Abstract
Chronic health problems may be related to body mass index (BMI, kg/m2), but this has been best documented in overweight and obese adults. The primary objective of this study was to identify factors associated with different categories of BMI in elderly men and women from the general population, also including the lower categories of BMI. In a cross-sectional population survey from the municipality of Tromsø, Norway we analyzed associations between BMI and a wide range of chronic disease conditions, lifestyle and socioeconomic factors. BMI was categorized into six groups (<20, 20.0–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9, ≥30.0 kg/m2). The study included 4,259 men and women aged 65 years and older from the general population. We found low relative weight (BMI < 20 kg/m2) to be associated with increasing prevalence of mental distress, hip fracture, smoking and low handgrip strength. A U-shaped relation to BMI was found for asthma and chronic bronchitis, poor current health and low physical activity. The higher categories of BMI were associated with low education level, a difficult economical situation, diabetes mellitus and ischemic heart disease. These results demonstrate that both low and high BMI are associated with a wide range of prevalent conditions and diseases in elderly men and women. For the clinician the findings emphasize the importance of nutritional assessment as part of the medical evaluation of elderly patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The elderly population is rapidly growing. By 2050, it is expected that one in three Europeans will be 60 years and older [1]. Chronic health problems are common in later life and may be closely related to nutritional status as reflected by body mass index (BMI).
Most previous studies of associations between BMI and various medical conditions have focused either on the detrimental effect of obesity [2, 3], adult populations without analysis of elderly participants in particular [4, 5], or some selected chronic diseases [6, 7]. A number of studies have found malnourished patients in hospitals or community to be at increased risk of disease [8]. However, there are few population-based studies of elderly persons including all categories of BMI. Thus, important factors associated with low BMI compared to other BMI categories in this age group may not have been identified.
The primary objective of the present study was to address these problems by exploring relationships between BMI and a wider selection of health-related variables in elderly men and women from the general population, including also the lower range categories of BMI.
Methods
Study population
The Tromsø study is a single centre, population-based longitudinal study with repeated health surveys of the municipality of Tromsø, Norway. The fourth cross-sectional survey of the population was conducted in 1994–1995. All inhabitants in the municipality aged 25 years and more were invited and examined at a research centre. The present analyses are restricted to participants aged 65 years and older. A total of 5,892 subjects in this age group were invited and 4,351 non-institutionalized persons attended the survey. Among them, 92 persons were not willing to take part in research or information concerning height and/or weight was missing. Thus, 2,447 women and 1,812 men with mean age (SD) 73.1 (5.6) and 72.3 (5.9) years, respectively, were included in the analysis. The overall attendance rate was 72%, declining with increasing age (Table 1). In subjects aged <79 years old, 81% attended.
The survey was approved by the regional board of research ethics, and each participating subject gave written informed consent.
Categories of body mass index
Height and weight were measured without shoes in light clothing. BMI was calculated as weight divided by the square of height (kg/m2).
The BMI was in the main analyses divided into six categories (<20.0, 20.0–22.4, 22.5–24.9, 25.0–27.4, 27.5–29.9, ≥30.0 kg/m2) and thereby included the WHO (World Health Organization) definitions of low weight (<20 kg/m2), overweight (25.0–29.9 kg/m2) and obesity (≥30 kg/m2) [9]. Subjects with BMI < 18.5 kg/m2 and 18.5–19.9 kg/m2 were merged in the analysis as only 80 subjects were in the former group. Furthermore, in the main tables, we present the results with BMI ≥ 30 kg/m2 as the top category due to low number of cases of some of the considered clinical conditions in obese subjects. In order to better describe differences across the range of BMI, we divided the 20.0–24.9 kg/m2 and the 25.0–29.9 kg/m2 brackets of BMI into two groups, respectively.
The category of BMI < 20 kg/m2 was in this study classified as low relative weight and included the categories borderline underweight and undernutrition from the ESPEN (European Society of Parenteral and Enteral Nutrition) guidelines for Nutrition Screening [10]. BMI < 20 kg/m2 has been proposed by several authors as the cut-off value indicating risk of malnutrition in elderly individuals [11, 12].
Medical conditions and lifestyle variables
A self-administrated questionnaire was completed by the participants and included questions across a wide range of diseases and symptoms, smoking habits, intake of alcohol, social conditions, education, financial difficulties and level of physical activity. Detailed information concerning present and past smoking habits were classified into never, previous or current smoking. Age of disease onset was, except for cancer, also self-reported. We calculated the time since diagnosis. Four groups of health-related variables were considered: (1) Specific medical conditions, (2) Self-assessed current health, (3) Social and lifestyle characteristics and (4) Functional level.
We selected nine symptomatic medical conditions prevalent in the elderly population that might have connection to either low weight or obesity [8, 13]. Most of these conditions were self-reported by answering survey questions as “Do you have or have you had….?” The considered conditions were cancer, mental distress, hip fracture, asthma or chronic bronchitis, stroke, angina pectoris or myocardial infarction and diabetes mellitus. We combined asthma and chronic bronchitis in the analysis as a high proportion responded positively for both diseases, and comparable spirometry values in both groups were found in a later evaluation of the same population [14]. Information regarding angina pectoris and previous myocardial infarction were merged into the variable ischemic heart disease (IHD). Data concerning history of cancer was obtained from the Norwegian Cancer Registry. The latter are based on mandatory registration.
The mental health was evaluated by means of an index based on seven questions concerning different dimensions of mental distress [15]. This mental distress index was partly derived from the Hopkins Symptom Check List [16] and the General Health Questionnaire (GHQ) [17]. The index has been compared with the Hospital Anxiety and Depression Scale [18] and Hopkins Symptom Check List with a reasonably good agreement also in elderly subjects. A cut-off value of 2.15 has been proposed to identify persons with significant mental distress [15].
The self-reported overall health was assessed by the question “What is your current state of health?” with the answer categories: Poor, not so good, good and very good. In the analyses, the first two categories were merged (labeled poor), as were the two last categories (labeled good).
Information on marital status was obtained from the National Population Register. Single marital status indicates in our analyses that the respondent has never been married, previously married or is a widow(er). Low educational level was defined as primary school only. Self-reported current economical situation was evaluated with four categories from very good to very difficult and the two lowest categories were categorized as difficult. This question was answered only by subjects aged 70 years and above. Alcohol consumption was low and dichotomized into drinking monthly or more frequently versus a lower consumption.
We defined the participants as having low physically activity if they reported lightly activity (not sweating or out of breath) less than 1 h a week during the past year. Handgrip strength of the non-dominant hand was registered as kilopascal (kPa) generated by manual compression of an air filled rubber bulb connected to a manometer. A measurement below the median value for each sex, respectively, was defined as low. All subjects aged 65–74 and a random sample (8% sample) of those aged 75–84 were eligible for measurement of grip strength and we have data from 74% (2,555/3,473) of these subjects.
Data analysis
In addition to simple descriptive statistics, the difference in the distribution of the BMI groups according to age group or sex (Table 2) was tested with a chi-square test, as were the relationships between the different dependent variables considered and the categories of BMI (Table 3). We calculated odds ratios for the different dichotomized chronic diseases, social and lifestyle factors according to the six different BMI categories using logistic regression (Table 4). The upper-normal category according to WHO [9], BMI 22.5–24.9 kg/m2, was chosen as the reference category. The estimates were adjusted for sex, age (65–71, 72–78, ≥79 years old) and smoking (current, previous and never smoking). In addition, for each analysis displayed in Table 4, we included, in a separate logistic regression analysis, a cross product terms of sex and BMI to test for interactions by sex. Furthermore, when the results from the logistic regression analysis suggested a non-linear (typically U- or inverse J-shaped) relationship, we tested for a non-linear relation with BMI by including as predictors the BMI-categories (coded 1–6 as a continuous variable) both as a linear term and a second order term. Similarly, when the results from the logistic regression analysis suggested a linear relationship, we tested for a linear relation with BMI. A two-sided P-value <0.05 was considered statistically significant.
Analyses were performed using SPSS statistical software version 15.0 (SPSS Inc, Chicago Illinois. USA).
Results
Prevalence of different BMI categories
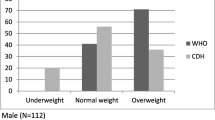
The overall proportion with BMI < 20 kg/m2 (low weight) was 5.1%, BMI 20.0–24.9 kg/m2 (normal weight) 35.8%, BMI 25.0–29.9 kg/m2 (overweight) 42.1% and BMI ≥ 30.0 kg/m2 (obesity) 16.9% (Table 2). The distribution of the BMI groups differed significantly between the sexes (P < 0.001). Obesity was more common in women than in men (21.8% vs. 10.4%), whereas a comparable proportion of women and men had BMI below 20 kg/m2, 5.4 and 4.7%, respectively. In women, no significant age difference was seen between BMI categories, whereas in men, indications of an inverse linear relationship between age and BMI was observed (P = 0.016).
Lifestyle, socio-economic status and medical conditions
Characteristics of the participants according to BMI category and sex are shown in Table 3. Compared to men, women tended to live alone, have lower education and consume alcohol less frequently. Current and previous smoking was much more prevalent in men than in women.
About 60% of the women and 50% of the men considered their overall current state of health to be poor or not so good. Approximately one in five subjects reported asthma, chronic bronchitis or IHD. The prevalences of mental distress, diabetes mellitus and history of hip fracture, stroke or cancer were between three and eleven percent (Table 3). The median time since the first diagnosis of stroke, hip fracture and cancer was four, 6 and 7 years, respectively.
Current smoking, mental distress and hip fracture were in both sexes more prevalent in the lower BMI categories. Asthma or chronic bronchitis and a poor current health were more frequent both in the lower and higher BMI categories. The higher BMI categories were associated with diabetes mellitus and IHD.
Associations between BMI categories, lifestyle and disease prevalence
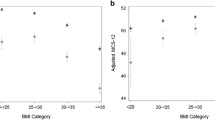
Table 4 shows the adjusted associations between BMI and the prevalence of some chronic diseases, social and lifestyle factors. The results for the medical conditions are displayed graphically in Fig. 1 as well. The test for interaction by sex was for all variables non-significant (P-values between 0.07 and 0.89) except for hand-grip strength (P = 0.016). However, stratified analyses revealed the same overall pattern also for this variable for men and women, and we therefore report the values for men and women combined in Table 4.
Adjusted odds ratios for associations between various medical conditions and BMI in elderly men and women (a–h). Subjects with 22.5–24.9 kg/m2 constitute the reference category. Error bars indicate 95% confidence interval. Adjusted for sex, age and smoking (current, former and never smoking). The Tromsø study
Low socioeconomic status was associated with the higher BMI categories. Low physical activity was more common both in the low weight and obese subjects, whereas reduced muscle strength was related to low weight. Current smoking was strongly inversely related to BMI. In Table 4 we give the results for current versus previous and never smokers combined as the results for never and previous smokers were similar.
Diabetes mellitus and IHD were associated only with the higher BMI categories; diabetes mellitus with obesity and IHD both with overweight and obesity. Asthma or chronic bronchitis and a poor current state of health showed a U-shaped relation to BMI (P-value for a second order term <0.05). The prevalence of mental distress and previous hip fracture were both inversely associated with BMI (P-value for linear trend 0.05 and <0.001, respectively). Figure 1e and h, may be suggest that both history of stroke and cancer were related to BMI < 20 kg/m2, although these associations did not reach statistical significance.
Discussion
The present study points out characteristics of the lower and higher categories of BMI in elderly men and women. The results demonstrate that low weight is associated with fractures, mental distress, and low muscle strength. U-shaped relationships with BMI were found for asthma or chronic bronchitis, low physical activity and a general poor current health. The higher weight categories were associated with IHD and diabetes. Low socioeconomic status was associated with a high BMI. To the best of our knowledge there is no other recent population-based study focusing on all BMI categories assessing a similar wide range of conditions in elderly persons.
The prevalence of low weight (BMI < 20 kg/m2) was about five percent. This is in accordance with findings from other community based studies [19, 20]. Both overweight and obesity were in this population less frequent than reported in studies of elderly individuals in the U.S. [21] but at the same level as found in a study with data from several European countries [4].
It could be assumed that low socioeconomic status reflected by difficult economy and low education and, should affect food habits adversely and predispose to a lower BMI. A study of elderly admitted patients found education below 12 years to be a risk factor for malnutrition [22]. In the present study, however, neither low education level nor difficult economic situation were related to low BMI. As earlier described in middle aged populations [23], a lower educational level was associated with obesity.
We observed a strong negative impact of current tobacco smoking on BMI. This has also previously been reported [24], and may be explained by increased basal metabolic rate [25] and impairment of smell and taste [26] in smokers.
Alcohol intake was very moderate in this population. Studies of hospital populations with more heavy drinkers have demonstrated a negative impact of alcohol use on nutritional status [27, 28].
Low physical activity, one aspect of physical function, was in this study associated with both low weight and obesity. A similar U-shaped relation between BMI and functional impairment was found in another study of community-dwelling elderly persons using a wider range of assessment techniques [29]. We also found low handgrip strength to be strongly associated with BMI < 20 kg/m2. Grip strength, important for daily life activities, is a predictor of disability [30] in addition to an indirect measure of lean body mass [31]. Low muscle mass in underweight individuals may explain both a reduced handgrip and a lower level of physical activity. Obesity has also in studies by other authors found to be associated with an impaired functional level [32]. Several mechanisms may explain these findings, including obesity related reduction in flexibility of movement and increased wear and tear on joints [33]. Furthermore, both underweight and obesity may be associated with diseases and conditions which in turn increase the risk of functional impairment [32].
Self assessed current state of health represent an overall subjective perception corresponding well with physicians’ assessments and other objective health measures [34]. Compared to the reference group, we found a higher frequency of self-assessed poor health in both the higher and lower categories of BMI including the lower normal category of 20–22.4 kg/m2. A similar U-shaped relationship was found when a corresponding question was used in a study evaluating obesity among adults in several European countries [4].
We found indications of increased mental distress among participants with BMI below 20 kg/m2. The symptoms of anxiety and depression are often overlapping, especially in the more minor forms [35] and the index of mental distress used in this study included both set of symptoms. Our findings correspond with results from a study of hospitalized elderly patients evaluating depressive symptoms only [36]. However, a study of non-institutionalized adult and elderly persons found an association of both mood, anxiety and personality disorders to overweight and obesity, but not to underweight [37]. We did not find any association between symptoms of anxiety or depression and the higher categories of BMI.
Hip fracture represents an acute incident often resulting in persistent functional decline [38]. In this study, the median time since the last hip fracture was 6 years and still there was an inverse relation between hip fracture and BMI. This is consistent with other studies [39, 40]. Underweight is a risk factor for osteoporosis [41], which in turn increases the risk of a fall resulting in fracture. One previous study found, even after adjustment for bone mineral density, that underweight was associated with fracture risk [42]. Insufficient protective padding over the hips in underweight individuals is one important mechanism [43].
We found a U-shaped association between chronic bronchitis or asthma and BMI and this relationship was retained when each variable was evaluated separately. These two conditions cover a high proportion of patients with chronic obstructive pulmonary disease (COPD) and there is considerable overlap between the subtypes of COPD [44]. Other community-based studies predominantly in adult and not elderly populations have confirmed an association of COPD to malnutrition and partly to obesity [6, 45].
Pulmonary cachexia, commonly identified by a low BMI, is an aspect of COPD characterized by both loss of muscle mass with or without loss of fat mass [46]. This muscle wasting is not completely understood, but may involve an increase in peripheral muscular vulnerability to oxidative stress [46]. The explanations of underweight in COPD patients further include insufficient nutritional intake because large meals can induce shortness of breath [6]. Additionally, both activity-induced and daily energy expenditure have been found to be increased in many of these patients [47]. There may be several explanations for the observed association between obesity and COPD, including a direct affect on airway calibre through chest wall restriction [6]. A more sedentary lifestyle in obese people may affect breathing pattern and pulmonary function adversely [6].
Diabetes mellitus and IHD were related to obesity, an association well documented in the literature [2, 4] and mainly mediated by an increase in insulin resistance [48]. Earlier studies comparing both adult and elderly populations have found the relative risk associated with overweight for diabetes mellitus [49] and IHD [49, 50] to decline with age. In our study, the risk associated with overweight was even more limited. We found IHD to be the only disease with significantly increased prevalence in the upper overweight category (BMI 27.5–29.9 kg/m2). More research is needed to define the upper limit of healthy weight in elderly individuals. However, as six out of ten subjects are overweight or obese, affected cases in the upper BMI categories constitute a high number.
Previous studies have shown malnutrition in acute stroke patients to increase the risk of both in-hospital mortality and a poor clinical outcome [51, 52]. In cancer patients, weight loss is often an indication of poor survival [53]. Consequently, survivor bias can explain the lack of significant association found between cancer, stroke and the lower BMI category in this study (Fig 1e, h). As the median time since the first cancer diagnosis was 7 years, the majority of these subjects were long-term survivors.
Our study has several strengths. All elderly men and women in the municipality were invited, the participation rate was high and a wide range of conditions was assessed. BMI values were based on measured rather than self-reported weight and height. Furthermore, including also the lower end of the BMI spectrum, gives important information about underweight individuals.
The use of BMI in an elderly population may be a source of error as body composition is not measured accurately. The relative fat mass is increasing in later life and at a given BMI value, an older person will have a higher proportion of the body as adipose tissue than a younger adult. Nevertheless, BMI is easy to use also in a clinical setting, has a reasonable good correlation with body fat [54], it is reproducible and it is the core measure in several nutrition risk screening instruments [10]. Additionally, most of the variables included in our study are self-reported. This implies a risk of misclassification, but this must be expected to be non-differential in most situations.
The cross-sectional design of this study restricts the possibility of cause-effect conclusions. For some of the variables the expected direction may be from disease or lifestyle variable to BMI category. This is likely for mental distress and smoking. For other medical conditions such as diabetes mellitus and IHD, a high BMI may increase the risk of disease. In some situations, both mechanisms may be of importance, thus creating a vicious circle. It has been shown that hip fracture patients who are malnourished at admission also lose weight during the course of the disease [55].
Conclusions
Our results demonstrate that both low and high BMI are associated with a wide range of prevalent conditions and diseases in elderly men and women. For the clinician this emphasizes the importance of nutritional assessment as part of the medical evaluation of elderly patients. Using BMI alone, a cut off of 20 kg/m2 identifies a subpopulation at risk in the lower part of the BMI spectrum. At the present time most attention is given to the link between the higher BMI categories and diseases, but our findings suggest that moderate overweight constitutes a relatively small health hazard in this age group.
Abbreviations
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- IHD:
-
Ischemic heart disease
- OR:
-
Odds ratio
- SD:
-
Standard deviation
References
World Population Prospects. The 2006 revision. New York: United Nations; 2007.
Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. 2004;27:1385–90.
Calza S, Decarli A, Ferraroni M. Obesity and prevalence of chronic diseases in the 1999–2000 Italian National Health Survey. BMC Public Health. 2008;28(8):140.
Andreyeva T, Michaud PC, van Soest A. Obesity and health in Europeans aged 50 years and older. Public Health. 2007;121:497–509.
Peytremann-Bridevaux I, Santos-Eggimann B. Health correlates of overweight and obesity in adults aged 50 years and over: results from the Survey of Health, Ageing and Retirement in Europe (SHARE). Obesity and health in Europeans aged > or =50 years. Swiss Med Wkly. 2008;138:261–6.
Guerra S, Sherrill DL, Bobadilla A, Martinez FD, Barbee RA. The relation of body mass index to asthma, chronic bronchitis, and emphysema. Chest. 2002;122:1256–63.
Choi BC, Shi F. Risk factors for diabetes mellitus by age and sex: results of the national population health survey. Diabetologia. 2001;44:1221–31.
Stratton RJ, Green CJ, Elia M, editors. Disease-related malnutrition: and evidence-based approach to treatment. Oxon: CABI Publishing; 2003. p. 93–155.
Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. Geneva: World Health Organization; 1995.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22:415–21.
Sergi G, Perissinotto E, Pisent C, Buja A, Maggi S, Coin A, et al. An adequate threshold for body mass index to detect underweight condition in elderly persons: the Italian Longitudinal Study on Aging (ILSA). J Gerontol A Biol Sci Med Sci. 2005;60:866–71.
Campillo B, Paillaud E, Uzan I, Merlier I, Abdellaoui M, Perennec J, et al. Value of body mass index in the detection of severe malnutrition: influence of the pathology and changes in anthropometric parameters. Clin Nutr. 2004;23:551–9.
Grundy EMD. The epidemiology of aging. In: Tallis RC, Fillit HM, editors. Brocklehurst’s textbook of geriatric medicine and gerontology. 6th ed. London: Churchill Livingstone; 2003. p. 3–21.
Medbø A, Melbye H. Lung function testing in the elderly—can we still use FEV1/FVC <70% as a criterion of COPD? Respir Med. 2007;101:1097–105.
Søgaard AJ, Bjelland I, Tell GS, Roysamb E. A comparison of the CONOR mental health index to the HSCL-10 and HADS. Nor J Epidem. 2003;13:279–84.
Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1–15.
Goldberg DP, Blackwell B. Psychiatric illness in general practice. A detailed study using a new method of case identification. Br Med J. 1970;1:439–43.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Perissinotto E, Pisent C, Sergi G, Grigoletto F. Anthropometric measurements in the elderly: age and gender differences. Br J Nutr. 2002;87:177–86.
de Groot CP, van Staveren WA. Survey in Europe on nutrition and the elderly, a concerted action. Undernutrition in the European SENECA studies. Clin Geriatr Med. 2002;18:699–708.
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55.
Feldblum I, German L, Castel H, Harman-Boehm I, Bilenko N, Eisinger M. Characteristics of undernourished older medical patients and the identification of predictors for undernutrition status. Nutr J. 2007;6:37.
Roskam AJ, Kunst AE. The predictive value of different socio-economic indicators for overweight in nine European countries. Public Health Nutr. 2008;11:1256–66.
Albanes D, Jones DY, Micozzi MS, Mattson ME. Associations between smoking and body weight in the US population: analysis of NHANES II. Am J Public Health. 1987;77:439–44.
Collins LC, Walker J, Stamford BA. Smoking multiple high versus low-nicotine cigarettes: impact on resting energy expenditure. Metabolism. 1996;45:923–6.
Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population. J Neurol. 2008;255:1121–6.
Manari AP, Preedy VR, Peters TJ. Nutritional intake of hazardous drinkers and dependent alcoholics in the UK. Addict Biol. 2003;8:201–10.
Santolaria F, Perez-Manzano JL, Milena A, Gonzalez-Reimers E, Gomez-Rodriguez MA, Martinez-Riera A, et al. Nutritional assessment in alcoholic patients. Its relationship with alcoholic intake, feeding habits, organic complications and social problems. Drug Alcohol Depend. 2000;59:295–304.
Galanos AN, Pieper CF, Cornoni-Huntley JC, Bales CW, Fillenbaum GG. Nutrition and function: is there a relationship between body mass index and the functional capabilities of community-dwelling elderly? J Am Geriatr Soc. 1994;42:368–73.
Rantanen T. Muscle strength, disability and mortality. Scand J Med Sci Sports. 2003;13:3–8.
Sternfeld B, Ngo L, Satariano WA, Tager IB. Associations of body composition with physical performance and self-reported functional limitation in elderly men and women. Am J Epidemiol. 2002;156:110–21.
Jenkins KR. Obesity’s effects on the onset of functional impairment among older adults. Gerontologist. 2004;44:206–16.
Launer LJ, Harris T, Rumpel C, Madans J. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA. 1994;271:1093–8.
Linn BS, Linn MW. Objective and self-assessed health in the old and very old. Soc Sci Med. 1980; 14A:311–5.
Katon W, Roy-Byrne PP. Mixed anxiety and depression. J Abnorm Psychol. 1991;100:337–45.
German L, Feldblum I, Bilenko N, Castel H, Harman-Boehm I, Shahar DR. Depressive symptoms and risk for malnutrition among hospitalized elderly people. J Nutr Health Aging. 2008;12:313–8.
Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: results from the national epidemiologic survey on alcohol and related conditions. Psychosom Med. 2008;70:288–97.
Wolinsky FD, Fitzgerald JF, Stump TE. The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health. 1997;87:398–403.
Lumbers M, New SA, Gibson S, Murphy MC. Nutritional status in elderly female hip fracture patients: comparison with an age-matched home living group attending day centres. Br J Nutr. 2001;85:733–40.
Meyer HE, Tverdal A, Falch JA. Risk factors for hip fracture in middle-aged Norwegian women and men. Am J Epidemiol. 1993;137:1203–11.
Michaelsson K, Bergstrom R, Mallmin H, Holmberg L, Wolk A, Ljunghall S. Screening for osteopenia and osteoporosis: selection by body composition. Osteoporos Int. 1996;6:120–6.
De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, et al. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330–8.
Slemenda C. Prevention of hip fractures: risk factor modification. Am J Med. 1997;103:65S–71S.
Marsh SE, Travers J, Weatherall M, Williams MV, Aldington S, Shirtcliffe PM, et al. Proportional classifications of COPD phenotypes. Thorax. 2008;63:761–7.
Chen Y, Breithaupt K, Muhajarine N. Occurrence of chronic obstructive pulmonary disease among Canadians and sex-related risk factors. J Clin Epidemiol. 2000;53:755–61.
Schols AM, Gosker HR. The pathophysiology of cachexia in chronic obstructive pulmonary disease. Curr Opin Support Palliat Care. 2009;3:282–7.
Baarends EM, Schols AM, Westerterp KR, Wouters EF. Total daily energy expenditure relative to resting energy expenditure in clinically stable patients with COPD. Thorax. 1997;52:780–5.
Bechtold M, Palmer J, Valtos J, Iasiello C, Sowers J. Metabolic syndrome in the elderly. Curr Diab Rep. 2006;6:64–71.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9.
Rimm EB, Stampfer MJ, Giovannucci E, Ascherio A, Spiegelman D, Colditz GA, et al. Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men. Am J Epidemiol. 1995;141:1117–27.
Davalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, et al. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996;27:1028–32.
Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65:39–43.
Bruera E. ABC of palliative care. Anorexia, cachexia, and nutrition. BMJ. 1997;315:1219–22.
Morabia A, Ross A, Curtin F, Pichard C, Slosman DO. Relation of BMI to a dual-energy X-ray absorptiometry measure of fatness. Br J Nutr. 1999;82:49–55.
Bachrach-Lindstrom M, Johansson T, Unosson M, Ek AC, Wahlstrom O. Nutritional status and functional capacity after femoral neck fractures: a prospective randomized one-year follow-up study. Aging (Milano). 2000;12:366–74.
Acknowledgments
This study was supported by a grant from the Centre for research in the elderly, the Northern Norway Regional health Authority. The National Health Screening Service helped organize and carry out the Tromsø 4 survey. J. -M. K. and B. K. J. were responsible for the design of the study. J. -M. K. did the analysis and wrote the first draft of the paper. B. K. J. contributed to the analysis, interpretation of the results and the review of the drafts. J. F. contributed to the study design, the interpretation of the results and reviewed the final draft. T. W. contributed to the statistical analysis, interpretation of the data and reviewed the final draft. All the authors approved the final version.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kvamme, JM., Wilsgaard, T., Florholmen, J. et al. Body mass index and disease burden in elderly men and women: The Tromsø Study. Eur J Epidemiol 25, 183–193 (2010). https://doi.org/10.1007/s10654-009-9422-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-009-9422-z