Abstract
Increased fibroblast growth factor 23 (FGF23) concentrations have emerged as a novel risk factor for heart failure and stroke but not for myocardial infarction (MI). Yet, most studies on MI were conducted in coronary artery disease (CAD) patients and the elderly. Evidence is unclear in subjects without CAD and for stroke subtypes. We investigated the relationships between FGF23 and overall major cardiovascular endpoints, incident MI, ischemic (IS) and haemorrhagic stroke (HS) in middle-aged adults without pre-existing cardiovascular disease. We used a case-cohort study nested within the European Prospective Investigation into Cancer and Nutrition-Germany, including a randomly drawn subcohort (n = 1,978), incident MI (n = 463) and stroke cases (n = 359 IS; n = 88 HS) identified during a mean follow-up of 8.2 years. Compared with participants with FGF23 levels in the lowest quartile, those in the highest quartile had a 36 % increased risk for cardiovascular events [hazard ratio: 1.36, 95 % confidence interval (CI): 1.02–1.82] after adjustment for established cardiovascular risk factors, patahyroid hormone and 25-hydroxyvitamin D3 levels, dietary calcium and phosphorus intake, and kidney function. However, sub-analyses revealed significant relationships with risk of MI and HS, but not IS. Compared with the lowest quartile, individuals in the top two FGF23 quartiles had a 1.62 (95 % CI 1.07–2.45) fold increased risk for MI and a 2.61 (95 % CI 1.23–5.52) fold increase for HS. Increased FGF23 emerged as a risk factor for both MI and HS. Further studies are warranted to confirm these results and to identify underlying mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases (CVD) are still the biggest killer in Europe. Therefore, the identification on novel CVD risk factors is highly warranted.
Fibroblast growth factor 23 (FGF23), a hormone mainly secreted by osteocytes and osteoblasts in bone [1], is an emerging marker of bone mineral metabolism. FGF23 affects phosphate and vitamin D metabolism [2]. Also, it regulates the expression of its co-receptor, α-klotho, and parathyroid hormone (PTH) levels [3]. Recently, higher FGF23 levels have been identified as a major non-traditional cardiovascular risk factor in chronic kidney disease patients [4]. Such insights raised the question whether FGF23 might predict cardiovascular events even in the general population.
So far, epidemiologic studies have examined FGF23 in relation to CVD risk, or mortality, [5–9] and found a significant relationship between FGF23, and heart failure (HF) [5, 7, 9, 10] as well as stroke [7, 11]; while no significant association was observed with coronary heart disease [6] or MI [5, 7, 9]. Recently, FGF23 has been shown to be a predictor of major cardiovascular events independently of mineral metabolism abnormalities and subclinical cardiovascular injury [8]. Yet, few previous studies including MI and stroke as endpoints were conducted in patients with stable/chronic coronary artery disease (CAD) and elderly people, or in men only, and did not differentiate between ischemic (IS) and haemorrhagic stroke (HS). Only one study specifically examined FGF23 levels as a risk factor for stroke and its subtypes, and found an association between higher FGF23 levels and risk of both total and intracerebral hemorrhage stroke events [11]. These findings, observed in an urban population of Hispanic/Latino participants, indeed need to be confirmed in other populations. Furthermore, based on the recent discovery that FGF23 regulates renal sodium and blood pressure, thus leading to hypertension and heart hypertrophy [12], we hypothesized that FGF23 might be involved in the pathophysiological mechanisms of myocardial infarction (MI) and stroke development [13]. Therefore, we aimed to investigate whether increased FGF23 is related to the risk of MI, total, IS and HS in a Caucasian population of apparently healthy middle aged men and women without pre-existing MI and stroke at baseline.
In the present study the relationships between FGF23 and the risk of developing MI, stroke and its subtypes (IS and HS) were investigated in a prospective case-cohort study nested within the European Prospective Investigation into Cancer and Nutrition (EPIC)-Germany cohort.
Methods
Study population and design
The EPIC is an ongoing multi-centre prospective cohort study designed to investigate the relationships between diet, metabolic characteristics, various lifestyle factors and the risk of cancer as well as other chronic diseases [14, 15]. Co-ordinated by the international agency for research on cancer (IARC) of the World Health Organisation (WHO) in Lyon, France, the EPIC-study started in 1992 and it currently includes 519,978 participants who were recruited until 2000 in 10 European countries, for a total of 23 centres. Among them two centres in Heidelberg and Potsdam represent the German contribution to the EPIC [16].
EPIC-Germany comprises two cohorts at the study centres in Potsdam (27,548 participants: 16,644 women and 10,904 men; 5th and 95th age percentiles: 36–64) and Heidelberg (25,543 participants: 13,614 women and 11,929 men; 5th and 95th age percentiles: 37–63). Participants were recruited from the local general populations between 1994 and 1998 [16, 17]. Active procedures including mailing of questionnaires in 2–4 year intervals, written reminders and telephone calls for the return of the follow-up questionnaire, tracing of subjects, personal interaction with participants and passive procedures comprising linkages with hospital data bases and death indexes are used to follow participants [18].
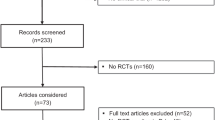
For the present analyses a case-cohort study design was chosen [19]. The study sample consisted of subcohorts randomly selected from Heidelberg and Potsdam cohorts. Both subcohorts were constructed using a sampling fraction of 5 %, stratified by centre, according to the protocol of the EPIC InterAct study on type 2 diabetes [20]. In contrast to the InterAct selection criteria, however, prevalent cases of type 2 diabetes mellitus were not excluded. Therefore, among n = 53,088, a subcohort of 2,280 individuals was randomly selected from those with available stored blood and buffy coat (n = 50,680). In addition, all verified incident cases of MI and stroke from complete follow-up rounds up to the end of December 2006 were included into the case-cohort study. After exclusion of participants with prevalent MI or stroke (n = 76), with unclear follow-up data (n = 66), belonging to a previous pilot study (n = 181), with unclear FGF23 and PTH measures (n = 7), or with a suspected primary parathyroid disorder (n = 29), the final case-cohort study consisted of a subcohort of 2,022 participants (of whom 44 CVD cases) and 886 external primary CVD cases (463 incident MI and 467 stroke cases) identified during a mean follow-up of 8.2 years (Fig. 1). Stroke cases were classified as IS (n = 359), HS (n = 88), and unknown (n = 20).
Ascertainment of incident myocardial infarction and stroke
Up to the end of December 2006 all incident MI and stroke cases from complete follow-up rounds were included into the case-cohort study. Only medically verified cases were used for the present analyses. To identify potential cases of incident MI or stroke several sources were used: self-report in one of the four follow-up questionnaires, death certificate or linkage with hospital databases. All identified potential CVD events were ascertained by study physicians, in cooperation with treating physicians and hospitals, who provided a detailed and systematic medical verification of self-reports and death certificates by clinical records [21, 22] according to World Health Organization monitoring of trends and determinants in cardiovascular disease (MONICA) criteria [23]. Thereby, information on clinical features, ECG and cardiac enzymes were used to verify and classify an MI. For definition and classification of stroke cases MRI or CT and clinical symptoms were used. According to the International Statistical Classification of Diseases, 10th Revision (ICD-10), cases were classified as incident MI (ICD-10 I21), IS (ICD-10 I63.0 to I63.9), intracerebral (ICD-10 I61.0 to I61.9) or subarachnoid hemorrhage (ICD-10 I60.0 to I60.9), or undetermined stroke (ICD-10 I64.0-I64.9) by two physicians in the study centre. Death within 28 days after diagnosis of MI or stroke and a death certificate in which the underlying cause of death was recorded with the above ICD-10 codes was considered as a fatal event [24].
Exposure and covariate measurements
At baseline, a blood sample was drawn, processed and stored in liquid nitrogen at –196 C [16, 25]. In 2011, FGF23, PTH, and 25-hydroxyvitamin D3 (25(OH)D3) were measured in the Institute of Agricultural and Nutritional Science, University of Halle, Germany. The Human FGF23 (C-Terminal) enzyme-linked immunosorbant assay (ELISA) kit (Immutopics, San Clemente, CA, USA) was used to measure FGF23 concentrations in citrate plasma [26]. Plasma PTH (intact) was measured by an ELISA Kit (Biomerica, Irvine, CA, USA). The plasma concentration of 25(OH)D3 was analysed by LC–MS/MS as described previously [24, 27]. The lower limit of quantification (LOQ) was 10 RU/mL, 10 pg/mL, and 4.6 ng/mL respectively for FGF23, PTH, and 25(OH)D3.
In Potsdam plasma creatinine was measured in 2008 at the Department of Internal Medicine, University of Tübingen; in Heidelberg at the Stichting Huisartsen Laboratorium (Breda, The Netherlands). Estimated glomerular filtration rate (eGFR) was calculated with the Cockcroft-Gault equation [28]. Lifestyle characteristics, smoking history, physical activity, and education were documented at baseline by trained interviewers during PC-guided interview [17]. The Cambridge physical activity index was used to categorize participants as inactive (“sedentary job and no recreational activity”), moderately inactive, moderately active, and active (“sedentary job with >1 h recreational activity per day, standing or physical job with some recreational activity, or a heavy manual job”) [29]. Educational attainment was categorized as follows: ‘low’: primary school or no school graduation; ‘medium’: secondary, technical or professional school graduation; ‘high’: longer education including university degree [24]. Prevalent hypertension, hyperlipidemia, and diabetes were self-reported at baseline.
Statistical analysis
Continuous normally distributed variables were reported as mean and 95 % confidence interval (CI); right skewed variables were natural log-transformed and reported as geometric mean and 95 % CI. Categorical variables were presented as percentages.
Age and sex adjusted analysis of covariance was used to compare baseline general characteristics between CVD cases and non-cases.
Analyses were performed with SAS 9.4 (SAS Institute, Cary, NC). Statistical tests were two-sided and P values <0.05 considered statistically significant.
Confounder selection
Directed acyclic graphs (DAG) was implemented to understand the underlying causal structure among the variables and to choose a minimal sufficient adjustment set of covariates [30].
Multiple imputation
A multivariable multiple imputation was used to impute missing values for FGF23, PTH and 25(OH)D3 data below the LOQ and for any of the covariates (see Table 1 for missing values percentages). Since the LOQ was known in advance, data were assumed to be missing at random [31]. Also the other missing data were assumed to be missing at random, and no systematic differences were observed between those with and without missing. SAS PROC MI with the Markov Chain Monte Carlo method for arbitrary missing patterns was used to generate 20 imputed datasets. The logarithmic transformation was taken for all the continuous right skewed variables. All variables (exposure, outcome, and covariates) included in the full Cox regression model were included in the procedure. Logical bounds were set on the variables subject to LOQ only (so that all estimates for measurements below the LOQ must be less than this limit). As these variables are biological markers, for which zero values are not possible in nature, no lower bound was specified while the upper bound was set to the log of the LOQ. For the remaining covariates no boundaries were imposed. SAS PROC MIANALYZE was used to combine the results of the analyses on 20 imputed datasets and to generate valid statistical inferences.
Prospective analysis
Prentice modified cox proportional-hazards regression [19] was used to estimate the associations between FGF23 and total CVD risk, MI, stroke and its subtypes for each imputed data set.
Age was the underlying time axis with “entry time” defined as age at baseline and “exit time” as age at diagnosis of MI or stroke or censoring. The baseline hazard function was allowed to vary by age at recruitment and centre. Possible nonlinear relationships between FGF23 and major CVD endpoints were examined with restricted cubic splines (RCS), with 4 knots at 5th, 35th, 65th, and 95th percentile of FGF23. The likelihood ratio test was used to select the best-fit model. For linear relationships FGF23 was transformed using the base 2 logarithm. The hazard ratios (HR) of the transformed values were interpreted as the increase in CVD endpoints risk corresponding to a doubling of FGF23 values. However, for comparison with other studies, we furthermore calculated the HR for the highest versus the lowest quartiles of FGF23. For nonlinear relationships the HR were calculated for quartiles of FGF23 levels based on the distribution of the subcohort.
Effect modifications were tested with cross-product terms in the fully adjusted multivariable model. The interactions terms centre × FGF23 (continuous), as well as sex × FGF23 (continuous), and major endpoints were not significant.
The proportional hazard assumption was tested for FGF23 with a Kolmogorov-type supremum test. No violation was found.
Sensitivity analyses
Values below the LOQ were substituted with the LOQ divided by the √2, and final statistical inferences compared to those derived with the use of multiple imputation. Lagged analyses were performed by excluding the first 2 years of follow-up to account for the latency period between pathology and clinical diagnosis.
Results
Confounder selection
The minimal sufficient adjustment set between FGF23 and CVD included the following covariates: age, gender, smoking habits, prevalent hypertension, hyperlipidemia and diabetes, dietary phosphorus an calcium intake, PTH, 25-Hydroxyvitamin D3, and eGFR [28] (Fig. 2). A competing DAG was drawn which additionally included BMI as covariate (not shown).
Directed acyclic graph (DAG) for the causal structure of the relationship between FGF23 (exposure) and cardiovascular disease risk (outcome; represented in solid black circles with grey line). This DAG represents two causal pathways between FGF23 and CVD: an indirect effect mediated by the “causal” mediators group: blood pressure and left ventricular hypertrophy (solid white circles with black line; dashed black arrows from FGF23 to mediators and from mediators to CVD) and a direct effect (unmediated by the “causal” mediators; dashed black arrow from FGF23 to CVD). The straight black dashed arrow from FGF23 to CVD shows the effect of interest. Confounders in this relationship are represented in solid grey circles with black line. A confounder is associated with both exposure (FGF23) and outcome (CVD) and provides an unblocked backdoor path [47] between CVD and FGF23. Furthermore, confounders are not on the causal pathway between FGF23 and CVD risk, like the covariates blood pressure and left ventricular hypertrophy grouped as mediators in the figure (solid white circles with black line). If, for example, kidney function is a confounder of the relationship between FGF23 and CVD, then it needs to cause both FGF23 and CVD (as indicated in the figure by the direction of the two arrows from kidney function to FGF23 and from kidney function to CVD). The covariates physical activity, socioeconomic status and adiposity, represented in solid grey circles, are risk factors for CVD however there are no evidence they have an impact on FGF23. Therefore they are not confounders. On the contrary, the covariates grouped as other markers are known to influence FGF23 levels but there is no evidence they have an impact on CVD. Therefore also this latter set of covariates is not part of the identified minimal sufficient adjustment set (i.e. lifestyles, demographics, comorbidities, kidney function, bone mineral metabolism markers)
Baseline general characteristics
Individuals who developed CVD were older and more likely to be male, smokers, less physically active, and less educated and more likely to have a history of hypertension, hyperlipidemia, and diabetes, than individuals free of CVD (Table 1). Furthermore, they had a higher body mass index, and higher levels of FGF23 and eGFR, but lower levels of 25(OH)D3. Table 2 depicts baseline general characteristics and risk factors by quartiles of FGF23 within the subcohort only, after multiple imputation. Individuals with higher FGF23 levels (median in the highest FGF23 quartile: 90.4 RU/mL, interquartile range 78.3–116.7) were more likely to be women and smokers, to have a higher waist circumference, to be less educated, physically active, and to have higher PTH levels. They furthermore have higher intakes of calcium and phosphorus.
Prospective associations
RCS regression showed a significant linear trend between FGF23 levels and incident total CVD. After adjustment for age, sex, and laboratory batch, the HR of total CVD per doubling of FGF23 was 1.22 (95 % CI 1.08–1.38, Table 3, Model 1), without evidence for effect modification by age. This association remained significant after additional adjustment for smoking habits, prevalent hypertension, hyperlipidemia and diabetes, dietary phosphorus and calcium intake, PTH, 25(OH)D3, and eGFR (HR per doubling: 1.16, 95 % CI 1.02–1.32, Table 3, Model 2). In stratified analyses by major endpoints FGF23 was linearly associated with MI in both the basic and the fully adjusted Model 2 (HR per doubling: 1.27, 95 % CI 1.05–1.53, Table 3). Results did not substantially change after further adjustment for BMI, as indicated by the competing DAG (HR per doubling of FGF23: 1.25, 95 % CI 1.03–1.51 for MI).
Concerning incident stroke, no significant association was observed with FGF23 levels after multivariable adjustment (HR for highest vs. lowest quartile: 1.30, 95 % CI 0.95–1.86, Table 3, Model 2). Also, non-significant was the association observed with IS (HR for highest vs. lowest quartile: 1.03, 95 % CI 0.69–1.55, Table 3, Model 2). A significant nonlinear relationship, as confirmed by RCS (P value = 0.02 for the cubic spline polynomial vs. the linear model), was observed between FGF23 levels and HS risk. Only individuals in the top quartile of FGF23 were at increased HS risk (HR for highest vs. lowest quartile: 2.61, 95 % CI 1.23–5.52, Table 3, Model 2). Results remained the same after further adjustment for BMI (HR for highest vs. lowest quartile: 2.60, 95 % CI 1.22–5.53).
No significant interactions were observed between FGF23 levels and eGFR for each endpoint (data not shown). Results did not change in sensitivity analyses described above (data not shown).
Discussion
In the present study, we observed significant positive relationships between higher FGF23 levels and the risk of developing total CVD, MI and HS. These associations were independent of established cardiovascular risk factors, including eGFR as well as PTH and 25(OH)D3. No relevant association was, instead, observed for IS.
To the best of our knowledge, this is the first study showing positive associations between circulating FGF23 and risk of MI. Also, we extend and confirm the recently published findings that higher FGF23 levels are related to increased risk of HS [11], now generalizable also to a Caucasian population.
A few epidemiologic studies have investigated FGF23 in relation to CVD endpoints and suggested an association between higher FGF23 levels and increased risk of HF mainly [5, 7, 9], and stroke [5, 7], but not of MI [5, 7, 9] or CHD [6]. However, no associations were observed between higher FGF23 levels and stroke risk in a nested case–control study of the PEACE trial [9], in the Reasons for Geographic and Racial Differences in Stroke study [32], and in the Atherosclerosis Risk in Communities Study [33]. Only one very recently published study specifically examined FGF23 levels as a risk factor for stroke and its subtypes, and found a significant association between higher FGF23 levels and risk of intracerebral hemorrhage [11]. This interesting finding observed in an US urban population of mostly Hispanic/Latino participants, known to be at increased intracerebral hemorrhage risk, is consistent with our finding on hemorrhagic stroke, now generalizable to other groups. Indeed, this adds further strength to our hypothesis that FGF23 may represent a novel modifiable risk factor for cardiovascular disease.
Nevertheless, with regard to MI, the reasons behind the conflicting findings could be found in the high heterogeneity of these previous studies, when compared to the present one, in terms of health status of individuals included in the analyses, age and sex, types of outcomes investigated, duration of follow-up, exposure modelling, and model adjustment. In fact, of these studies three were in patients with CAD [5, 9, 34], two in elderly people [7, 8], and one in an apparently healthy male population [6]. For instance, in the Heart and Soul Study participants with higher FGF23 levels had an increased risk of CVD (a composite of MI, stroke combined with transient IS attack, and HF) and mortality after adjustment for traditional risk factors, C-reactive protein, and kidney function. However, in stratified analysis, the associations were significant for HF and stroke, but not for acute MI [5]. Although this latter finding is in line with the results of the Health Professionals Follow-up Study—a nested case–control study in which circulating FGF23 was not significantly related to CHD risk [6]—major limitations of these two studies deserve further discussion. In the Heart and Soul study all participants were CAD patients and only 88 of them had MI, thus with a limited power to detect a small association with FGF23 levels as observed in the present study. Furthermore, it is likely that their findings may differ in younger persons and in subjects without CAD, as confirmed in our study population [5]. With regard to the Health Professionals Follow-up Study, the all-male study population may limit the generalizability of their results.
However, the mechanisms linking FGF23 to CVD development remain unclear.
It is possible that FGF23 has a direct cardiac and vascular toxicity [35, 36]. Or that FGF23 exerts its toxicity in part by inhibiting calcitriol synthesis with consequent activation of the renin-angiotensin-aldosterone system [37, 38], in turn implicated in the pathophysiology of hypertension, acute MI, congestive HF, and stroke [39]. It is conceivable too that high FGF23 levels might increase the risk of MI (and stroke) via its mechanism in inducing left ventricular hypertrophy [40–42], although this mechanism warrants additional experimental setting [43, 44]. In agreement, recently, FGF23 has been associated with incident CVD events (composite of hospital-treated MI and stroke, and all-cause mortality) independently of eGFR. Interestingly, these associations were attenuated after adjustment for putative mediators such as left ventricular mass, endothelial function, serum phosphate and calcium, suggesting a direct effect of FGF23 on the heart and vascular wall [8]. Collectively, these findings suggest that FGF23 may play a role in the development of MI by affecting cardiac and vascular functions [45]. Yet, evidence seem to suggest that FGF23 may reflect an important pathophysiological pathway in HF, as shown in vitro and in animal model studies [41], in humans [46], and as observed in our previous study as well [10]. Therefore, the association between FGF23 and MI observed in the present study might be driven by left ventricular hypertrophy and HF. However, we could not test this hypothesis due to the lack of information about echocardiographic findings at baseline.
With regard to stroke our findings of an increased risk of HS, but not of IS, in participants in the top quartile of FGF23 levels are in line with those recently observed in the Northern Manhattan Study [11]. As also claimed by the authors of this previous study, our findings are unexpected. No mechanism, so far, linking FGF23 to HS has been hypothesized, proposed, or studied. Indeed, one of the most common causes of HS is hypertension. Interestingly, in an animal model study FGF23 was shown to regulate renal sodium and blood pressure [12]. In particular, the gain in the FGF23 function of wild type mice treated with recombinant FGF23 led to decreased urinary sodium excretion and urine volume, increased blood pressure and heart-to-body weight ratio thus, independently of αKlotho and dietary sodium, leading to hypertension and heart hypertrophy [12]. However, as also addressed by Wright and colleagues, adjustment for blood pressure, a putative mediator, did not attenuate the association with HS suggesting an independent effect [11].
Strengths of this study include its prospective design, the high follow-up response rate, and the laboratory blinded biomarker measurements. All cases were validated by medical records. Bias due to inappropriate adjustment for potential confounders was reduced by the implementation of causal diagrams; and a multiple imputation approach was employed to handle missing values.
There are, however, several limitations too. Serum calcium and phosphate, as well as blood pressure measures were not available or only partly available in both study cohorts. Yet, these variables were not identified in the DAG. The analyses were based on one single baseline measurement of the biomarker. However, the good reliability of plasma FGF23 levels observed over time suggests that a single measurement may provide reliable relative risk in prospective cohort studies [26]. Finally, important CVD risk factors such as hyperlipidemia, hypertension and diabetes were self-reported. Though it might be argued that residual confounding by these variables is present in our data, we compared the risk estimates for CVD by self-reported prevalent hyperlipidemia, hypertension and diabetes, other than other conventional cardiovascular risk factors (i.e. age, sex, and smoking). Yet, after multivariable and mutual adjustment, self-reported comorbidities data were still positively and significantly related to several fold increased CVD risk, thus indicating that residual confounding by these variables is not likely. Furthermore, even though we adjusted our analyses for self-reported comorbidities, as identified by the DAG, these covariates (i.e. prevalent hypertension, hyperlipidemia, and diabetes) were, however, not associated with our exposure (i.e. FGF23), thus they did not satisfy one of the necessary condition for confounding. Therefore, adjustment for these self-reported data unlikely distorted the magnitude of the relationships between FGF23 and cardiovascular events. In summary, our findings provide epidemiological evidence for potential relationships between FGF23 and risk of developing MI and HS. However, the limited number of HS cases, and the small magnitude of the association observed between FGF23 levels and MI risk, require a cautious interpretation of these findings and indicate the need for further studies. Evidence for a causal role of FGF23 in the pathogenesis of MI and HS could be derived from a Mendelian randomization approach. Indeed, results from clinical trials may shed light on whether FGF23 is a modifiable cardiovascular risk factor.
References
Quarles LD. The bone and beyond: ‘Dem bones’ are made for more than walking. Nat Med. 2011;17(4):428–30. doi:10.1038/nm0411-428.
Hori M, Shimizu Y, Fukumoto S. Minireview: fibroblast growth factor 23 in phosphate homeostasis and bone metabolism. Endocrinology. 2011;152(1):4–10. doi:10.1210/en.2010-0800.
Krajisnik T, Bjorklund P, Marsell R, Ljunggren O, Akerstrom G, Jonsson KB, et al. Fibroblast growth factor-23 regulates parathyroid hormone and 1alpha-hydroxylase expression in cultured bovine parathyroid cells. J Endocrinol. 2007;195(1):125–31.
Kovesdy CP, Quarles LD. Fibroblast growth factor-23: what we know, what we don’t know, and what we need to know. Nephrol Dial Transplant. 2013. doi:10.1093/ndt/gft065.
Parker BD, Schurgers LJ, Brandenburg VM, Christenson RH, Vermeer C, Ketteler M, et al. The associations of fibroblast growth factor 23 and uncarboxylated matrix Gla protein with mortality in coronary artery disease: the heart and soul study. Ann Intern Med. 2010;152(10):640–8. doi:10.1059/0003-4819-152-10-201005180-00004.
Taylor EN, Rimm EB, Stampfer MJ, Curhan GC. Plasma fibroblast growth factor 23, parathyroid hormone, phosphorus, and risk of coronary heart disease. Am Heart J. 2011;161(5):956–62. doi:10.1016/j.ahj.2011.02.012.
Ix JH, Katz R, Kestenbaum BR, de Boer IH, Chonchol M, Mukamal KJ, et al. Fibroblast growth factor-23 and death, heart failure, and cardiovascular events in community-living individuals: CHS (cardiovascular health study). J Am Coll Cardiol. 2012;60(3):200–7. doi:10.1016/j.jacc.2012.03.040.
Arnlov J, Carlsson AC, Sundstrom J, Ingelsson E, Larsson A, Lind L, et al. Serum FGF23 and risk of cardiovascular events in relation to mineral metabolism and cardiovascular pathology. Clin J Am Soc Nephrol CJASN. 2013;8(5):781–6. doi:10.2215/CJN.09570912.
Udell JA, O’Donnell T, Morrow D, Jarolim P, Omland T, Sloan S, et al. Association of fibroblast growth factor (FGF)-23 levels with risk of cardiovascular events in patients with stable coronary artery disease. J Am Coll Cardiol. 2012;59(13):E1480. doi:10.1016/S0735-1097(12)61481-8.
di Giuseppe R, Buijsse B, Hirche F, Wirth J, Arregui M, Westphal S, et al. Plasma fibroblast growth factor 23, parathyroid hormone, 25-HydroxyvitaminD3 and risk of heart failure: a prospective, case-cohort study. J Clin Endocrinol Metab. 2013. doi:10.1210/jc.2013-2963.
Wright CB, Dong C, Stark M, Silverberg S, Rundek T, Elkind MS, et al. Plasma FGF23 and the risk of stroke: the Northern manhattan study (NOMAS). Neurology. 2014. doi:10.1212/WNL.0000000000000410.
Andrukhova O, Slavic S, Smorodchenko A, Zeitz U, Shalhoub V, Lanske B, et al. FGF23 regulates renal sodium handling and blood pressure. EMBO Mol Med. 2014. doi:10.1002/emmm.201303716.
Heine GH, Seiler S, Fliser D. FGF-23: the rise of a novel cardiovascular risk marker in CKD. Nephrology, dialysis, transplantation : official publication of the European dialysis and transplant association—European renal association. 2012;27(8):3072–81. doi:10.1093/ndt/gfs259.
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, et al. European prospective investigation into cancer and nutrition (EPIC): study populations and data collection. Public Health Nutr. 2002;5(6B):1113–24. doi:10.1079/PHN2002394.
Riboli E, Kaaks R. The EPIC project: rationale and study design. European prospective investigation into cancer and nutrition. Int J Epidemiol. 1997;26(Suppl 1):S6–14.
Boeing H, Wahrendorf J, Becker N. EPIC-Germany—a source for studies into diet and risk of chronic diseases. European investigation into cancer and nutrition. Ann Nutr Metab. 1999;43(4):195–204.
Boeing H, Korfmann A, Bergmann MM. Recruitment procedures of EPIC-Germany. European investigation into cancer and nutrition. Ann Nutr Metab. 1999;43(4):205–15.
Bergmann MM, Bussas U, Boeing H. Follow-up procedures in EPIC-Germany—data quality aspects. European prospective investigation into cancer and nutrition. Ann Nutr Metab. 1999;43(4):225–34.
Prentice LR. A case-cohort design for epidemiologic cohort studies and disease prevention trials. Biometrika. 1986;73:1–11.
InterAct C, Langenberg C, Sharp S, Forouhi NG, Franks PW, Schulze MB, et al. Design and cohort description of the interact project: an examination of the interaction of genetic and lifestyle factors on the incidence of type 2 diabetes in the EPIC study. Diabetologia. 2011;54(9):2272–82. doi:10.1007/s00125-011-2182-9.
Weikert C, Stefan N, Schulze MB, Pischon T, Berger K, Joost HG, et al. Plasma fetuin-a levels and the risk of myocardial infarction and ischemic stroke. Circulation. 2008;118(24):2555–62. doi:10.1161/CIRCULATIONAHA.108.814418.
Weikert C, Berger K, Heidemann C, Bergmann MM, Hoffmann K, Klipstein-Grobusch K, et al. Joint effects of risk factors for stroke and transient ischemic attack in a German population: the EPIC potsdam study. J Neurol. 2007;254(3):315–21. doi:10.1007/s00415-006-0358-x.
Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583–612.
Kuhn T, Kaaks R, Teucher B, Hirche F, Dierkes J, Weikert C, et al. Plasma 25-hydroxyvitamin D and its genetic determinants in relation to incident myocardial infarction and stroke in the European prospective investigation into cancer and nutrition (EPIC)-Germany study. PLoS one. 2013;8(7):e69080. doi:10.1371/journal.pone.0069080.
Danesh J, Saracci R, Berglund G, Feskens E, Overvad K, Panico S, et al. EPIC-Heart: the cardiovascular component of a prospective study of nutritional, lifestyle and biological factors in 520,000 middle-aged participants from 10 European countries. Eur J Epidemiol. 2007;22(2):129–41. doi:10.1007/s10654-006-9096-8.
di Giuseppe R, Hirche F, Montonen J, Buijsse B, Dierkes J, Stangl GI, et al. Reliability of plasma fibroblast growth factor 23 as risk biomarker in epidemiological studies measured over a four-month period. Ann Clin Biochem. 2012;49(Pt 6):542–5. doi:10.1258/acb.2012.011273.
Buijsse B, Boeing H, Hirche F, Weikert C, Schulze MB, Gottschald M, et al. Plasma 25-hydroxyvitamin D and its genetic determinants in relation to incident type 2 diabetes: a prospective case-cohort study. Eur J Epidemiol. 2013;28(9):743–52. doi:10.1007/s10654-013-9844-5.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41.
Wareham NJ, Jakes RW, Rennie KL, Schuit J, Mitchell J, Hennings S, et al. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European prospective investigation into cancer and nutrition (EPIC) study. Public health Nutr. 2003;6(4):407–13. doi:10.1079/PHN2002439.
Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22(5):745. doi:10.1097/EDE.0b013e318225c2be.
Hopke PK, Liu C, Rubin DB. Multiple imputation for multivariate data with missing and below-threshold measurements: time-series concentrations of pollutants in the Arctic. Biometrics. 2001;57(1):22–33.
Panwar B, Jenny N, Howard V, Wadley V, Muntner P, Judd S, et al. Abstract T P134: fibroblast growth factor 23 and risk of incident stroke in the regards study. Stroke. 2014;45(Suppl 1):ATP134.
Lutsey PL, Selvin E, Misialek JR, Michos ED, Rebholz CM, Gottesman RF, et al. Abstract P222: serum fibroblast growth factor-23 and risk of incident stroke: the atherosclerosis risk in communities study (ARIC). Circulation. 2014;129(Suppl 1):AP222.
Tuñón J, Cristóbal C, Tarin N, Gonzalez-Parra E, Aceña Á, Gonzalez-Casaus ML, et al. Fibroblast growth factor 23 and low 25 OH Vitamin D plasma levels are independent predictors of cardiovascular events in patients with chronic coronary artery disease. J Am Coll Cardiol. 2013. doi:10.1016/S0735-1097(13)61451-5.
Wolf M. Forging forward with 10 burning questions on FGF23 in kidney disease. J Am Soc Nephrol JASN. 2010;21(9):1427–35. doi:10.1681/ASN.2009121293.
Mirza MA, Larsson A, Lind L, Larsson TE. Circulating fibroblast growth factor-23 is associated with vascular dysfunction in the community. Atherosclerosis. 2009;205(2):385–90.
Zoccali C, Yilmaz MI, Mallamaci F. FGF23: a mature renal and cardiovascular risk factor? Blood Purif. 2013;36(1):52–7. doi:10.1159/000351001.
de Borst MH, Vervloet MG, ter Wee PM, Navis G. Cross talk between the renin-angiotensin-aldosterone system and vitamin D-FGF-23-klotho in chronic kidney disease. J Am Soc Nephrol JASN. 2011;22(9):1603–9. doi:10.1681/ASN.2010121251.
Ma TK, Kam KK, Yan BP, Lam YY. Renin-angiotensin-aldosterone system blockade for cardiovascular diseases: current status. Br J Pharmacol. 2010;160(6):1273–92. doi:10.1111/j.1476-5381.2010.00750.x.
Gutierrez OM, Januzzi JL, Isakova T, Laliberte K, Smith K, Collerone G, et al. Fibroblast growth factor 23 and left ventricular hypertrophy in chronic kidney disease. Circulation. 2009;119(19):2545–52. doi:10.1161/CIRCULATIONAHA.108.844506.
Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, et al. FGF23 induces left ventricular hypertrophy. J Clin Invest. 2011;121(11):4393–408. doi:10.1172/JCI46122.
Mirza MA, Larsson A, Melhus H, Lind L, Larsson TE. Serum intact FGF23 associate with left ventricular mass, hypertrophy and geometry in an elderly population. Atherosclerosis. 2009;207(2):546–51.
Bots ML, Nikitin Y, Salonen JT, Elwood PC, Malyutina S, de Freire Concalves A, et al. Left ventricular hypertrophy and risk of fatal and non-fatal stroke. EUROSTROKE: a collaborative study among research centres in Europe. J Epidemiol Community Health. 2002;56(Suppl 1):i8–13.
Bauml MA, Underwood DA. Left ventricular hypertrophy: an overlooked cardiovascular risk factor. Clevel Clin J Med. 2010;77(6):381–7. doi:10.3949/ccjm.77a.09158.
Schoppet M, Hofbauer LC, Brinskelle-Schmal N, Varennes A, Goudable J, Richard M, et al. Serum level of the phosphaturic factor FGF23 is associated with abdominal aortic calcification in men: the STRAMBO study. J Clin Endocrinol Metab. 2012;97(4):E575–83. doi:10.1210/jc.2011-2836.
Imazu M, Takahama H, Asanuma H, Funada A, Ohara T, Hasegawa T, et al. Clinical significance of serum fibroblast growth factor 23 as a surrogate marker of the cardiorenal hemodynamic state in patients with heart failure. Eur Heart J. 2013;34(suppl 1):P4242.
Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10(1):37–48.
Acknowledgments
We are indebted to Ellen Kohlsdorf (data management), Wolfgang Fleischhauer (case ascertainment), and Wolfgang Bernigau (statistical assistance) in EPIC-Potsdam, and to Marie-Luise Groß (case ascertainment), and Jutta Schmitt (data management) in EPIC-Heidelberg. This work was supported by a grant from the German Heart Research Foundation. Measurements of PTH and 25(OH)D3 in the subcohort were paid by a grant from the Federal Ministry of Education and Research (BMBF FZK0315668).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
Study procedures have been approved by the Ethics Committee of the Medical Association of the State of Brandenburg and by the Ethics Committee of the Heidelberg University Medical School, respectively for Potsdam and Heidelberg, and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants gave their written informed consents priori to their inclusion in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
di Giuseppe, R., Kühn, T., Hirche, F. et al. Plasma fibroblast growth factor 23 and risk of cardiovascular disease: results from the EPIC-Germany case-cohort study. Eur J Epidemiol 30, 131–141 (2015). https://doi.org/10.1007/s10654-014-9982-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-014-9982-4