Abstract
The diagnostic utility of detecting K-ras mutations for the diagnosis of exocrine pancreatic cancer (EPC) has not been properly studied, and few reports have analysed a clinically relevant spectrum of patients. The objective was to evaluate the clinical validity of detecting K-ras mutations in the diagnosis of EPC in a large sample of clinically relevant patients. We prospectively identified 374 patients in whom one of the following diagnoses was suspected at hospital admission: EPC, chronic pancreatitis, pancreatic cysts, and cancer of the extrahepatic biliary system. Mutations in the K-ras oncogene were analysed by PCR and artificial RFLP in 212 patients. The sensitivity and specificity of the K-ras mutational status for the diagnosis of EPC were 77.7% (95% CI: 69.2–84.8) and 78.0% (68.1–86.0), respectively. The diagnostic accuracy was hardly modified by sex and age. In patients with either mutated K-ras or CEA > 5 ng/ml, the sensitivity and specificity were 81.0% (72.9–87.6) and 62.6% (72.9–87.6), respectively. In patients with mutated K-ras and CEA > 5 ng/ml the sensitivity was markedly reduced. In comparisons with a variety of non-EPC patient groups sensitivity and specificity were both always greater than 75%. In this clinically relevant sample of patients the sensitivity and specificity of K-ras mutations were not sufficiently high for independent diagnostic use. However, it seems premature to rule out the utility of K-ras analysis in conjunction with other genetic and ‘omics’ technologies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The diagnosis of exocrine pancreatic cancer (EPC) remains a difficult challenge in clinical care. Early symptoms and laboratory findings are usually non-specific [1–4], and few tumour markers are widely accepted for routine use [2, 3, 5]. When pancreatic cancer is clinically suspected, imaging techniques offer good diagnostic efficiency. Computed tomography (CT), the most sensitive procedure, non-invasively identifies approximately 90% of cases [6]. However, since CT has less than perfect specificity (approximately 54%), cytological confirmation of radiology findings is usually required. The only curative treatment for EPC is surgical resection, but it is feasible in as few as 20% of cases [1, 2], and is not without problems [7–11]. More rapid and accurate methods to diagnose EPC are hence vital to identify patients who would benefit from surgical resection.
Activating point mutations at codon 12 of the K-ras gene are the most frequent oncogene alteration in EPC; at diagnosis they are detected in 75–90% of patients with EPC [12, 13]. Therefore, it has long been argued that detecting K-ras mutations could be clinically useful in the differential diagnosis of EPC and related disorders [14]. In blood or stools of pancreatic patients K-ras mutations are detected at a much lower frequency than in tumour tissue [14–16]; thus, detection in such samples has not been proven effective in EPC diagnosis. Similarly, detecting mutated K-ras in pancreatic juice or bile has limited diagnostic usefulness [17]. By contrast, K-ras analysis can feasibly be performed in cytohistological specimens, which are often obtained through pancreatic duct brushing, fine needle aspiration, percutaneous biopsy or at surgery. Whether detecting K-ras mutations in these specimens has diagnostic utility is not established, with few reports of sufficient methodological quality, and conflicting results [14]: studies recommend detecting mutated K-ras for diagnosis of EPC as an independent test [18, 19], as an adjunct to cytology [20, 21], only in certain situations such as atypical cytology [22, 23], or not at all [7, 24, 25].
The diagnostic validity of a potential test should be evaluated in relevant populations [26–30]. It is particularly important that the ultimate stage of validation be carried out in a population as close as possible to that in which the test would be used in practice. Therefore, reports demonstrating the utility of K-ras mutations for distinguishing between patients diagnosed with pancreatic cancer and a group of controls (either healthy or with a distinct diagnosis) do not reflect the relevant clinical practice, where the test would be used to detect EPC among symptomatic patients with apparently related and competing diagnoses. Furthermore, to allow for biological variation, it is important to assess the test in a large number patients. None of the above mentioned studies on K-ras and EPC meets these requirements: most studies had a limited patient spectrum, reduced study size, or inadequate description of inclusion criteria.
The aim of this study was to evaluate the clinical validity of detecting K-ras mutations in the diagnosis of EPC in a sample of clinically relevant patients.
Patients and methods
Selection of patients
Detailed methods of the PANKRAS II study have been previously described [4, 31–43]. Briefly, subject recruitment took place between 1992 and 1995 at five general hospitals in the eastern Mediterranean part of Spain. Aided by the study research physicians, trained monitors prospectively identified hospital patients in whom one of the following diagnoses was suspected at admission: cancer of the exocrine pancreas, chronic pancreatitis, pancreatic cysts and pseudocysts (including those secondary to acute pancreatitis), and cancer of the extrahepatic biliary system [32, 33]. The broad eligibility criteria are due to the main objective of the PANKRAS II study: to assess the clinical usefulness of detecting mutations in the K-ras for the diagnosis of cancers of the exocrine pancreas and the extrahepatic biliary system. A total of 602 subjects were selected. The ethics committees of the participating hospitals approved the study protocol, and all patients gave consent to be included in the study.
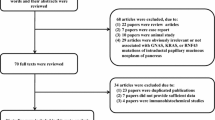
The present report is based on patients in whom a diagnosis of EPC was suspected at hospital intake, or who were definitively diagnosed with EPC during the study. Furthermore, the analysis is limited to individuals for whom cytological or histological material was available for K-ras analysis and in whom mutational status was determined (Fig. 1). Table 1 presents the socio-demographic and clinical characteristics of the study population and compares the final study population with the individuals who met the inclusion criteria but in whom K-ras mutational status was not established [44].
Flow of participants through the recruitment process. 1 At least one of the following diagnoses was suspected at hospital admission: exocrine pancreatic cancer (EPC), chronic pancreatitis, pancreatic cysts and pseudocysts, cancer of the extra-hepatic biliary system. 2 Percentage calculated with respect to the box immediately above (e.g., 37.9% = 228/602 * 100). 3 43 (37.1%) cases were definitively diagnosed as EPC. 4 21 (45.7%) cases were definitively diagnosed as EPC
Data collection
A structured form was used to collect clinico-pathological information from medical records, including details on presenting symptoms, past medical history, the physical examination at admission, ancillary diagnostic procedures, laboratory results and follow-up care [32, 33, 41, 45]. Diagnostic tests included ultrasound scan, computerized axial tomography, fibrogastroscopy, endoscopic retrograde cholangio-pancreatography (ERCP), transparietohepatic cholangiography (TPHC), gammagraphy, laparoscopy and exploratory laparotomy [46]. We classified as ‘invasive’ diagnostic tests fibrogastroscopy, ERCP, TPHC, gammagraphy, laparoscopy and laparotomy. When a diagnostic procedure was performed more than once, the physician who extracted the data chose the more informative result. Socio-demographic information and additional information regarding symptoms and medical history were obtained directly from patients during their hospital stay by interview with trained monitors [4, 44].
Definitive diagnosis
A panel of experts in gastrointestinal diseases, comprising surgeons and gastroenterologists with extensive experience in pancreatic and biliary cancer, a medical oncologist and several physician epidemiologists, reviewed the hospital discharge diagnosis and all pathological and clinical information available, including follow-up, to achieve a consensual definitive diagnosis [32, 33, 44] This process was carried out blinded to the results of K-ras analysis and has also been described elsewhere in detail [33]. The definitive diagnosis was categorised into five groups: EPC, cancer of the extra-hepatic biliary system, other malignancy, benign pancreatic disease, and other benign disease. For the purpose of this study, these groups were used for the reference standard. The diagnostic index was calculated comparing patients definitively diagnosed with EPC with all other patients in the remaining four categories.
Detection of K-ras mutations
Details of laboratory protocols have also been described elsewhere [31, 36–44]. Briefly, mutations in codon 12 of K-ras oncogene were studied using DNA extracted from paraffin-embedded tumor tissue. Amplifications were done in two steps by nested PCR; an artificial BstNI restriction endonuclease site was introduced to discriminate between wild-type and mutated K-ras codon 12 sequences. Products were analyzed by acrylamide gel electrophoresis and ethidium bromide staining. This technique was able to detect one homozygous mutated cell in the presence of 102 normal cells. To characterize the nucleotide substitution in codon 12, all mutated samples were further analyzed using a similar RFLP-based approach. Interpretation of digestion products’ electrophoresis was performed independently by two investigators to confirm the results.
Statistical analysis
Univariate statistics were computed as customary [47]. For comparisons between continuous variables, Mann–Whitney’s U test and Student’s t test were used. In contingency tables, Fisher’s exact test for homogeneity or independence was applied to assess the relationship between two categorical variables. Diagnostic accuracy of detecting K-ras mutation was expressed in terms of sensitivity and specificity with their corresponding 95% confidence intervals (CI) [26, 28]. Data analysis was performed with SPSS 15.0 and Stata 8.0.
Results
Representativeness of the sample of patients
In this study, 212 patients contributed to the analysis of the diagnostic potential of detecting K-ras mutations. Although we prospectively attempted to include all individuals with suspected EPC or a definitive diagnosis of EPC, we were unable to include 162 patients due, first, to unavailability of a sample suitable for K-ras analysis and, to a lesser extent, to failure to establish the mutational status of the oncogene. Table 1 shows that excluded individuals were older than patients included in the analyses, and were less likely to be diagnosed definitively with EPC. Differences were observed in the diagnostic techniques performed in these two patient groups and in the recruitment hospital; diagnostic procedures vary by hospital and are linked to availability of tissue sample, the primary factor relating to failure to determine K-ras. Furthermore, the diagnostic work-up is influenced by a number of factors, including patient characteristics as age (e.g., older patients are less likely to undergo invasive tests).
Definitive diagnoses and K-ras mutations
Among patients included in the study, the most frequent pathologies were EPC (n = 121 patients, 57.1%) and cancer of the extrahepatic biliary system (35, 16.5%). K-ras codon 12 was mutated in approximately half of all patients (114, 53.8%). While K-ras mutations were observed in all diagnostic groups (Table 2), the frequency was highest in patients definitively diagnosed with EPC (94, 77.7%), followed by cancer of the extra-hepatic biliary system (11, 31.4%), and other malignant diseases (6, 24.0%). Thus, 27 of the 121 subjects with EPC (22.3%) had wild-type K-ras. Tumours of patients with EPC had the following stage distribution: 25 (20.7%) were in stage I, 21 (17.4%) in stage II, 15 (12.4%) in stage III, and 60 (48.6%) in stage IV. There was no significant difference in the prevalence of mutated K-ras across stages, with 18 (72%) of stage I cancers harbouring the mutation, 19 (90.5%) of stage II, 12 (80.0%) of stage III, and 45 (75%) of stage IV cancers (P = 0.441).
Diagnostic validity of K-ras mutations for exocrine pancreatic cancer
The sensitivity and specificity of the K-ras mutational status for the diagnosis of EPC in our patient sample were 77.7% (95% CI: 69.2–84.8) and 78.0% (68.1–86.0), respectively. If we limit the analysis to the 196 patients who entered the study with a suspected diagnosis of EPC, thus excluding 16 patients with a definitive diagnosis of EPC but missing information on the suspected diagnosis, the values of sensitivity and specificity were almost identical (77.1 and 78.0%, respectively). The diagnostic accuracy was unmodified by the sex or age of the patient (Table 3). We also evaluated the diagnostic validity of K-ras in certain clinical subgroups related with results from blood analyses and imaging tests, and found that the observed values for both sensitivity and specificity did not change significantly (Supplementary data, Tables S1, S2, and S3). We further assessed the potential clinical validity of detecting K-ras mutations in combination with other clinical information. Thus, in patients with either mutated K-ras or CEA > 5 ng/ml, the sensitivity and specificity were 81.0% (72.9–87.6) and 62.6% (72.9–87.6), respectively. When we considered only patients with mutated K-ras and CEA > 5 ng/ml the sensitivity was markedly reduced. This pattern was seen with all other analytes considered (Supplementary data, Tables S4 and S5). Results on the diagnostic accuracy of K-ras according to different comparisons and patient populations are shown in Table S6. Sensitivity was below 60% when the target disease was all malignant disorders, which is an uncommon clinical scenario. For all other comparisons, sensitivity and specificity were both greater than 75% (Supplementary data, Table S6).
Discussion
In this clinically relevant large sample of patients the sensitivity and specificity of K-ras mutations were less than ideal, 77.7% (95% CI: 69.2–84.8) and 78.0% (68.1–86.0), respectively. The clinical validity of mutated K-ras as an independent form of identifying EPC is hence limited, because more than 20% of the cases would erroneously be classified as non-pancreatic cancer (false negatives), and at least 20% of patients classified as EPC due to mutated K-ras would actually suffer from a distinct disease (false positives).
Diagnostic accuracy values remained remarkably stable when socio-demographic or clinical variables were considered. In this study, K-ras analysis was performed in histological and cytological samples, thus taking advantage of the two common procedures. K-ras mutational analysis could be used as an adjunct to cytology, potentially increasing the sensitivity, or it could be ordered only in cases where cytology is negative or inconclusive. In this study, we were unable to consider these scenarios, whose feasibility in a research study is uncertain.
As expected on clinical grounds, it was not possible to perform K-ras analysis in all patients who entered the PANKRAS II study with a suspicion of EPC. Nevertheless, selection criteria are among the widest on this field, and the pragmatic allowance of different methods of tissue collection made it possible to include a patient spectrum rather greater than in most previous studies [14]. The prompt identification of cases is an another strength of the study [48]. We included 19 patients who were definitively diagnosed with EPC during the study but in whom information regarding suspected diagnosis at hospital admission was missing. The decision to include these patients did not take into account their K-ras mutational status and, therefore, the diagnostic sensitivity we calculated was not influenced. In our population the prevalence of EPC may be different than in other clinical contexts; since positive and negative predictive values are highly influenced by disease prevalence, the predictive values of K-ras mutations will differ in other settings from values estimated in this report [27–30].
Although fieldwork for PANKRAS II study was carried out more than a decade ago, in our view the results presented here are pertinent and relevant today. During this time little progress has been made in the development of valid, evidence-based diagnostic procedures, including new molecular and ‘omics’ techniques [14]. Also regrettably, patients continue to be diagnosed late, often precluding any chance of curative treatment. On a population basis, survival rates for this aggressive tumour have remained stable in many regions worldwide [2, 49].
In many cases, cytological or histological samples were collected during exploratory laparotomy, a relatively common procedure when EPC is suspected. However, K-ras analysis was also common in cytological samples obtained through less invasive measures as fine needle aspiration. Nevertheless, the sensitivity and specificity of K-ras did not depend on the method of tissue collection.
In conclusion, we have calculated the sensitivity and specificity of K-ras mutation for detecting EPC in a wide spectrum of patients with a variety of related pathologies common in many clinical settings. While the diagnostic index for detecting K-ras mutations in this context was not sufficiently high for independent diagnostic use, it seems premature to rule out the analysis of K-ras in conjunction with other technologies, especially in light of the advances in the ‘omics’ fields.
Abbreviations
- BPD:
-
Benign pancreatic disease
- CEBS:
-
Cancer of the extra-hepatic biliary system
- CI:
-
Confidence interval
- CP:
-
Chronic pancreatitis
- EPC:
-
Exocrine pancreatic cancer
- ERCP:
-
Endoscopic retrograde cholangio-pancreatography
- IQR:
-
Interquartile range
- OBD:
-
Other benign disease
- OM:
-
Other malignancy
- OR:
-
Odds ratio
References
Stathis A, Moore MJ. Advanced pancreatic carcinoma: current treatment and future challenges. Nat Rev Clin Oncol. 2010;7:163–72.
Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–17.
Takhar AS, Palaniappan P, Dhingsa R, Lobo DN. Recent developments in diagnosis of pancreatic cancer. BMJ. 2004;329:668–73.
Porta M, Fabregat X, Malats N, Guarner L, Carrato A, de Miguel A, et al. Exocrine pancreatic cancer: symptoms at presentation and their relation to tumour site and stage. Clin Transl Oncol. 2005;7:189–97.
Duffy MJ, Sturgeon C, Lamerz R, Haglund C, Holubec VL, Klapdor R, et al. Tumor markers in pancreatic cancer: an European group on tumor markers (EGTM) status report. Ann Oncol. 2010;21:441–7.
Freelove R, Walling A. Pancreatic cancer: diagnosis and management. Am Fam Physician. 2006;73:485–92.
Beger HG, Matsuno S, Cameron JL. Diseases of the pancreas: current surgical therapy. Berlin: Springer; 2008.
von Hoff DD, Evans DB, Hruban RH, editors. Pancreatic cancer. Boston: Jones and Bartlett; 2005.
Howard JM, Idezuki Y, Ihse I, Prinz RA, editors. Surgical diseases of the pancreas. 3rd ed. Baltimore: Williams and Wilkins; 1998.
Beger HG, Warshaw AL, Büchler MW, Carr-Locke DL, Neoptolemos JP, Russell C, Sarr MG, editors. The pancreas. Vol. 2. Oxford: Blackwell; 1998.
Abraham SC, Wilentz RE, Yeo CJ, Sohn TA, Cameron JL, Boitnott JK, et al. Pancreaticoduodenectomy (Whipple resections) in patients without malignancy: are they all ‘chronic pancreatitis’? Am J Surg Pathol. 2003;27:110–20.
Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M. Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell. 1998;53:549–54.
Tada M, Omata M, Ohto M. Clinical application of ras gene mutation for diagnosis of pancreatic adenocarcinoma. Gastroenterology. 1991;100:233–8.
Parker LA, Lumbreras B, Hernández-Aguado I, Porta M. How useful is it clinically to analyse the K-ras mutational status for the diagnosis of exocrine pancreatic cancer? A systematic review and meta-analysis. Eur J Clin Invest. 2011 (in press).
Marchese R, Muleti A, Pasqualetti P, Bucci B, Stigliano A, Brunetti E, et al. Low correspondance between K-ras mutations in pancreatic câncer tissue and detection of K-ras mutations in circulating DNA. Pancreas. 2006;32:171–7.
Wenger FA, Zieren J, Peter FJ, Jacobi CA, Müller JM. K-ras mutations in tissue and stool samples from patients with pancreatic cancer and chronic pancreatitis. Langenbecks Arch Surg. 1999;384:181–6.
Trümper L, Menges M, Daus H, Köhler D, Reinhard JO, Sackmann M, et al. Low sensitivity of the ki-ras polymerase chain reaction for diagnosing pancreatic cancer from pancreatic juice and bile: a multicenter prospective trial. J Clin Oncol. 2002;20:4331–7.
Liu TH, Wang ZY, Cui QC. Significance of the detection of Ki-ras codon 12 mutation in the diagnosis of pancreatic carcinoma. Int J Surgical Path. 1995;3:93–100.
Van Laethem JL, Vertongen P, Deviere J, Van Rampelbergh J, Rickaert F, Cremer M, Robberecht P. Detection of c-Ki-ras gene codon 12 mutations from pancreatic duct brushings in the diagnosis of pancreatic tumours. Gut. 1995;36:781–7.
Zheng M, Liu LX, Zhu AL, Qi SY, Jiang HC, Xiao ZY. K-ras gene mutation in the diagnosis of ultrasound guided fine-needle biopsy of pancreatic masses. World J Gastroenterol. 2003;9:188–91.
Mora J, Puig P, Boadas J, Urgell E, Montserrat E, Lerma E, et al. K-ras gene mutations in the diagnosis of fine-needle aspirates of pancreatic masses: prospective study using two techniques with different detection limits. Clin Chem. 1998;44:2243–8.
Shibata D, Almoguera C, Forrester K, Dunitz J, Martin SE, Cosgrove MM, et al. Detection of c-K-ras mutations in fine needle aspirates from human pancreatic adenocarcinomas. Cancer Res. 1990;50:1279–83.
Villanueva A, Reyes G, Cuatrecasas M, Martínez A, Erill N, Lerma E, et al. Diagnostic utility of K-ras mutations in fine-needle aspirates of pancreatic masses. Gastroenterology. 1996;110:1587–94.
Pugliese V, Pujic N, Saccomanno S, Gatteschi B, Pera C, Aste H, Ferrara GB, Nicolò G. Pancreatic intraductal sampling during ERCP in patients with chronic pancreatitis and pancreatic cancer: cytologic studies and k-ras-2 codon 12 molecular analysis in 47 cases. Gastrointest Endosc. 2001;54:595–9.
Van Laethem JL, Bourgeois V, Parma J, Delhaye M, Cochaux P, Velu T, et al. Relative contribution of Ki-ras gene analysis and brush cytology during ERCP for the diagnosis of biliary and pancreatic diseases. Gastrointest Endosc. 1998;47:479–85.
Parker LA, Gómez Saez N, Lumbreras B, Porta M, Hernández-Aguado I. Methodological deficits in diagnostic research using ‘-omics’ technologies: Evaluation of the QUADOMICS tool and quality of recently published studies. PLoS One. 2010;5(7):e11419.
Fletcher RH, Fletcher SW. Clinical epidemiology. The essentials. 4th ed. Philadelphia: Lippincott, Williams and Wilkins; 2005.
Haynes RB, Sackett DL, Guyatt GH, Tugwell P. Clinical epidemiology. How to do clinical practice research. 3rd ed. Philadelphia: Lippincott, Williams and Wilkins; 2005.
Pepe MS, Etzioni R, Feng Z, Potter JD, Thompson ML, Thornquist M, et al. Phases of biomarker development for early detection of cancer. J Natl Cancer Inst. 2001;93:1054–61.
Porta M, ed. A dictionary of epidemiology. 5th ed. New York: Oxford University Press; 2008. p. 66, 69, 191, 201, 227, 233–6, 255, 258.
Porta M, Malats N, Jariod M, Grimalt JO, Rifà J, Carrato A, et al. Serum concentrations of organochlorine compounds and K-ras mutations in exocrine pancreatic cancer. Lancet. 1999;354:2125–9.
Soler M, Malats N, Porta M, Fernandez E, Guarner L, Maguire A, et al. Medical conditions in patients with pancreatic and biliary diseases: validity and agreement between data from questionnaires and medical records. Dig Dis Sci. 1999;44:2469–77.
Porta M, Costafreda S, Malats N, Guarner L, Soler M, Gubern JM, et al. Validity of the hospital discharge diagnosis in epidemiologic studies of biliopancreatic pathology. Eur J Epidemiol. 2000;16:533–41.
Porta M, Malats N, Alguacil J, Ruiz L, Jariod M, Carrato A, et al. Coffee, pancreatic cancer, and K-ras mutations: updating the research agenda. J Epidemiol Community Health. 2000;54:656–9.
Real FX, Malats N, Lesca G, Porta M, Chopin S, Lenoir GM, et al. Family history of cancer and germline BRCA2 mutations in sporadic exocrine pancreas cancer. Gut. 2002;50:653–7.
Alguacil J, Porta M, Malats N, Kauppinen T, Kogevinas M, Benavides FG, et al. Occupational exposure to organic solvents and K-ras mutations in exocrine pancreatic cancer. Carcinogenesis. 2002;23:101–6.
Morales E, Porta M, Vioque J, López T, Mendez MA, Pumarega JA, et al. Food and nutrient intakes and K-ras mutations in exocrine pancreatic cancer. J Epidemiol Community Health. 2007;61:641–9.
Crous-Bou M, De Vivo I, Porta M, Pumarega JA, López T, Alguacil J, et al. CYP1B1 polymorphisms and K-ras mutations in patients with pancreatic ductal adenocarcinoma. Dig Dis Sci. 2008;53:1417–21.
Crous-Bou M, Porta M, López T, Jariod M, Malats N, Alguacil J, et al. Lifetime history of tobacco consumption and K-ras mutations in exocrine pancreatic cancer. Pancreas. 2007;35:135–41.
Crous-Bou M, Porta M, López T, Jariod M, Malats N, Morales E, et al. Lifetime history of alcohol consumption and K-ras mutations in pancreatic ductal adenocarcinoma. Environ Mol Mutagen. 2009;50:421–30.
Crous-Bou M, Porta M, Morales E, López T, Carrato A, Puigdomènech E, et al. Past medical conditions and K-ras mutations in pancreatic ductal adenocarcinoma: a hypothesis-generating study. Cancer Causes Control. 2009;20:591–9.
Porta M, López T, Pumarega J, Jariod M, Crous-Bou M, Marco E, et al. In pancreatic ductal adenocarcinoma blood concentrations of some organochlorine compounds and coffee intake are independently associated with KRAS mutations. Mutagenesis. 2009;24:513–21.
Gasull M, Porta M, Pumarega J, Vioque J, Bosch de Basea M, Puigdomènech E, et al. The relative influence of diet and serum concentrations of organochlorine compounds on K-ras mutations in exocrine pancreatic cancer. Chemosphere. 2010;79:686–97.
Crous-Bou M. Clinical and environmental influences on the prevalence of mutations in the K-ras oncogene in patients with pancreatic ductal adenocarcinoma. Doctoral dissertation [Dir.: Porta M], Universitat Autònoma de Barcelona, Barcelona, Spain; 2009. (http://www.imim.es/programesrecerca/epidemiologia/en_documentsgrecm.html [accessed 23 Nov 2010].
Porta M, Pumarega J, López T, Jariod M, Marco E, Grimalt JO. Influence of tumor stage, symptoms and time of blood draw on serum concentrations of organochlorine compounds in exocrine pancreatic cancer. Cancer Causes Control. 2009;20:1893–906.
Porta M, Ferrer-Armengou O, Pumarega J, López T, Crous-Bou M, Alguacil A, et al. Exocrine pancreatic cancer clinical factors were related to timing of blood extraction and influenced serum concentrations of lipids. J Clin Epidemiol. 2008;61:695–704.
Armitage P, Berry G, Matthews JNS. Statistical methods in medical research. 4th ed. Blackwell: Oxford; 2002.
Porta M, Pumarega J, Ferrer-Armengou O, López T, Alguacil J, Malats N, et al. Timing of blood extraction in epidemiologic and proteomic studies: results and proposals from the PANKRAS II Study. Eur J Epidemiol. 2007;22:577–88.
Gudjonsson B. Pancreatic cancer: survival, errors and evidence. Eur J Gastroenterol Hepatol. 2009;21:1379–82.
Acknowledgments
Supported in part by research grants from the Government of Catalonia (2009 SGR 1350, CIRIT 1999 SGR 00241 and 1998/BEAi400011); CIBER de Epidemiología y Salud Pública (CIBERESP), ‘Red temática de investigación cooperativa de centros en cáncer’ (C03/10), ‘Red temática de investigación cooperativa de centros en Epidemiología y salud pública’ (C03/09), and Fondo de Investigación Sanitaria (91/595, 92/0007, 95/0017 and 97/1138), Instituto de Salud Carlos III, Madrid, Government of Spain. The authors gratefully acknowledge scientific and technical assistance provided by Antonio Salas, Montserrat Andreu, Josep Lluís Piñol, Angels Serrat, David J. MacFarlane, Laura Ruiz, Elisabeth Carrillo, José Pumarega, Marta Crous-Bou, Leo Español, Puri Barbas and Yolanda Rovira.
Conflict of interest
The authors declare they have no competing financial interests nor other conflicts of interest. The study sponsors had no role and no involvement in the study design, nor in the collection, analysis, and interpretation of data; they also had no role and no involvement in the writing of the report, nor in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the PANKRAS II Study Group: Members of the Multicentre Prospective Study on the Role of the K-ras and other Genetic Alterations in the Diagnosis, Prognosis and Etiology of Pancreatic and Biliary Diseases (PANKRAS II) Study Group are mentioned in previous publications.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Parker, L.A., Porta, M., Lumbreras, B. et al. Clinical validity of detecting K-ras mutations for the diagnosis of exocrine pancreatic cancer: a prospective study in a clinically-relevant spectrum of patients. Eur J Epidemiol 26, 229–236 (2011). https://doi.org/10.1007/s10654-011-9547-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9547-8