Abstract
Incidence of dementia increases sharply with age and, because of the increase in life expectancy, the number of dementia cases is expected to rise dramatically over time. Some studies suggest that controlling some modifiable risk factors for dementia like diabetes or hypertension could lower its incidence. However, as treating these vascular factors would also reduce mortality risk, the actual impact of such public-health intervention on dementia prevalence is not known. Accounting for the impact of dementia and risk factors on mortality, the aim of this work was (1) to compute projections of age- and-sex specific prevalence of dementia in France from 2010 to 2030, (2) to evaluate how public-health interventions targeting risk factors for dementia could change these projections. Age-and-sex specific incidence of dementia and mortality of demented subjects were estimated from the Paquid population-based cohort using a semi-parametric illness-death model. Future global mortality rates and population sizes were obtained from national demographic projections. Under the assumption that life expectancy will increase by 3.5 years for men and 2.8 years for women by 2030, the number of subjects with dementia was estimated to increase by about 75 % from 2010 to 2030 with a 200 % increase after 90 years of age. Therapeutic intervention on the whole population reducing high blood pressure prevalence would lead to a decrease in both dementia incidence rates and mortality and would have a modest impact on the number of dementia cases. On the other hand, a preventive dementia treatment targeting ApoE4 carriers would probably not improve survival and hence would decrease dementia prevalence by 15–25 %.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia is a frequent disease in the elderly characterized by progressive decline of cognitive abilities leading to loss of autonomy and death. Dementia prevalence rates increase with age, reaching about 38 % in women older than 85 years old in France (24 % for men) [1]. At advanced stages of the disease, patients need important daycare often leading to nursing home placement. As a consequence, with the aging of the world population, the global socio-economic burden of dementia is expected to increase dramatically in the future [2] and it is essential to be able to predict future prevalence to plan the resources needed for patient care. In the last 10 years, accumulated evidence supported the role of modifiable risk factors, such as cardio-vascular risk factors, on the risk of dementia [3]. It was suggested these risk factors could be the target of intervention aiming at reducing the risk of dementia [4]. For public health decisions, it is important to assess how such interventions could change the course of prevalence evolution. In this work, we will use “prevalence” for the number of demented individuals and “prevalence rate” for the proportion.
Projections of age-specific prevalence require knowledge of age-specific incidence rates and of future population sizes and mortality rates for both demented and non-demented individuals. Dementia incidence rates may be estimated from population-based cohort studies while national or worldwide demographic projections may provide population sizes and mortality rates for the general population. Using such data, projections of dementia prevalence have been computed assuming that the mortality rates without disease were equal to the mortality rates of the general population [5–8]. However, this assumption is not tenable since the risk of death is much higher among demented compared to non-demented subjects [9–11] and the prevalence of dementia is very high (especially among the oldest) [12, 13]. As a consequence, the mortality among non-demented subjects is lower than in the general population. In addition, previously published projections were based on restrictive assumptions about mortality of demented subjects. Brookmeyer and colleagues [5, 6] assumed a constant relative risk of death for demented subjects compared to non-demented subjects, independent on both age and calendar time. On the other hand, Mura et al. [8] assumed 3 different relative risks specific to age-groups and Brookmeyer et al. [7] assumed that the death risk increased only for late-stage of the disease (about 6 years after dementia onset).
Brookmeyer et al. [5, 7] evaluated the impact on prevalence projections of a public health intervention that would directly decrease the incidence rates of dementia. More recently, using the population attributable risk, Barnes and Yaffe [4] computed the number of dementia cases that could be prevented by reducing the prevalence of cardio-vascular and lifestyle risk factors. However, none of these estimations accounted for the possible direct impact of the intervention on mortality whereas most of the risk factors for dementia are also risk factors for death. Some authors [7] accounted for the change in mortality due to the change in late-stage dementia prevalence but the mortality among healthy and among early-stage demented was assumed not affected by the intervention. Typically, high blood pressure (HBP) is a well known risk factor for cardio-vascular mortality [14] and an increasing number of studies support its association with higher risk of dementia [15, 16]. Although still controversial [17], this result suggests that a prevention campaign aiming at reducing HBP prevalence could reduce both mortality and dementia incidence. However, the increase in life expectancy due to lowering blood pressure would by itself increase the number of demented individuals and thus the evaluation of the impact of the intervention on dementia prevalence must account for the change in mortality. Another preventive strategy could focus on carriers of the \(\epsilon4\) allele of apolipoprotein E which is recognized as the main genetic risk factor for sporadic late-onset alzheimer’s disease [18, 19] and was found associated with general mortality [20]. A treatment increasing the clearance of the Abeta protein in the brain of Apoe4 subjects could decrease the risk of dementia for these subjects [21, 22].
Using a multi-state approach, the first objective of this paper was to estimate dementia prevalence in France for the next 20 years accounting for the difference between the mortality of the general population and the mortality of non-demented subjects. The second objective was to estimate changes in these prevalence projections assuming various scenarios of public health interventions that aim at reducing the prevalence or the impact of risk factors for dementia.
Method
In this section we describe the principle of the method and all the required assumptions as well as the data used. The detailed statistical method with all mathematical formulas may be found in Joly et al. [23].
Model and assumptions for prevalence projections
The estimation method is based on the 3-state model displayed in Fig. 1 [24] that describes the possible transitions between the three states: healthy (i.e. alive and free of dementia), demented (and alive) and dead. We denote α 01(t, a), α 02(t, a) and α 12(t,a) the transition intensities between the three states with t the calendar year and a the age: α 01(t,a) is the instantaneous risk of dementia (or dementia incidence rate) at year t for healthy subjects of age a; α 02(t,a) and α 12(t,a) are the instantaneous risk of death (or mortality rate) for healthy and demented subjects respectively. For brevity, in the following, we will used “risk” for “instantaneous risk”. The dementia prevalence at time t is the number of subjects in state 1 at time t and the age-specific prevalence is the number of subjects of age a in state 1 at time t.
According to available data and knowledge on the epidemiology of dementia, we used 4 assumptions to compute dementia prevalence.
Assumption 1
The age-specific incidence is null before 65 years:
This assumption was made because dementia incidence is very low before 65 years and there are few reliable data below this age.
Under assumption 1, the computation of the prevalence requires only the size of the population aged 65 years for each calendar year and estimates of the incidence rates of dementia and mortality rates for both non-demented and demented subjects [23]. The population sizes were obtained from national demographic projections. The next two assumptions were used for estimating dementia incidence and mortality rates.
Assumption 2
Without public health intervention, the age-specific risk of dementia does not depend on calendar time t.
Thus, the risk of dementia is a function of age a but does not change with calendar time if no prevention campaign is organized. This assumption, that will be discussed in “Discussion” section, makes possible the estimation of the incidence rates of dementia α 01(a) from cohort data.
Assumption 3
The death risk for demented subjects follows the same time trend as the death risk for healthy subjects with a hazard ratio depending only on age:
Indeed, it is well known that the death risk increases with age and tends to decrease with calendar time in developed countries. The age-specific hazard ratio r(a) may be estimated from cohort data as the ratio \(\hat{\alpha}_{12}(a)/\hat{\alpha}_{02}(a).\) To estimate future values of death risk among healthy and demented subjects, we used national demographic projections for age-specific mortality rates for the total French population. Neglecting the difference between global mortality and mortality of healthy people, some authors have directly used these mortality projections to estimate future prevalence of dementia. Joly et al. [23] have shown that this leads to an underestimation of dementia prevalence and proposed a method to estimate the death risk of healthy people α 02(t,a) from the projections of the global mortality rates and from cohort estimates of dementia incidence rates α 01(a) and hazard ratios of death for demented subjects r(a). Then α 12(t,a) was estimated with formula (3).
Using the above estimates of the three transition intensities α 01(a), α 02(t, a), α 12(t, a) and the sizes of the population reaching age 65 for each calendar year, we computed the prevalence of dementia in the future. To account for uncertainty about estimations of α 01(a) and r(a), 95 % confidence bands for the estimated prevalence were computed by a Monte–Carlo method [23]. Sensitivity to mortality projections for the French population were evaluated by estimating dementia prevalence using three different scenarios about mortality trend (high, central and low life expectancy).
Method for estimating the impact of a prevention campaign
Let us denote z = 0, 1, the binary variable coding for the risk factor that is the target of the intervention.
Assumption 4
The risk factor is not modifiable after age 65.
Thus, subjects exposed (respectively unexposed) at age 65 remained exposed (respectively unexposed) all along the rest of their life. This is equivalent to consider that acquisition or loss of the risk factor later in life has no impact on the dementia risk and mortality. This strong assumption is suitable for many dementia risk factors that are mid-life health conditions (see “Discussion” section).
Assumption 5
The risk factor is associated with the risk of dementia and/or with the risk of death among healthy and demented individuals according to a proportional intensities assumption:
with α 0 hj (t, a) = α hj (t, a|z = 0) the transition intensity from state h to state j (h = 0, 1, j = 1, 2) for unexposed subjects and θ hj the hazard ratios.
The prevalence of the risk factor at age 65, denoted p, as well as the hazard ratios θ hj in the current population were assumed to be known. The risks of dementia and death for the whole population α hj (t, a) were estimated using the method described in “Model and assumptions for prevalence projections” section. The baseline risks α 0 hj (t,a) for unexposed subjects were obtained from α hj (t, a), θ hj and p using least square estimation with cubic spline approximation [23].
We assumed that the intervention began in 2010, was maintained till 2030 and targeted individuals aged 65 years; it could change either the risk factor prevalence p at age 65 or the hazard ratios θ hj . Subjects younger than 65 in 2010 underwent the intervention the year they reached 65 years. Subjects older than 65 in 2010 were not affected by the intervention. Thus, by 2030, the intervention impacted only the dementia prevalence projection for the ages 65–85. Knowing the baseline transition intensities α 001 (a), α 002 (t, a) and α 012 (t, a), the post-intervention transition intensities among the exposed population were obtained by the proportional intensities model (4) using the hypothesized post-intervention hazard ratios θ * hj . Then we computed the projection of disease prevalence for unexposed and exposed subjects and for the general population for any combination of post-intervention values p * and θ * hj .
The Paquid cohort
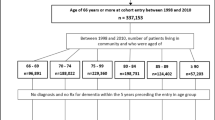
Dementia incidence rates and hazard ratios of death for demented versus non-demented subjects were estimated separately for each gender from the Paquid cohort. It is a prospective study on cognitive ageing including 3,777 subjects aged 65 years and older and living at home at baseline in 1988–1989 in two South–West French departments. The Paquid study has been approved by ethic committees and all participants gave their informed consent prior to their inclusion. Subjects were initially interviewed at home by psychologists trained for home-interview in 1988 and 1, 3, 5, 8, 10, 13, 15, 17 and 20 years later. Dementia diagnosis was assessed at each visit according to the DSM-III-R criteria for dementia using a two-stage procedure: screening by the psychologist and final diagnosis by a senior neurologist following a clinical examination. After excluding subjects demented at baseline, the sample included 3,675 subjects, 58 % were women, 34.8 % had no diploma, 43.7 % had a primary diploma and 21.5 % had higher education. The mean age at entry in the cohort was 75.3 (SE 6.8). During the 20-year follow-up, 832 incident cases of dementia were diagnosed (247 men and 585 women), 639 subjects died after dementia diagnosis (208 men and 431 women) and 2,298 subjects died without diagnosis of dementia (1,103 men and 1,195 women). Exact dates of death were collected for all deaths.
Assuming the three transition intensities depended only on age and sex, the illness-death model (Fig. 1) was estimated for women and men by maximum penalized likelihood accounting for interval censoring of the age at diagnosis of dementia [9]. This method handles the possible unobserved transition to dementia for subjects who died and were not demented at their last visit and avoids parametric assumptions on the transition intensities.
Demographic data
The population sizes of 65-years old men and women at the 1st of January for each year from 1975 to 2030 were obtained from the French National Institute of Statistics INSEE. They were computed from census data till 2006 and projections were performed from 2007 [25]. Similarly INSEE provided projections for age-and-sex-specific mortality rates for the general population from 2007 to 2030 and values before 2007 were computed from the observed number of deaths and the population sizes by sex and age.
The annual mortality rates are approximately equal to the annual death intensities [26]. It was shown that INSEE mortality rates for the general population in the year 2000 fit well the annual death intensities estimated from the whole Paquid sample (1988–2009) [23]. This result supports representativeness of the Paquid sample. As the Paquid estimates of dementia incidence rates and hazard ratios for death were continuous functions of age, we fitted a Gompertz–Makeham model [27] to the INSEE annual mortality rates to obtain a continuous function of age. The Gompertz–Makeham model fitted very well the age trend of mortality.
Results
Prevalence projections for dementia in France from 2010 to 2030
All the estimations and projections were done separately for men and women to account for the differential incidence rates of dementia and mortality rates between genders. Table 1 displays the estimated prevalence in 2010 and 2030 for women, men and both genders according to the three INSEE scenarios about general French mortality projections. The central scenario assumes that mortality trend follows the trend observed in France from 1988 to 2002 (except for women above 85 years and for men above 91 years for whom more optimistic mortality rates were assumed accounting for the improvement observed between 2002 and 2007). For indication, this scenario leads to a life expectancy at birth in 2030 of 87.6 years for women and 81.5 years for men. The low and high life expectancy scenarios respectively correspond to −1.3 and +1.3 years of life expectancy in 2030 for men and women as compared to the central scenario [28].
According to the central scenario for life expectancy, 1,146,000 women (95 % confidence interval: [1,054,000; 1,348,000]) and 604,000 men [525,000; 743,000] between 65 and 99 years old will be demented in France in 2030. Over 20 years (2010–2030), the increase in prevalence is larger for men (+94.8 %) than for women (+67 %). This is the consequence of the larger increase in life expectancy expected for men compared to women (+3.5 years versus +2.8 years over the same 20 year period) according to the current mortality trend. For the entire French population, the estimated number of dementia cases will increase by 75.7 % from 996,000 [897,000; 1,197,000] in 2010 to 1,750,000 [1,409,000; 1,873,000] in 2030. An additional increase in life expectancy of 1.3 years in 2030 (high life expectancy scenario) would increase by about 12 % the number of individuals with dementia. Figure 2 displays the estimated prevalence from 2010 to 2030 for the three mortality scenarios.
In terms of dementia prevalence rates, we found that the proportion of demented subjects among male and female populations should only slightly increase from 2010 to 2030 (Table 2). Knowing that these projections rely on the assumption of constant dementia incidence rates (assumption 2), this increase is entirely explained by the higher life expectancy for demented subjects since mortality of demented subjects was assumed progress following the same time trend as the general mortality.
Figure 3 displays the estimated age-and-sex-specific prevalences (Fig. 3a) and prevalence rates (Fig. 3b) for 2010 and 2030 for the central mortality scenario. The relationship between age and the prevalence rates of dementia is similar in 2010 and 2030 (Fig. 3b). For both 2010 and 2030, the prevalence rates among women continuously increase from age 65 to 99 with a dramatic acceleration from age 80. For men, the prevalence rates increase regularly from age 65 to 95 and then level off around 30 % in 2010 and 36 % in 2030.
Estimated age-and-sex-specific prevalences of dementia (in numbers for each year, a) and prevalence rates (b) for 2010 and 2030 according to the central mortality projection scenario. Estimated prevalence in female population in 2010 (solid line) and in 2030 (dashed line) and in male population in 2010 (dotted line) and in 2030 (dash-dotted line)
Figure 3a highlights both the large increase in the number of dementia cases between 2010 and 2030 at all the ages above 65 and, more importantly, the change in the age-distribution of demented subjects. The irregularities in the age-specific prevalence curves are explained by the deficit in births during the two world wars (1914–1918 and 1939–1945) and the subsequent baby-booms. For both 2010 and 2030, the estimated dementia prevalences are similar for men and women aged less than 78 years, but higher for women than men at older ages. This reflects the higher incidence rates estimated among women after this age in the Paquid cohort [9]. Table 3 summarizes the prevalence estimates by age-groups. The number of demented subjects between 90 and 99 years is expected to increase by 208 % over the 20 year period (from 203,000 cases in 2010 to 626,000 cases in 2030) whereas the number of cases is expected to increase by only 55 % for ages 80–89 and by 72 % below age 79. This is due to the combination of the life expectancy improvement and the small size of the population aged 90–99 in 2010 due to the first world war.
Impact of a prevention intervention
Table 4 presents the baseline estimated prevalence in 2030 for subjects between 65 and 85 years (under the assumptions 1, 2 and 3 of section “Model and assumptions for prevalence projections”) and the modified prevalence projections evaluating the impact of public health interventions according to different scenarios (under the assumptions 4 and 5 of section “Method for estimating the impact of a prevention campaign”)
Scenario 1 mimics an intervention focusing on HBP. The prevalence rate of HBP at 65 years was assumed to be p = 0.40 and the deleterious effect of HBP was stronger for death (θ 12 = θ 02 = 2) than for dementia (θ 01 = 1.5). With these assumptions, an intervention that would reduce HBP prevalence at 65 years by half (the prevalence of the risk factor would become p* = 0.2 from 2010 onwards for people aged 65, scenario 1.a) or that would eradicate HBP at age 65 (p* = 0, scenario 1.b), would lead to almost no change in dementia prevalence 20 years later (−1.4 % with −4 % among women and +2 % among men). With the same initial values for the HBP prevalence p and the associated hazard ratios (θ hj ), an anti-hypertensive drug that would reduce the risk of dementia among hypertensive subjects by 15 % (θ *01 = 1.27), as found in a meta-analysis [29], and the risk of death among hypertensive subjects by 43 % (θ *12 = θ *02 = 1.15) [30] without modifying HBP prevalence, would increase the global prevalence of dementia in 2030 among subjects aged 65–85 by 5.6 % (scenario 1.c). The number of demented cases would increase because, with this scenario, mortality would decrease more than dementia incidence. Whether the risk of death decreased by only 13 % (θ *12 = θ *02 = 1.74) as suggested in a more recent meta-analysis of clinical trials [31], the dementia prevalence would decrease by 2.7 % (scenario 1.d).
Scenario 2 is similar to scenario 1 but the risk factor was not associated with mortality among demented individuals (θ 12 = 1). Thus, reduction in the risk factor frequency would lead to a decrease of dementia prevalence in both women and men (scenario 2.b: −12.4 % among women, −9.2 % among men and −11 % together) because, contrary to scenario 1, the intervention would not change the death risk among demented subjects and thus the duration of the disease would not be lengthened. In scenario 3, the risk factor was more deleterious for dementia and less for death; thus, if it was eradicated (p* = 0, scenario 3.b), the risk of dementia in the population would reduce more than the mortality, leading to a deeper decrease of dementia prevalence (−17.5 %).
Scenarios 4 and 5 corresponds to two extreme situations and are only displayed for comparison. Reducing the prevalence of a risk factor for death which is not associated with dementia would obviously increase the number of demented subjects (scenario 4) while reducing the prevalence of a risk factor for dementia which is not associated with death would obviously decrease dementia prevalence (scenario 5): the reduction would be of −25.3 % if a risk factor with a hazard ratio of 2 and an initial prevalence of 0.4 disappeared (scenario 5.b). Comparison of scenario 5.b and 3.b highlights the need to account for the association of the risk factor with mortality. If the risk factor increased moderately the risk of death (θ 12 = θ 02 = 1.5 in scenario 3.b instead of θ 12 = θ 02 = 1 in scenario 5.b), the decrease in dementia prevalence due to the eradication of the risk factor would be only of 17.5 %.
Scenarios 6 and 7 evaluate the impact of an hypothetical treatment lowering the risk of dementia among APOE4 carriers. In these scenarios, the risk factor prevalence was fixed to 20 % as found for APOE4 carriers in the Paquid cohort [32]. In scenario 6, the hazard ratio for dementia associated with APOE was twice (θ 01 = 3) the hazard ratio for death (θ 02 = θ 12 = 1.5) while, in scenario 7, APOE4 did not impact mortality because results in the literature on this association are inconsistent. As the prevalence of a genetic factor can not be changed, we evaluated the impact of a treatment aiming at reducing the dementia risk among APOE4 carriers. If the hazard ratio was reduced by half (θ *01 = 1.5), the dementia prevalence would decrease by 15 % (scenario 6) or 17 % (scenario 7) and for a perfectly efficient treatment (θ *01 = 1), the dementia prevalence would decrease by 21 % (scenario 6) or 24 % (scenario 7).
Discussion
This study highlights the large impact of the evolution of mortality on the future number of demented subjects. Whatever the scenario regarding mortality trend in France among the three scenarios of INSEE and assuming no change in the incidence rates of dementia, the dementia prevalence will increase by at least 60 % from 2010 to 2030 and the increase could reach 95 % according to the most optimistic scenario for mortality trend. In particular, we will have to face a dramatic rise of the number of very old demented individuals (+200 % over 20 years in the age range 90–99).
We also investigated the impact on future dementia prevalence of various scenarios of intervention targeting risk factors for dementia and/or mortality. Assuming an intervention implemented from 2010 onwards on subjects aged 65 years, by 2030, this would only impact dementia prevalence under age 85. Using sensible hypotheses for the association of HBP with both dementia and death (HBP prevalence at 65 years of 40 % and hazard ratios equal to 1.5 for dementia and 2 for death), the estimated impact of a better care of patients with HBP on dementia prevalence in 2030 for the age range 65–85 was modest: from −2.7 % to +5.6 % according to the efficiency of the intervention. Thus, prevention campaigns against HBP and/or extended use of blood pressure lowering drugs as currently recommended to prevent coronary heart disease and stroke [33] could decrease both mortality and dementia incidence rates but would lead to little change in the number of demented cases by 2030.
Deeper decrease of dementia prevalence was obtained when the intervention targeted a risk factor that was not associated with death in demented subjects (−11 % in scenario 2.b) or more strongly associated with dementia than with death (−17 % in scenario 3.b) or when the intervention reduced only the risk of dementia (scenarios 6 and 7). For example, a perfectly efficient treatment targeting only APOE4 carriers could lead to a 24 % decrease of dementia prevalence. However, this very optimistic scenario is unlikely.
The main strength of this work is the careful handling of mortality for both demented and non-demented subjects and for subjects exposed and unexposed to risk factors. Mainly, these projections of prevalence required no assumption on the association between age and dementia mortality and accounted for the difference between mortality of non-demented subjects and global mortality. We previously showed that neglecting this difference under-estimated the prevalence by about 30 % [23]: 1,203,000 demented subjects in 2030 instead of 1,750,000. Here, we assumed that the mortality rates of demented subjects was higher than the global mortality rates but followed the same time trend. We think it is the most sensible assumption. Assuming alternatively that mortality of demented subjects remained stable with time, the global prevalence in 2030 was estimated as 1,396,000 (20 % lower) and the estimation was less sensitive to the hypothesis about global mortality trend because changing this hypothesis impacted only the at-risk population size and not the duration of the disease [23]. Our prevalence estimates are higher than previous published projections for France [8]. Indeed, the previous projections were based on Eurodem incidence estimates [34] obtained without handling death competing risk and interval censoring while we used the most recent incidences from the French Paquid cohort accounting for these methodological issues. Moreover, mortality of healthy was overestimated in Mura et al. [8] because it was assumed equal to general mortality and because the general mortality projections have been recently updated to account for the mortality decrease in the oldest. Consequently, the main differences between these two estimations regard prevalence among the oldest.
When estimating the impact of a change in the prevalence of risk factors, we accounted for both its direct and indirect (through its association with dementia) effects on mortality. Consequently, the estimated rates of change in the number of cases as compared to the projections without intervention are much less optimistic than the estimations based on the population attributable risk [4]. Indeed the later can be interpreted as a rate of change in prevalence only by assuming that risk factor reduction does not impact mortality and population size.
As explained in the “Method” section, these results rely on several assumptions to be discussed. Assumption 1 that age-specific incidence is null before 65 years has a negligible impact on the prevalence estimation above age 65. Indeed, the incidence before age 65 being very low, we can neglect, at age 65, the differences between the global population size and the population size of non-demented subjects and between the global mortality and the mortality of non-demented subjects. Moreover, including demented subjects before age 65 would not change significantly the global estimated number of demented cases. More importantly, without any intervention, the incidence of the disease is assumed constant with time (assumption 2). The main reason for this assumption is that the time trend for dementia incidence is unknown. Estimations of the time trend have been based on cohort studies with long follow-up and on comparison of cohorts. However, such comparisons are blurred by differential sample selection, by dropout rates during the follow-up and by changes in diagnosis criteria. Current results are inconclusive. Previous analyses from the Paquid cohort suggested both an increase of dementia incidence and a decrease of mortality rates of demented subjects that could be better explained by a shift towards earlier diagnosis rather than a true decrease of incidence [26]. On the other hand, Schrijvers et al. [35] found a non-significant decrease in dementia incidence from 1990 to 2005 and Rocca et al. [36] reported no trend in two population-based samples but a decline between 1985 and 1994 in dementia incidence estimated from a medical record-linkage system without standardized diagnosis. Of note, the main hypothesis suggested to explain a possible decrease in dementia incidence is a better care of cardio-vascular factors. If this declining trend was confirmed, future dementia prevalence could be lower than our projections. In future work, we will extend the method to account for this possible decreasing trend. Finally, according to assumption 3, the estimations were based on a Markov model where mortality of demented depended on age and calendar time but not on the duration of the disease. Previous analyses on the Paquid cohort supported this assumption since a non-homogeneous Markov model was found slightly better than the homogeneous semi-markov model where the risk of death depended on the dementia duration [37].
Representativeness of the Paquid cohort used for estimating dementia incidence and hazard ratio for death may also have consequences on our projections. Paquid was designed to be representative of two departments from South–West France and we found that the global mortality in Paquid fitted very well the French mortality [23]. Moreover, the estimation procedure for the Illness-death model accounted for competing mortality and interval censoring of dementia. Nevertheless, the estimates of dementia incidence and mortality risk for demented subjects suffer from a large uncertainty for the youngest and the oldest subjects due to small sample sizes or/and small number of events in these age ranges. This uncertainty is accounted for in the confidence intervals displayed in Table 1.
For evaluating the consequences of a public health intervention targeting a risk factor, we assumed that the risk factor was not modifiable after age 65 or that a later change in the risk factor did not change dementia and death risks. This strong assumption is supported by many observational studies suggesting that only mid-life HBP (40–65 years), and more generally mid-life cardio-vascular risk factors [3, 16], are associated with a higher risk of dementia while late-life HBP was found unassociated or protective (probably due to selection process or reverse causality) [17]. Moreover, dementia being a chronic disease with a very long and progressive pathological process [38] it is unlikely that late changes in risk factors have a great impact on dementia risk. The intervention was assumed to target individuals aged exactly 65 years old. In fact, the important assumption was that the intervention did not impact mortality rates before age 65. For instance our results are valid for an intervention targeting subjects aged 45–65 if it leaded to negligible change in mortality before age 65. This is a sensible assumption for HBP. Nevertheless, for other risk factors, it will be useful to extend the method to relax this assumption.
In conclusion, we provided updated projections of prevalence of dementia by 2030 according to several scenarios for mortality. In all cases, without change in the incidence rates, a large increase of the prevalence is expected (probably around 75 %) due to aging of the population and improvement in life expectancy. In particular, the prevalence among the oldest could be multiplied by three. A better care of HBP that would impact both mortality and dementia incidence rates would have a modest impact on dementia prevalence in 2030. We focused on hypertension because it is a frequent risk factor found associated with both dementia and mortality and for which effective treatments and prevention strategies are available. On the other hand, ApoE4 is a non-modifiable risk factors but a treatment targeting these subjects was recently envisaged [21, 22]. An efficient treatment of ApoE4 carrier would not change mortality and thus would reduce the number of dementia cases by 15–25 %. Up to now, few data are available to propose detailed scenarios of public-health intervention for dementia. Especially, intervention studies are needed to measure efficiency of treatment of HBP for reducing dementia incidence. Nevertheless, these results help to anticipate change in dementia prevalence according to different hypotheses and the method may be used to evaluate other scenarios.
References
Gallez C. Rapport sur la maladie d alzheimer et les maladies apparentées. Office Parlementaire d’Évaluation des Politiques de Santé, Bibliothèque des Rapports Publics. http://www.assembleenationale.fr/12/rap-off/i2454.asp (2005).
Alzheimer-Association. Alzheimer’s disease facts and figures. Alzheimers Dement. 2012;8:131–168.
Polidori MC, Pientka L, Mecocci P. A review of the major vascular risk factors related to alzheimer’s disease. J Alzheimers Dis. 2012;32:521–530.
Barnes DE, Yaffe K. The projected effect of risk factor reduction on alzheimer’s disease prevalence. Lancet Neurol. 2011;10(9):819–828.
Brookmeyer R, Gray S, Kawas C. Projections of alzheimer’s disease in the united states and the public health impact of delaying disease onset. Am J Public Health 1998;88(9):1337–1342.
Brookmeyer R, Gray S. Methods for projecting the incidence and prevalence of chronic diseases in ageing populations: application to alzheimer’s disease. Stat Med. 2000;19(11–12):1481–1493.
Brookmeyer R, Johnson E, Ziegler-Graham K, Arrighi HM. Forecasting the global burden of alzheimer’s disease. Alzheimers Dement. 2007;3(3):186–191.
Mura T, Dartigues JF, Berr C. How many dementia cases in france and europe? Alternative projections and scenarios 2010–2050. Eur J Neurol. 2010;17(2):252–259.
Joly P, Commenges D, Helmer C, Letenneur L. A penalized likelihood approach for an illness-death model with interval-censored data: application to age-specific incidence of dementia. Biostatistics 2002;3(3):433–443.
Ostbye T, Hill G, Steenhuis R. Mortality in elderly Canadians with and without dementia: a 5-year follow-up. Neurology 1999;53(3):521–526.
Jagger C, Andersen K, Breteler MM, Copeland JR, Helmer C, Baldereschi M, et al. Prognosis with dementia in Europe: a collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology 2000;54(11 supp l5):S16–S20.
Ramaroson H, Helmer C, Barberger-Gateau P, Letenneur L, Dartigues JF. Prevalence of dementia and Alzheimer’s disease among subjects aged 75 years or over: updated results of the PAQUID cohort. Rev Neurol. 2003;159(4):405–411.
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, et al. Global prevalence of dementia: a delphi consensus study. Lancet 2006;366(9503):2112–2117.
WHO. World health report 2002. Reducing risks, promoting healthy life. Geneva: WHO, 2002. World Health Organization, Geneva, Switzerland, http://www.who.int/whr/2002 (2002).
Duron E, Hanon O. Hypertension, cognitive decline and dementia. Arch Cardiovasc Dis. 2008;101(3):181–189.
Tolppanen AM, Solomon A, Soininen H, Kivipelto M. Midlife vascular risk factors and alzheimer’s disease: evidence from epidemiological studies. J Alzheimers Dis. 2012;32:531–540.
Power MC, Weuve J, Gagne JJ, McQueen MB, Viswanathan A, Blacker D. The association between blood pressure and incident alzheimer disease: a systematic review and meta-analysis. Epidemiology 2011;22(5):646–659.
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R, et al. Effects of age, sex, and ethnicity on the association between apolipoprotein e genotype and alzheimer disease. JAMA 1997;278(16):1349–1356.
Genin E, Hannequin D, Wallon D, Sleegers K, Hiltunen M, Combarros O, et al. Apoe and alzheimer disease: a major gene with semi-dominant inheritance. Mol Psychiatry 2011;16(9):903–907.
Tilvis RS, Kähönen-Väre MH, Jolkkonen J, Valvanne J, Pitkala KH, Strandberg TE. Predictors of cognitive decline and mortality of aged people over a 10-year period. J Gerontol A Biol Sci Med Sci. 2004;59(3):M268–M274.
Cramer PE, Cirrito JR, Wesson DW, Lee CY, Karlo JC, Zinn AE, et al. Apoe-directed therapeutics rapidly clear {beta}-amyloid and reverse deficits in ad mouse models. Science 2012;335(6075):1503–1506.
Strittmatter WJ. Old drug, new hope for alzheimers disease. Science 2012;335(6075):1447–1448.
Joly P, Touraine C, Georget A, Dartigues JF, Commenges D, Jacqmin-Gadda H. Prevalence projections of chronic diseases and impact of public health intervention. Biometrics 2013;69:109–117.
Keiding N. Age-specific incidence and prevalence: a statistical perspective. J R Stat Soc Series A 1991;154(3):371–412.
Blanpain N, Chardon O. Projections de population 2007–2060 pour la france métropolitaine: méthode et principaux résultats. Document de travail 2010;F1008. http://alexandre.cor-retraites.fr/IMG/pdf/doc-1446.pdf.
Commenges D, Joly P, Letenneur L, Dartigues JF. Incidence and mortality of Alzheimer’s disease or dementia using an illness-death model. Stat Med. 2004;23:199–210.
Gompertz Benjamin. On the nature of the function expressive of the law of human mortality, and on a new mode of determining the value of life contingencies. Philos Trans R Soc Lond. 1825;115:513–583.
Blanpain N, Chardon O. Projections de population à l’horizon 2060. un tiers de la population âgé de plus de 60 ans. Insee première 2010;1320:1–4.
Peters R, Beckett N, Forette F, Tuomilehto J, Clarke R, Ritchie C, et al. Incident dementia and blood pressure lowering in the hypertension in the very elderly trial cognitive function assessment (hyvet-cog): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7(8):683–689.
Dahlöf B, Hansson L, Lindholm LH, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the swedish trial in old patients with hypertension (stop-hypertension). Lancet 1991;338(8778):1281–1285.
Staessen JA, Gasowski J, Wang JG, Thijs L, Den Hond E, Boissel JP, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 2000;355(9207):865–872.
Winnock M, Letenneur L, Jacqmin-Gadda H, Dallongeville J, Amouyel P, Dartigues JF. Longitudinal analysis of the effect of apolipoprotein e ε 4 and education on cognitive performance in elderly subjects: the paquid study. J Neurol Neurosurg Psychiatry 2002;72(6):794–797.
Law MR, Morris JK, Wald NJ, et al. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338(191):1245–1253.
Fratiglioni L, Launer LJ, Andersen K, Breteler MM, Copeland JR, Dartigues JF, et al. Incidence of dementia and major subtypes in europe: a collaborative study of population-based cohorts. neurologic diseases in the elderly research group. Neurology 2000;54(11 Suppl 5): S10.
Schrijvers EMC, Verhaaren BFJ, Koudstaal PJ, Hofman A, Ikram MA, Breteler MMB. Is dementia incidence declining? Trends in dementia incidence since 1990 in the rotterdam study. Neurology 2012;78(19):1456–1463.
Rocca WA, Petersen RC, Knopman DS, Hebert LE, Evans DA, Hall KS, et al. Trends in the incidence and prevalence of alzheimers disease, dementia, and cognitive impairment in the united states. Alzheimers Dement. 2011;7(1):80–93.
Commenges D, Joly P, Gégout-Petit A, Liquet B. Choice between semi-parametric estimators of markov and non-markov multi-state models from coarsened observations. Scand J Stat. 2006;34(1):33–52.
Amieva H, Le Goff M, Millet X, Orgogozo JM, Pérès K, Barberger-Gateau P, et al. Prodromal alzheimer’s disease: successive emergence of the clinical symptoms. Ann Neurol. 2008;64(5):492–498.
Acknowledgments
PAQUID is partly funded by IPSEN and Novartis Laboratories.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacqmin-Gadda, H., Alperovitch, A., Montlahuc, C. et al. 20-Year prevalence projections for dementia and impact of preventive policy about risk factors. Eur J Epidemiol 28, 493–502 (2013). https://doi.org/10.1007/s10654-013-9818-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-013-9818-7