Abstract
Objectives To investigate the independent associations between occupational and educational based measures of socioeconomic status (SES) and cause-specific mortality, and the extent to which potentially modifiable risk factors smoking and body mass index (BMI) explain such relationships. Design, setting and participants Prospective population study of 22,486 men and women aged 39–79 years living in the general community in Norfolk, United Kingdom, recruited using general practice age-sex registers in 1993–1997 and followed up for total mortality using death certification to 2006. Main results In men a strong inverse relationship was found between social class and all cause, cardiovascular and cancer mortality, with relative risk of social class V compared to I of 2.21 for all cause mortality (95% CI 1.54–3.17, P < 0.001). This was attenuated but not abolished after adjusting for modifiable risk factors, smoking and BMI, with relative risk of social class V compared to I for all cause mortality of 1.92 (95% CI 1.34–2.77, P < 0.001). A similar, but smaller effect was seen in women. Educational status was not associated with mortality independently of social class. Conclusions Social class and education are not necessarily interchangeable measures of SES. Some but not all of the socioeconomic differential in mortality can be explained by potentially modifiable risk factors smoking and BMI. Further understanding of the mechanisms underlying the association of each socioeconomic indicator with specific health outcomes is needed if we are to reduce inequalities in health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Throughout history socioeconomic status (SES) has been linked with health [1–3], with those of higher SES enjoying better health than those lower down the scale. In spite of the general agreement among experts that SES is complex and multifactorial, the majority of research has focused on the role of one indicator of SES at a time, for example occupational social class [4, 5], education [6–8], or income [9, 10]. Comparisons are made between studies with little consideration given to the measures used to define SES, and it can appear that indicators are treated as interchangeable measures of an underlying entity. More research is now considering the roles of the different indicators separately, however it is still common to examine which specific indicator provides the “optimum” measure of the social gradient in health, often judged to be that with the strongest association [11, 12]. As each indicator measures different, although often related, aspects of SES, this method is unlikely to capture fully the association and may miss the complex pathways through which health inequalities arise. Moreover different indicators may be more or less relevant to different health outcomes at different stages of the life course. Even if different indicators do have a similar relationship with health outcomes, it does not imply that all indicators represent the same causal processes [13]. In order to understand why health inequalities continue to exist despite impressive social and economic health improvements and steadily falling mortality rates, we need to disentangle not ignore the respective contributions of the various SES indicators.
We studied the relations between social class and education and cause-specific mortality in a population of middle-aged men and women. We asked whether any socioeconomic differentials in mortality could be explained by smoking and body mass index (BMI), and whether education and social class were each independently linked to mortality once the other is taken into account. Independent relationships would suggest that each represents somewhat different aetiologic exposures and provide further support for the argument that indicators should not be used interchangeably.
Methods
Participants and measurements
The participants were part of a prospective population study of men and women aged 39–79 years, 99.5% white (as self-defined on questionnaire), resident in Norfolk, United Kingdom. Norfolk is a county that encompasses a wide socioeconomic and urban-rural distribution. The cohort was recruited between 1993 and 1997 from age-sex registers of general practices as part of the Norfolk component of the European Prospective Investigation of Cancer (EPIC-Norfolk) [14]. As virtually 100% of people in the UK are registered with general practitioners through the National Health Service, the age-sex registers form a population-based sampling frame. Detailed descriptions of the study methodology have been reported previously [15]. Approval for the study was obtained from the Norfolk Local Research Ethics Committee. Altogether 30,445 participants gave informed signed consent and completed a detailed health and lifestyle questionnaire. Of these, 25,639 agreed to attend a health examination.
Social class was classified according to the Registrar General’s occupation based classification scheme [16, 17]. Social class I consists of professionals, class II includes managerial and technical occupations, class III is subdivided into non-manual and manual skilled workers (IIInm and IIIm), class IV consists of partly skilled workers, and class V comprises unskilled manual workers (the detailed classification is described elsewhere [17]). For descriptive purposes, the variable was also grouped into non manual classes (classes I, II and IIInm) and manual classes (IIIm, IV and V). For men, social class was coded using their current occupation at the time of survey except when they were unemployed in which case their partner’s social class was used. Last employment was used for men who were retired. Unemployed men without partners were unclassified. Social class in women was based on their partner’s social class except when the partner’s social class was unclassified, missing, or they had no partner, in which case social class was based on their own occupation. An unemployed woman without a partner was coded as unclassified.
Educational status was based on the highest qualification attained and was categorised into four groups: degree or equivalent, A-level or equivalent, O-level or equivalent, and less than O-level or no qualifications. O-level indicates educational attainment to the equivalent of completion of schooling to the age of 15 years and A-level indicates educational attainment to the equivalent of completion of schooling to the age of 17 years. For descriptive purposes educational status was also regrouped into those who finished school (degree or equivalent, A-level or equivalent, O-level or equivalent) and those who did not (less than O-level or no qualifications).
Personal medical history was assessed using the question in the Health and Lifestyle Questionnaire “Has the doctor ever told you that you have any of the following?” followed by a checklist of diseases including myocardial infarction, stroke, and cancer. Yes/no responses to the questions “Have you ever smoked as much as one cigarette a day for as long as a year?” and “Do you smoke cigarettes now?” were used to derive smoking history [18, 19]. Height and weight were measured by trained nurses with participants dressed in light clothing and with their shoes removed [20]. A stadiometer was used to measure height to the nearest 0.1 cm. Salter scales were used to measure weight to the nearest 100 g. Body mass index (BMI) was then calculated as weight (kg)/height2 (m2).
Endpoint ascertainment
All individuals have been flagged for death at the UK Office of National Statistics (ONS). Death certificates are coded by trained nosologists using International Classification of Disease (ICD), revisions 9 and 10. Causes of death were classified as the main underlying cause of death. The categories used were death due to:
-
(i)
all causes,
-
(ii)
underlying cardiovascular disease (CVD),
-
(iii)
cancer,
-
(iv)
all other causes (i.e. non-cardiovascular and non-cancer deaths).
Cardiovascular death was defined as ICD–9 codes 401-448 or ICD-10 codes I10-I79; cancer deaths were defined as ICD-9 codes 140-208 or ICD-10 codes C00-C97.
Statistical analysis
Descriptive statistics including means and percentages are used to show characteristics of the study sample. Two sample t-tests were used to compare differences in mean values, these are two tailed tests. The assumption of equal variances was verified. Differences in percentages were compared using χ2-tests. Analysis of variance was used to obtain mean values of each descriptive variable for each category of SES. Differences in mean total values across the groups were evaluated using F-tests.
Cause-specific rates of mortality were calculated, stratified by social class and by education separately, and χ2-tests for linear trend were used to assess statistical significance. The separate relationships of both social class and education with cause-specific mortality were examined adjusting for potential covariates using Cox’s proportional hazards regression [21]. The proportionality assumption was assessed using Nelson-Aalen plots and by testing for evidence of a statistical interaction with the time scale of the models. There was no evidence of any violation of the proportionality assumption in any models. We examined the relative risks after adjusting for age, smoking and BMI. Wald tests were used to examine the effect of the socioeconomic indicator (social class or education) in each model. Analysing time to an event in a survival analysis gives more power than logistic regression and provides a more accurate model as participants are censored when they die or leave the study, for the purpose of this study follow-up time for an individual began at the date of the first health check. Results will be presented for mortality up to the end of March 2006, about 10 years average follow-up time from the first health check. All statistical analyses will be performed separately for men and women using Stata version 8.0.
Results
Of the 25,639 participants who attended the health check, 570 with no details of their last occupation, and two who had died but had no date of death available were excluded. A further 2,366 participants who reported prevalent heart attack, stroke, and cancer at baseline were excluded to avoid potential reverse causality. Prevalent severe illness, such as coronary heart disease, stroke or cancer is associated both with a higher risk of mortality and may also cause a downward drift in social class, or individuals may be less likely to be upwardly mobile and there is a higher proportion of people with such prevalent illness in lower social classes. Another 215 participants with incomplete data for the covariates BMI and smoking were excluded. This left a total of 22,486 men and women in the current analyses. There were 2,038 deaths during the follow up period (225,537 Person-years), 683 due to CVD, 862 due to cancer and 493 due to other causes.
Descriptive characteristics of the cohort are displayed in Table 1. Men were on average slightly older and had higher BMIs than women. The proportion of current smokers in each sex was similar, a greater proportion of men were former smokers, while a greater proportion of women have never smoked. A much larger proportion of men were educated to O level standard or higher.
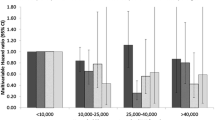
Table 2 shows the characteristics of the participants according to category of social class. Mean age, mean BMI and the percentage of current smokers increased with decreasing social class in both men and women. The percentage of men and women who finished school decreased with decreasing social class. The characteristics of the participants according to level of education are displayed in Table 3. Mean age, mean BMI, the proportion of current smokers and the proportion categorised as manual social class all decreased with increasing educational level in both men and women.
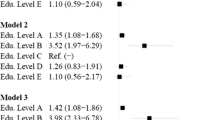
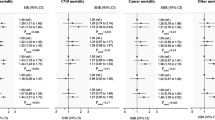
Table 4 shows mortality rates and adjusted relative risks for cause-specific mortality by social class in men and women. In men the age adjusted risk of mortality from all causes, from cardiovascular disease, and from cancer increased with decreasing social class. Adjustment for smoking attenuated the association but the trend was consistent; adjustment for BMI had little effect. Further analyses indicated that this association was independent of education. There was some evidence of an association between mortality from other causes and social class in the adjusted models, however a trend was not clear and the small number of cases gave large confidence intervals. In women trends of increasing risk of mortality from all causes and from cardiovascular disease with decreasing social class were observed, however these were non-significant after adjustment for age. Adjustment for smoking and BMI further attenuated the association. The effect appeared to be smaller than in men. There was no evidence of a relationship between social class and cancer mortality or mortality from other causes in the unadjusted or adjusted models.
Table 5 shows mortality rates and adjusted relative risks for cause-specific mortality by educational level in men and women. In men the risk of all cause mortality and of cardiovascular mortality decreased with increasing educational achievement, this trend was attenuated but consistent after adjusting for smoking, although adjusting for BMI had little effect. After adjustment for social class the association was no longer significant. The risk of mortality from cancer appeared to be lower in men with a degree, but after adjusting for smoking the effect was no longer significant. There was no evidence of an association between level of education and mortality from other causes. In women no association between risk of all cause mortality and education was seen. The risk of cardiovascular mortality in women appeared to decrease with increasing levels of education, similar to the effect seen in men though non-significant. Risk of mortality from cancer appears similar within each educational level. There was no evidence of an association between education and mortality from other causes.
We also examined the social class relation with mortality stratified by educational level but there were no significant differences in the mortality gradient.
Discussion
Social class
How social class affects health outcomes is not well understood. Modifiable lifestyle factors are thought to mediate at least some of the effect [7, 22–24], a theory supported by this study. In men there was strong evidence of an association between social class and mortality from all causes, CVD, and cancer, after adjusting for age. Adjustment for smoking attenuated the association, implying that some of the relationship between social class and mortality can be explained by social class differences in smoking. Differences in BMI explain a small proportion of the association of social class with all cause and with cancer mortality, and a slightly larger proportion of the association with CVD mortality, as indicated by the greater attenuation after adjustment.
There is little debate regarding the need to reduce health inequalities, however the appropriate focus of policies is less clear. Changing individual health behaviours is a key aim in the USA and the UK [24, 25]. However our results and previous research [22, 24, 26, 27] suggest that despite strong socioeconomic differentials in health behaviours, such differences only account for a modest proportion of social inequalities in mortality. Part of the gradient was explained by education, as expected since it strongly affects the type of job people can hold [13, 28, 29], while the remaining independent association implies additional causal processes are at work. Social class reflects experiences and exposures in adult life. It represents the material resources relevant for health and status, as well as aspects relevant to job characteristics, for example psychosocial aspects such as the degree of control over work, or physical risks such as occupational injury, or exposure to toxic substances [28, 30]. Current social class is also strongly related to childhood and parental social class and may well also reflect early life influences. These potential pathways require further investigation.
In women trends of increasing all cause and CVD mortality risk with decreasing social class were seen, which were partially explained by smoking and BMI. The smaller effect might be due to the smaller number of events meaning a lack of power, or this may partly reflect more difficulty in classifying social class in women. There is some controversy over whether a woman’s social class should be graded using her own occupation or that of her husband [31–34]. Studies have shown no clear difference between the two measures in women aged >60, and a stronger association with husband’s social class in women aged 20–59 years [31, 33, 35]. Thus husband’s social class was considered an appropriate classification in this cohort. A weaker socioeconomic mortality gradient in women is consistent with much of the literature [4, 36–40].
Education
Risk of all cause and CVD mortality in men decreased with increasing levels of educational achievement. Some of the education effect was accounted for by smoking and BMI, but a strong effect remained unexplained. Cancer mortality may be lower in men with a degree, an effect partially explained by smoking. In women there was a trend of decreasing risk of mortality from CVD with increasing levels of education; smoking and BMI accounted for very little of this effect. Thus again it appears that only a modest proportion of the mortality gradient was explained by smoking and BMI.
We would expect part of the effects of education to be mediated through social class, however adjustment for social class fully attenuated the association. No independent association between education and all cause or CVD mortality was found, in this cohort all the effects of education appear to be mediated through social class. This supports theories that education’s protective effects work through its long term influence on socioeconomic circumstances in adulthood. Some previous studies have also found that any effects education may have on health are largely explained by other socioeconomic indicators [24, 29, 41]. Whereas others have found an independent association between education and health [8, 13, 30, 42], implying that as well as improving job prospects, education confers additional protective effects, potentially through improved health attitudes and behaviour and a greater ability to utilise health knowledge. Increased education may mean an individual is more receptive to health education messages, either because such messages are written in the language of the educated or because material and cultural resources allow them to adapt to health behaviours more easily. Previous studies have shown that better compliance [43] and a higher commitment to treatment [13] are associated with better education, potentially due to a greater understanding of therapeutic measures.
A recent study has reported changes in the total and independent effects of education and social class on mortality [30]. In a cohort of 40–59 year old Finns, the effects of education on mortality that were mediated by social class increased since the 1970s, while the independent effects declined. It is proposed that such changes are due almost completely to social class differences in mortality increasing at a much greater rate than educational differences in mortality. Such changes might explain the lack of an independent association seen in this cohort, if so this would imply an even more rapid increase in educational differences in mortality in the UK compared to Finland. Given that the SES gradient has been shown to be shallower in more egalitarian countries such as the Scandinavian countries [44], and that these countries have long had health and welfare policies in place that aim to improve public health and reduce social inequalities [45] this might be plausible.
Alternatively many of the cohort were from a wartime generation in whom education was disrupted. Almost half of men completed A-levels, however almost one third did not complete O-levels, and getting a degree was not common. It is possible that the findings reflect the education distribution of this particular generation and may not be easily generalisable to another generation in which education was more universal.
Limitations
This study has a number of limitations. People with medical conditions that could potentially have confounded the relationship between SES and mortality were excluded from the analyses. Prevalent illness, such as CHD, stroke or cancer is associated both with a higher risk of mortality and may also cause a downward drift in social class, or individuals may be less likely to be upwardly mobile. Nevertheless we cannot exclude the possible effect of prevalent subclinical disease, which may explain some of the association between SES and mortality. While we examined how far smoking and BMI might account for some of the socioeconomic differential, we did not examine other potential factors, such psychosocial factors or other lifestyle or physiological factors that explain some of the differences. We recognise the importance of such factors in explaining the socioeconomic differential, but wished to confine our analyses to examining the influence of the two main accepted modifiable behaviours, smoking and BMI, on the socioeconomic differential in mortality.
Mortality was ascertained using a regular record linkage system with national deaths registration. We do not have the resources to do a validation study of the accuracy of the cause of death in our death certificate data. However, mortality registries are recommended as a key source of data for studying health inequalities [46], and this method is one of the most frequently used in epidemiological studies. The cause-specific coding of death may have some error [47, 48], however the main focus of this paper was total mortality, for which the data are virtually complete in Britain. Education and occupation details were obtained at the baseline survey between 1993 and 1997. Some degree of inaccuracy in reporting or recording this information is inevitable, however it seems unlikely that misclassifications would be non-random. Normally random measurement error is likely only to attenuate any relationships, not produce spurious relationships [49]. Although it has been shown that there are some situations where random misclassification can bias effect measures for misclassified multi-level exposures away from or beyond the null [50], we do not expect the misclassification patterns in our data to be of sufficient magnitude to explain our results.
The socioeconomic differentials in mortality are not as wide as have been reported in other studies. This may reflect attenuation due to misclassification of social class and/or educational status as discussed. Alternatively, it is possible that in Norfolk the socioeconomic differentials may reflect less variation in lifestyles such as diet and physical activity than in more urban environments.
EPIC-Norfolk is composed of participants willing to complete detailed questionnaires and attend health checks, and the response rate was quite low at about 45% [51], thus selection bias may be a problem if non response was associated with social class or with health status given a certain social class. It is possible that we may have selected a particularly health conscious study cohort, particularly in the lower social classes, and thus there may be some attenuation of the socioeconomic differential in our results. However the range of socioeconomic circumstances of the participants was wide [16, 52], and in terms of anthropometric variables, serum lipids and blood pressure [15] and of physical and mental functional health [53], the cohort was similar to the general resident population in England, although there were fewer current smokers. Selection of a more health conscious cohort would mean that the external generalisability of the study results may be affected, but the internal validity of the study results should not be affected. Excluding those with unclassified or missing data for SES or mortality could cause bias, but only if these people differed from those included in the study with respect to the relation between SES and mortality, which seems unlikely.
Conclusions
Social class and education are not necessarily interchangeable measures of SES. Some but not all of the socioeconomic differential in mortality can be explained by potentially modifiable risk factors smoking and BMI. Further understanding of the mechanisms underlying the association of each socioeconomic indicator with specific health outcomes is needed if we are to reduce inequalities in health.
Abbreviations
- BMI:
-
Body mass index
- EPIC-Norfolk:
-
European Prospective Investigation of Cancer and Nutrition
- SES:
-
Socioeconomic status
References
Deaton A. Policy implications of the gradient of health and wealth. An economist asks, would redistributing income improve population health? Health Aff. 2002;21(2):13–30.
Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, et al. Socioeconomic status and health: the challenge of the gradient. Am Psychol. 1994;49(1):15–24.
Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18(1):341–78. doi:10.1146/annurev.publhealth.18.1.341.
Gregorio DI, Walsh SJ, Paturzo D. The effects of occupation-based social position on mortality in a large American cohort. Am J Public Health. 1997;87(9):1472–5.
Kunst AE, Groenhof F, Mackenbach JP. EU working group on socioeconomic inequalities in health, Leon DA. Occupational class and cause specific mortality in middle aged men in 11 European countries: comparison of population based studies. BMJ. 1998;316(7145):1636–42.
Elo IT, Preston SH. Educational differentials in mortality: United States, 1979–1985. Social Sci Med. 1996;42(1):47–57.
Schrijvers CT, Stronks K, van de Mheen HD, Mackenbach JP. Explaining educational differences in mortality: the role of behavioral and material factors. Am J Public Health. 1999;89(4):535–40.
Ross C, Wu C. The links between education and health. Am Sociol Rev. 1995;60(5):719–45. doi:10.2307/2096319.
Ecob R, Davey Smith G. Income and health: what is the nature of the relationship? Social Sci Med. 1999;48(5):693–705.
Rahkonen O, Arber S, Lahelma E, Martikainen P, Silventoinen K. Understanding income inequalities in health among men and women in Britain and Finland. Int J Health Serv. 2000;30(1):27–47. doi:10.2190/VBJT-5LFB-62Y0-4Y29.
Davey Smith G, Hart C, Hole D, MacKinnon P, Gillis C, Watt G, et al. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998;52(3):153–60.
Duncan GJ, Daly MC, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92(7):1151–7.
Geyer S, Hemstrom O, Peter R, Vagero D. Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. J Epidemiol Community Health. 2006;60(9):804–10.
Riboli E, Kaaks R. The EPIC project: rationale and study design European prospective investigation into cancer and nutrition. Int J Epidemiol. 1997;26(Supplement 1):S6–14.
Day N, Oakes S, Luben R, Khaw KT, Bingham S, Welch A, et al. EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer. 1999;80(Suppl 1):95–103.
Shohaimi S, Luben R, Wareham N, Day N, Bingham S, Welch A, et al. Residential area deprivation predicts smoking habit independently of individual educational level and occupational social class. A cross sectional study in the Norfolk cohort of the European Investigation into Cancer (EPIC-Norfolk). J Epidemiol Community Health. 2003;57(4):270–6.
Elias P, Halstead K, Prandy K. CASOC: computer-assisted standard occupational coding. London: HMSO; 1993.
Smith MR, Kinmonth A-L, Luben RN, Bingham S, Day NE, Wareham NJ, et al. Smoking status and differential white cell count in men and women in the EPIC-Norfolk population. Atherosclerosis. 2003;169(2):331–7.
Sargeant L, Wareham N, Bingham S, Day N, Luben R, Oakes S, et al. Vitamin C and hyperglycemia in the European Prospective Investigation into Cancer-Norfolk (EPIC-Norfolk) study: a population-based study. Diabetes Care. 2000;23(6):726–32.
Sargeant LA, Khaw K-T, Bingham S, Day NE, Luben RN, Oakes S, et al. Cigarette smoking and glycaemia: the EPIC-Norfolk study. Int J Epidemiol. 2001;30(3):547–54.
Cox DR. Regression models and life tables. J R Stat Soc (B). 1972;34:187–220.
Bucher HC, Ragland DR. Socioeconomic indicators and mortality from coronary heart disease and cancer: a 22-year follow-up of middle-aged men. Am J Public Health. 1995;85(9):1231–6.
Vescio M, Davey Smith G, Giampaoli S. Socio-economic-position overall and cause-specific mortality in an Italian rural population. Eur J Epidemiol. 2003;18:1051–8. doi:10.1023/A:1026121620501.
Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen J. Socioeconomic factors, health behaviors, and mortality: results from a nationally representative prospective study of US adults. JAMA. 1998;279(21):1703–8.
Department of Health. Tackling Health Inequalities: Status Report on the Programme for Action; 2005 11th August 2005 Gateway reference, 3835. Product Number, 267589. Series No. Cm6374.
Zajacova A. Education, gender, and mortality: does schooling have the same effect on mortality for men and women in the US? Social Sci Med. 2006;63(8):2176–90.
Steenland K, Henley J, Thun M. All-cause and cause-specific death rates by educational status for two million people in two American Cancer Society cohorts, 1959–1996. Am J Epidemiol. 2002;156(1):11–21.
Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff. 2002;21(2):60–76.
Lahelma E, Martikainen P, Laaksonen M, Aittomaki A. Pathways between socioeconomic determinants of health. J Epidemiol Community Health. 2004;58(4):327–32.
Martikainen P, Blomgren J, Valkonen T. Change in the total and independent effects of education and occupational social class on mortality: analyses of all Finnish men and women in the period 1971–2000. J Epidemiol Community Health. 2007;61(6):499–505.
Arber S, Ginn J. Gender and inequalities in health in later life. Social Sci Med. 1993;36(1):33–46.
Arber S, Lahelma E. Inequalities in women’s and men’s ill-health: Britain and Finland compared. Social Sci Med. 1993;37(8):1055–68.
Martikainen P, Kauppinen TM, Valkonen T. Effects of the characteristics of neighbourhoods and the characteristics of people on cause specific mortality: a register based follow up study of 252 000 men. J Epidemiol Community Health. 2003;57(3):210–7.
Krieger N, Chen J, Selby J. Comparing individual-based and household-based measures of social class to assess class inequalities in women’s health: a methodological study of 684 US women. J Epidemiol Community Health. 1999;53(10):612–23.
Arber S. Class, paid employment and family roles: making sense of structural disadvantage, gender and health status. Social Sci Med. 1991;32(4):425–36. doi:10.1016/0277-9536(91)90344-C.
Bopp M, Minder CE. Mortality by education in German speaking Switzerland, 1990–1997: results from the Swiss National Cohort. Int J Epidemiol. 2003;32(3):346–54.
Koskinen S, Martelin T. Why are socioeconomic mortality differences smaller among women than among men? Social Sci Med. 1994;38(10):1385–96.
Mackenbach JP, Kunst AE, Groenhof F, Borgan JK, Costa G, Faggiano F, et al. Socioeconomic inequalities in mortality among women and among men: an international study. Am J Public Health. 1999;89(12):1800–6.
Manor O, Eisenbach Z, Israeli A, Friedlander Y. Mortality differentials among women: the Israel Longitudinal Mortality Study. Social Sci Med. 2000;51(8):1175–88.
Stronks K, van de Mheen H, van den Bos J, Mackenbach JP. Smaller socioeconomic inequalities in health among women: the role of employment status. Int J Epidemiol. 1995;24(3):559–68.
House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Social Behav. 2001;43(June):125–42.
Miech RA, Hauser RM. Socioeconomic status and health at midlife: a comparison of educational attainment with occupation-based indicators. Ann Epidemiol. 2001;11(2):75–84.
Goldman DP, Smith JP. Can patient self-management help explain the SES health gradient? PNAS. 2002;99(16):10929–34.
Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Ann NY Acad Sci.. 1999;896(1):3–15.
Lahelma E, Manderbacka K, Rahkonen O, Karisto A. Comparisons of inequalities in health: evidence from national surveys in Finland, Norway and Sweden. Social Sci Med. 1994;38(4):517–24.
Kunst AE, Mackenbach JP. Measuring socioeconomic inequalities in health; 2000 Document Number, EUR/ICP/RPD 416.
Lauer MS, Blackstone EH, Young JB, Topol EJ. Cause of death in clinical research: Time for a reassessment? J Am Coll Cardiol. 1999;34(3):618–20.
Lenfant C, Friedman L, Thom T. Fifty years of death certificates: the framingham heart study. Ann Intern Med. 1998;129(12):1066–7.
Flegal KM, Brownie C, Haas J. The effects of exposure misclassification on estimates of relative risk. Am J Epidemiol. 1986;123(4):736–51.
Dosemeci M, Wacholder S, Lubin JH. Does nondifferential misclassification of exposure always bias a true effect toward the null value? Am J Epidemiol. 1990;132(4):746–8.
Myint PK, Luben RN, Surtees PG, Wainwright NWJ, Welch AA, Bingham SA, et al. Relation between self-reported physical functional health and chronic disease mortality in men and women in the European Prospective Investigation Into Cancer (EPIC-Norfolk): a prospective population study. Ann Epidemiol. 2006;16(6):492–500.
Wainwright NWJ, Surtees PG. Places, people, and their physical and mental functional health. J Epidemiol Community Health. 2004;58(4):333–9.
Surtees PG, Wainwright NW, Khaw KT. Obesity, confidant support and functional health: cross-sectional evidence from the EPIC-Norfolk cohort. Int J Obes Relat Metab Disord. 2004;28(6):748–58. doi:10.1038/sj.ijo.0802636.
Acknowledgments
We thank the participants and general practitioners who took part in the study and the staff of EPIC-Norfolk. Funding: EPIC-Norfolk is supported by research programme grant funding from the Cancer Research Campaign and Medical Research Council with additional support from the Stroke Association, British Heart Foundation, and Research Into Ageing. Contributors: KTK, SB, and NW are principal investigators in the EPIC-Norfolk population study. SB is responsible for the dietary measurements and analyses. RL is responsible for data management and computing and data linkages for post coding. EM conducted the data analyses and wrote the paper with KTK with contributions from other coauthors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McFadden, E., Luben, R., Wareham, N. et al. Occupational social class, educational level, smoking and body mass index, and cause-specific mortality in men and women: a prospective study in the European Prospective Investigation of Cancer and Nutrition in Norfolk (EPIC-Norfolk) cohort. Eur J Epidemiol 23, 511–522 (2008). https://doi.org/10.1007/s10654-008-9267-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-008-9267-x