Abstract
Environmental pollution in many regions of Kazakhstan poses a threat to the growth and development of local children. For children living the near the Aral Sea, chrome processing and gas processing regions, we undertook a medical examination, including physical and sexual development parameters, laboratory studies (complete blood count, urinalysis, blood chemistry), bone age, blood levels of microelements (chromium, manganese, nickel, lead, copper) and hormones [thyroid (T3, T4, TSH), sexual (LH, FSH), growth (STH, IGF-1)], in consultation with relevant specialist doctors. Statistical analysis showed a significant prevalence of short stature among children living, on average, 22.9 versus 7.8% in the control region. Children in these regions have high blood levels of toxic chromium, manganese, lead and nickel compounds. The main causes of short stature in children living in the Aral Sea, chrome processing and oil and gas processing regions are cerebral–endocrine pathologies, hereditary diseases, somatogenic diseases, constitutional growth delay, a toxic chemical load and ecologically determined short stature. A working classification of short stature in children living in the Aral Sea, chrome processing and gas processing regions, including ecologically dependent short stature, has been developed. The scheme of medical and recreational measures for children living in the Aral Sea, chrome processing and gas processing regions was proposed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intensive use of rich natural deposits of chrome and nickel ores, phosphates, oil, gas and other natural resources over the past 50 years in the West Kazakhstan region has led to the environmental tension. Anthropogenic environmental pollution in many regions of Kazakhstan creates a tense ecological situation that poses a potential danger to public health, primarily for the growth and development of children. Chrome compounds, which cause polytropic damage, present extreme ecological danger: carcinogenic, mutagenic, embryo- and gonadotoxic and other negative effects (Avtsyn et al. 1991; Karimov and Shkolbulova 2008; Bermagambetova et al. 2008; Iztleuova et al. 2009; Mukyshova et al. 2009; Kuchma 2002). The planned reduction in the levels of human exposure to chemical compounds and shutdown of some mining and processing industries contributed to the emergence of the problem of the effects of small concentrations of chemical compounds on public health in modern hygiene science. These unfavorable factors interfere with growth and development of children, as well as their body functions, which due to anatomical and physiological characteristics are still imperfect, unstable and may be easily disrupted during this period (Revich et al. 2004; Vitebskaya 2007; Sharova et al. 2006; Zhumalina et al. 2008).
Therefore, special attention is paid to healthcare activities aimed at the improvement in the system for active public health monitoring focused on children and adolescents who live in the regions contaminated with chrome compounds, as well as oil and gas products. Physical development is the most important integral indicator of public health, including children population of the country. Studies of physical development of children in the oncoming global environmental pollution become an urgent problem not only for Kazakhstan, but for the entire world community. In this connection, studies of the mechanisms of short stature formation in children require the development of methods for early diagnosis of short stature due to environmental factors.
Short stature is a term applied to a child whose height is 2 standard deviations (SD) or more below the mean for children of that sex and chronologic age (and ideally of the same racial–ethnic group). This corresponds to a height that is below the 2.3 percentile. It should be noted that to date there are no methods for early diagnosis of short stature in children who live in the regions contaminated with chrome compounds, as well as oil and gas products.
Growth and development are significantly affected by endocrine disorders (Lyalikov and Lyalikova 2008; Bukina et al. 2007; Vasiliev 2005; Uzunova et al. 2008; Sobolev et al. 2007; Bobak and David 1999; Cowveina et al. 2004; Liu et al. 2003). Constitutional growth and puberty are closely interconnected, the morphological and functional relationships of which are explained by a single hypothalamic–pituitary regulation (Zhukovsky 1982; Blunk 1981). Numerous clinical observations confirm this statement. Therefore, the development of new programs for timely diagnosis, treatment and prevention of environmentally determined growth delay in children living in ecologically unfavorable regions is an extremely urgent task (Bayevsky 1990).
A systemic approach that includes a comprehensive study of physical development of schoolchildren to identify the causes and mechanisms of short stature in children who live in the regions contaminated with chrome compounds, as well as oil and gas products, is a promising area of health care of the younger generation of our country and therapeutic, preventive and rehabilitation care.
Study purpose: To develop scientifically justified proposals on the prevention and treatment of environmentally determined constitutional growth delay in children in the West Kazakhstan region.
Objectives of the study:
-
1.
To study the prevalence of growth delay in children who live in the regions contaminated with chrome compounds, as well as oil and gas products.
-
2.
To establish a relationship between the level of environmental pollution and physical development of schoolchildren.
-
3.
To investigate clinical and pathogenetic mechanisms of short stature formation in children living in the Aral Sea, chrome processing and gas processing regions.
-
4.
To develop an algorithm for early diagnosis, treatment and prediction of short stature in children living in the Aral Sea, chrome processing and gas processing regions.
The experiments were carried out in accordance with the requirements of the European Convention for the Protection of Vertebrate Animals used for Experimental and Other Scientific Purposes (Strasbourg 1986) and were approved by the Ethics Committee of the West Kazakhstan Marat Ospanov State Medical University.
Clinical characteristics and study methods
In accordance with the goals and objectives of the study, the examination was carried out in stages.
Stage 1. The in-depth examination program included a detailed history survey using questionnaires, personal examination and follow-up: antenatal and postnatal periods, history of diseases, analysis of family history including age of parents at child’s birth, duration of residence in a particular region, parents’ height, familial endocrine and somatic diseases and social conditions of children (day regimen, nutrition, family size, bad habits, quality of housing, etc.).
Stage 2. Parameters of physical development, functional status and health of children and adolescents were studied:
-
(a)
identification of children with growth delay;
-
(b)
hormonal studies (T3, T4, TSH, LH, FSH, STH), blood levels of microelements;
-
(c)
assessment of bone age;
-
(d)
ultrasound examination of the thyroid gland.
Stage 3. Development of a clinical and laboratory method for early diagnosis and prediction of short stature in children living in the Aral Sea, chrome processing and gas processing regions.
To study constitutional growth in children, anthropometric measurements (height and body weight) using a unified technique developed by the M.V. Lomonosov Institute of Anthropology and described in detail by Bunak (1941), Stavitskaya and Aron (1959) were used. The instruments included a wooden vertical scale and floor scales. The studies were conducted in the morning (on an empty stomach). The height was measured in a standing position, the measurement accuracy was 0.5 cm, and weighing was carried out using a precalibrated scales. Accuracy of measurement of body weight was ± 50 g.
The examination included standard clinical and laboratory methods of investigation: complete blood count (hemoglobin, erythrocytes, leukocytes, color index, erythrocyte sedimentation rate) and urinalysis according to the standard method; biochemical studies of plasma proteins, urea and creatinine were carried out according to indications; instrumental methods were used to study respiratory organs, digestive and urinary systems; consultations of specialists include neurologist, ophthalmologist, otolaryngologist, endocrinologist, orthopedist according to indications.
To establish “bone age” (BA), X-rays of the hands including wrist joints were carried out due to the presence of numerous nuclei of ossification and epiphyseal areas in this part of the skeleton. BA was estimated according to data of Perepust (1977); BA parameters were calculated (ossification factor—the ratio between bone and passport age)—the ratio between growth and radiographic age (Perepust 1977). Blood plasma was studied for the levels of thyroxine (T4), triiodothyronine (T3), thyrotropin (TSH), follicle-stimulating hormone (FSH) and luteinizing hormone (LH) using enzyme-linked immunoassay(ELISA) using the Vector Best kit produced by DRG (USA). Blood was collected in the morning, on an empty stomach, between 7 and 10 o’clock.
Statistical data processing was carried out using the SAS program, version 9.2. Normality of distribution was estimated using the Kolmogorov–Smirnov test. The results of the study are presented as means (M) and standard deviation (SD). To assess the statistical significance of the differences, a two-sample t test with unequal variances (t) was used. Test results with P ≤ 0.05 were considered statistically significant. This study was conducted in accordance with the international requirements of good clinical practice (GCP).
Results and discussion
Schoolchildren (7–17 years old) living in the ecologically favorable area (Kobda) were examined as a control group. The design of a cohort prospective study is presented in Table 1.
The analysis of the comparative results of the study showed that the constitutional growth of children living in the regions studied has its own characteristics, first of all, quantitative discrepancies. The statistical analysis of the constitutional growth of children in terms of anthropometric data showed that the absolute values of mean height and body weight in boys increase throughout the entire length of the ontogenesis studied.
Thus, in boys from 7 years, height increases from 119.0 to 163.7 cm. The average annual increase in height is 4.1 cm. In children of the control group, during this period, height increases from 121.9 to 171.1 cm, and the average annual increase is 4.5 cm. However, in boys from the studied regions, the maximum height increase is observed at the age of 12 years and is on average 6.9 cm. The same maximum increase in height in boys of the control group is observed at the age of 14 years and is on average 9.9 cm. The same pattern is observed for the increase in the body weight of boys. Thus, body weight of the control group increases from 23.5 kg at the age of 7 years to 65.9 kg by 17 years; the average annual increase is 3.9 kg. In boys of the studied regions, this parameter varies from 20.0 to 59.0 kg, and the average annual increase is 3.6 kg. In boys from the control group, the maximum annual body weight gain occurs at the age of 14 years, similar to height, and is on average 9.5 kg per year. The maximum annual body weight gain in boys from the studied regions coincides with the maximum height increase, i.e., at the age of 12 years and is 6.2 kg per year.
In girls from the control group, height is 122 cm at the age of 7 years and 164 cm by 17 years; on average, the average increase in height is 3.8 cm per year. The maximum annual increase was registered at the age of 11 years and is 7 cm per year. In girls from the studied regions, height increases from 118.0 to 159.4 cm, and the average height increase is 3.8 cm per year, with a maximum increase at the age of 11 years, similar to girls from the control group, by 6.0 cm. The increase in body weight in girls occurs throughout the entire study period and is 23.3 kg in the control group at the age of 7 years and 56.6 kg by 17 years. The average increase in body weight is 3.0 kg, with a maximum annual increase at the age of 11.8 years by 5.8 kg. In girls from the studied regions, body weight increases from 18.0 to 51.4 kg, and the average weight gain is 3.0 kg, with a maximum increase at the age of 12 years by 5.6 kg.
The first intersection of the height curves in boys and girls from the studied regions is observed at the age of 12 years, whereas in the control group it is observed at the age of 9 years. The second intersection in girls and boys is observed at the age of 15 years and around 13–14 years in the control group. The first intersection of the body weight curves of the studied segment in children of the control group is observed at the age of 9–10 years, and in children living in the studied regions in both groups—also at the age of 9 years.
As for the absolute values of the mean chest size, we have found the maximum increase in the growth rate in girls at the age of 12–13 years, i.e., 6.7 cm in girls of the control group and 4.9 cm per year in the study group, while the average annual increase is 2.1 cm, similar to the control group. In boys, the average annual increase in chest circumference is 1.7 cm regardless of their residence. The maximum increase in chest circumference in boys is observed at the age of 12–13 years, similar to girls, but the increase in size is somewhat lower and is 3 cm in boys and 3.6 cm in boys from Kobda.
In summary, the results of a comparative analysis of the main parameters of constitutional growth in children from different regions of residence confirm that the current environmental conditions in the regions studied have an adverse effect on the growth and development of children. Epidemiological parameters which reflect chances, risks and relationships include:
-
chance of disease among the exposed, in this case, to ecological impact—A/B, 145/487 = 0.297;
-
• chance of disease among those who were not exposed—C/D, 48/573 = 0.083;
-
odds ratio OR reflects risks (A/B)/(C/D); 0.297/0.083 = 3.578, therefore > 1, which shows a positive relationship;
-
incidence disease ratio IDR = ID among the exposed (IDe)/ID among the non-exposed (IDo) = (A/A + B)/(C/C + D); (145/145 + 487)/(48/48 + 573) = 0.850;
-
Associated risk (AR) shows an excessive risk of the disease compared to those who have not been exposed (AR = Ie-I0). AR assumes a causative relationship; AR = 0.297–0.083 = 0.214 > 0; AR > 0 shows number of cases absent in the absence of the risk factor;
-
percentage of the associated risk—associated risk expressed in % is also known as associated level percentage or associated proportion [AR/Ie × 100 = (Ie − I0)/Ie] 0.214/0.297 × 100 = 72.05%;
-
population associated risk (PAR) measures the excess level of disease in the general population of exposed and non-exposed subjects which is associated with exposure.
$${\text{PAR}} = \frac{{{\text{IT}} {-} I_{0} }}{\text{IT}} = \frac{{0.154 {-} 0.083}}{0.154} = \, 0.461$$(1)where IT = ratio of the total number of patients suffering from the disease to the number of patients with and without disease
$${\text{IT}} = \frac{193}{1253} = 0.154.$$(2)
Multivariate analysis of anamnestic data of children living in the Aral Sea, chrome processing and gas processing regions
The authors have analyzed the anamnestic data of children living in the Aral Sea, chrome processing and gas processing regions. The analysis of development histories (n. 112) and information received from children and parents showed that all subjects were born and resided permanently in the regions studied.
The age of the parents at the time of child’s birth ranged from 16 (1 case) to 43 years in the mothers and from 21 to 51 in the fathers, which does not differ from the average figures in the population. The average age of mothers is 25.7 years, fathers—27.3 years. According to data on the health of parents, it was found that 153 mothers and 185 fathers were healthy. The rest had different pathologies. And the number of unhealthy mothers increased from 43.1 to 60.5%, respectively. 51.2% of children were born in the 1st pregnancy, 24.4% in the second pregnancy, 24.1% in the third and more; 58.7% were born in the 1st labor, 32% in the 2nd, 9.3% in the 3d and more; pregnancy was normal in 57.2% of mothers, delivery in 62%.
The frequency of perinatal pathological factors in children (unfavorable outcome of a previous pregnancy, toxicosis and threat of abortion, pathological labor: premature, rapid, with stimulation, breech presentation and others; asphyxia, birth trauma and neonatal diseases) was analyzed. With an increase in the degree of GD (growth delay), the proportion of children with perinatal pathology increased from 53 ± 6 to 71 ± 5% (P < 0.05). The number of perinatal factors was 1.69 to 2.01, respectively.
For better characterization of children, we analyzed their anthropometric parameters by the time of delivery. Data of Dementieva et al. (1984) were considered normal means (M ± 1δ) of body length and weight of full-term newborns, according to which body length of 49.5–53.5 cm and body weight of 3100–4000 g are average, > 54 cm and > 4100 g labor above average and < 49 cm and < 3000 g labor below average. As the data refer to full-term newborns, only full-term newborns were included in the study, especially as there were only 10 premature newborns in the group. A retrospective analysis showed that the average body length and body weight at birth were 326 (51.3%) and 384 (60.5%), respectively, 285 (44.9%) and 244 (38.5%) below average, 24 (3.8%) and 6 (1%)above average. Consequently, more than one-third of children at birth had body length and body weight values below average.
Table 2 shows mean length and body weight of the whole group, depending on the degree of GD. Parameters of constitutional growth in the control group of Kobda were considered controls. The analysis showed that the average body length and weight of newborns are significantly lower than those in the control group (P < 0.05). The values of the length–weight coefficient in GD did not differ significantly from the control. However, it should be noted that with the increase in GD degree, number of children with values of this coefficient above normal increased. The analysis of feeding showed that 66% of children were on natural feeding, including up to 1 year—20%, 7.2% were breastfed up to 2 years or longer, and 28% of children received early formula feeding.
Therefore, summarizing the results of the anamnestic study in three regions, it should be noted that children had a fairly high degree of perinatal risk, as evidenced by a high incidence of extragenital pathologies and complications of pregnancy and childbirth. The analysis of disease incidence in children of the first year of life showed that 20.5% suffered from rickets, 10.5% had hypotrophy and 34.5% had anemia. Rickets was more often detected in boys (58%). Half of the children had rickets at the age of 7–9 months. In children who were breastfed, rickets was detected in 25% of cases, and in children who received formula feeding rickets was detected in 42% of cases. Hypotrophy was observed in 10.5% of cases. In general, incidence in girls was higher (51.2%). Therefore, a high incidence of underlying diseases (66%), as well as infectious and ENT pathologies (65.2%), was characteristic features of postnatal history. Children on formula feeding had higher rates of underlying diseases (do Nascimento et al. 2018).
Clinical and functional parameters in children with short stature living in the Aral Sea, chrome processing and gas processing regions
We conducted a survey of children’s complaints. Children’s complaints are difficult to assess objectively, as some children presented complains independently, willingly, extensively and almost professionally, which is obviously associated with frequent visits to doctors, but most children only answered questions and not always reliably. After the survey, it was found that 133 (19%) children from the Aral Sea region, 138 (18.5%) from Aktobe and 125 (26%) from Zhanazhol had respiratory complaints: difficult nasal breathing, nasal discharge, cough and sputum. A large percentage of children from Aktobe 226 (30.2%), less from the Aral Sea region 140 (20%) and 91 (19%) from Zhanazhol had cardiovascular complaints: heartache, palpitations, joint pain. Complaints of abdominal pain, nausea, poor appetite, heartburn, pain in the right hypochondrium, propensity to constipation were observed in all three regions, respectively (28%, 30%, 26%). 49 (7%) children from Aktobe, 39 (6.1%) from the Aral Sea region and 22 (5.0%) from Zhanazhol reported pain in the lower back. In addition, it should be noted that, despite obvious pathologies of the skin, respiratory system, cardiovascular and digestive systems, part of the children, namely 25%, did not have complaints, which indicates that their symptoms had become and were perceived as a natural “normal” state. At the first level of examination, functional pathologies of systems and organs, skin, endocrine system or musculoskeletal system are not usually determined. At the second and third level of examination, an in-depth clinical study of children was conducted with the involvement of specialists and laboratory–instrumental diagnostic methods.
The analysis of changes in the skin and mucous membranes showed that the most common clinical symptoms were pallor in 68.3% of children, dryness and desquamation in 54.2%, scratching (12%), lichenization (11.2%), angular cheilitis (9.6%), geographic tongue (13.1%) and dry lips (22%). A fairly high prevalence of skin symptoms that are not considered characteristic for children, pigment metabolism disorder in 5.7%, especially in children living in the Aral Sea region, should be noted. 12.1% had hypertrichosis, and 9.2% had trophic nail disorders.
The frequency of musculoskeletal disorders was high. In 9.2% of children, the tone of the muscles of the anterior abdominal wall was reduced; 19.7% had deformations of the chest (the ratio between antero-posterior and lateral dimensions), which may be a manifestation of the history of rickets; 1.5% had camptomelia. The prevailing musculoskeletal pathology was impaired posture in 22.6% of children.
All children underwent an external respiration function test using a pneumotachometer. The analysis showed that 20.9% of children living in the Aral Sea and chrome processing region had ventilatory insufficiency, which was more expressed in children living in Zhanazhol (24.1%). The majority of the examined children (60.1%) had obstructive ventilatory insufficiency, which is caused by bronchospasm, respiratory mucosal edema, hypersecretion of mucus and impaired elasticity of the lung tissue. In Zhanazhol, obstructive ventilatory insufficiency was found in children (25%) with relapsing obstructive bronchitis, but in 75% of children, who had no bronchopulmonary pathology, it could be caused by a decrease in vital capacity (VC) as a result of decreased chest wall complexity due to its deformation and impaired posture.
Despite the fact that children did not complain, they had extensive respiratory symptomatology which in some cases confirmed the presence of pathology and in a number of children it was the basis for diagnosis that had not been previously established. In addition to objective examination and spirography, the diagnosis of the upper respiratory tract was based on the examinations of children by the otolaryngologist, which provided local diagnosis of the pathological process and, to a certain extent, allowed differentiation between allergic and inflammatory processes of the upper respiratory tract.
It should be noted that the highest percentage of cardiovascular changes were observed in children living near chrome processing plants. Cardiovascular disorders included changes in heart rate, with predominant tachycardia in 10.2% and bradycardia in 3.1%. Abnormal blood pressure (BP) was observed in 10.5% of children, mainly lower blood pressure in 9.1% and a slight increase in 1.4% of children. Auscultatory, 20% of children had changes in the heart tones in the form of muffled heart tones.
Changes in the ECG were observed in 30.1% of children, mainly in the form of sinus tachycardia, dysmetabolic changes in the myocardium and blockades at various levels. Echocardiography was performed in children with clinical symptoms of cardiovascular disorders and changes in the ECG. Three (0.42%) children from the Aral Sea region and Aktobe were diagnosed with congenital heart disease, and in Zhanazhol the diagnosis of congenital heart disease was confirmed in 2 (0.41%) children.
The analysis of the digestive system and oral cavity showed that 75% of children had furred tongue, most often covered with white fur, mainly at the root, sometimes of grayish color. 50% of children had tenderness in the epigastric region, and 12% had tenderness along the bowel or in the navel. After fibrogastroscopy, diagnoses were established and confirmed: For the Aral Sea region, in 2 (0.41%) children liver enlargement was observed and the diagnosis of chronic persistent hepatitis was confirmed; in 11 (1.56%) children, a combined pathology of the digestive system and chronic nasopharyngeal pathology was observed; in Aktobe 1 child had a malformation of the large intestine, 8 (1.06%) children had chronic gastroduodenitis, and 5 (0.66%) children had a combined pathology of the digestive system and chronic nasopharyngeal pathology; in Zhanazhol 10 (2.07%) children were primarily diagnosed with chronic gastroduodenitis and 4 (0.82%) children had combined pathology of the digestive system and chronic nasopharyngeal pathology. At objective examination, 4.5% of children had pastose eyelids. The ultrasound examination of the urinary system confirmed the diagnosis in 5 children.
All children were examined by an endocrinologist, and the analysis of the pathology of the endocrine system showed lower rates of occurrence in younger school children, which may be related to the characteristics of pubertal age. The occurrence of enlarged thyroid gland and hypothalamic dysfunction in older school children increases by a factor of 2. In the Aral Sea region, 6 (0.85%) children had hypothyroidism, 1(0.14%) child had a growth hormone deficiency, and 1(0.14%) child had thymic hyperplasia II; in Aktobe, hypothyroidism was newly diagnosed in 5 (0.66%) children, growth hormone deficiency in 2 children (0.26%) and thymic hyperplasia II in 1 (0.14%) child; in Zhanazhol, 4 (0.82%) children had hypothyroidism and 1(0.20%) child had immune deficiency.
To fully characterize the processes of growth and sexual development of children, data on the radiographic age were analyzed. In the Aral Sea region, the radiologic age was analyzed in 340 children, in the chrome processing region (Aktobe) in 385 children and in the gas processing region (Zhanazhol) in 328 children. Most of them showed delayed ossification. In the Aral Sea region, ossification corresponded to the passport age in 213 (62.5%) children and was delayed for not more than 2 years in 110 (32.5%) children and more than 2 years in 17 (5%) children; in Aktobe, respectively, it was normal in 252 (65.5%), delayed in 120 (31.1%) and delayed for more than 2 years in 13 (3.4%) children; in Zhanazhol, in 198 (60.4%) children it corresponded to the passport age, in 114 (34.9%) it was delayed for not more than 2 years and in 16 (4.7%) for more than 2 years. It should be noted that in the studied regions, a significant degree of ossification (> 2 years) was less common in girls (31.6 and 68%, respectively), compared to boys.
Laboratory results in the studied groups of children
Impaired function of endocrine glands in a growing organism significantly influences its growth and development, which requires investigation of this problem in children with delayed constitutional growth. Somatotropic hormone of the pituitary gland (its levels increase after 3 years and decrease in the beginning of puberty), thyroid hormones, as well as sex hormones, which promote growth in pre- and pubertal period, have effects on growth. As before the onset of prepubertal period, at the age of 7–10 years, the levels of studied hormones are relatively constant, we considered it possible to pool these children into one group.
The age and sex parameters of the functional state of the pituitary–thyroid system showed that the content of microelements (chrome, nickel, manganese, copper and lead) was determined in children living in the Aral Sea region and in chrome processing (Aktobe) regions. Identical microelements were determined in children from the control region. Children did not differ in age. The levels of microelements in the blood of children, depending on the place of residence, were different. Namely, in children living in the Aral Sea region, the content of chrome, manganese and lead was higher (P < 0.05). In children living in the chrome processing region, chrome content exceeded normal in the control region; levels of manganese were increased by 3.4 times and nickel by 1.5 times (P < 0.05).
When the hormonal status of children living in the Aral Sea, chrome processing and gas processing regions was studied, a number of changes were established that could affect their physical and sexual development. They include:
-
lack of activation of thyroid-stimulating hormone—thyroid gland, typical for normal conditions in the prepubertal period;
-
insufficient levels and impaired ratio of gonadotropins;
On average, the concentration of triiodothyronine (T3) in children living in the Aral Sea region was 1.57 ± 0.06 ng/ml, in chrome processing region 1.67 ± 0.05 ng/ml and in gas processing region 1.63 ± 0.06 ng/ml. The lowest concentration of T3 in all three studied regions was observed at the age of 12 years. In the control region, it was 2.0 ± 0.09 ng/ml (P < 0.001).
There is a significant difference in the average levels of thyroxine (T4) in children living in the Aral Sea region and in gas processing regions: The concentration was 96.2 ± 0.44 ng/ml and 89.4 ± 1.28 ng/ml (P < 0.001), respectively; in children living near chrome processing plants, it was 97.4 ± 1.28 ng/ml (P < 0.001); and in the control region it was 117.3 ± 0.74 ng/ml. It should be noted that in children living in different ecologically unfavorable regions, the levels of thyroxine decrease with age and reach minimum values in the Aral Sea and chrome processing regions at the age of 15–16 years and are, respectively, 93.0 ± 0.44 and 92.0 ± 1.28 ng/ml; in gas processing regions—at the age of 12 years and are 81.0 ± 1.38 ng/ml. By the age of 17, the values are slightly higher, but do not meet physiological needs for this age.
The comparative analysis of the thyroid-stimulating hormone showed that with age the levels of TSH decrease in all three regions and, on average, were 1.37 ± 0.16 mIU/ml in children living in the Aral Sea and chrome processing regions, 1.20 ± 0.07 mIU/ml in children living near gas processing plants, while in the control region it was 2.2 ± 0.10 mIU/ml (P < 0.001). In ecologically unfavorable regions, this may be a compensatory reaction to the increase in T4, which, in turn, is also increased for compensation.
The levels of gonadotropins up to 13–14 years vary in relatively narrow limits, not differing significantly from the initial level. Studies have shown that in children living in different ecologically unfavorable regions gonadotropin levels increase with age: Luteinizing hormone (LH) levels increase by almost 5.5 times by the age of 13, and by 17 years in children living in the Aral Sea region it reaches, on average, 7.65 ± 0.13 mIU/ml; in chrome processing regions—7.8 ± 0.10 mIU/ml; in gas processing regions—4.96 ± 0.29 mIU/ml; and in the control group—8.0 ± 0.19 mIU/ml. These data show that low levels of LH are observed in children living in the gas processing region, and this affects their sexual development and puberty, especially in those living near gas processing plants. It is possible that, in order to ensure puberty, higher concentrations of LH are required compared to normal conditions.
Follicle-stimulating hormone (FSH) levels in all children and adolescents in various ecologically unfavorable regions evenly increased to a maximum by the age of 17 and were 9.1 ± 0.16 mIU/ml in girls living in the Aral Sea region, 9.0 ± 0.11 mIU/ml in children from chrome processing region, 5.6 ± 0.31 mIU/ml in gas processing regions and 11.01 ± 0.22 mIU/ml in the control group. These parameters are also lower in children living in the gas processing region. Apparently, the unusual ratio of gonadotropins observed in children living in the studied regions with delayed sexual development adversely affects the latter. It should be noted that the concentration of gonadotropins increased with age, but it still did not reach the levels typical for children from the control group by 17 years.
To study the somatotropic function of the pituitary gland, children with short stature were subjected to a stimulation test with clonidine. The secretion of somatotropic hormone (STH) was determined after pharmacological stimulation. These data were compared with the corresponding parameters of the control group (children from Kobda) in order to study possible features of the secretion of STH in children with GD after taking clonidine.
The obtained results show that the baseline level of STH in normally growing children of the control group ranged from 0.3 to 6.0 ng/ml. After taking clonidine, as we expected, there was an increase in the levels of STH. The frequency of the maximum (peak) values of the STH in different time intervals of the test was of interest. Thirty minutes after clonidine administration, STH concentrations were low (1.9 and 3.1 ng/ml), which is consistent with the literature data. On the 60th minute of the test, the average concentration of STH, compared to baseline, increased in children from the Aral Sea region by 7.8 times, from chrome processing region by 8.2 times and from gas processing region by 7.9 times, which almost coincides with the control group. The range of differences in all three regions was from 0.6 to 65 ng/ml and in the control group from 1.1 to 80 ng/ml. 90 min after taking clonidine, the levels of STH remained high and exceeded baseline for all three regions approximately equally, i.e., by 6.1 times (in the control group, 5.0 times). Individual variations were 2.0–35.4 ng/ml for the Aral Sea region, 2.2–38.1 ng/ml for chrome processing region and 2.0–37.9 ng/ml for gas processing region; in the control group this parameter was 2.5–38.0 ng/ml. On the 120th minute of the test, the levels of STH decreased significantly, and the range of variations in all three regions was approximately the same, from 0.5 to 15.5 ng/ml. It should be noted that in all three regions the average levels of STH did not differ from the initial values, similar to the control group (P > 0.1). Consequently, during the clonidine test, the STH levels are poorly informative after 30 min, while in the range of 60–90 min after taking the drug, somatotropinemia reaches its peak values in all children. After 120 min, the level of STH decreases, not significantly differing from the initial values (P > 0.01).
The maximum values of STH were recorded in the interval between 60 and 90 min after administration of clonidine without differences in mean values. Therefore, in children with short stature living in the Aral Sea, chrome processing and gas processing regions, the growth function of the pituitary gland is at a lower limit of the norm.
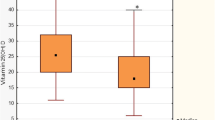
The insulin-like growth factor (IGF) is of particular practical importance, which is responsible for the realization of the biological effect of the growth hormone at the tissue level and the feedback regulation of the somatotroph cell function. IGF-1 circulates in the blood in a bound state. The levels of IGF-1 in the blood were studied in 30 children with growth delay. The study of the IGF-1 levels showed a decrease in its concentration (Fig. 1). Comparison of the above values indicates significantly reduced IGF-1 levels in children living in the Aral Sea, chrome processing and gas processing regions.
The peak of growth rates is noted in the III and IV stages of the puberty period (according to Tanner) and usually finishes by the V stage. IGF-1 levels reflect the endogenous secretion of STH. The examined children did not have a significant increase in IGF-1 in the pubertal period. The microelement blood levels in children living in the chrome processing region (Aktobe) are shown in Table 3. The values were also compared to normal and control values.
In conclusion, there are differences in blood levels of microelements in children depending on the place of residence. Namely, the children of Aktobe have higher chrome and nickel levels in their blood (P < 0.05).
Major causes and clinical forms of short stature and development of clinical and laboratory methods for early diagnosis, treatment and prediction of short stature in children living in the Aral Sea, chrome processing and gas processing regions
After an in-depth study of children living in the Aral Sea, chrome processing and gas processing regions, we analyzed the causes of short stature according to the Silver classification as the most complete classification of the causes of short stature in childhood (Silver et al. 1953). Considering the fact that a large percentage of the studied children did not belong to the classification groups proposed by Silver, we distributed the children within the framework of the working classification developed by us as follows (Table 4). Therefore, according to the proposed working classification, a group of children with ecologically dependent short stature was singled out: in the Aral Sea region—58.1%, in the chrome processing region (Aktobe)—53.6%, in the gas processing region (Zhanazhol)—48.1% (P < 0.05).
Based on the results of the study, it should be emphasized that residents of the Aktobe region, including Aktobe, are affected by factors that have a negative impact on the growth of children. We have developed a scheme of the mechanism of short stature development in children exposed to chrome and its compounds and gas products. To develop clinical and laboratory methods for early diagnosis and prediction of short stature in children exposed to chrome compounds, as well as oil and gas products, we established a correlation between environmental factors (internal and external) and physical development of the child. The analysis of the correlation of socially determined environmental factors that can influence physical development of children has proved to be multifactorial, with an average correlation value of 0.61, without predominance of any leading extreme risk factor.
In our study, we analyzed paired correlation coefficients of height and body weight—two leading anthropometric parameters—with a number of morphological and functional parameters in children 7–17 years old. Namely, we made a correlation between growth rates in children living in the Aral Sea region and levels of thyroid hormones (T3, T4, TSH), sex hormones (LH, FSH) and IGF-1 and received the following results. In children living in the Aral Sea region and in chrome processing regions, a direct average correlation with T3 levels (0.66) and strong inverse correlation with T4 and TSH (respectively, 0.95 and -0.77) were found. The highest direct correlation in all age and sex groups was established between sex hormones (LH and FSH) and height and was equal to 0.94 and 0.95, respectively. An average direct correlation of low growth rates in children living in the Aral Sea and chrome processing regions was established with IGF-1, which averaged 0.68. An average inverse correlation was found between the content of chrome in the blood and height and body weight (P < 0.001).
In children from the gas processing region, a strong direct correlation with T3 levels (0.77) and strong inverse correlation with T4 and TSH levels (− 0.71 and − 0.74, respectively) were found. A distinctive direct correlation was registered, similar to children living in the Aral Sea and chrome processing regions, between the levels of sex hormones (LH and FSH) and height equal to 0.94 and 0.93, respectively. An average direct correlation between low growth rates in children living in gas processing regions and IGF-1 was established, which averaged 0.68. In general, the material obtained gives an idea of the relationship and mutual influence of various factors and degree of influence on the rate of constitutional growth.
Based on the obtained study data, we developed an algorithm for diagnosis of growth delay in children living in the Aral Sea, chrome processing and gas processing regions. We analyzed various clinical and diagnostic features and developed a mathematical model for the diagnosis of growth delay risks. The prognostic coefficients of each parameter were determined using the Naive Bayes algorithm for probability modeling.
For the convenience of handling the list of growth delay risk factors, predicting the final growth of the child and determining the proportion and information value of each parameter, the significance of each risk factor was calculated using its prognostic factor. Based on the results obtained, a prognostic table was constructed, based on the prediction of growth delay probability in children in each specific case. A list of test parameters is presented where each attribute is expressed as a numerical prognostic coefficient with a positive or negative value.
A sum equal to 13 with a positive and negative value was considered a threshold value. If the reached threshold value is positive (+ 13), the examined child has a high probability of growth delay. The negative threshold value (− 13) indicates a minimal risk of growth delay in the subject.
Therefore, the obtained clinical and laboratory data of children with short stature living in the Aral Sea, chrome processing and gas processing regions are due to the adaptive condition aimed at ensuring of body functions and are on the borderline between norm and pathology. The clinical significance of this condition is that it cannot be compensated by social factors, but is realized only at the expense of morpho-functional adjustments of the body itself. These children and children at risk need, above all, medical and recreational measures. Based on the conducted studies, clinical and laboratory results, mathematical calculations and correlation dependencies, a concept of a clinical and pathogenetic justification of the formation of short stature in children living in the Aral Sea, chrome processing and gas processing regions was developed (Fig. 2). It is known that chrome compounds contaminate soil, water, air and food. With the latter, chemical compounds enter the body through the gastrointestinal tract, respiratory and other pathways of people who are not directly involved in chrome production. At the same time, chrome, which has membrane-damaging, sensitizing and toxic effects, causes damage to the hematopoietic, endocrine, digestive and hormonal systems. This damage is manifested in the development of short stature in children.
In general, the material obtained gives an idea of the relationship and mutual influence of various factors and degree of influence on the rate of constitutional growth. In addition, the study of the nature of correlations between parameters allows a deeper consideration of the issues of “normal” development, methods of evaluation and intragroup features of the morpho-functional development of a growing body, early diagnosis and prediction of short stature in children caused by environmental contamination with chrome compounds and oil and gas processing products. Based on the obtained study data, we developed an algorithm for diagnosis of growth delay in children living in ecologically unfavorable regions (Fig. 3).
The authors propose a scheme of medical and recreational measures for children living in the Aral Sea, chrome processing and gas processing regions. The increased sensitivity of the child’s body to external influences and mobility of metabolic processes make corrective measures more effective and less time-consuming. The complex of corrective measures at all stages (polyclinic, organized groups and sanatorium) includes medical and preventive measures. Medical measures are aimed at the correction of identified pathologies in major systems and organs and preventive measures are aimed at the strengthening of children’s health. A continuous condition for their effectiveness is the year-round health improvement.
The complex of corrective measures should be aimed at the prevention and elimination of the effects of irritating, skin-resorptive and general toxic effects. The main methods of health improvement in children are: daily routine, rational nutrition, exercise therapy, massage, oxygen therapy, phytotherapy and pharmacotherapy. To determine the effectiveness of the complex of medical and corrective measures, a developed table (map) was used, which is a list of signs and laboratory results, where each attribute and parameter are expressed in points. This allows an integral assessment of the condition of the child’s body. The following steps are performed:
-
1.
evaluation in points of numerical values of clinical and laboratory parameters according to the table;
-
2.
total score before and after treatment;
-
3.
calculation of the efficiency coefficient by dividing the total score before treatment by the score after treatment.
Conclusion
This scientific research is aimed at the development of concepts for the prediction of short stature, study of clinical and pathogenetic mechanisms for the formation of short stature, improvement and development of new approaches and new technologies in the prevention and treatment of short stature in children living in ecologically unfavorable regions. Summing up the results of the conducted study of the physical development of children living in the Aral Sea, chrome processing and gas processing regions, we have come to the following conclusions.
-
1.
The prevalence of short stature in the Aral Sea region was 23.0% of the total number of studied subjects; in chrome processing region—23.6%; in gas processing region—22.2%. In the control region, the rate of short stature was 7.8%.
-
2.
The pathology of ante- and perinatal periods (51.1%), low weight and body length at birth (43.5%), as well as unfavorable social factors—low educational level of parents, poor housing conditions, low cost of living and unsatisfactory nutrition (57.2%)—are observed in children with short stature who live in the Aral Sea, chrome processing and oil and gas processing regions.
-
3.
In children living in conditions of environmental contamination with chrome compounds and oil and gas products, a high content of toxic compounds of chrome (1.381 ± 0.36 μg/l), manganese (1.220 ± 0.45 μg/l), lead (0.213 ± 0.09 μg/l) and nickel (0.133 ± 0.02 μg/l) (P < 0.05) is observed.
-
4.
The imbalance of the hormonal status was observed in children with short stature living in the Aral Sea, chrome processing and oil and gas processing regions, which is characterized by changes in the concentration of thyroid-stimulating hormones (T3 (1.69 ± 0.17 ng/ml), T4 (94.4 ± 1.28 ng/ml), TSH (1.58 ± 0.16 ng/ml) and gonadotropins, LH (4.86 ± 0.10 ng/ml) and FSH (4.78 ± 0.09 ng/ml), low levels of STH (2.0–37.1 ng/ml) and a decrease in IGF-1 (258.2 md/l) in the pre- and pubertal periods (P < 0.05).
-
5.
The main causes of short stature in children living in the Aral Sea, chrome processing and oil and gas processing regions are cerebral–endocrine pathologies, hereditary diseases, somatogenic diseases, constitutional growth delay and ecologically determined short stature.
-
6.
Etiopathogenetic mechanisms of formation of short stature in children living in the Aral Sea, chrome processing and oil and gas processing regions are based on the detection of toxic chemical compounds in the blood, structural and functional changes in vital functions together with hormonal homeostasis imbalance.
The scientifically justified program for the prevention and treatment of environmentally determined diseases in children of the West Kazakhstan region will improve the parameters of physical development, which is of great importance for girls in terms of preparation for child-bearing age and boys in terms of preparation for military service, which ultimately improves the quality life of children and has social effects. The proposed new methods of forecasting, prevention and correction possess no economical damage.
References
Avtsyn, A. P., Zhavoronkov, A. A., Rish, M. A., & Strochkova, L. S. (1991). Mikroelementozy rights. Moscow: Medicine.
Bayevsky, R. M. (1990). Prediction of conditions on the verge of norm and pathology. Moscow: “M”.
Bermagambetova, S. K., Zhumalina, A. K., Tusupkalieva, K Sh, Tusupkaliev, B., & Tuyakbaev, A. M. (2008). Linkage of morbidity indicators with the level of microelements of blood in children living near chrome-mining and processing enterprises. Batys Kazakh Medical Journal, 4(20), 79–81.
Blunk, W. (1981). Pediatric endocrinology. Moscow: Medicine.
Bobak, M., & David, A. L. (1999). Pregnancy outcomes and outodoor air pollution: An ecological study in regions of the Czech Republic 1986–1998. Occupational and Environmental Medicine, 8(56), 539–543.
Bukina, L. G., Kuznetsova, A. P., & Leontieva, T. N. (2007). The physical development of girls in an industrial city. Physiology of humans and animals: from experiment to clinical practice: theses. doc. VI youth scientific. Conf. Institute of Physiology, Komi Science Center, Ural Branch of the Russian Academy of Sciences, March 20–22, Syktyvkar.
Bunak, V. V. (1941). Anthropometry. Moscow: Uchpedgiz.
Cowveina, N. B., Bremner, S. A., & Novaes, N. (2004). Association of ambient air pollution and birth in San Paulo. Journal of Epidemiology and Community Health, 1(58), 11–17.
Dementieva, G. M., Kozlova, A. E., & Nissan, L. G. (1984). Evaluation of the physical development of newborns. Moscow: Nauka.
do Nascimento, S., de Andrade Júnior, F. P., Alves, T. W. B., & Menezes, M. E. S. (2018). Seeds of chia (salviahispanica L.) as an agent in prevention, treatment and control of some diseases chronicles: A review. Periódico Tchê Química, 15(30), 402–414.
Iztleuova, G. M., Mavlyudova, N. M., Iztlev, E. M., & Iztlevov, M. K. (2009). Nephroprotective effect of the oil extract of nettle leaves and lipoic acid in chroinduced nephropathy. Batys Kazakh Medical Journal, 3(23), 32.
Karimov, T. K., & Shkolbulova, D. T. (2008). Negative influence of industrial enterprises on the river Ilek of Aktobe region. Health and Disease, 9(75), 30–31.
Kuchma, V. R. (2002). Assessment of the risk of the influence of environmental factors on the health of children and adolescents. Hygiene and Sanitation, 6, 51–53.
Liu, Sh, Krewski, D., Shi, Y., Che, Y., & Burnett, R. T. (2003). Association between gaseous ambient air pollutants and pregnancy in vancouver. Environmental Health Perspectives, 14(111), 1773–1778.
Lyalikov, S. A., & Lyalikova, V. I. (2008). Periodization of childhood on the basis of anthropometric indicators. Journal of the State Min and Metal Universe, 4, 28–32.
Mukyshova, G. D., Iztleuov, M. K., Sundetov, Zh S, Omarova, K. P., & Iztleuov, E. M. (2009). Correction of the hemothoxic effect of hexavalent chromium. Batys Kazakh Medical Journal, 3(23), 38.
Perepust, L. A. (1977). Determination of age according to roentgenograms of the bones of the hand. Method of recommendation. Kiev: Vyshcha shkola.
Revich, B. A., Avaliani, S. L., & Tikhonova, G. I. (2004). Ecological epidemiology. Moscow: Academy.
Sharova, A. A., Volevodz, N. N., & Peterkova, V. A. (2006). Low growth in children: Causes, differential diagnosis and treatment options (literature review). Reproductive Health of Child and Adolescents, 3, 53–63.
Silver, H. K., Kiyasu, W., George, J., & Deamcr, W. C. (1953). Syndrome of congenital hemihypertrophy, shortness of stature and elevated urinary gonadotrophins. Pediatrics, 12, 368–376.
Skalnyi, A. V. (2000). Human microelementoses: Hygiene diagnosis and correction. Microelements in Medicine, 1, 2–8.
Sobolev, V. A., Zemlyanaya, G. M., & Revazova, Yu A. (2007). Conducting medical examinations of children living in sanitary-epidemiologically unfavorable territories. Hygiene and Sanitation, 4, 22–27.
Stavitskaya, A. B., & Aron, D. I. (1959). Methods of studying the physical development of children and adolescents. Moscow: Medgiz.
Uzunova, A. N., Tsvetova, I. P., Neryakhina, S. V., Lopatin, O. V., & Zaitsev, M. L. (2008). Features of physical development in the zone of environmental problems. Hygiene and Sanitation, 2, 89–91.
Vasiliev, A. V. (2005). Physiometric indicators of children living in areas with different levels of aerotechnogenic load. Hygiene and Sanitation, 1, 39–40.
Vitebskaya, A. V. (2007). Modern trends in the diagnosis and therapy of idiopathic stuntedness. Problems of Endocrinology, 1, 46–53.
Zhukovsky, M. A. (1982). Pediatric endocrinology. Moscow: Medicine.
Zhumalina, A. K., Zhilkibaeva, B Zh, & Tungatarova, M. A. (2008). Problems of stunting in children living in ecologically disadvantaged regions. The possibilities of early diagnosis at the present stage. Bulletin of the Kazakhstan Natural Medicine Universe, 1, 102–103.
Acknowledgements
The study was carried out within the framework of grant financing of scientific research activities of the Ministry of Education and Science of the Republic of Kazakhstan for 2013–2015 for The Improvement of Technologies for Children’s Health Care and Reproductive Health, Registration number of NTI: 0113RK00439.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Rights and permissions
About this article
Cite this article
Zhumalina, A.K., Bekmukhambetov, E.Z., Tusupkaliev, B.T. et al. Development of scientifically justified proposals on the prevention and treatment of environmentally determined constitutional growth delay in children in the West Kazakhstan region. Environ Geochem Health 41, 1251–1265 (2019). https://doi.org/10.1007/s10653-018-0210-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10653-018-0210-0