Abstract
To identify predictive factors for 2-year mortality in frail elderly patients after acute hospitalisation, and from these to derive and validate a Mortality Risk Index (MRI). A prospective cohort of elderly patients was set up in nine teaching hospitals. This cohort was randomly split up into a derivation cohort (DC) of 870 subjects and a validation cohort (VC) of 436 subjects. Data obtained from a Comprehensive Geriatric Assessment were used in a Cox model to predict 2-year mortality and to identify risk groups for mortality. A ROC analysis was performed to explore the validity of the MRI. Five factors were identified and weighted using hazard ratios to construct the MRI: age 85 or over (1 point), dependence for the ADL (1 point), delirium (2 points), malnutrition risk (2 points), and co-morbidity level (2 points for medium level, 3 points for high level). Three risk groups were identified according to the MRI. Mortality rates increased significantly across risk groups in both cohorts. In the DC, mortality rates were: 20.8% in the low-risk group, 49.6% in the medium-risk group, and 62.1% in the high-risk group. In the VC, mortality rates were respectively 21.7, 48.5, and 65.4%. The area under the ROC curve for overall score was statistically the same in the DC (0.72) as in the VC (0.71). The proposed MRI appears as a simple and easy-to-use tool developed from relevant geriatric variables. Its accuracy is good and the validation procedure gives a good stability of results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It’s well recognised today that hospitalisation following the occurrence of an acute disease, notwithstanding treatment, puts elderly people at risk for functional, physical and/or mental deterioration [1]. However this risk seems to persist during post-hospital recovery [2]. Despite stabilisation of chronic diseases and/or treatment of acute pathologies, elderly people after discharge seem to be at high risk for rehospitalisation and above all for death. Thus care management of elderly patient hospitalised for an acute medical problem is a major focus in geriatric clinical practice. Indeed, acute hospitalisation is frequently associated with high mortality rates in the months following admission [3]. It is however difficult to rapidly and clearly identify appropriate therapeutic procedures, because of poly-pathology and multiple organ failures. Furthermore these patients present frequent associations of medical and psychological problems. Therapeutic options are usually limited by the risk of iatrogenic events.
Even if numerous predictors of mortality have already been reported in elderly people, the identification of vulnerable subjects remains empirical. Therefore an objective tool that, at the beginning of the hospital stay, identifies predictive factors for death following acute hospitalisation could be useful for practitioners to identify higher risk groups. It has been shown that it is possible to substantially reduce mortality among vulnerable elderly people if the risk factors for which there is scope for action are identified and dealt with early on [4]. Geriatric evaluation tools appear to provide an efficient tool to screen for individuals at risk [4, 5]. Better knowledge of the factors involved would provide assistance in therapeutic decisions, and would enable better definition of the aims of the care provision, and of relevant procedures [6, 7].
A French Study named SAFES (Sujet Âgé Fragile: Évaluation et Suivi-Frail Elderly Subject: Evaluation and Follow up) was set up. It was intended to constitute a cohort of elderly subjects considered a priori to be frail, in order to highlight their characteristics, their outcomes and their in-hospital itineraries. A way of targeting these subjects was to recruit them from emergency department. Indeed, an acute hospitalisation is often revealing of medical, psychological and social crisis situations that could have repercussions on the health condition of elderly people. The frailer patients (from a medical point of view) potentially need care in geriatric wards, but clinicians needs indicators to identify them more efficiently and to instate the most suitable modes of care provision.
The aim of the present study was, firstly, to identify predictive factors for 2-year mortality on a cohort of frail patients aged 75 or over following acute hospitalisation; and secondly, to derive a Mortality Risk Index (MRI) from predictive factors for death identified, and to validate this measure.
Methods
Study population
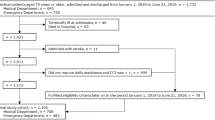
The SAFES cohort was formed within a National Research Program into the recruitment of emergency units in nine teaching hospitals. All nine centres had a geriatric ward.
The inclusion of subjects ran from March 1st 2001 to January 17th 2002. To be eligible, patients were to be 75 or over. They were to have been hospitalised in a medical ward in the same hospital as the emergency unit to which they were initially admitted. Subjects were not eligible if hospitalisation was into intensive care or surgery, or if admission did not occur after admission to the emergency unit. Every day in each centre, patients admitted to the emergency unit were registered. From the list thus obtained, patients were selected by random draw stratified at two levels: in each week, 5 days were selected randomly, and for each of these days, two patients were chosen randomly. Next, each patient was visited by a specialist in geriatrics familiar with the survey procedures. In the course of this interview, patients were informed about the study, prior to signing the consent form. If the clinical status and/or the cognitive status of the patient did not enable informed consent, the interviewer referred to the subject’s representative. Follow-up was by telephone interview after the 1st, 8th and 21st month and by face-to-face interviews after the 5th, 12th, 18th and 24th month following the initial hospitalisation. The patient was free to opt out of the study at any time on simple request, without any alteration to care provided, in observance of the Declaration of Helsinki and French law relating to biomedical research involving human subjects. The ethic committee required that patients give again their consent for the second year of follow up.
We randomly split up the subjects included in the SAFES cohort study into two samples, using SAS “Surveyselect” procedure (SAS Institute, release 9.0): two thirds of the population served to derive the prediction model, and one third to validate it.
Variables studied in both DC and VC
The following socio-demographic and environmental variables were studied: age, gender, living location (private home vs. institution), and educational level (primary or secondary school, or university).
The comprehensive geriatric assessment (CGA) included several measures. Dependency levels for activities of daily living (ADL) at baseline were assessed using Katz’s index [8]. Baseline performance for ADL was defined as the dependence level of the subject before the occurrence of the event motivating hospitalisation (performance in ADL 2 weeks before admission) [9]. The patient or someone close to him/her was questioned about the subject’s ability to perform the following activities: transferring, washing, dressing, toileting, eating, and continence. Dependence for the ADL was defined by the inability of the subject to perform at least one of these activities. Diagnosis of delirium was performed by a geriatrician according to DSM-IV criteria: disturbance of consciousness (defined by a Folstein’s Mini-Mental State Examination (MMSE) score of 24 or less [10]), change in cognition, and development over a short period of time [11]. Mood disorders and risk of depression were assessed using Schwab and Gilleard’s scale (score greater than 14) [12]. Evaluation of postural disorders and risk of falling was carried out using respectively the One-Leg Standing Balance Test [13] and reference to the occurrence of at least one fall in the preceding 12 months. The patient was considered to have difficulties balancing if s/he was unable to stand on either leg for at least 5 s. When s/he required more than 20 s to complete the Timed Get-up and Go Test, s/he was considered to have walking difficulties. A risk of malnutrition was defined as a Mini Nutritional Assessment short Form score of less than 12 [14]. The risk of developing pressure sores was assessed using the Norton’s scale: a score of 14 or less indicated risk of developing pressure sores [15]. A modified version of the Charlson’s co-morbidity index [16] (applicable to the tenth revision of the International Classification of Diseases) made it possible to define three levels of co-morbidity: low (score = 0 or 1), medium (score = 2 to 4), and high (score of 5 or more). These thresholds have already been used by other authors [17].
Conditions of admission to the Emergency Department (ED) were recorded: the day of admission, and whether or not there was a previous hospitalisation within the preceding 3 months.
Statistical analyses
Descriptive analysis of the administrative, socio-demographic, and clinical variables of the patients was performed. Numerical variables are described with mean and standard deviation (SD). For categorical variables, sample sizes and percentages are presented.
Survival time was the dependent variable in all analyses. For people who died within 2 years, survival time was defined as the duration between the admission to the ED and the date of death. The others were censored. The vital status was updated from the hospital wards (using the hospital network data-processing, or by a telephone follow-up) or, if missing, from the appropriate registry department where deaths are systematically registered in France.
Bivariable relationships between each risk factor and mortality in the DC were measured using Kaplan and Meier’s method and the Log Rank test.
For multivariable analysis, the Cox regression model was used in a stepwise method after looking for confounders and interactions in the stratified analyses. The threshold probability for entering variables into the model was P < 0.20. Removal threshold was P > 0.05. Age and investigating centre were considered as systematic adjustment variables. Results were presented in terms of Hazard Ratio (HR) and 95% Confidence Interval (CI).
To provide for proportionality of risks, age was dichotomised at the median. The three- (or more) level qualitative variables were converted into “dummy” variables [18].
Subjects who were still alive after 36 months were censored at the end-point. Those who were lost of follow-up or who withdrew their consent before the end-point were censored at the date of the last contact.
A mortality risk index to stratify subjects into different levels of risk for 2-year mortality was constructed. A point value was assigned to each characteristic according to the hazard ratio in the final model. Point values for all mortality-related characteristics present for each patient were rounded to the nearest integer and summed. Three groups were determined: low-risk group (score less than or equal to the first quartile), medium-risk group (score in the interquartile range), and high-risk group (score over the third quartile).
The accuracy of the mortality risk scoring system was determined by calculating and comparing the c-statistic, representing the area under the Receiver Operating Characteristic (ROC) curves, in both the DC and the VC [19–21].
Statistical analyses were performed using SAS software release 9.1, (SAS Institute, Inc., Cary, NC). Tests were considered as significant for P-values less than 0.05.
Results
Characteristics of participants
The 1,306 patients of the SAFES cohort were on average 85.0 ± 5.9 years old and women were more numerous (65%).
The mean age in the DC was 84.9 ± 5.9 years. Sixty-four percent were women (Table 1). On average, the women were older than the men (85.6 ± 5.9 vs. 83.6 ± 5.5 respectively, P < 0.001). Within the 2-year period, 383 (44.0%) out of 870 patients died, 114 (13.1%) withdrew their consent, and 68 (7.8%) were lost to follow-up.
In the VC mean ± SD age was 85.0 ± 6.1 years. The women were more numerous (64.4%) and were, on average, older than the men (85.6 ± 6.2 vs. 83.8 ± 5.8 respectively, P = 0.003). During the 2-year follow-up, 192 (44.0%) out of 436 patients died, 55 (12.6%) took back their consent, and 37 (8.5%) were lost to follow-up.
There were no survival rate differences between DC and VC (P = 0.91). Other characteristics for both the DC and the VC are fully described in Table 1.
Bivariable analysis
Predictive factors significantly associated with 2-year mortality in bivariable analysis in the DC included (Table 2): age of 85 years and older (P < 0.001), living in institution (P < 0.001), dependence for the ADL (P < 0.001), delirium (P < 0.001), malnutrition risk (P < 0.001), pressure sore risk (P < 0.001), walking difficulties (P < 0.001), medium (P = 0.003) or high co-morbidity level (P < 0.001), and hospitalisation within the previous 3 months (P = 0.004).
Multivariable analysis
The independent predictive factors for death identified in the DC were (Table 2): age of 85 years and older (P = 0.002), dependence for the ADL (P = 0.02), delirium (P < 0.001), malnutrition risk (P < 0.001), medium (P = 0.003) or high co-morbidity level (P < 0.001). A few factors significantly associated with 2-year mortality in bivariable analysis were not found to be independently linked to 2-year mortality in multivariable analysis. This was the case for living location, walking difficulties, and history of recent hospitalisation. Female gender was of borderline significance (P = 0.07). There was no significant effect of the investigating centre on 2-year mortality.
Derivation and validation of the mortality risk index
The point values assigned to each of the predictive factors identified in the final model are listed in Table 3. The score was calculated for each patient by summing the point values for each risk factor that was present. For example, an 87-year-old patient (age over 85 = 1 point) with delirium (defined according to DSM-IV criteria = 2 points), malnutrition risk (MNA-SF score less than 12 = 2 points), dependence for the ADL (loss of at least one ADL = 1 point), and with a medium level of co-morbidity (Charlson Co-morbidity Index between 2 and 4 = 2 points) would have a Mortality Risk Score of 8.
The mean score was 4 ± 2, the median = 4, and the range = [0–10]. The first quartile was 2 and the third quartile was 5.
As described in the methods section, three risk groups were determined: low-risk group: risk score less than 3 points; medium-risk group: score from 3 to 5 points; high-risk group: score greater than 5 points.
In the DC, the 2-year mortality rate increased significantly (P < 0.001) across risk groups. Similar results were observed in the VC (Table 3). The mortality risk index had roughly the same discriminant power in the DC (c-statistic = 0.72) as in the VC (c-statistic = 0.71).
Discussion
The aim of this study was to identify predictive factors for 2-year mortality and to provide an accurate and useful tool that could help to stratify elderly people into mortality risk groups. This work confirms the hypothesis that a CGA could be used to predict mortality within two years after an acute medical event.
The MRI we have developed includes socio-demographic variables (age) and medical conditions (cognitive function, nutritional status, functional status, and co-morbid conditions). These findings are consistent with the observation that mortality in older adults does not depend on a single factor [22, 23].
Among these variables, co-morbidity was found to be the strongest independent predictive factor for death. Other authors have found similar results [24, 25]. In our study as in that by Ponzetto [24], a Charlson index score of 2 or more constituted a significant risk of death. Alongside the co-morbidity level, nutritional disorders (measured using the MNA-SF) appeared as a risk factor for death within 2 years. In a 2-year follow-up, Van Nes [26] also observed a significant link between the MNA-SF score and mortality. In fact, whatever the measure (weight loss, body mass index, waist-hip ratio, nutritional status score, albuminaemia…), nutritional disorders appear constantly as a risk factor for death [7, 22, 26–28]. Delirium was also an independent predictive factor for death. Several studies confirm these results [29–31]. The effect of cognitive impairment on mortality is well known in the long term [25, 29, 32–35]. Functional status and age appeared as moderate factors for risk of death. In other studies [7, 9, 25, 35–37], the negative role of loss of autonomy with respect to mortality at 2 years has systematically been demonstrated. This association persisted in the present study even after adjustment for co-morbidity level. Age was also significantly associated with mortality. Teno [29] found similar results. Conversely, Walter [22] did not use age in his prognostic index because of a lack of significant association with death.
For methodological aspects, a differential bias could have been induced by an unbalanced distribution of lost of follow up or refusals in the three risk groups. However, an a posteriori analysis proved no significant difference in the distribution of these patients in the three risk groups, as well in the DC as in the VC. Several strong points deserve to be underlined. Indeed, it was a multi-centre prospective cohort study. The number of events observed was large, and this provided strong statistical power for the tests implemented. The interviewers were geriatricians, and the measures used have been validated and present good psychometric properties. Our models (derivation and validation) predicted 2-year mortality and had good discriminant power. Moreover, the proposed MRI was successfully validated in a randomly selected sample. Its accuracy is nearly the same as that of the index developed by Teno et al. [29], and better than that of an index proposed by other authors [35]. Lee et al. [38] proposed a similar method to develop a 4-year mortality prognostic index on larger cohorts. He obtained greater accuracy (c-statistic was 0.84 in the VC and 0.82 in the DC) but it is difficult to compare the two studies. Lee’s tool intended to assess younger subjects (50 and over) living in the community. Our tool specifically targets a frail geriatric population. Olsson et al. [39] also created a score for nonsurgical emergency department patients of 15 years or over to predict long-term mortality. This tool seems to be very relevant for emergency practitioners. Ours was intended to assist non-surgical post-emergency wards physicians in making decisions for elderly patients. That is why we focused on a CGA instead of acute state variables (such as arterial pressure, pulse rate, respiratory rate, oxygen saturation, Glasgow Coma Scale Score). In a clinical approach, the proposed MRI seems easy to use and helpful. Indeed, this prognostic index can be used as a simple point scoring system to classify elderly patients into low-, medium-, and high-risk groups for 2-year mortality. This information, used in non-surgical medical wards, could enable the early identification of the more vulnerable subjects (patients in group III) so as to improve their prognosis or to instate the most appropriate care. Their referral should be above all to geriatric medicine wards so that suitable care is provided from the start of hospitalisation. This applies with the exception of patients presenting a terminal disease (e.g. metastatic cancer) that requires management in a palliative care unit. Patients in group I can be admitted into non-geriatric medical wards because their condition probably does not require specific geriatric care. For patients in group II, early geriatric advice should be sought. Despite the accuracy of the tool, an external validation with a pilot study is required.
The results obtained were in line with starting hypotheses, and also with data in the literature. They have provided information that responds to the need to be able to identify potential risk factors present at the start of hospitalisation, in order to take specific action for subjects hospitalised in a medical ward. For reasons of feasibility (time required), it is difficult to implement a CGA. Thus, it would seem relevant to focus on widely available and easy-to-use risk factors for to 2-year mortality: co-morbidity level, nutritional status, functional status, and cognitive function. These factors could enable, on admission, early identification of high-risk patients for whom geriatric multidimensional interventions seem essential. Once the subjects at higher risk are clearly identified, it will be possible to focus on appropriate interventions: treating acute pathologies, improving nutritional status, diagnosing and managing cognitive disturbances, exercise training, physiotherapy, occupational therapy and so fourth.
As a conclusion, this prognostic index provides a simple tool that can help to characterise a group of patients that can be considered as very vulnerable. The majority of these patients will have an unfavourable outcome, and may indeed die within the two years following their admission. The variables identified as independent predictive factors can all lead to targeted therapeutic options.
References
Lang PO, Heitz D, Hedelin G, Drame M, Jovenin N, Ankri J, et al. Early markers of prolonged hospital stays in older people: a prospective, multicenter study of 908 inpatients in French acute hospitals. J Am Geriatr Soc. 2006;54:1031–9. doi:10.1111/j.1532-5415.2006.00767.x.
Lotus Shyu YI, Chen MC, Lee HC. Caregiver’s needs as predictors of hospital readmission for the elderly in Taiwan. Soc Sci Med. 2004;58:1395–403. doi:10.1016/S0277-9536(03)00334-4.
Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–23.
Saltvedt I, Mo ES, Fayers P, Kaasa S, Sletvold O. Reduced mortality in treating acutely sick, frail older patients in a geriatric evaluation and management unit. A prospective randomized trial. J Am Geriatr Soc. 2002;50:792–8. doi:10.1046/j.1532-5415.2002.50202.x.
Winograd CH, Gerety MB, Chung M, Goldstein MK, Dominguez F Jr, Vallone R. Screening for frailty: criteria and predictors of outcomes. J Am Geriatr Soc. 1991;39:778–84.
Palmer RM. Acute care. In: Hazzard WR, Blass JP, Ettinger WH, Halter JB, Ouslander JG, editors. Principles of geriatric medicine and gerontology. New York: McGraw-Hill; 1999. p. 483–487.
Zuliani G, Romagnoni F, Soattin L, Leoci V, Volpato S, Fellin R. Predictors of two-year mortality in older nursing home residents. The IRA study. Istituto di riposo per anziani. Aging (Milano). 2001;13:3–7.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of adl: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.
Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–8. doi:10.1046/j.1532-5415.2003.51152.x.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi:10.1016/0022-3956(75)90026-6.
American Psychiatry Association. DSM IV, diagnostic and statistical manual mental disorders. 4th ed. Washington: American Psychiatric Association; 1994.
Gilleard CJ, Willmott M, Vaddadi KS. Self-report measures of mood and morale in elderly depressives. Br J Psychiatry. 1981;138:230–5. doi:10.1192/bjp.138.3.230.
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45:735–8.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (mna-sf). J Gerontol A Biol Sci Med Sci. 2001;56:M366–72.
Norton D, Mclaren R, Exton-Smith A. An investigation of nursing problems in hospitals. New-York: Churchill Livingstone; 1975.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New icd-10 version of the charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57:1288–94. doi:10.1016/j.jclinepi.2004.03.012.
Buntinx F, Niclaes L, Suetens C, Jans B, Mertens R, Van den Akker M. Evaluation of charlson’s comorbidity index in elderly living in nursing homes. J Clin Epidemiol. 2002;55:1144–7. doi:10.1016/S0895-4356(02)00485-7.
Heckman J. Dummy endogenous variables in a simultaneous equation system. Econometrica. 1978;46:931–60. doi:10.2307/1909757.
Green DM, Swets JA. Signal detection theory and psychophysics. New-York: Wiley; 1966.
Swets JA, Pickett RM. Evaluation of diagnostic systems: methods from signal detection theory. New-York: Academic Press; 1982.
Metz CE. Receiver operating characteristics methodology in radiologic imaging. Invest Radiol. 1986;21(9):720–33. doi:10.1097/00004424-198609000-00009.
Walter LC, Brand RJ, Counsell SR, Palmer RM, Landefeld CS, Fortinsky RH, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285:2987–94. doi:10.1001/jama.285.23.2987.
Kohn RR. Cause of death in very old people. JAMA. 1982;247:2793–7. doi:10.1001/jama.247.20.2793.
Ponzetto M, Maero B, Maina P, Rosato R, Ciccone G, Merletti F, et al. Risk factors for early and late mortality in hospitalized older patients: the continuing importance of functional status. J Gerontol A Biol Sci Med Sci. 2003;58:1049–54.
Temkin-Greener H, Bajorska A, Peterson DR, Kunitz SJ, Gross D, Williams TF, et al. Social support and risk-adjusted mortality in a frail older population. Med Care. 2004;42:779–88. doi:10.1097/01.mlr.0000132397.49094.b3.
Van Nes MC, Herrmann FR, Gold G, Michel JP, Rizzoli R. Does the mini nutritional assessment predict hospitalization outcomes in older people? Age Ageing. 2001;30:221–6. doi:10.1093/ageing/30.3.221.
Incalzi RA, Capparella O, Gemma A, Landi F, Bruno E, Di Meo F, et al. The interaction between age and comorbidity contributes to predicting the mortality of geriatric patients in the acute-care hospital. J Intern Med. 1997;242:291–8. doi:10.1046/j.1365-2796.1997.00132.x.
Inouye SK, Bogardus ST Jr, Vitagliano G, Desai MM, Williams CS, Grady JN, et al. Burden of illness score for elderly persons: risk adjustment incorporating the cumulative impact of diseases, physiologic abnormalities, and functional impairments. Med Care. 2003;41:70–83. doi:10.1097/00005650-200301000-00010.
Teno JM, Harrell FE Jr, Knaus W, Phillips RS, Wu AW, Connors A Jr, et al. Prediction of survival for older hospitalized patients: the help survival model. Hospitalized elderly longitudinal project. J Am Geriatr Soc. 2000;48:S16–24.
Inouye SK. Delirium in older persons. N Engl J Med. 2006;354:1157–65. doi:10.1056/NEJMra052321.
Roche V. Southwestern internal medicine conference. Etiology and management of delirium. Am J Med Sci. 2003;325:20–30. doi:10.1097/00000441-200301000-00005.
Donini LM, Savina C, Rosano A, De Felice MR, Tassi L, De Bernardini L, et al. Mna predictive value in the follow-up of geriatric patients. J Nutr Health Aging. 2003;7:282–93.
Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, et al. Risk factors for 5-year mortality in older adults: the cardiovascular health study. JAMA. 1998;279:585–92. doi:10.1001/jama.279.8.585.
Frisoni GB, Fratiglioni L, Fastbom J, Viitanen M, Winblad B. Mortality in nondemented subjects with cognitive impairment: the influence of health-related factors. Am J Epidemiol. 1999;150:1031–44.
Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz RI, Concato J. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–93. doi:10.1001/jama.279.15.1187.
Cohen HJ, Saltz CC, Samsa G, McVey L, Davis D, Feussner JR. Predictors of two-year post-hospitalization mortality among elderly veterans in a study evaluating a geriatric consultation team. J Am Geriatr Soc. 1992;40:1231–5.
Ho SC. Health and social predictors of mortality in an elderly Chinese cohort. Am J Epidemiol. 1991;133:907–21.
Lee SJ, Lindquist K, Segal MR, Covinsky KE. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–8. doi:10.1001/jama.295.7.801.
Olsson T, Terent A, Lind L. Rapid emergency medicine score can predict long-term mortality in nonsurgical emergency department patients. Acad Emerg Med. 2004;11(10):1008–13. doi:10.1111/j.1553-2712.2004.tb00667.x.
Acknowledgments
To sources of funding: The French Ministry of Health, funding the Clinical Research Hospital Projects (PHRC 1998); The National Health Insurance Agency for Wage Earners–CNAMTS, France; The Institute of Longevity and Ageing–INSERM, France. To Angela Swaine Verdier for her help with the English draft.
Conflicts of interest declaration
The authors each declare no conflict of interest. The financial sponsors played no role in the design, execution, analysis and interpretation of data, or in writing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dramé, M., Novella, J.L., Lang, P.O. et al. Derivation and validation of a mortality-risk index from a cohort of frail elderly patients hospitalised in medical wards via emergencies: the SAFES study. Eur J Epidemiol 23, 783–791 (2008). https://doi.org/10.1007/s10654-008-9290-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-008-9290-y