data collection and management. We also wish to thank the study participants for their contribution to the study. This work was part of the project ‘Diet and prevention of ischemic heart disease: a translational approach’ (DIPI, www.dipi.dk), which is supported by the Danish Council for Strategic Research (Innovation Fund Denmark) (Contract 0603-00488B). The primary data collection for the Diet, Cancer and Health cohort was funded by the Danish Cancer Society. The funding agencies had no influence on the design, analysis or writing of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Laursen, A.S.D., Dahm, C.C., Johnsen, S.P. et al. Substitutions of dairy product intake and risk of stroke: a Danish cohort study. Eur J Epidemiol 33, 201–212 (2018). https://doi.org/10.1007/s10654-017-0271-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-017-0271-x