Abstract
To disclose risk factors of incident aortic stenosis (AS) and progression of established AS. A prospective cohort study. The Tromsø Study, a population based health survey. Over a 14 years span we performed three repeated echocardiographic examinations (1994, 2001 and 2008) of a random sample of initially 3,243 participants. Data from the only hospital serving this population were included in the follow up. Throughout the study 132 participants were diagnosed with incident AS, defined as mean aortic valve gradient ≥15 mmHg. Cox proportional hazards regression disclosed age (HR 1.11, 95 %CI 1.08–1.14), systolic blood pressure (BP) (HR 1.01, 95 % CI 1.00–1.02), active smoking (HR 1.71, 95 % CI 1.09–2.67), and waist circumference (HR 1.02, 95 % CI 1.00–1.03) as independent predictors of incident AS. Analysis of risk factors for progression of AS disclosed a higher mean aortic gradient at first measurement (p = 0.015), weight (p = 0.015), a low haemoglobin (Hgb) (p = 0.030) and high density lipoprotein (HDL) (p = 0.032) as significant independent predictors. Age, systolic BP, smoking and waist circumference were independent predictors of incident AS, whereas cholesterol was not. Mean aortic gradient at first measurement, weight, an elevated HDL and low Hgb increase the progression rate of the disease. Our data indicate that calcific aortic valve disease is a distinct pathophysiological process, with age, smoking and “wear and tear” of the valve being major contributors to the disease development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcific aortic valve disease is a slowly progressive disorder with a disease spectrum ranging from aortic sclerosis, where the valve leaflets have only mild focal thickening, to severe aortic stenosis (AS), with major ventricular outflow obstruction due to impaired leaflet motion [1]. Aortic sclerosis is prevalent in more than 25 % of subjects over 65 years and there is an exponentially increasing prevalence of AS with age [2–5] Severe AS is the primary indication for valve replacement surgery in the western world. AS includes both bileaflet and trileaflet valves as we know that the tissue changes appear to be similar in both valve types [6].
A number of causes of AS have been suggested, and the evidence for any of them is conflicting. The reason for this is probably that many studies are retrospective, cross-sectional and based on clinical, not population-based data [7]. Referral bias may have influenced several studies and the definition of AS has been varying.
Recently we reported longitudinal population based prospective data on prevalence, incidence and progression of AS [5]. These data also gave us an opportunity to study a broad range of risk factors for developing AS in subjects without evidence of the disease at baseline, with the aim of detecting targets for prevention and treatment. We also evaluated their influence on the progression rate of the disease.
Methods
Study population
The Tromsø Study was initiated in 1974 and is an ongoing population-based cohort study in the municipality of Tromsø, a city in Northern Norway with 70,000 inhabitants. The cohort consists of complete birth cohorts and random population samples examined in six surveys from 1974 to 2008, attendance rates being >75 % in the first five surveys and 66 % in 2008 [8].
Echocardiography
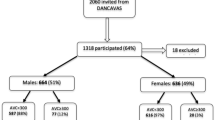
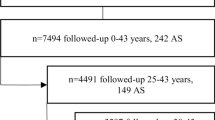
In 1994 information was obtained concerning cardiovascular diseases and risk factors through standardized questionnaires, physical examinations and laboratory tests. Subgroups of the participants were invited to a second visit in 1994 with extended examinations, including echocardiography. They represent a cohort within the cohort and have been the basis for invitations to the two later surveys. All subjects aged 55–74 as well as smaller (5–8 %) random samples of other age groups (25–84 years) were invited, with an attendance rate at the second visit of 76 %. At baseline 30 subjects already had AS and were excluded. The echocardio-graphy subgroup thus consisted of 3,243 subjects (Fig. 1). We defined AS to be present if the transvalvular mean gradient was ≥15 mmHg and graded as follows: mild AS ≥ 15–29 mmHg, moderate AS ≥ 30–49 mmHg, severe AS ≥ 50 mmHg. Aortic regurgitation and left ventricular function were also evaluated. Those with mean gradients ≥15 due to aortic regurgitation alone or subAS were not classified as AS (n = 4 in T5, n = 3 in T6). The same population was invited to follow-up echocardiographic screenings in 2001 and 2008. Data from the only hospital serving this population were included in the follow up. A total of 132 participants were found to have incident AS during the survey. Regarding further details of the echocardiographic examination we refer to our recently published article [5].
A subgroup of 118 of the 132 participants with incident AS had two or more measurements of the mean aortic gradient either in the survey and/or at the hospital. They were thus eligible for evaluation of risk factors for increased progression rate of AS. The subgroup had a mean follow-up time of 6.4 years (range 1–14 years). The mean progression/year was 3.2 mmHg (range −1.0 to 13.0).
Statistics
Univariate analyses of risk factors for AS were performed using Cox proportional hazards regression. In addition we performed age adjusted analyses for each variable. Censoring occurred when participants moved, at death or end of follow up. Being a slowly progressive disease, and with long echocardiographic examination intervals of 7 years, we assumed that those found to be incident cases in 2001 and 2008 had the disease a few years prior to the examination. Thus, the diagnostic time-point for incident cases was estimated to be at 3/4 of the time interval from baseline to 2001/2008. Significance level was set at 0.05.
Independent risk factors for aortic valve stenosis were determined by a backward multivariate analysis using Cox proportional hazards regression. The proportional hazards assumption was assessed by visual inspection of plots, statistical analysis of Schoenfeld residuals and by time-dependant variables for each predictor. A p value from the univariate analyses of <0.25 was used for entry into the multivariate analysis. This included age, systolic blood pressure (BP), waist circumference, coronary disease, smoking, diabetes, osteoprotegerin (OPG), white blood cells, fibrinogen, medication for hypertension, intensive physical activity and moderate physical activity. We excluded weight, hip circumference and body mass index (BMI) due to their high correlation with waist circumference, the latter being the most significant of these factors in the crude analyses. Both systolic and diastolic BP were univariatly significant factors, but multicollinearity excluded diastolic BP. It was the variance proportions on the same eigenvalue that disclosed the multicollinearity between these variables, not the tolerance values or the variance inflation factors (VIF).
The influence on progression rate of AS was calculated in the before mentioned subgroup (n = 118), first in crude regression analyses of risk factors, secondly in a multivariate regression model. A p value of <0.25 was used for entry. The model included haemoglobin (Hgb), high density lipoprotein (HDL) cholesterol, OPG, age, BMI, pulse, osteoporosis, moderate physical activity, intensive physical activity, cod liver oil supplementation and mean aortic gradient at the first echocardiographic evaluation. Weight was excluded due to multicollinearity with BMI. Here also variance proportions on the same eigenvalue disclosed the multicollinearity, not the tolerance values or VIF’s.
The statistical analyses were performed using SPSS, version 18.0.
Ethics
The study was approved by the Regional Ethical committee. All participants gave written consent to scientific use of the health survey data and linkage to health registries. Our study complies with the Declaration of Helsinki.
Results
Of the 3,243 participants, 132 developed incident AS during follow up. Forty-nine of the incident cases were diagnosed at the hospital, in-between the first to second or second to third screening. At the end of the study, AS stage status was: mild AS 64, moderate AS 29, severe AS 19 and aortic valve replacement 20. Only two participants had a bicuspid aortic valve. The number of dead in the total study group was 787, of which 36 had AS.
Descriptions of continuous and categorical risk factors for incident AS are displayed in Table 1. The results of the crude and age adjusted analyses are shown in Table 2. We found that age, systolic and diastolic BP, antihypertensive treatment, OPG, waist circumference, BMI, hip circumference, weight and coronary disease were unadjusted significant predictors. After adjusting for age, only systolic BP, diastolic BP, waist circumference, weight, and hip circumference had a p value <0.05. BMI and active smoking had borderline values <0.055.
The results of the backward multivariate analysis are also shown in Table 2. Age, systolic BP, active smoking and waist circumference were significant independent predictors, with a Wald score of 51.3, 6.03, 5.49 and 5.28, respectively. Active smokers had a HR for AS of 1.7 compared to non-smokers. For each decade increase in age there was a 171 % increase in risk of developing AS, whereas each standard deviation (SD) increase in waist circumference (11.4 cm) gave a 23 % increased risk of AS. Further, each SD increase in systolic BP (22.3 mmHg) gave a 25 % increased risk of incident AS.
In a subanalysis we excluded participants with a mean aortic gradient of 10–15 mmHg (n = 105) in order to remove a “dilution effect” of those assumed to have aortic sclerosis. Accordingly we found a slightly strengthened HR (95 % CI) for two of the significant predictors: active smoking 2.01 (1.23, 3.46) and age 1.12 (1.08, 1.15). Further analysis revealed an interaction between age and waist, showing that waist was a significant risk factor in the younger population only (<65 years in 1994). In this age group (incident cases = 43) we also found that OPG was a significant risk factor (HR 1.30, 95 % CI 1.03–1.65) whereas active smoking was not.
Factors affecting the progression rate was initially evaluated in a crude regression analysis, finding the mean aortic gradient at first measurement (p = 0.01), hip circumference (p = 0.034) and Hgb (p = 0.039) to be predictors (Table 3). Entry of variables into multivariate regression analysis disclosed a higher mean aortic gradient at baseline (p = 0.015), weight (p = 0.015), a low Hgb (p = 0.030), and a high HDL (p = 0.032) as significant independent predictors on the progression rate of AS ( Table 3). Age as a continuos variable was not significant, neither in the crude nor in the multivariate regression analyses.
Discussion
Methods
This is in our opinion the first prospective population based analysis of possible causative factors in truly incident AS. No previous study has included only patients who did not have the disease at baseline. We also studied only risk factors that were present before onset of the disease. This is highly preferable, since it separates potential causes of disease from consequences of it. The inability to perform this separation may easily pollute cross-sectional studies. AS may for instance influence BP, exercise habits, dietary habits and also cause anemia, which may cause spurious associations and obscure true associations.
We have used a strict Doppler-based hemodynamic definition of AS and due to the repeated examinations we know that all cases are true incident cases. The 14 years time span between risk factor sampling and the last follow up gives sufficient exposure time for eventual risk factors to be expressed.
Previous authors of population based studies have addressed similar, but not identical questions and with different methods [3, 9–11]. Three of these studies are cross-sectional and have therefore analysed risk factors sampled at the same time as the condition of the aortic valve was studied [3, 9, 10]. All four studies were image based and have observed aortic sclerosis, defined as small morphological changes of the aortic valve either by CT or 2-D echocardiography. The functional importance of these changes has not been assessed and very few patients with properly defined AS seems to have been included. One study (Stritzke et al.) is prospective, but had an echocardiographic evaluation of the valve only at follow-up and there were only three cases with AS [11].
The low number of bicuspid aortic valves in our study may be explained by a selection bias. A substantial proportion of those with bicuspid valves is hidden within those with aortic valve replacement (n = 4) or established AS at baseline (n = 30). We only included those in 1994 without AS as we wanted to explore risk factors of incident AS.
Risk factors of incident AS
Our results confirm that aging is an important risk factor, with a close to tripled increase in risk for each 10 years. Smoking, systolic BP and waist circumference were also significant factors in the multivariate analyses. Active smoking has been significantly related to AS both in the KORA/MONICA study (OR 1.7) and in the Cardiovascular Health Study (OR 1.35) [3, 11]. Our data (HR 1.7) confirm these earlier studies.
The association with obesity was confirmed by the significant results regarding hip circumference, weight and BMI in the univariate analysis. Systolic BP, diastolic BP and antihypertensive treatment were all significant risk factors in the crude analyses, and both systolic and diastolic BP maintained significance when entered separately into the multivariate model.
In contrast to the image based studies, we found no association between AS and lipids. The links to factors influencing calcification were also very weak. OPG, a protein that inhibits osteoclast activity, was a significant factor only in the crude analysis and in stratified multivariate analysis in subjects under the age of 65, but not in the main multivariate model.
Risk factors of AS progression
The first measured mean aortic gradient was the major predictor of the progression rate. This correlates to our previous study in this population [5], delineating a more rapid progression with advancing valve calcification, also demonstrated in some prior retrospective studies [12–16]. When this was accounted for, age did not appear as an important factor. Weaker findings were associations between progression rate and a lowered Hgb level and, paradoxically, with an elevated HDL level. The finding of a low Hgb as a risk factor is supported by one previous study [17]. Again, other lipids did not appear to be of importance.
The pathophysiolgy of AS
The traditional view has been that AS primarily is an age-associated degenerative condition, aggravated by mechanical stress. The association with age is confirmed both by this and our previous study on the epidemiology of AS [5]. Recently two alternative models have been discussed, seeing AS either as an atherosclerotic process or as linked to factors influencing calcification.
Several clinically based retrospective studies and three of the population based papers quoted above have linked AS to lipids [3, 7, 10, 11]. Combined with the associations with other core cardiovascular risk factors this led to the hypothesis that AS was essentially an atherosclerotic disease. In marked contrast to previous studies we did not find any association between lipids and AS, neither with regard to initiation, nor progression of the disease. This is compatible with the negative results of the three intervention studies on lipid lowering in AS [18–20]. Although several other “atherosclerotic factors” may have a role in the pathogenesis of the disease, conventionally measured lipids do not. A small study indicating that statins still may have a role in mild AS needs support from larger trials and is not supported by our findings of zero effect of lipids in the transition from no disease to early disease [21]. A recent genetic study indicate a causative role of Lp(a), and another study demonstrated a stepwise increase in risk of AS with increasing levels of Lp(a) in a general population [22, 23].
Thus, the atherosclerotic model for AS seems weakened. Although several factors involved in the development of AS are also atherosclerotic factors, the dissociation regarding lipids indicate a different type of process. This is supported by other differences making AS appear as a distinctive pathophysiological entity. Early lesions of AS are characterized by subendothelial accumulation of oxidised LDL and inflammation with T-lymfocytes and macrophages [24]. Smooth muscle cells are prominently involved in atherosclerosis but are not seen in diseased aortic valve lesions, where the fibroblasts and myofibroblasts dominate [1]. In addition, the calcific changes are present at an earlier stage and more prominently in AS than in an atherosclerotic plaque [25]. Only one-half of the patients with AS have coronary artery disease, and a minority of patients with coronary artery disease have concomitant AS [26].
The calcification process in AS seems to be an active process initiated by locally produced factors, transforming fibroblasts into osteoblasts [27]. It is also well known that diseases with altered calcium metabolism, like end-stage renal disease, Paget’s disease and hyperparathyroidism are associated with AS [6]. A polymorphism of the vitamin D receptor is associated with both AS and osteoporosis [28]. In contrast, we did not find any strong associations with calcium metabolism. A recent study used PET and CT imaging in patients with calcific aortic valve disease to compare calcification of the aortic valves with that of thoracic atheromas and skeletal bone [29]. They found that active calcification was most pronounced in aortic valves, whereas inflammation dominated in atheromas. Valve calcifications were poorly related to calcific activity in the aorta, coronary arteries and bone but strongly related to the severity of aortic valve disease. In accordance with our findings, they imply that once valvular calcification has begun, it proceeds largely independently of external factors.
Although an active inflammatory process is involved in the development of AS, none of the i markers in ours study (CRP, white blood cells and fibrinogen) were significant, neither in the crude nor multivariate analyses. A key initiating factor appears to be mechanical stress. Blood-flow dynamics may also contribute, since lesions are located in regions at the aortic side of the valve with low shear stress, thus often affecting the non-coronary cusp first where the shear stress is low due to absence of diastolic coronary flow [25]. Another aspect of importance is the anatomical relations between valve leaflets, corresponding sinuses and sinotubular junction. Normal anatomy in these structures seems to create an optimal distribution of pressure load. Due to aging the aortic root is stiffened by the loss of elasticity, and the aortic leaflet dynamics change. The role of aging is thus not restricted to mechanical stress on the valve alone, but also to the changing dynamics of neighbouring structures, making the process continuous and progressive [25]. When sclerosis is established, the leaflets themselves also promote unfavourable stress distribution, causing a self-perpetuating process.
If age is important it is easy to imagine that all factors increasing the mechanical stress on the valve may enhance the process. This is in accordance with our findings regarding BP and obesity. Thus, an age-dependant process aggravated by “wear and tear” and the toxic effect of smoking may still be the best model of the causes of AS in the general population. The wear and tear theory may also gain support from the experience with bicuspid valves, which develop AS 10–20 years earlier than the tricuspid AS population [30].
The clinical implications of this study are simple. Sticking to a healthy life-style, similar to that advocated to prevent coronary heart disease, may probably reduce your risk of having AS to some extent. However, when the disease has started to develop it constitutes mostly a self-perpetuating process, uninfluenced by external factors.
Strengths and limitations
We believe that the design of the study was well suited and had sufficient power to identify possible causative factors of AS. On the other hand, some of the categorical risk factors, for instance diabetes, had such a low prevalence in our population that the power to detect associations was weakened. The number of subjects with AS is not large, but this is compensated for by the long time span of observations. Risk factors were measured in 1994 only, and changes in these variables over time were not included in the analyses. Therefore, many molecular factors, which has been suggested as causes of AS, could not be studied. The long follow up, with catchment of non-participants in later screenings (2001 and 2008) at the only hospital serving the survey area, strengthens the validity of our findings. As there was a higher prevalence of smoking, obesity and hypertension among those who died before a new screening, those who moved or otherwise did not attend, this could have caused an underestimation of AS incidence and consequently also a bias of the risk estimates associated with these factors.
Conclusions
Our results seem to challenge current thinking on the causes of AS and also gives some credibility to the traditional model of “wear and tear”. Neither lipids nor calcification modifying factors seems to be heavily involved. From our study AS appears to constitute a distinctive age related degenerative and inflammatory disease, which may be aggravated by smoking and a number of factors increasing the mechanical stress on the aortic valve.
References
Freeman RV, Otto CM. Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation. 2005;111(24):3316–26.
Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368(9540):1005–11.
Stewart BF, Siscovick D, Lind BK, et al. Clinical factors associated with calcific aortic valve disease. cardiovascular health study. J Am Coll Cardiol. 1997;29(3):630–4.
Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol. 1993;21(5):1220–5.
Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. The Tromso study. Heart. 2012;. doi:10.1136/heartjnl-2012-302265.
Kurtz CE, Otto CM. Aortic stenosis: clinical aspects of diagnosis and management, with 10 illustrative case reports from a 25-year experience. Medicine. 2010;89(6):349–79. doi:10.1097/MD.0b013e3181fe5648.
Chan KL. Is aortic stenosis a preventable disease? J Am Coll Cardiol. 2003;42(4):593–9.
Jacobsen BK, Eggen AE, Mathiesen EB, Wilsgaard T, Njolstad I. Cohort profile: the Tromso study. Int J Epidemiol. 2011;. doi:10.1093/ije/dyr049.
Ix JH, Shlipak MG, Katz R, et al. Kidney function and aortic valve and mitral annular calcification in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Kidney Dis. 2007;50(3):412–20. doi:10.1053/j.ajkd.2007.05.020.
Katz R, Wong ND, Kronmal R, et al. Features of the metabolic syndrome and diabetes mellitus as predictors of aortic valve calcification in the multi-ethnic study of atherosclerosis. Circulation. 2006;113(17):2113–9.
Stritzke J, Linsel-Nitschke P, Markus MR, et al. Association between degenerative aortic valve disease and long-term exposure to cardiovascular risk factors: results of the longitudinal population-based KORA/MONICA survey. Eur Heart J. 2009;30(16):2044–53. doi:10.1093/eurheartj/ehp287.
Perkovic V, Hunt D, Griffin SV, du Plessis M, Becker GJ. Accelerated progression of calcific aortic stenosis in dialysis patients. Nephron Clin Prac. 2003;94(2):c40–5. doi:10.1159/000071280.
Bahler RC, Desser DR, Finkelhor RS, Brener SJ, Youssefi M. Factors leading to progression of valvular aortic stenosis. Am J Cardiol. 1999;84(9):1044–8.
Palta S, Pai AM, Gill KS, Pai RG. New insights into the progression of aortic stenosis: implications for secondary prevention. Circulation. 2000;101(21):2497–502.
Rosenhek R, Binder T, Porenta G, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000;343(9):611–7. doi:10.1056/nejm200008313430903.
Nassimiha D, Aronow WS, Ahn C, Goldman ME. Association of coronary risk factors with progression of valvular aortic stenosis in older persons. Am J Cardiol. 2001;87(11):1313–4.
Yamamoto K, Yamamoto H, Yoshida K, et al. Prognostic factors for progression of early- and late-stage calcific aortic valve disease in Japanese: the Japanese Aortic Stenosis Study (JASS) Retrospective Analysis. Hypertens Res. 2010;33(3):269–74. doi:10.1038/hr.2009.225.
Rossebo AB, Pedersen TR, Boman K, et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N Engl J Med. 2008;359(13):1343–56.
Cowell SJ, Newby DE, Prescott RJ, et al. A randomized trial of intensive lipid-lowering therapy in calcific aortic stenosis. N Engl J Med. 2005;352(23):2389–97. doi:10.1056/NEJMoa043876.
Rosenhek R, Rader F, Loho N, et al. Statins but not angiotensin-converting enzyme inhibitors delay progression of aortic stenosis. Circulation. 2004;110(10):1291–5. doi:10.1161/01.CIR.0000140723.15274.53.
Antonini-Canterin F, Hirsu M, Popescu BA, et al. Stage-related effect of statin treatment on the progression of aortic valve sclerosis and stenosis. Am J Cardiol. 2008;102(6):738–42. doi:10.1016/j.amjcard.2008.04.056.
Kamstrup PR, Tybjaerg-Hansen A, Nordestgaard BG. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J Am Coll Cardiol. 2014;63(5):470–7. doi:10.1016/j.jacc.2013.09.038.
Thanassoulis G, Campbell CY, Owens DS, et al. Genetic associations with valvular calcification and aortic stenosis. N Engl J Med. 2013;368(6):503–12. doi:10.1056/NEJMoa1109034.
Otto CM, Kuusisto J, Reichenbach DD, Gown AM, O’Brien KD. Characterization of the early lesion of ‘degenerative’ valvular aortic stenosis. Histological and immunohistochemical studies. Circulation. 1994;90(2):844–53.
Hermans H, Herijgers P, Holvoet P, et al. Statins for calcific aortic valve stenosis: into oblivion after SALTIRE and SEAS? An extensive review from bench to bedside. Curre Probl Cardiol. 2010;35(6):284–306. doi:10.1016/j.cpcardiol.2010.02.002.
Otto CM, Burwash IG, Legget ME, et al. Prospective study of asymptomatic valvular aortic stenosis. clinical, echocardiographic, and exercise predictors of outcome. Circulation. 1997;95(9):2262–70.
Yetkin E, Waltenberger J. Molecular and cellular mechanisms of aortic stenosis. Int J Cardiol. 2009;135(1):4–13. doi:10.1016/j.ijcard.2009.03.108.
Ortlepp JR, Hoffmann R, Ohme F, Lauscher J, Bleckmann F, Hanrath P. The vitamin D receptor genotype predisposes to the development of calcific aortic valve stenosis. Heart. 2001;85(6):635–8.
Dweck MR, Khaw HJ, Sng GK, et al. Aortic stenosis, atherosclerosis, and skeletal bone: is there a common link with calcification and inflammation? Eur Heart J. 2013;34(21):1567–74. doi:10.1093/eurheartj/eht034.
Roberts WC, Ko JM. Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation. 2005;111(7):920–5. doi:10.1161/01.cir.0000155623.48408.c5.
Acknowledgments
Tom Wilsgård for statistical support. This study was supported by the Northern Norway Regional Health Authorities (PhD Grant Number SFP-727-08).
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eveborn, G.W., Schirmer, H., Lunde, P. et al. Assessment of risk factors for developing incident aortic stenosis: the Tromsø Study. Eur J Epidemiol 29, 567–575 (2014). https://doi.org/10.1007/s10654-014-9936-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-014-9936-x