Abstract
The role of reproductive factors, such as parental age, in the pathogenesis of childhood leukemias is being intensively examined; the results of individual studies are controversial. This meta-analysis aims to quantitatively synthesize the published data on the association between parental age and risk of two major distinct childhood leukemia types in the offspring. Eligible studies were identified and pooled relative risk (RR) estimates were calculated using random-effects models, separately for childhood acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). Subgroup analyses were performed by study design, geographical region, adjustment factors; sensitivity analyses and meta-regression analyses were also undertaken. 77 studies (69 case–control and eight cohort) were deemed eligible. Older maternal and paternal age were associated with increased risk for childhood ALL (pooled RR = 1.05, 95 % CI 1.01–1.10; pooled RR = 1.04, 95 % CI 1.00–1.08, per 5 year increments, respectively). The association between maternal age and risk of childhood AML showed a U-shaped pattern, with symmetrically associated increased risk in the oldest (pooled RR = 1.23, 95 % CI 1.06–1.43) and the youngest (pooled RR = 1.23, 95 % CI 1.07–1.40) extremes. Lastly, only younger fathers were at increased risk of having a child with AML (pooled RR = 1.28, 95 % CI 1.04–1.59). In conclusion, maternal and paternal age represents a meaningful risk factor for childhood leukemia, albeit of different effect size by leukemia subtype. Genetic and socio-economic factors may underlie the observed associations. Well-adjusted studies, scheduled by large consortia, are anticipated to satisfactorily address methodological issues, whereas the potential underlying genetic mechanisms should be elucidated by basic research studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The two most common subtypes of childhood leukemia are acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). Genetic, environmental and lifestyle risk factors have been addressed in the literature regarding the pathogenesis of these conditions [1], including ionizing radiation [2], chemicals, timing of infectious diseases [3], allergy [4], parental smoking [5], maternal and childhood diet [6, 7], fertility treatments [8, 9] and birth weight [10]. The role of parental reproductive factors in the pathogenesis of childhood cancer seems to represent an intensively examined field, with rapid accumulation of knowledge [11].
The notion of maternal age in reproductive epidemiology becomes increasingly important, on account of the postponement of the first pregnancy to a later age due to the pursuit of career opportunities, as well as the growing awareness of infertility treatment options [12]. Parental age may therefore represent a multivalent index, integrating infertility problems, life decisions [13], as well as the socio-economic status of the family in which children are born [14].
Numerous studies examining the association between leukemia risk and parental age (maternal or paternal) have reached controversial results [15–19]. A meta-analysis has been recently published [20], addressing the association between risk for childhood ALL and maternal factors; among the latter, maternal age was not significantly associated with ALL risk. On the contrary, significant associations with birth order, maternal education and maternal smoking were observed [20]. Nevertheless, it should be underlined that the aforementioned meta-analysis suffered from methodological problems [21] and treated maternal age as a binary variable (>30 vs. <30 years or >35 vs. <35 years), precluding any examination of an underlying U-shaped curve; of note, the effect of paternal age was not addressed. Meaningful subgroups, such as separate synthesis in cohort and case–control studies, were not addressed either therein. Moreover, the association between parental age and childhood AML represents a totally undiscovered field at the meta-analytical level.
Taking the aforementioned into account, the present meta-analysis aims to examine the associations between parental age (maternal as well as paternal) with childhood leukemia types (ALL, AML), addressing a variety of potentially meaningful methodological considerations in the individual studies.
Materials and methods
Search strategy and eligibility of studies
This meta-analysis was performed in accordance with the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines. The potentially eligible publications were sought in PubMed using the search algorithm [(parental OR paternal OR maternal OR mother OR mother’s OR father OR father’s) AND age] AND (leukemia OR leukaemia OR leukemias OR leukaemias OR [(haematological OR hematological) AND (cancer OR cancers OR malignancy OR malignancies)] AND (child OR children OR childhood) with end of search date September 30, 2014. There was no restriction regarding publication language; reference lists were systematically searched for relevant articles (“snowball” procedure).
Eligible articles included case–control as well as cohort studies examining the association between maternal/paternal age and risk of childhood leukemia (acute lymphoblastic leukemia, ALL; acute myeloid leukemia, AML; mixed reporting of leukemia cases) in the offspring. Studies exclusively recruiting children with Down syndrome, or studies whose controls were not cancer-free children were not deemed eligible for this meta-analysis. Similarly to previous meta-analyses issued by our team [5, 14], the most recent NARECHEM data were provided updating earlier relevant publications on the field.
In case of overlapping study populations (>50 % of cases), only the larger study was included. Nevertheless, in cases of partial overlap (25–50 %), as was the case in large consortia, both studies were retained and one of them was thereafter removed in a sensitivity analysis. The corresponding authors were contacted twice (a reminder e-mail was sent 7 days after the first e-mail) for the clarification of overlap between studies in case this was not clear from the manuscripts. The selection of studies was performed by authors working in pairs, blindly to each other; in case of disagreement, the decision was made with team consensus.
Data extraction and effect estimates
The extraction of data comprised first author’s name, study year, journal, type of study, follow-up period, study region, subjects’ age (range, mean), percentage of males, numbers and sources of information for cases and controls (for case–control studies), matching factors (for case–control studies), cohort size, incident cases, cohort features and definition of the outcome (for cohort studies), type of cases (incident; mortality), case ascertainment, participation rate, source of information regarding parental age, factors adjusted for in multivariate analyses, primary exposure of interest in the studies. The data abstraction was performed by authors working in pairs, blindly to each other; in case of disagreement, the decision was made with team consensus.
The maximally adjusted effect estimates i.e., Odds Ratios (ORs) for case–control studies or Relative Risks (RRs) for cohort studies, with their Confidence Intervals (CIs) were extracted from each study by leukemia subtype, maternal or paternal age categories or increments. In case the aforementioned information was not available, crude effect estimates and 95 % CIs were calculated by means of 2 × 2 tables presented in the articles.
Statistical analysis
Random-effects (DerSimonian-Laird) models were used to calculate pooled effect estimates, as appropriate. Between-study heterogeneity was evaluated through Cochran Q statistic and by estimating I 2 [22]. Pooling of studies comprised two distinct approaches: first, the incremental effect estimates of maternal/paternal age (in 5-year increments) on childhood leukemia risk were pooled. Moreover, the “youngest” versus intermediate, as well as the “oldest” versus intermediate comparisons between age categories were pooled, to evaluate the presence of U-shaped effects, if any. Sensitivity analyses were performed by partial overlap and cut-off values of extreme age categories (>35, >40, <20 years of age).
Separate analyses were conducted for ALL, AML and studies with mixed reporting of leukemia cases; maternal and paternal age was analyzed separately. Subgroup analyses were performed by study design (case–control; cohort), geographical region and quality of studies (degree of adjustment; overall Newcastle-Ottawa Quality score). Regarding the degree of adjustment, the term “with mutual adjustment” refers to studies that have adjusted maternal age for paternal age measurements, and paternal for maternal, whereas the term “no mutual adjustment” refers to studies that adjusted only for other factors. Statistical analysis was performed using STATA/SE version 13 (Stata Corp, College Station, TX, USA).
Risk of bias, meta-regression analysis
The quality of the included studies was evaluated using the Newcastle-Ottawa Quality scale [23]. Regarding longitudinal cohort studies, the item assessing whether the follow-up period was enough for the outcome to occur, the cut-off value was a priori set at 4 years, whereas the item evaluating the adequacy of follow-up required a minimum of 80 %. The evaluation of the quality in the eligible studies was performed by authors working in pairs, blindly to each other; in case of disagreement, the decision was made with team consensus.
Egger’s statistical test was implemented to evaluate the evidence of publication bias. For the interpretation of Egger’s test, statistical significance was defined as p < 0.1. Meta-regression analysis aimed to assess whether publication year (in increments of 10 years, assuming there is a continuous change in effect estimates over calendar time), gender of the offspring (expressed as percentage of males in the eligible studies/study arms) and age (expressed as the mean age in the individual studies/study arms) modified the documented associations. Meta-regression analysis and evaluation of publication bias were performed using STATA/SE 13 (Stata Corp, College Station, TX, USA).
Results
The flow chart describing the successive steps during the selection of eligible studies is presented in Supplemental Figure 1. A total of 767 abstracts were identified and screened; details regarding the selection of studies, the e-mails sent to the corresponding authors and the reference list of the included studies are presented in Supplemental Results, whereas Supplemental Table 1 presents the list of studies retrieved in full text that were afterwards excluded for a variety of stated reasons.
Tables 1 and 2 present the characteristics of the included studies, namely 69 case–control and eight cohort studies, respectively. Taken as a whole, 67 studies reported on maternal age as a categorical variable, namely 60 case–control studies (corresponding to 25,335 ALL cases, 4164 AML cases, 24,469 cases of “mixed” childhood leukemias and 111,055 controls) and seven cohort studies (1850 incident ALL, 114 AML and 1746 mixed leukemia cases in a total cohort size of 12,522,500 children). On the other hand, 15 studies examined maternal age as an incremental variable, namely 12 case–control studies (corresponding to 13,642 ALL, 2461 AML, 14,068 “mixed” childhood leukemia cases and 56,061 controls) and three cohort studies (1003 incident ALL, 114 AML and 1427 mixed leukemia cases in a total cohort size of 8,608,739 children).
Regarding paternal age, 38 studies examined paternal age as a categorical variable, namely 34 case–control studies (corresponding to 21,371 ALL cases, 3647 AML cases, 15,688 cases of “mixed” childhood leukemia cases and 69,740 controls) and four cohort studies (1191 incident ALL, 114 AML and 1427 mixed leukemia cases in a total cohort size of 9,043,672 children). Twelve studies evaluated paternal age as an incremental variable, namely nine case–control studies (corresponding to 12,736 ALL, 2202 AML, 13,522 “mixed” childhood leukemia cases and 46,674 controls) and three cohort studies (1003 incident ALL, 114 AML and 1427 mixed leukemia cases in a total cohort size of 8,608,739 children).
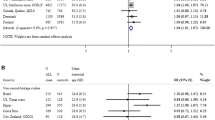
Maternal age and risk for ALL
The upper part of Table 3 presents the results of meta-analyses regarding the association between maternal age and risk of ALL. The incremental analysis pointed to an association between older maternal age and increased risk for childhood ALL (pooled RR = 1.05, 95 % CI 1.01–1.10, per 5 years, Fig. 1), which was particularly evident among cohort and European studies. Of note, this association was also significant among the subset of unadjusted studies (pooled RR = 1.09, 95 % CI 1.03–1.14, Supplemental Figure 2).
Similarly to this pattern, the “oldest versus middle” comparison pointed to increased risk for ALL among the offspring from oldest mothers (pooled RR = 1.10, 95 % CI 1.00–1.21, Supplemental Figures 3–6), a finding which was reproducible among the subset of case–control studies, as well studies published in the Americas. The paucity of effect estimates with mutual adjustment between maternal and paternal age became evident, as only three studies adopted such a design (Supplemental Figure 5). Sensitivity analyses according to the cut-off adopted (Supplemental Figure 6) indicated persistence of the positive association among studies setting the cut-off at 35 years (pooled RR = 1.14, 95 % CI 1.02–1.27); however, only five studies adopted a cut-off point at 40 years and their pooling yielded a sizable but non-significant effect estimate (pooled RR = 1.27, 95 % CI 0.89–1.81).
The “youngest versus middle” comparison did not point to nominally significantly increased risk for ALL among youngest mothers (pooled RR = 1.09, 95 % CI 0.99–1.19, p = 0.077). No consistently significant associations arose in subgroup analyses, including the sensitivity analysis examining the extreme age category of women giving birth prior to 20 years of age (Supplemental Figures 7–10).
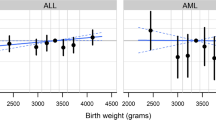
Maternal age and risk for AML
The lower parts of Table 3 present the results of meta-analyses on the association of maternal age and risk of AML. The overall pattern showed a U-shaped association, as both oldest (pooled RR = 1.23, 95 % CI 1.06–1.43, Fig. 2a) and youngest extremes (pooled RR = 1.23, 95 % CI 1.07–1.40, Fig. 2b) were symmetrically associated with increased risk for AML; consequently, the incremental analysis was close to the null value of one (pooled RR = 1.02, 95 % CI 0.95–1.10).
Subgroup and sensitivity analyses were rather hampered by the small number of study arms; it seems however worth noting that regarding oldest age (Supplemental Figures 11–13), the association was reproducible among high-quality studies. Moreover, only three studies examined age categories older than 40 years and yielded a sizable but non-significant effect estimate (pooled RR = 1.99, 95 % CI 0.45–8.89). Concerning youngest age (Supplemental Figures 14–15), the sizable association with AML risk persisted among studies with adjusted effect estimates, including those with mutual adjustment between maternal and paternal age. Regarding incremental analyses, the null association persisted except for an association in non-adjusted studies (Supplemental Figure 16).
Paternal age and risk for ALL
The upper parts of Table 4 present the results pertaining to the association between paternal age and risk of ALL. The incremental analysis suggested a positive association between older paternal age and increased risk for childhood ALL (pooled RR = 1.04, 95 % CI 1.00–1.08, per 5 years, Fig. 3), which was particularly evident among high-quality, case–control and European studies, which at any case represented the majority of eligible study arms. Similarly to maternal age, this association was significant among unadjusted studies (pooled RR = 1.09, 95 % CI 1.00–1.19, Supplemental Figure 17).
The “oldest versus middle” comparison pointed to increased risk for childhood ALL among offspring from oldest fathers (pooled RR = 1.10, 95 % CI 1.02–1.19, Supplemental Figures 18–20); this was reproducible in high-quality, case–control, European and unadjusted studies, which represented the majority of synthesized data. Sensitivity analyses on the adopted cut-off (Supplemental Figure 20) indicated persistence of the positive association among studies setting the cut-off at 35 years (pooled RR = 1.12, 95 % CI 1.03–1.21), whereas only five studies set a cut-off value at 40 years or older and did not point to a sizable association.
The “youngest versus middle” comparison suggested a marginally elevated risk for ALL among youngest fathers (pooled RR = 1.09, 95 % CI 1.00–1.20), which was mainly due to case–control, intermediate-quality and unadjusted studies (Supplemental Figures 21–23).
Paternal age and risk for AML
The results of meta-analyses on the association between paternal age and risk of AML are presented in the lower parts of Table 4. No significant association was documented either at the incremental analysis (pooled RR = 1.04, 95 % CI 0.98–1.09, Supplemental Figures 24–25) or at the “oldest versus middle” comparison (pooled RR = 1.05, 95 % CI 0.87–1.26, Supplemental Figures 26–28). On the other hand, increased risk for AML was noted in offspring from younger fathers (pooled RR = 1.28, 95 % CI 1.04–1.59, Supplemental Figures 29–31); this association was evident in case–control, intermediate-quality and unadjusted studies.
Risk for leukemia in studies with mixed reporting
Supplemental Table 1 (Supplemental Figures 32–34) presents the results of meta-analyses examining the association between maternal/paternal age and risk of leukemia in studies with mixed reporting of subtypes. Given the admixture of subtypes and superimposition of patterns, no consistent associations were observed, except for a positive association between maternal age and risk of leukemia in the incremental analysis.
Additional sensitivity analysis removing studies with partial overlap
The results of the additional sensitivity analysis removing studies with partial overlap are depicted in Supplemental Figures 35–38. The documented associations persisted during this approach, as a rule.
Evaluation of quality of studies, meta-regression analysis and risk of bias
The evaluation of quality of studies is presented in Supplemental Table 2. Notions that led to decreased quality of case–control studies included the lack of adjusted effect estimates, the self-reported parental age, as well as the inclusion of hospital-based controls. The quality of cohort studies was often compromised by unadjusted effect estimates; on the other hand, the length of follow-up was satisfactory, as a rule.
Supplemental Table 3 presents the results of meta-regression analysis. No modifying effects mediated by publication year or mean age of study subjects were observed. Larger percentage of male offspring in the individual studies was associated with 1.5-fold increased RRs for mixed leukemia at the analysis pertaining to oldest mothers (exponentiated coefficient = 1.45, 95 % CI 1.02–2.05) and 1.8-fold increased RRs for AML at the analysis concerning youngest fathers (exponentiated coefficient = 1.85, 95 % CI 1.02–3.35).
The results of Egger’s test are presented in Supplemental Table 4; no evidence of publication bias was documented in any analysis.
Discussion
This meta-analysis, based on a considerable number of study subjects and a well-defined exposure variable, presents a compendium of novel messages regarding the role of parental age in the epidemiology of childhood leukemia. Older maternal age was found to be associated with 5 % increased risk for childhood ALL in the offspring for every 5-year increase in maternal age; this was reflected among the oldest maternal age categories across all included studies, which presented with 10 % increased risk for childhood ALL compared to the averagely-aged mothers. On the other hand, maternal age was associated with risk of childhood AML in a U-shaped manner, as both oldest and youngest extremes were symmetrically associated with 23 % increased risk for AML; consistently, in view of the underlying, strikingly symmetric pattern, the incremental analysis yielded a null result.
Apart from the mother, this meta-analysis also brings to the foreground the role of fathers in the epidemiology of childhood leukemia. Although the roles of maternal and paternal age cannot be easily disentangled, as they are often be closely associated with each other, the meta-analysis yielded evidence that older paternal age correlated with increased risk for childhood ALL in the offspring, with 4 % increased risk observed for every 5-year increase in paternal age. Interestingly, younger fathers seemed at 28 % increased risk of having a child with childhood AML compared to their average-aged counterparts; the respective association with ALL was substantially milder, therefore not being able to neutralize the overall incremental pattern.
Regarding older parental age, the underlying mechanisms seem to entail a genetic component, given that older parental age could theoretically lead to increased risk for childhood leukemia in view of genetic hits accumulating in the germ cells [24]. Apart from this traditionally anticipated association applying to both parents, the increased risk for leukemias (AML and, to a lesser extent, ALL) noted among the offspring of younger fathers seems considerably more intriguing. Strikingly, a recently published study highlighted elevated germline mutation rates in teenage fathers, with the sperm cells of adolescent boys having more than six times the rate of DNA mutations as the equivalent egg cells in adolescent girls, a fact that may result in higher rates of DNA mutations being passed down to children of teenage fathers [25]. Apart from the genetic factor, the lower socioeconomic and educational status of the youngest parents [26] may underlie the observed associations; a broader analogy emerges, as studies in various fields have documented increased morbidity among children stemming from younger parents [27]. Lower socioeconomic status in teenaged parenthood may also signal the presence of numerous coexistent potential risk factors, such as parental smoking [28] or alcohol consumption, that are often intercorrelated and socially patterned [29]. Furthermore, it should be kept in mind that this finding was mainly based on case–control studies; recruitment of young father controls may have been historically difficult due to limited phone access or high mobility, hence the results should be interpreted with caution.
As our eligible studies span nearly six decades and researchers have supported the importance of temporal trends along birth cohorts [30], it seemed of special importance to perform a meta-regression analysis, which suggested, however that publication year did not modify the observed associations. Moreover, the observed associations were not modified by the mean age of participants. On the other hand, male offspring seemed occasionally more burdened by the effects of parental age; the underlying mechanisms for this observation remain unknown. It seems worth noting nevertheless that meta-analyses on the detrimental effects of parental age on other conditions, such as schizophrenia [31] and autism [32], have pointed to special vulnerability of male versus female offspring.
Apart from pooling data to arrive to a meta-estimate, this study served the effort to address heterogeneity in the published data. Regarding oldest and youngest maternal age, heterogeneity was moderate for ALL but impressively small for AML; moderate heterogeneity was noted for father’s age at the respective analyses, as a rule. On the other hand, incremental analyses presented with substantial heterogeneity for ALL in both maternal and paternal age, whereas the respective measures were only indicative of moderate heterogeneity for AML; notably, in all major analyses, I 2 value was <75 % [22]. As evident in the conducted subgroup analyses and meta-regression analyses, sources of heterogeneity included study design, geographic regions reflecting genetic factors as well as socio-cultural aspects pertaining to the reproductive age, the overall study quality and especially adjustment factors, as well as the degree of representation of male children in the studies. On the other hand, period effects (assessed through publication year) did not seem to play a major role.
From a methodological point of view, this meta-analysis highlights many features and shortcomings of the existing literature, opening the way to future studies. Numerous studies presented unadjusted effect estimates; moreover, among those which presented adjusted relative risks, only a small subset proceeded to a mutual adjustment between maternal and paternal age. Nevertheless, in view of the present findings, which equally recognize the importance of the maternal and paternal factor, it seems desirable to envisage future studies discriminating between the two effects in terms of elaborate adjusting, taking always care of the potential collinearity that these factors may present. At this point, the limitation of the meta-analysis approach as a research tool versus the pooled analysis of individual data should be acknowledged; consortia with individual family data on both maternal and paternal age seem to be needed for the optimal evaluation of this research question. Regarding the external generalizability of findings, it seems worth underlining that the majority of studies came from Europe and North America; Asia, Latin America were underrepresented, whereas there was a lack of data concerning Africa.
Further on, it seems desirable that future studies proceed to meticulous analyses, presenting both incremental and categorical approaches. On one hand, given the U-shaped association in AML, a purely incremental analysis seems inadequate. On the other hand, incremental analyses provide a straightforward, uniform way to quantify the effect of exposure; in our meta-analyses, only a subset of studies approached the phenomenon incrementally and therefore the study numbers in incremental analyses were considerably smaller than the respective categorical ones. Moreover, wherever possible given the sample size, extreme age subgroups should also be examined; in our approach, sensitivity analyses focusing on the extremes of <20 and >40 years of age were undertaken in an attempt to explore dose–response patterns, but were essentially hampered by the small number of eligible study arms. Separate reporting by ALL and AML seems a minimum recommendation, given that admixture of cases in studies examining total leukemia does not allow the emergence of clear patterns, as highlighted by our Supplementary analysis. In addition, future studies should ideally aim to report results by immunophenotype or genetic subgroups, to allow the testing of underlying mechanisms on a genetic basis.
Despite the aforementioned notions pertaining to the methodology of constituent eligible studies, the meta-analysis bears certain strengths, among which the large number of studies and study subjects, the lack of publication bias, as well as the fact that cohort and case–control studies pointed to the same direction, as a rule. Nevertheless, additional data derived from cohort studies seem desirable, as the majority of data came from case–control studies, which are inherently prone to biases [33]. Finally, in our subgrouping strategy, we did not further subdivide on the basis of geography, degree of adjustment or overall quality, separately in the case–control and cohort subsets, in view of the emerging small numbers of study arms that would render the effect estimates unstable.
In conclusion, this meta-analysis portrays maternal as well as paternal age as meaningful risk factors for childhood leukemias. ALL and AML may well follow distinct patterns in their associations with parental age. Further, well-adjusted studies, eventually coming from large consortia, are anticipated to address methodological issues satisfactorily, whereas the potential underlying genetic mechanisms should be elucidated by basic research studies.
References
Belson M, Kingsley B, Holmes A. Risk factors for acute leukemia in children: a review. Environ Health Perspect. 2007;115:138–45.
Adami HO, Hunter D, Trichopoulos D. Textbook of cancer epidemiology. Oxford: Oxford University Press; 2008.
Urayama KY, Buffler PA, Gallagher ER, Ayoob JM, Ma X. A meta-analysis of the association between day-care attendance and childhood acute lymphoblastic leukaemia. Int J Epidemiol. 2010;39:718–32.
Lariou MS, Dikalioti SK, Dessypris N, Baka M, Polychronopoulou S, Athanasiadou-Piperopoulou F, et al. Allergy and risk of acute lymphoblastic leukemia among children: a nationwide case control study in Greece. Cancer Epidemiol. 2013;37:146–51.
Klimentopoulou A, Antonopoulos CN, Papadopoulou C, Kanavidis P, Tourvas AD, Polychronopoulou S, et al. Maternal smoking during pregnancy and risk for childhood leukemia: a nationwide case-control study in Greece and meta-analysis. Pediatr Blood Cancer. 2012;58:344–51.
Diamantaras AA, Dessypris N, Sergentanis TN, Ntouvelis E, Athanasiadou-Piperopoulou F, Baka M, et al. Nutrition in early life and risk of childhood leukemia: a case-control study in Greece. Cancer Causes Control. 2013;24:117–24.
Petridou E, Ntouvelis E, Dessypris N, Terzidis A, Trichopoulos D. Maternal diet and acute lymphoblastic leukemia in young children. Cancer Epidemiol Biomarkers Prev. 2005;14:1935–9.
Rudant J, Amigou A, Orsi L, Althaus T, Leverger G, Baruchel A, et al. Fertility treatments, congenital malformations, fetal loss, and childhood acute leukemia: the ESCALE study (SFCE). Pediatr Blood Cancer. 2013;60:301–8.
Petridou ET, Sergentanis TN, Panagopoulou P, Moschovi M, Polychronopoulou S, Baka M, et al. In vitro fertilization and risk of childhood leukemia in Greece and Sweden. Pediatr Blood Cancer. 2012;58:930–6.
Caughey R, Michels K. Birth weight and childhood leukemia: a meta-analysis and review of the current evidence. Int J Cancer. 2009;124:2658–70.
Hargreave M, Jensen A, Toender A, Andersen KK, Kjaer SK. Fertility treatment and childhood cancer risk: a systematic meta-analysis. Fertil Steril. 2013;100:150–61.
Kimberly L, Case A, Cheung AP, Sierra S, AlAsiri S, Carranza-Mamane B, et al. Advanced reproductive age and fertility: no. 269, November 2011. Int J Gynaecol Obstet. 2012;117:95–102.
Sergentanis T, Dessypris N, Kanavidis P, Skalkidis I, Baka M, Polychronopoulou S, et al. Socioeconomic status, area remoteness, and survival from childhood leukemia: results from the Nationwide Registry for Childhood Hematological Malignancies in Greece. Eur J Cancer Prev. 2012.
Petridou ET, Sergentanis TN, Perlepe C, Papathoma P, Tsilimidos G, Kontogeorgi E, et al. Socioeconomic disparities in survival from childhood leukemia in the United States and globally: a meta-analysis. Ann Oncol. 2015;26:589–97.
Ou SX, Han D, Severson RK, Chen Z, Neglia JP, Reaman GH, et al. Birth characteristics, maternal reproductive history, hormone use during pregnancy, and risk of childhood acute lymphocytic leukemia by immunophenotype (United States). Cancer Causes Control. 2002;13:15–25.
Ma X, Metayer C, Does MB, Buffler PA. Maternal pregnancy loss, birth characteristics, and childhood leukemia (United States). Cancer Causes Control. 2005;16:1075–83.
Reynolds P, Von Behren J, Elkin EP. Birth characteristics and leukemia in young children. Am J Epidemiol. 2002;155:603–13.
Kaye SA, Robison LL, Smithson WA, Gunderson P, King FL, Neglia JP. Maternal reproductive history and birth characteristics in childhood acute lymphoblastic leukemia. Cancer. 1991;68:1351–5.
Stark CR, Mantel N. Maternal-age and birth-order effects in childhood leukemia: age of child and type of leukemia. J Natl Cancer Inst. 1969;42:857–66.
Yan K, Xu X, Liu X, Wang X, Hua S, Wang C. The associations between maternal factors during pregnancy and the risk of childhood acute lymphoblastic leukemia: a meta-analysis. Pediatr Blood Cancer. 2015.
Thomopoulos TP, Sergentanis TN, Karalexi MA, Petridou ET. Methodological remarks regarding the meta-analysis on possible associations of maternal factors during pregnancy with the risk of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 2015.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. In: The Cochrane Collaboration. 2011 http://handbook.cochrane.org/. Accessed 30 Jan 2014.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa: Ottawa. 2011. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm. Accessed 30 Jan 2014.
Walter CA, Walter RB, McCarrey JR. Germline genomes—a biological fountain of youth? Sci Aging Knowledge Environ. 2003; 2003:PE4.
Forster P, Hohoff C, Dunkelmann B, Schurenkamp M, Pfeiffer H, Neuhuber F, et al. Elevated germline mutation rate in teenage fathers. Proc Biol Sci. 2015;282:20142898.
Mills M, Rindfuss RR, McDonald P, te Velde E. Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update. 2011;17:848–60.
McGrath JJ, Petersen L, Agerbo E, Mors O, Mortensen PB, Pedersen CB. A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiatry. 2014;71:301–9.
Antonopoulos CN, Sergentanis TN, Papadopoulou C, Andrie E, Dessypris N, Panagopoulou P, et al. Maternal smoking during pregnancy and childhood lymphoma: a meta-analysis. Int J Cancer. 2011;129:2694–703.
Wellings K, Wadsworth J, Johnson A, Field J, Macdowall W. Teenage fertility and life chances. Rev Reprod. 1999;4:184–90.
Maule MM, Merletti F, Pastore G, Magnani C, Richiardi L. Effects of maternal age and cohort of birth on incidence time trends of childhood acute lymphoblastic leukemia. Cancer Epidemiol Biomarkers Prev. 2007;16:347–51.
Miller B, Messias E, Miettunen J, Alaraisanen A, Jarvelin MR, Koponen H, et al. Meta-analysis of paternal age and schizophrenia risk in male versus female offspring. Schizophr Bull. 2011;37:1039–47.
Sandin S, Hultman CM, Kolevzon A, Gross R, MacCabe JH, Reichenberg A. Advancing maternal age is associated with increasing risk for autism: a review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2012;51(477–86):e1.
Schwartzbaum J, Ahlbom A, Feychting M. Berkson’s bias reviewed. Eur J Epidemiol. 2003;18:1109–12.
Acknowledgments
The authors would like to thank Dr. Jie Song, Karolinska Institutet, for the translation of Chinese articles on the field, as well as the corresponding authors of studies who replied to our Letters, as detailed in the Supplemental Results section.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sergentanis, T.N., Thomopoulos, T.P., Gialamas, S.P. et al. Risk for childhood leukemia associated with maternal and paternal age. Eur J Epidemiol 30, 1229–1261 (2015). https://doi.org/10.1007/s10654-015-0089-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-015-0089-3