Abstract
Presence of cerebral microbleeds indicates underlying vascular brain disease and has been implicated in lobar hemorrhages and dementia. However, it remains unknown whether microbleeds also reflect more systemic vascular burden. We investigated the association of microbleeds with all-cause and cardiovascular related mortality in the general population. We rated the brain magnetic resonance imaging scans of 3979 Rotterdam Scan Study participants to determine presence, number, and location of microbleeds. Cox proportional hazards models, adjusted for age, sex, subcohort, vascular risk factors, and other MRI markers of cerebral vascular disease, were applied to quantify the association of microbleeds with mortality. After a mean follow up of 5.2 (±1.1) years, 172 (4.3 %) people had died. Presence of microbleeds, and particularly deep or infratentorial microbleeds, was significantly associated with an increased risk of all-cause mortality [sex-, age-, subcohort adjusted hazard ratio (HR) 2.27; CI 1.50–3.45], independent of vascular risk factors (HR 1.87; 95 % CI 1.20–2.92). The presence of deep or infratentorial microbleeds strongly associated with the risk of cardiovascular related mortality (HR 4.08; CI 1.78–9.39). Mortality risk increased with increasing number of microbleeds. The presence of microbleeds, particularly multiple microbleeds and those in deep or infratentorial regions, indicates an increased risk of mortality, independent of other MRI markers of cerebral vascular disease. Our data suggest that microbleeds may mark severe underlying vascular pathology associated with poorer survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vascular diseases are worldwide the leading cause of mortality, currently accounting for 30 % of all deaths [1]. With the dramatic surge of vascular risk factors expected in the developing world, the incidence of vascular mortality will only further increase in coming decades [2]. In the brain, vascular disease may manifest itself not only as stroke, but also as cognitive decline and dementia [3], all of which are related to shorter survival [4–7]. Before vascular disease becomes clinically apparent, usually a long pre-clinical phase has passed during which vascular pathology steadily accumulates. A cornerstone of preventive research has been to identify markers that are indicative of such pre-clinical pathology and thus predict poor survival [8]. For vascular disease in the brain, several pre-clinical markers have been identified and include white-matter lesions (WML) and lacunar infarcts, which can both be visualized on magnetic resonance imaging (MRI) [9]. Indeed, previous studies have established that presence of these markers relates to shorter survival [10–12].
In recent years, cerebral microbleeds have emerged as a novel MRI marker of vascular brain disease, and microbleeds are highly prevalent in the general population [13, 14]. In contrast to WML and lacunar infarcts, which reflect ischemic changes in the brain, cerebral microbleeds are thought to be small foci of leakage of blood cells [15]. It remains unknown to what extent microbleeds increase the risk of mortality. Also, it is unclear whether presence of microbleeds only reflects vascular disease in the brain, or whether it actually indicates systemic vascular disease.
Until now, two patient-based studies have investigated the association between microbleeds and mortality. One study in memory clinic patients found that presence of microbleeds was associated with risk of mortality independently of other MRI markers of vascular brain disease [10], whilst another study in patients with increased risk of cardiovascular disease reported that it was primarily the number of microbleeds that was related to mortality [16]. We were particularly interested to see whether we could extent these findings to a large group of presumably asymptomatic individuals, since the prevalence of microbleeds is high in the general population. We therefore investigated the association between presence, number and location of microbleeds with regard to all-cause, and cardiovascular related mortality in the general middle aged and elderly population.
Methods
Study design and participants
The study is embedded in the Rotterdam Study, an ongoing prospective population-based cohort study aimed at assessing the incidence, prevalence and determinants of chronic diseases in the elderly. The initial cohort was extended with participants enrolled at a younger age in subsequent years of the study. Rationale and study design have been described previously [17, 18]. The institutional review board approved the study [17]. From 2005 until 2009, a total of 4,898 participants of the Rotterdam Study were invited to undergo brain MRI in the context of the Rotterdam Scan Study [18]. Participants with prevalent dementia (N = 30), and MRI contra-indications (N = 389) were considered ineligible. Of the eligible participants, 4,082 (91 %) gave written informed consent. After excluding participants with physical inabilities to complete MRI (N = 44), and MR images of low quality due to artifacts (N = 59), ratings of microbleeds were available for 3,979 participants.
Brain MRI, assessment of MRI markers
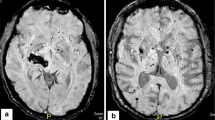
We used a multisequence MRI protocol on the same 1.5-T scanner (GE Healthcare Milwaukee, WI) in all participants [18]. Microbleeds were rated as focal areas of signal loss on 3D T2* GRE-weighted MR imaging (repetition time = 45 ms, echo time = 31, matrix size = 320 × 244, flip angle = 13, field-of-view = 25 × 17.5 cm2, parallel imaging acceleration factor = 2, 96 slices encoded with a slice thickness of 1.6 mm zero padded to 192 slices of 0.8 mm, acquisition time 5 min 55 s) [19]. The presence, number and location of cerebral microbleeds was recorded. Microbleeds were categorized into lobar, deep, and infratentorial, as described previously [14]. The presence of lacunar and cortical infarcts was rated on FLAIR, proton density weighted and T1-weighted sequences [14]. WML and total brain volume were fully automatically segmented and quantified by summation of all voxels of each tissue class across the whole brain [20].
Follow up for mortality
In the Rotterdam Study, information on vital status is obtained from municipal health authorities in Rotterdam on a monthly basis, and from general practitioners in the study area on a continuous basis. For each reported event, information on cause of death is obtained from general practitioners, and by checking medical records. Deaths due to cardiovascular causes were identified using the ‘Rotterdam Study cardiovascular mortality classification’[21]. For all-cause mortality participants were followed from date of entry until date of death, lost to follow up or July 1st 2012, whichever came first. Information on cause specific mortality was available up to January 1st 2011. Accordingly, for cause specific mortality participants were followed from date of entry until date of death, lost to follow up or January 1st 2011, whichever came first.
Assessments of vascular covariates
Potential vascular risk factors were selected based on previous literature published on microbleeds [13, 14]. Research nurses collected data on all participants attending the research center by structured interviews, physical and laboratory examinations [17]. Blood pressure was measured in two readings using a random zero sphygmomanometer in sitting position, and both measures were averaged. Serum total cholesterol and high-density lipoprotein were measured using an automated enzymatic procedure [17]. Smoking behavior was defined as “ever” or “never” smoked. Diabetes was defined as having fasting blood glucose of ≥7.0 mmol/l, and/or the use of any glucose lowering medication. The use of any medication was assessed during home visits by standardised interviews. APOE genotyping was performed on coded genomic DNA samples [22]. Distribution of APOE genotype and allele frequencies in this population were in Hardy–Weinberg equilibrium.
Statistical analysis
Baseline characteristics of the study population, by microbleed status, were investigated cross-sectionally using Student t-tests and Chi square tests to determine differences. WML volume was natural log transformed due to its skewed distribution.
Cox proportional hazards models were fitted to obtain the estimated hazard ratios and 95 % confidence intervals on all-cause, and cardiovascular related mortality associated with the presence of one or more microbleeds. In addition, to determine the presence of a dose response association, we preformed analyses by categories of microbleed count assigning participants as having no (reference category), one, two through four, and five or more microbleeds [23, 24]. Finally, since microbleeds at different locations of the brain are considered to relate to different etiology, we explored the risk of mortality associated with the presence of microbleeds at different locations of the brain (i.e. strictly lobar vs. no microbleeds, and deep or infratentorial microbleeds with or without presence of lobar microbleeds vs. no microbleeds). We constructed four statistical models. In Model 1, we adjusted only for age, sex and Rotterdam Study subcohort. In Model 2, we additionally adjusted for conventional vascular risk factors, namely systolic and diastolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, lipid lowering medication, antihypertensive medication, diabetes, and smoking. These were selected because of their strong association with deep or infratentorial microbleeds. In Model 3, we focused on reported risk factors for lobar microbleeds. Because APOE carriership is strongly related to lobar microbleeds [14] we adjusted this model for APOE genotype. Since APOE genotype affects lipid metabolism we additionally adjusted model 3 for cholesterol levels and lipid lowering medication. Finally, in Model 4 we extended Model 1 by adjustments for other imaging markers of vascular brain disease, specifically brain infarcts, WML and total brain volume [adjusted for intracranial volume (ICV)]. The proportional hazards assumption was tested using Schoenfeld residuals. Kaplan–Meier survival curves were constructed for categories of microbleed count for all-cause mortality. All analyses were conducted using statistical software package SPSS (version 20.0). P values <0.05 were considered statistically significant.
Results
Baseline characteristics of the population are shown in Table 1. Of the 3,979 Rotterdam Scan Study participants, 609 (15.3 %) had one or more cerebral microbleeds at baseline MRI. Of these, 413 (67.8 %) had strictly lobar microbleeds, and 196 (32.2 %) had microbleeds in deep or infratentorial regions. As previously reported [13], higher age, systolic blood pressure, smoking, APOE-e4 carriership, lacunar infarcts and white-matter lesions on MRI, and total brain volume were significantly associated with the presence of cerebral microbleeds. After a mean follow up of 5.2 (±1.1) years, a total of 172 (4.3 %) people had died. Of the 124 participants who died before January 1st 2011, cause of death was known, and 36 (29.0 %) died of cardiovascular causes: 19 participants died of coronary heart disease, 6 due to ischemic stroke, 3 due to hemorrhagic stroke, 2 participants died of unspecified stroke, and 6 of other atherosclerotic or cardiovascular diseases.
Table 2 shows the estimated hazard ratios for presence of cerebral microbleeds in relation to all-cause, cardiovascular, stroke, and non-cardiovascular related mortality after basic adjustments for age, sex, and Rotterdam Study subcohort. After these adjustments, the presence of microbleeds related to a higher risk of all-cause [hazard ratio (HR) 1.56; 95 % CI 1.12–2.17], and cardiovascular related mortality (HR 2.37; 95 % CI 1.19–4.70). When investigating microbleeds with respect to their location in the brain, we found that microbleeds located deep or infratentorial in the brain were strongly associated with all-cause (HR 2.27; 95 % CI 1.50–3.45), cardiovascular (HR 4.08; 95 % CI 1.78–9.39), stroke (HR 5.02; 95 % CI 1.33–18.91), and non-cardiovascular related mortality (HR 1.81; 95 % CI 0.99–3.29), whilst strictly lobar microbleeds were not related to mortality (Table 2). In a post hoc analysis we found that people with strictly deep or infratentorial microbleeds had an increased risk of all-cause mortality compared with people without microbleeds (age, sex, subcohort adjusted HR: 1.84; 95 % CI 0.93–3.64).
Table 3 and Fig. 1 show the association between microbleed count and the risk of mortality. The risk of all-cause mortality increased gradually with larger numbers of microbleeds in the brain (Fig. 1). Participants with five or more cerebral microbleeds, had a 2.8 times (95 % CI 1.65–4.62) higher risk of dying, compared to people without cerebral microbleeds, whereas participants with one cerebral microbleed had a 1.3 times (95 % CI 0.84–2.02) higher risk (Table 3). Testing for linear trends in the hazard of microbleed count per category showed a P value of 0.001. Also, the risk of cardiovascular, and stroke related mortality was higher when the number of microbleeds increased (Table 3).
After adjusting for vascular risk factors the presence of microbleeds, and especially deep or infratentorial microbleeds, associated strongly with all-cause mortality (Table 4, model 2 and 3). Similar results were found after adjustment for infarcts, WML load and brain volume (Table 4, model 4). Particularly the presence of 5 or more microbleeds indicated an increased risk of all-cause mortality after adjusting for vascular risk factors (HR 2.41; 95 % CI 1.37–4.24), and after adjusting for other MRI markers of vascular brain disease (HR 2.01; 95 % CI 1.16–3.48).
Discussion
We found that the presence of deep or infratentorial microbleeds, but not lobar microbleeds, was related to increased risk of all-cause mortality. These associations were strongest with cardiovascular mortality. In people with more than five microbleeds, these associations were independent from vascular risk factors and other MRI markers of vascular brain disease.
Strengths of our study include the population-based setting, which aids generalizability, and the large sample size, facilitating various subgroup analyses. Linkage with data from municipal health authorities ensured virtually complete follow up for mortality. Also, we were able to investigate the association between microbleeds and risk of mortality independent of vascular risk factors and imaging markers due to detailed assessment in the Rotterdam Study. Our scan protocol was optimized to increase conspicuity of microbleeds [19]. Care should be taken that the number of microbleeds detected may differ in various scan settings as it strongly depends on imaging parameters used [19]. We categorized microbleeds as done conventionally into strictly lobar versus deep or infratentorial microbleeds based on their presumable underlying pathology [14]. However, such categorization might suffer from the fact that people with deep or infratentorial microbleeds may have more microbleeds than those with only lobar microbleeds. It is thus possible that the association between deep or infratentorial microbleeds and mortality is driven by numbers of microbleeds rather than location. To address this issue, we performed a post hoc analysis, comparing people with strictly deep or infratentorial microbleeds with people without microbleeds. We found that strictly deep or infratentorial microbleeds still increased the risk of mortality by 84 % (age, sex, subcohort adjusted HR: 1.84; 95 % CI 0.93–3.64). It is noteworthy that the number of cardiovascular deaths (including strokes) in our study group was relatively small. One explanation is that non-participants (e.g. those with MRI contraindications, such as pacemaker, metal implants) have a high likelihood of cardiovascular death. Furthermore, over two-thirds of the cardiovascular deaths (including strokes) occur beyond the age of 75 [25]. In our study group, 92.3 % of the population was younger than 75 years, and thus less likely to die of cardiovascular causes.
We found that presence of microbleeds associates with an increased risk of mortality. These findings are in line with previous studies conducted in a memory clinic population [10], and in a population of people with an increased risk of developing cardiovascular disease (PROSPER study) [16]. We now show that these findings can be extended to people of the general population, emphasizing the role of microbleeds as a preclinical marker of vascular disease in asymptomatic individuals. People with microbleeds were not only more likely to die from vascular brain disease (i.e. strokes) but also from vascular disease outside the brain (i.e., myocardial infarction, heart failure). Previously, it has been suggested that vascular brain disease may to a large extent reflect systemic vascular disease [11, 26–28]. It is therefore viable that microbleeds not only reflect changes in cerebral vessels but may also reflect systemic vascular changes which indicate poorer survival. Further evidence for this notion comes from our observation that especially deep or infratentorial microbleeds drove the associations [16]. Indeed, deep or infratentorial microbleeds are thought to reflect hypertensive arteriopathy [14], which overlaps considerably with systemic vascular disease, whereas lobar microbleeds are more indicative of cerebral amyloid angiopathy, which is primarily restricted to the brain [29]. This might also explain findings from a previous study that showed lobar microbleeds to be associated with stroke-specific mortality [16]. It is likely that these strokes were intracerebral hemorrhages, a major clinical sequel of lobar microbleeds [29]. In our study, the overall number of stroke related mortality was small, precluding robust observations.
The association between deep or infratentorial microbleeds and non-cardiovascular deaths may be explained by deaths due to other neurological causes (i.e. neurodegenerative disease). Another potential explanation may be misclassification of underlying cause of death in people dying from presumably non-vascular causes (70 % of non-cardiovascular deaths was attributed to death from cancer).
We found that the associations between microbleeds and all-cause mortality weakened after adjustment for vascular risk factors. Still, we found that deep or infratentorial microbleeds relate to a higher risk of cardiovascular mortality, even after adjustment for vascular risk factors. This suggests that microbleeds reflect risk factors for vascular brain disease that we did not measure in our study (e.g., genetic factors), or microbleeds may be a more sensitive marker of mortality than these concomitantly measured vascular risk factors. Finally, we showed that multiple microbleeds associate with mortality independent of other MRI markers of vascular brain disease. Therefore, (multiple) microbleeds may be used in addition to other imaging markers such as brain infarcts, WML to identify presence and severity of cerebral vascular disease, and to indicate poorer survival [10–12]. Future studies should indicate whether implementing MRI techniques as a screening method will be cost-effective.
In conclusion, our study shows that in the general population the presence of deep or infratentorial microbleeds is associated with an increased risk of mortality, especially cardiovascular mortality. This implies that microbleeds may be a novel sensitive marker of severe vascular disease and thus an increased risk of death.
Abbreviations
- APOE-e4:
-
Apolipoprotein E4
- CMBs:
-
Cerebral microbleeds
- HDL:
-
High-density lipoprotein
- HR:
-
Hazard ratio
- MRI:
-
Magnetic resonance imaging
- WML:
-
White matter lesions
References
World Health Organization. Cardiovascular diseases. Fact sheet number 317. 2013. Available at: http://www.who.int/mediacentre/factsheets/fs317/en/index.html. Accessed 1 July 2013.
Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112:3547–53.
Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9:689–701.
Barclay LL, Zemcov A, Blass JP, Sansone J. Survival in Alzheimer’s disease and vascular dementias. Neurology. 1985;35:834–40.
Borjesson-Hanson A, Gustafson D, Skoog I. Five-year mortality in relation to dementia and cognitive function in 95-year-olds. Neurology. 2007;69:2069–75.
Feng W, Hendry RM, Adams RJ. Risk of recurrent stroke, myocardial infarction, or death in hospitalized stroke patients. Neurology. 2010;74:588–93.
Melkas S, Putaala J, Oksala NK, Pohjasvaara T, Oksala A, Kaste M, et al. Small-vessel disease relates to poor poststroke survival in a 12-year follow-up. Neurology. 2011;76:734–9.
Wang TJ. Assessing the role of circulating, genetic, and imaging biomarkers in cardiovascular risk prediction. Circulation. 2011;123:551–65.
Patel B, Markus HS. Magnetic resonance imaging in cerebral small vessel disease and its use as a surrogate disease marker. Int J Stroke. 2011;6:47–59.
Henneman WJ, Sluimer JD, Cordonnier C, Baak MM, Scheltens P, Barkhof F, et al. MRI biomarkers of vascular damage and atrophy predicting mortality in a memory clinic population. Stroke. 2009;40:492–8.
Ikram MA, Vrooman HA, Vernooij MW, van der Lijn F, Hofman A, van der Lugt A, et al. Brain tissue volumes in the general elderly population. The Rotterdam Scan Study. Neurobiol Aging. 2008;29:882–90.
Levy RM, Steffens DC, McQuoid DR, Provenzale JM, MacFall JR, Krishnan KR. MRI lesion severity and mortality in geriatric depression. Am J Geriatr Psychiatry. 2003;11:678–82.
Poels MM, Vernooij MW, Ikram MA, Hofman A, Krestin GP, van der Lugt A, et al. Prevalence and risk factors of cerebral microbleeds: an update of the Rotterdam Scan Study. Stroke. 2010;41:S103–6.
Vernooij MW, van der Lugt A, Ikram MA, Wielopolski PA, Niessen WJ, Hofman A, et al. Prevalence and risk factors of cerebral microbleeds: the Rotterdam Scan Study. Neurology. 2008;70:1208–14.
Fazekas F, Kleinert R, Roob G, Kleinert G, Kapeller P, Schmidt R, et al. Histopathologic analysis of foci of signal loss on gradient-echo T2*-weighted MR images in patients with spontaneous intracerebral hemorrhage: evidence of microangiopathy-related microbleeds. AJNR Am J Neuroradiol. 1999;20:637–42.
Altmann-Schneider I, Trompet S, de Craen AJ, van Es AC, Jukema JW, Stott DJ, et al. Cerebral microbleeds are predictive of mortality in the elderly. Stroke. 2011;42:638–44.
Hofman A, van Duijn CM, Franco OH, Ikram MA, Janssen HL, Klaver CC, et al. The Rotterdam study: 2012 objectives and design update. Eur J Epidemiol. 2011;26:657–86.
Ikram MA, van der Lugt A, Niessen WJ, Krestin GP, Koudstaal PJ, Hofman A, et al. The Rotterdam Scan Study: design and update up to 2012. Eur J Epidemiol. 2011;26:811–24.
Vernooij MW, Ikram MA, Wielopolski PA, Krestin GP, Breteler MM, van der Lugt A. Cerebral microbleeds: accelerated 3D T2*-weighted GRE MR imaging versus conventional 2D T2*-weighted GRE MR imaging for detection. Radiology. 2008;248:272–277.
Ikram MA, Vernooij MW, Hofman A, Niessen WJ, van der Lugt A, Breteler MM. Kidney function is related to cerebral small vessel disease. Stroke. 2008;39:55–61.
Leening MJ, Kavousi M, Heeringa J, van Rooij FJ, Verkroost-van Heemst J, Deckers JW, et al. Methods of data collection and definitions of cardiac outcomes in the Rotterdam study. Eur J Epidemiol. 2012;27:173–85.
Wenham PR, Price WH, Blandell G. Apolipoprotein E genotyping by one-stage PCR. Lancet. 1991;337:1158–9.
Biffi A, Halpin A, Towfighi A, Gilson A, Busl K, Rost N, et al. Aspirin and recurrent intracerebral hemorrhage in cerebral amyloid angiopathy. Neurology. 2010;75:693–8.
Soo YO, Yang SR, Lam WW, Wong A, Fan YH, Leung HH, et al. Risk vs benefit of anti-thrombotic therapy in ischaemic stroke patients with cerebral microbleeds. J Neurol. 2008;255:1679–86.
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–220.
Doubal FN, MacGillivray TJ, Patton N, Dhillon B, Dennis MS, Wardlaw JM. Fractal analysis of retinal vessels suggests that a distinct vasculopathy causes lacunar stroke. Neurology. 2010;74:1102–7.
Lanfranconi S, Markus HS. COL4A1 mutations as a monogenic cause of cerebral small vessel disease: a systematic review. Stroke. 2010;41:e513–8.
Thompson CS, Hakim AM. Living beyond our physiological means: small vessel disease of the brain is an expression of a systemic failure in arteriolar function: a unifying hypothesis. Stroke. 2009;40:e322–30.
Viswanathan A, Greenberg SM. Cerebral amyloid angiopathy in the elderly. Ann Neurol. 2011;70:871–80.
Acknowledgments
The Rotterdam Study is funded by Erasmus Medical Center and Erasmus University, Rotterdam; the Research Institute for Diseases in the Elderly; the Ministry of Education, Culture, and Science; the Ministry for Health, Welfare, and Sports; the European Commission (DG XII); and the Municipality of Rotterdam. Dr. Ikram was supported by the Netherlands Heart Foundation (2012T008). The current study is supported by a research fellowship (MWV) from Erasmus MC University Medical Center, Rotterdam, The Netherlands. The funding sources had no influence on study design, collection, analysis, or interpretation of the data or approval of the manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akoudad, S., Ikram, M.A., Koudstaal, P.J. et al. Cerebral microbleeds and the risk of mortality in the general population. Eur J Epidemiol 28, 815–821 (2013). https://doi.org/10.1007/s10654-013-9854-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-013-9854-3