Abstract
Declining trends in case fatality (CF) of MI events have been generally reported in western countries. It is, however, not clear whether the development has been equally beneficial in both sexes. Data from two large population based registers, FINAMI and the Finnish National Cardiovascular Disease Register (CVDR) were used to determine whether the CF of incident MI events has declined less in women than in men. All patients aged 35 and over were included. CF was calculated for different time periods after the onset of the MI event, the main emphasis was in pre-hospital, 28-day, and 1-year CF. Figures were compared between two study periods: 1994–1996 and 2000–2002. A total of 6,342 incident MI events were recorded in FINAMI and 117,632 events in CVDR during the study periods. Comparison between the two study periods showed that the CF was generally declining. However, a slower decline in short-term CF was seen among young (aged < 55 years) women (P for sex by study period interaction in pre-hospital CF = 0.028 in FINAMI and 0.003 in CVDR, and for 28-day CF P = 0.016 in FINAMI and <0.0001 in CVDR). In conclusion, the short and long-term prognosis of MI events has improved in both sexes. Pre-hospital CF has declined less among younger women than among men and among older women. This slower decline in early CF was responsible for the slower improvement in 28-day and 1-year prognosis in young women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Age-standardised coronary heart disease (CHD) mortality rates have steadily declined during the past decades in western countries. One-third of total CHD mortality decline is due to an increase in survival after myocardial infarction (MI) [1]. Sex differences in CHD mortality have been widely studied during the past two decades, and many of the previous studies have shown higher short-term case fatality (CF) among women [2–4]. In some studies the poorer prognosis among women was shown to be explained by higher age, clinical presentation, higher prevalence of co-morbidities, greater problems in diagnosis and lesser use of reperfusion therapies [2–9]. However, in several studies the sex difference in short-term CF has been apparent even after these factors were adjusted for [11, 12]. Most of these studies have analyzed hospitalized patients only [4–12]. This may distort sex differences, since more men than women are known to die in out-of-hospital circumstances [13]. Population-based studies evaluating total short-term CF taking pre-hospital deaths into account, have reported higher pre-hospital CF for men, higher in-hospital CF for women and no sex differences in overall short-term CF [2, 13–16]. Moreover, younger women (≤55 years) have been shown to have higher in-hospital CF compared to men and older women [3, 17]. This age and sex related difference in MI prognosis has been shown to exist even after adjustments for co-morbidities [18].
Studies on sex differences in the long-term survival after MI have also shown conflicting results. Some have reported higher long-term mortality after incident MI in women [19], while others have shown better or similar long-term prognosis after MI among women [9, 10, 16].
Since CHD mortality rates have declined slower among young women also in Finland [20], we wanted to investigate further whether the slower decrease in mortality is due to less favourable case fatality trends in this patient group. We used data from two large population-based MI registers in Finland to investigate whether the sex difference in CF exists in different time intervals after the onset of the first MI. The main emphasis was in pre-hospital CF, 28-day CF and 1-year CF after the onset of the symptoms. To assess the development over time, the CF proportions among men and women were compared between two time-periods: 1994–1996 and the 2000–2002.
Methods
Data were extracted from two large population-based MI registers, the FINAMI register and the Finnish National Cardiovascular Disease Register (CVDR). The FINAMI register aims to record all suspected MI events and CHD deaths among the permanent residents in four separate geographical regions: (1) the town of Joensuu and certain rural areas in the former province of North Karelia, (2) the town of Kuopio in Eastern Finland, (3) the town of Oulu in Northwestern Finland, and (4) the town of Turku in Southwestern Finland. The average size of the population aged ≥35 years in the FINAMI regions was ~313,000 during the study period. Local registration teams, comprising a trained nurse supervised by a physician, collected data on all coronary events suspected to be MI from hospital admission diagnoses, hospital documents, death certificates and autopsy reports. The data are annually cross-checked with nation-wide Causes-of-Death and Hospital Discharge Registers for completeness. These country-wide administrative registers cover all deaths and hospitalizations among the Finnish residents. International Classification of Diseases (ICD) 9 codes 410–414 and 798 (except 7980A), and ICD-10 codes, (used since 1996 in Finland) I20–I25, R96, R98, I46.1 and I46.9 were used for cross-checking [21].
The CVDR has been compiled using data from the nation-wide Hospital Discharge Register and Causes of Death Register. All hospitalizations due to CHD with the ICD codes listed above as the main or additional diagnoses were included. All deaths having the above mentioned ICD codes as the underlying or immediate cause of death and also deaths where MI was a contributing cause of death (IDC-10: I21–I22/ICD-9:410) were included. The data on deaths and hospitalizations from the period 1991–2007 have been linked using the unique Finnish social security ID codes to form the CVDR. Further details are available in the Internet (http:\\www.ktl.fi/cvdr/). Because the CVDR covers the whole country, most of the cases in the FINAMI register are also included in the CVDR. The overlap between these registers is, however, relatively small, approximately 5% in men and 5–6% in women.
The FINAMI register and CVDR have both been approved by the Ethical Committee of the National Institute for Health and Welfare.
Case definitions
In the FINAMI register, events were classified based on biomarker findings, symptoms, ECG and possible autopsy results, as suggested in the AHA Scientific Statement of 2003 [22]. MI events and CHD deaths with the classes ‘definite’, ‘probable’ and ‘possible’ were all included as cases. In FINAMI, a case was considered as incident if the local registration team did not find any evidence for a prior clinically symptomatic MI event from the hospital records. In CVDR, an event was incident if there were no events in the Hospital Discharge Register for the person in question during the preceding 7 years. In both registers, the most severe diagnosis during the period of 28 days was used. The 28-day period for one event was defined following the practice of the WHO MONICA Project (1) so that the day of onset was taken as day 0 and the last day was day 27.
CF was defined as the proportion of cases that ended up fatally within a specified period of time. Pre-hospital CF was defined as the proportion of cases that did not reach a coronary care unit or a hospital ward alive, i.e., they died in out-of-hospital circumstances or in the emergency room. In terms of calendar time, the survival was <1 day after the onset of symptoms. The 28-day CF was defined as the proportion of deaths that occurred between the onset of the symptoms (=0-day) and the end of the 27th day after the event. The CF during days 2–27, i.e., after the prehospital phase, reflects mainly in-hospital deaths. The 1-year CF was defined as the proportion of MI events that ended up fatally at any time between the onset of the event and the end of the 364th day after the event. CFs for the time periods 2–364 and 28–364 days after the event were defined using similar logic as described above.
In the FINAMI register, autopsies were performed in pre-hospital deaths for 64.9% of men and 33.9% of women in the first period and for 73.4% of men and 43.3% of women in the second period. In CVDR, the respective numbers were 36.7% of men and 16.4% of women in the first period and 42.7% of men and 17.9% of women in the second period.
Statistical methods
The CFs were expressed as a percentage (the number of deceased cases divided by the number of all incident cases, multiplied by 100). Age-standardization was done with the direct method using weights based on the combined age distribution of cases in the MI and stroke registers of the WHO MONICA Project. Weights for each 5-year age groups were: 5, 9, 16, 26, 42, 56, 75, 93, 100, 100, 100, beginning from the age group 35–39 years and ending to the age group 85+ years.
The CF proportions were compared between the two time periods, 1994–1996 and 2000–2002, except for Oulu for which the earlier time period was 1993 and 1997 and the latter time period 2000–2002.
Pre-hospital CF was analyzed using logistic regression. For the 28-day CF we considered Cox proportional hazards regression models, but scaled Schoenfeld residuals (cox.zph, survival-package) and a score process based test (scoreproptest, proptest-package) in the statistical software package ‘R’ suggested that the proportional hazards assumptions were not met. Therefore, logistic regression was also used for analyzing the 28-day CF. For 28–364 day CF global and effectwise proportional hazards assumptions were met and the analyses were carried out using Cox proportional hazard models. In both logistic regression and Cox proportional hazards regression we used the study period (later vs. earlier time period), sex (as baseline difference women vs. men) and history of diabetes mellitus, including an interaction with sex (coded as men = 0, women = 1) as explanatory variables. Sex-specific age effects were linear with 5-year age groups, and had significant sex-specific changing points (interaction) at the age ≥55 years. For the main study question, the interaction of sex with the study period was examined separately for younger (age <55) and older (age ≥55 years) patients.
In Cox proportional hazard regression models entry was day 28 after the onset of the event and the non-fatal events were censored at day 364. Mortality due to other causes was taken as a censoring event. We considered P < 0.05 to be statistically significant.
Statistical analyses were done using the SAS software, version 9 (SAS Institute Inc, Cary; NC; USA), and R version 2.9.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
A total of 2,846 incident MI events (1,451 in men and 1,395 in women) were recorded in the FINAMI register during the first study period and 3,496 (1,775 in men and 1,721 in women) during the latter period. Corresponding numbers in the CVDR were 57,593 events (31,432 in men and 26,161 in women) and 60,039 events (31,936 in men and 28,103 in women). Numbers of fatal events by sex, age group and time after the onset of the event are shown together with other descriptive data in Table 1.
Pre-hospital case-fatality of incident MI events
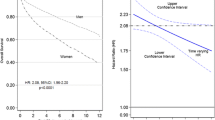
The age-standardized pre-hospital CF of incident MI events among men consistently declined between the study periods in all age-groups: in FINAMI from 29.7 to 26.7% and in CVDR from 33.6 to 29.5%. In women, the trends in pre-hospital CF, were not entirely consistent between the two registers: in FINAMI from 24.1 to 25.6% and in CVDR from 27.0 to 24.4%. When divided by the age group, the CF among the older women (>55 years) did not change in FINAMI (from 24.4 to 25.5%) but declined in CVDR (from 27.1 to 24.3%) (Fig. 1). In younger women (< 55 years), however, the pre-hospital case-fatality increased in FINAMI from 9.4 to 29.6% and no change was observed in CVDR (from 25.7 to 25.2%) (Fig. 1). Among young men the decline was from 27.4 to 27.0% in FINAMI and from 30.8 to 29.2% in CVDR. In older men, a decline was evident in both registers, from 30.1 to 26.6% in FINAMI and from 34.0 to 29.6% in CVDR (Fig. 1). Logistic regression analyses (Table 2) showed that the decline was slower among young women than among men and older women: in the FINAMI register (P for study period by sex interaction = 0.028 for young women) and in CVDR (P = 0.003, respectively), whereas the decline was similar among older women compared to men.
28-day case fatality of incident MI events
The age-standardized 28-day CF was generally lower among young women than among men and older women. Including all age groups, the 28-day CF declined in men from 46.5 to 41.0% in the FINAMI register and from 54.7 to 50.1% in CVDR. Corresponding numbers in women were from 53.5 to 48.6% in FINAMI and from 58.9 to 54.6% in CVDR. In the older age group i.e. >55 years the decline among men was from 48.8 to 43.5% in FINAMI and from 57.6 to 52.6% in CVDR (Fig. 1). A similar decline was seen in older women from 54.4 to 49.1% in FINAMI and from 59.6 to 55.2% in CVDR (Fig. 1). However, in the age group <55 years the declines differed between the sexes. Among men the decline was from 34.1 to 29.2% in FINAMI and from 36.1 to 33.7% in CVDR. Among women, a modest decline from 32.7 to 31.2% was observed in CVDR and even an increasing trend was seen in FINAMI register from 15.6 to 31.5%. The change was significantly different among young women than among men and older women, P = <0.0001 in CVDR and 0.016 in the FINAMI register (Table 3).
We further analysed sex differences in CF during the hospitalization (from the 2nd day after admission to the end of the 27th day). Logistic regression analyses showed no differences between sexes (P for female sex by study period interaction in the age group <55 years = 0.639 in FINAMI and 0.434 in CVDR, and correspondingly in older women P = 0.241 in FINAMI and 0.557 in CVDR) indicating equal decline in in-hospital mortality for both sexes in both studied age groups.
The 1-year case fatality
Similar declines were seen in 1-year (0–364 day) CF in both sexes and registers, in the FINAMI register from 49.5 to 45.1% among men and from 59.4 to 54.4% among women. Corresponding numbers in CVDR were from 59.2 to 55.1% among men and from 65.7 to 61.8% among women. However, when subdivided by age group, increasing CF trend was seen among young women in the FINAMI register, from 18.8 to 31.5%, and no change was seen in CVDR, from 33.8 to 32.2% (Fig. 1). In the group of <55 year old men the decline was from 35.9 to 30.2% in FINAMI and from 37.5 to 34.8% in CVDR.
On the other hand, among older women the decline was slightly steeper when compared to men in both age groups. Decline was from 60.3 to 55.1% in the FINAMI register for older women and from 66.6 to 62.6% in CVDR (Fig. 1). The corresponding change among older men was from 52.0 to 48.5% in FINAMI and from 62.7 to 58.1%in CVDR.
The 28–364 day case fatality of incident MI events
The 28–364 day CF was further analyzed with Cox regression models (Table 4), which showed no significant sex difference in the younger age group compared to the other groups: HR 0.84 (0.39–1.81), P = 0.659 for female sex by study period interaction in patients <55 years old in CVDR. In FINAMI this could not be tested, because there were no deaths among young women in the latter study period in this time interval.
Discussion
Our study showed that the short-term CF and 1-year prognosis of incident MI have improved in both sexes from the mid 1990s to 2002 in Finland. However, the decline in pre-hospital CF was slower among young women compared to men and older women. This higher CF during the critical early hours of the event was reflected also in the 28-day CF after the incident MI. During the period 2–364 days after the onset of the event the decline was similar in both sexes in both age groups. In our earlier paper [20] we showed that the incidence and mortality of first MI events were declining slower in young women than in men and in older women. The present study continues and extends this earlier work by showing that the early CF of MI has developed less favourably in young women. Thus, both incidence and CF seem to have contributed to the less favourable mortality trend in young women.
Pre-hospital case fatality
Higher short-term CF in women compared to men has been reported from hospital-based surveys [4–12], whereas in epidemiological studies sex differences have not been so easily interpretable. Previous studies have shown that more men than women die in pre-hospital conditions [23]. In our study, the pre-hospital CF was also higher in men compared to women in both registers. Two large population-based studies from New Zealand and Scotland examining short-term CF differences between sexes found, similarly to our study, higher pre-hospital CF among men and no sex difference in 28 or 30 day CF [14, 15]. Sex differences in trends in out of hospital CF have also been shown previously. Capewell et al. [24] showed smaller declination in out-of-hospital mortality among women in the Scottish population during the 1986–1995. A more recent report from the ARIC study, having data until 2004, showed a smaller decline in sudden cardiac deaths among women than among men [25]. Some studies have reported even an increasing trend in sudden cardiac deaths among young women [26]. These are important findings since changes in out of hospital deaths are known to comprise over half of overall CHD mortality decline in women [27].
An interesting question is whether this unfavourable change in pre-hospital CF among young women is due to differences in pathophysiology and clinical presentation during the acute phase or insufficiency of primary preventive actions among the women. In epidemiological studies, pre-hospital mortality due to first cardiac events is often used as an indicator for efficiency of primary prevention. Women are often considered to have atypical symptoms, and limited awareness of cardiac disease, which may lead to time-delay in seeking help. In most interventional studies women have been reported to have a longer delay in reaching the hospital after symptom onset than men [28]. Also, due to either atypical symptoms or even lack of any symptoms before the fatal event, women may not have seeked medical help to obtain preventive medications before the fatal event. It has been shown that symptoms before the fatal event are absent more often in women than in men, even though most of the women who die suddenly, have at least one elevated CHD risk factor [29]. This probably explains in part why in our study diabetes was associated with a lower risk of pre-hospital CF, although for longer-term prognosis it was clearly deleterious. Diabetic patients are probably treated for and aware of their high CHD risk and thus may have a shorter delay in contacting the health care system in case of chest pain symptoms. Some previous studies have concluded that diabetes, though more prevalent among women, does not explain the higher short-term CF in women [17, 30]. An opposite conclusion was, however, recently reported from a Swedish population-based study [3].
Smoking may in part explain the slower decline in prehospital case fatality among young women. In Finland, smoking has been increasing among young women until recently [31]. An autopsy study of patients who had died suddenly from cardiac causes showed a 2.0-fold risk for sudden cardiac death in smokers [32]. Pathology studies have shown that young women with sudden cardiac death were more likely to be smokers and have a plaque erosion leading to coronary thrombosis [33]. One of the possible mechanisms is coronary spasm, which are found particularly in smoking women [34]. Smoking, regarded as the strongest risk factor for MI in young individuals, causes epicardial vasocontriction, affects adversely endothelial function and enhances the thrombus formation [35, 36].
Anatomical and pathophysiological sex differences may also explain this tendency towards higher pre-hospital CF among younger women. Women have smaller coronary artery size, which makes them more prone to occlude, and a thinner vessel wall, which is more inclined to dissect [37]. Myocardial ischemia is known to activate autonomic nervous control, which has age related sex differences. In young women the parasympathetic control is the main regulator of cardiovascular system and sympathetic tone is known to dominate after the menopause [38]. It has been speculated that the increased vagal reflexes among young women protect them from ventricular fibrillation but on the other hand an extreme vagal activation is known to lead to asystole and hemodynamic instability [39].
2–27 day case fatality
In our study, 2–27 day CF was similar in both sexes. Most of the percutaneous coronary intervention (PCI) and revascularization procedures are conducted during these days. Some previous studies, using data from 1995 and earlier, before and in the beginning of the present state-of-the-art coronary procedures, have shown higher in-hospital CF for women [14, 15]. Recent reports have shown more encouraging results. Jneid et al. [6] reported an equal in-hospital CF between the sexes after age and co-morbidity adjustments. However, CF remained higher among women with ST-elevation myocardial infarction (STEMI). They also reported lower use of cardiac catheterization and revascularization procedures after MI among women [6]. Opposite results were reported by Zimmermann et al. [28] studying 566 STEMI patients undergoing PCI during 1999–2006. They reported the same frequency of PCI therapy among women as among men and, despite of the higher co-morbidity and higher age among women, the 30-day mortality was similar. In line with these reports, a recent epidemiological study showed improvements in women’s in-hospital CF from 1994 to 2006, showing largest improvement among younger women [40].
Long-term prognosis
Sex differences in long-term prognosis have not been as evident as in the short-term CF. Goldberg et al. found even better long-term prognosis among women, while others concluded no sex differences in long-term survival [9, 10, 17]. However, these studies did not evaluate age related sex differences separately. Schreiner et al. [41] showed a higher amount of fatal recurrent events among men than among women of similar age during a 5 year follow-up of 28-day survivors after an incident MI. Vaccarino et al. [19] showed higher 2-year mortality among women aged <60 years, using data collected from hospital survivors and a similar conclusion was reported for 1-year mortality among women aged <50 years in Sweden [3]. Furthermore, a cross-sectional study comprising 4,347 consecutive patients hospitalized in France showed recently that higher one year mortality was explained by the higher risk of younger women to die during the first days of hospitalization [30]. Taken together, these findings together with our results are alarming indications of the higher risk of fatal outcome in acute MI among young women warranting more attention to primary prevention and acute treatment in young women’s MI.
Strengths and limitations
Two population-based registers, which have complementary approaches, were used in our study. CVDR records all coronary events in the country, whereas FINAMI is based on detailed review of all clinical information according to a standardized protocol. For the main part, these two registers gave consistent results. The registers enabled the inclusion of pre-hospital deaths, which is necessary for unbiased assessment of sex differences in CF. A limitation was the lack of data on the use of different medications and investigations, except revascularizations and thrombolysis in FINAMI. Also, our information on risk factors and comorbidities other than diabetes were limited. FINAMI study population was collected in four mainly urban regions, where the event rates are lower than in the rural areas. However, although FINAMI may not represent Finland as a whole, CVDR covers the whole country.
Conclusion
Pre-hospital, 28-day and 1-year case-fatality declined in both sexes in Finland. The pre-hospital CF has declined more slowly among young (<55 years old) women compared to men and older women. This slower decline in early CF after an incident MI was responsible also for the slower decline in 28-day and 1-year CF among young women. Further studies are warranted to find out the reasons for this less favourable development in young women.
Abbreviations
- CF:
-
Case fatality
- CHD:
-
Coronary heart disease
- MI:
-
Myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- STEMI:
-
ST-elevation myocardial infarction
References
Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E, Amoyuel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Lancet. 1999;353:1547–57.
Lundberg V, Wikström B, Boström S, Asplund K. Exploring sex differences in case fatality in acute myocardial infarction or coronary death events in the northern Sweden monica project. J Intern Med. 2002;251:235–44.
Rosengren A, Spetz C-L, Köster M, Hammar N, Alfredsson L, Rosen M. Sex differences in survival after myocardial infarction in Sweden. Eur Heart J. 2001;22:314–22.
Gan SC, Beaver SK, Houck PM, MacLehose RF, Lawson HW, Chan L. Treatment of acute myocardial infarction and 30-day mortality among women and men. N Engl J Med. 2000;343:8–15.
Jiang SL, Ji PX, Zhao YX, et al. Predictors of in-hospital mortality difference between male and female patients with acute myocardial infarction. Am J Cardiol. 2006;98:1000–3.
Jneid H, Fonarow GC, Cannon CP, et al. Sex differences in medical care and early death after acute myocardial infarction. Circulation. 2008;18:2803–10.
Berger JS, Elliot L, Gallup D, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–82.
Koek HL, Bruin A, Gast F, et al. Short-and long-term prognosis after acute myocardial infarction in men versus women. Am J Cardiol. 2006;98:993–9.
Nicolau JC, Ferraz MA, Nogueira PR, Garzon SAC, Serrano CV, Ramires JAF. The role of sex in long-term prognosis of patients with myocardial infarction submitted to fibrinolytic treatment. Ann Epidemiol. 2004;14:17–23.
Gottlieb S, Harpaz D, Shotan A, et al. Sex differences in management and outcome after acute myocardial infarction in the 1990s. Circulation. 2000;102:2484–90.
Weaver WD, White HD, Aylward PE, et al. Comparisons of characteristics and outcomes among women and men with acute myocardial infarction treated with thrombolytic therapy. GUSTO-I investigators. JAMA. 1996;275:777–82.
Milcent C, Dormont B, Durand-Zaleski I, Steg PG. Sex differences in hospital mortality and use of percutaneous coronary intervention in acute myocardial infarction. Circulation. 2007;115:833–9.
Tunsdall-Pedoe H, Morrison C, Woodward M, Fitzpatrick B, Watt G. Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985 to 1991. Circulation. 1996;93:1981–92.
Sonke GS, Beaglehole R, Stewart AW, Jackson R, Stewart FM. Sex differences in case fatality before and after admission to hospital after acute cardiac events: analysis of community based coronary heart disease register. BMJ. 1996;313:853–5.
MacIntyre K, Stewart S, Capewell S, et al. Sex and survival: a population-based study of 201, 114 men and women following a first myocardial infarction. J Am Coll Cardiol. 2001;38:729–35.
Goldberg RJ, Gorak EJ, Yarzebski J, et al. A community-wide perspective of sex differences and temporal trends in the incidence and survival rates after acute myocardial infarction and out-of-hospital deaths caused by coronary heart disease. Circulation. 1993;87:1947–53.
Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National registry of myocardial infarction 2 participants. N Engl J Med. 1999;341:217–25.
Andrikopoulos GK, Tzeis SE, Pipilis AG, et al. Younger age potentiates post myocardial infarction survival disadvantage of women. Int J Cardiol. 2006;108:320–5.
Vaccarino V, Krumholz HM, Yarzebki J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Inter Med. 2001;134:173–81.
Lehto H-R, Lehto S, Havulinna AS, et al. Are coronary event rates declining slower in women than in men-evidence from two population-based myocardial infarction registers in Finland. BMC Cardiovasc Disord. 2007;7:35.
Salomaa V, Ketonen M, Koukkunen H, et al. Trends in coronary events in Finland during 1983–1997; The FINAMI study. Eur Heart J. 2003;24:311–9.
Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from AHA council on epidemiology and prevention; AHA Statitics committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108:2543–9.
Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90:583–612.
Capewell S, MacIntyre K, Stewart S, et al. Age, sex and social trends in out-hospital cardiac deaths in Scotland 1986–95: a retrospective cohort study. Lancet. 2001;358:1213–7.
Ni H, Coady S, Rosamund W, et al. Trends from 1987 to 2004 in sudden death due to coronary heart disease: the atherosclerosis risk in communities (ARIC) study. Am Heart J. 2009;157:46–52.
Zheng ZJ, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63.
Salomaa V, Ketonen M, Koukkunen H, et al. Decline in out-hospital coronary heart disease deaths has contributed the main part to the overall decline in coronary heart disease mortality rates among persons 35 to 64 years of age in Finland. Circulation. 2003;108:691–6.
Zimmermann S, Ruthrof S, Nowak K, et al. Short-term prognosis of contemporary interventional therapy of ST-elevation myocardial infarction: does sex matter? Clin Res Cardiol. 2009;98:709–15.
Albert CM, Chae CU, Grodstein F, et al. Prospective study of sudden cardiac death among women in United States. Circulation. 2003;107:2096–101.
Tabassome S, Mary-Krause M, Cambou JP, et al. Impact of age and sex on in-hospital and late mortality after acute myocardial infarction: increased early risk in younger women. Eur Heart J. 2006;27:1282–8.
Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Männistö S, Sundvall J, Jousilahti P, Salomaa V, Valsta L, Puska P. Thirty-five-year trends in cardiovascular risk factors in Finland. Int J Epidemiol. 2010;39:504–18.
Kaikkonen KS, Kortelainen ML, Huikuri HV. Comparison of risk profiles between survivors and victims of sudden cardiac death from an acute coronary event. Ann Med. 2009;41:120–7.
Burke AP, Farb A, Malcom GT, Liang Y, Smialek J, Virmani R. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation. 1998;2(97):2110–6.
Caralis DG, Deligonul U, Kern MJ, Cohen JD. Smoking is a risk factor for coronary spasm in young women. Circulation. 1992;85:905–9.
Lavi S, Prasad A, Yang EH, et al. Smoking is associated with epicardial coronary endothelial dysfunction and elevated white blood cell count in patients with chest pain and early coronary artery disease. Circulation. 2007;115:2621–7.
Hung J, Lam JY, Lacoste L, Letchacovski G. Cigarette smoking acutely increases platelet thrombus formation in patients with coronary artery disease taking aspirin. Circulation. 1995;92:2432–6.
Yang F, Minutello RM, Bhagan S, Sharma A, Wong SC. The impact of sex on vessel size in patients with angiographically normal coronary arteries. J Interv Cardiol. 2006;19:340–4.
Lavi S, Nevo O, Thaler I, et al. Effect of aging on the cardiovascular regulatory systems in healthy women. Am J Physiol Regul Intergr Comp Physiol. 2007;292:788–93.
Airaksinen KEJ, Ikäheimo MJ, Linnaluoto MK, Tahvanainen KUO, Huikuri HV. Sex difference in autonomic and hemodynamic reactions to abrupt coronary occlusion. J Am Coll Cardiol. 1998;31:301–6.
Vaccarino V, Parsons L, Peterson ED, Rogers WJ, Kiefe CI, Canto J. Sex differences in mortality after acute myocardial infarction. Arch Intern Med. 2009;169:1767–74.
Schreiner PJ, Niemelä M, Miettinen H, et al. Sex differences in recurrent coronary events. Eur Heart J. 2001;22:762–8.
Acknowledgments
Supported by grants from the Finnish Foundation for Cardiovascular Research to HRL and VS. We have no relationships with industry relevant to the present study.
Conflict of Interest
None to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is conducted by FINAMI Study Group.
All investigators of the FINAMI Study Group are listed in the Appendix.
Appendix: Investigators of the FINAMI Study Group
Appendix: Investigators of the FINAMI Study Group
Kuopio University Hospital: Heli Koukkunen, Seppo Lehto, Heikki Miettinen, Kalevi Pyörälä
North Karelia Central Hospital: Matti Ketonen, Juha Mustonen
Oulu University Hospital and Biocenter Oulu:Tapani Jerkkola, Y. Antero Kesäniemi
Oulu City Hospital: Päivi Kärjä-Koskenkari
Turku University Hospital: Pirjo Immonen-Räihä, Juhani Airaksinen, Tapio Vuorenmaa
Turku Town Hospital: Aapo Lehtonen
THL-National Institute for Health and Welfare: Veikko Salomaa, Kari Kuulasmaa, Aki S. Havulinna, Jorma Torppa, Anne Juolevi, Jaakko Tuomilehto
Rights and permissions
About this article
Cite this article
Lehto, HR., Lehto, S., Havulinna, A.S. et al. Sex differences in short- and long-term case-fatality of myocardial infarction. Eur J Epidemiol 26, 851–861 (2011). https://doi.org/10.1007/s10654-011-9601-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9601-6