Summary
This open-label first-in-human study evaluated JPH203, which is a novel selective L-type amino acid transporter 1 inhibitor. We also evaluated the association between the N-acetyltransferase 2 phenotype and outcomes. Japanese patients with advanced solid tumors received daily intravenous JPH203 treatment for 7 days, followed by a 21-day rest period, at escalating doses of 12–85 mg/m2. Dose-limiting toxicities were evaluated during the first cycle using a 3 + 3 design. The study enrolled 17 patients, although grade 3 liver dysfunction was detected in one of six patients receiving 60 mg/m2 and in the first patient to receive 85 mg/m2. Further enrollment was terminated and the maximum tolerated dose was defined as 60 mg/m2. The AUC∞ increased between 12 mg/m2 and 25 mg/m2, although no differences were observed at 25–40 mg/m2. Partial response was observed for one patient with biliary tract cancer (BTC) at the 12 mg/m2 dose, and disease control was achieved by 3 of 6 patients at the 12 mg/m2 and 25 mg/m2 dose levels. Based on these results, we recommend a phase II dose of 25 mg/m2. The disease control rate for BTC was 60%. Two patients with grade 3 liver dysfunction had the rapid N-acetyltransferase 2 phenotype, and disease control was more common for the non-rapid phenotype (50% vs. 12.5%). It appears that JPH203 was well-tolerated and provided promising activity against BTC. The N-acetyltransferase 2 phenotype might help predict the safety and efficacy of JPH203. Clinical trial registration: UMIN000016546.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer cells require more glucose and amino acids than normal cells because of their rapid proliferation rate. Therefore, cancer cells tend to have higher expression of transmembrane nutrient transporters, such as those for glucose and amino acids [1]. Hosios et al. recently reported that, in cancer-related cellular proliferation, the majority of the cell mass (blocks) is derived from non-glutamine amino acids, while the consumption of glucose and glutamine is mainly involved in metabolism (i.e., as energy sources) rather than for the cell block increase during the proliferation of normal tissues and cancer growth [2]. Thus, non-glutamine amino acids seem to be more important in both normal and cancer cell growth, relative to glucose for normal tissue regeneration, which involves different amino acid uptake processes that are mentioned below.
The L-type amino acid transporter (LAT) is responsible for transporting large neutral amino acids with branched or aromatic side chains through the plasma membrane [3]. Various LATs have been identified, including LAT1, LAT2, LAT3, and LAT4 [4,5,6,7], with the LAT1 protein being originally isolated from C6 rat glioma cells [4]. Various cancer cells have high expression of LAT1, although high expression is also observed in human fetal tissues (such as the liver) and low-to-moderate LAT1 expression is observed in the human placenta, testes, bone marrow, and brain [8]. Several preclinical studies have shown that inhibition of LAT1 induces cancer cell apoptosis, which is related to the depletion of amino acids required for cancer cell growth and the induction of cell cycle arrest [9,10,11]. Furthermore, several studies of resected or biopsy samples have identified LAT1 expression as a potential prognostic factor in patients with various cancers [12,13,14,15,16,17,18,19,20,21]. These findings suggest that LAT1 could be a molecular target for anticancer therapies, although we are not aware of any clinical trials that have investigated an LAT1 inhibitor.
The plasma free amino acids (PFAAs) that serve as substrates for LAT1 include leucine, isoleucine, phenylalanine, methionine, tyrosine, histidine, tryptophan, and valine [4]. Most of these amino acids, with the exception of tyrosine, are essential amino acids in humans. A novel selective LAT1 inhibitor (JPH203) inhibits cancer cell growth by depleting the levels of these amino acids in cancer cells. In a nude mice model, JPH203 inhibited the growth of inoculated HT-29 cancer cells, which were derived from a human colon cancer [22]. A preclinical pharmacokinetic study also revealed that JPH203 is metabolized into N-acetyl JPH203 [23]. When JPH203 is administered intravenously, it is taken up via organic anion transporters into liver cells, where it is predominantly acetylated to N-acetyl-JPH203 (Nac-JPH203) by the N-acetyltransferase 2 (NAT2) and is passively excreted in bile [23, 24]. Single nucleotide polymorphisms (SNPs) in the NAT2 coding region had been identified, with their corresponding alleles and haplotypes: rs1801279 (191G > A), rs1041983 (282C > T), rs1801280 (341T > C), rs1799929 (481C > T), rs1799930 (590G > A), rs1208 (803A > G), and rs1799931 (857G > A) [25]. Furthermore, there are three known NAT2 phenotypes, which can be classified as rapid, intermediate, and slow acetylators. It has been suggested that the NAT2 acetylation process is the rate-limiting step in Nac-JPH203 production, and it is possible that the NAT2 acetylator phenotypes may help predict the safety and efficacy of JPH203.
This first-in-human phase I study evaluated JPH203 to determine its safety, maximum tolerated dose (MTD), and recommended phase II dose (RP2D) among Japanese patients with advanced solid tumors. We also evaluated the pharmacokinetics (PK), pharmacodynamics (PD), and preliminary antitumor effects of JPH203. Finally, we analyzed the associations between the NAT2 phenotypes and clinical outcomes in patients who received JPH203.
Materials and methods
Study design and ethical considerations
This first-in-human study was designed as a single-center, open-label, single-arm, dose-escalation phase I trial using a 3 + 3 design. The study protocol was approved by the institutional review board at Kyorin University and was registered as UMIN000016546. All patients provided informed consent before enrollment. This study was conducted in accordance with the Declaration of Helsinki and good clinical practice. An independent data and safety monitoring board reviewed all safety-related data. Furthermore, we retrospectively examined the associations between the NAT2 phenotypes and clinical outcomes using whole-blood samples from the prospective portion of the study. The retrospective analysis was also approved by the institutional review board at Kyorin University.
Patients with advanced solid tumors received daily JPH203 treatments (via a 90-min intravenous infusion) for 7 days, followed by a 21-day rest period. The planned dose escalations were 12 mg/m2, 25 mg/m2, 40 mg/m2, 60 mg/m2, and 85 mg/m2. Before starting this schedule, we confirmed the drug’s safety during a 7-day observation period after the patient received a single dose of JPH203 and then rested. The starting dose was determined based on toxicology experiments using rats, which revealed no clear adverse effects at a dose of 2 mg/kg, which is equivalent to a human dose of 12 mg/m2.
The primary endpoints were defined as safety outcomes, the MTD, dose-limiting toxicities (DLTs), and the RP2D. The secondary endpoints were defined as PK findings, PD findings, and efficacy outcomes.
Patient population
Patients were considered eligible based on the following criteria: male or female Japanese patients who were ≥ 20 years old, provided informed consent, had histopathologically confirmed advanced or refractory solid tumors, had no response to standard therapies, had a life expectancy of >90 days, and had an Eastern Cooperative Oncology Group performance status of 0 or 1. In addition, patients were required to have adequate bone marrow, renal, and liver functions: neutrophil count of ≥1500/mm3, hemoglobin level of ≥9.0 g/dL, platelet count of ≥75,000/mm3, serum creatinine level of ≤1.5× the upper limit of normal (ULN), serum total bilirubin level of ≤1.5× the ULN, and serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels of ≤2.5× the ULN (or ≤ 5.0× the ULN for patients with liver metastasis and/or biliary drainage). The key exclusion criteria were: severe underlying disorders and/or unstable complications as judged by the investigator; infection requiring systemic therapy; seropositivity for the HBs antigen, HCV antibodies, or HIV-1 antibodies; clinically significant electrocardiographic abnormalities; pleural effusion, pericardial effusion or ascites requiring drainage; presence of brain metastasis; history of radiation therapy to >33% of the hematopoietic bone marrow before enrollment; frequent diarrhea or watery stools; pregnancy or lactation; and receiving regular systemic steroid therapy, chemotherapy, radiotherapy, or immunotherapy during the 4 weeks before enrollment.
Safety assessment
Complete hematological tests, blood biochemistry tests, and urine tests were performed at the screening, before single-dose treatment, at 25.5 h after the single-dose treatment, and then on days 1, 4, 7, 14, 21, and 28 of cycle 1, followed by testing on days 1, 8, 14, 21, and 28 of subsequent cycles, and at the end of treatment. Physical examinations, including assessment of vital signs, were performed daily during the course of JPH203 administration and at the time of patient visits (at least every 7 days). Adverse events (AEs) were evaluated in accordance with the Common Terminology Criteria for Adverse Events version 4.0. The withdrawal criteria were: appearance of a DLT, a clinical or imaging-based diagnosis of disease progression, occurrence of a serious adverse event, patient refusal of treatment, pregnancy, or treatment discontinuation based on the investigators’ judgement. We defined DLTs as AEs for which a causal relationship with JPH203 could not be ruled out during the first treatment cycle: Grade 3 non-hematological toxicities, excluding rash acneiform, rash maculo-papular, urticaria, nausea, vomiting, anorexia, diarrhea, constipation, or fatigue, which resolved to grade 1 severity within 7 days after optimal medical treatment; investigator judgement that the drug should be withdrawn; Grade 4 hematological toxicities or Grade ≥ 3 thrombocytopenia requiring transfusion; and febrile neutropenia. If a patient developed a DLT, other patients were added to the treatment group until the total reached 6 patients, and we confirmed that no other patients experienced a DLT before escalating to the next dose level. If ≥2 patients developed a DLT in any dose group, that dose was pre-defined as the MTD. The RP2D was determined based on the DLT results, the PK/PD data, and the preliminary efficacy data.
Pharmacokinetics and pharmacodynamics
The PK parameters were evaluated based on plasma and urine JPH203 concentrations. Blood samples were collected before the single-dose treatment and at 10 subsequent timepoints: 0.5 h, 1 h, 1.5 h, 2 h, 3 h, 4.5 h, 6 h, 12 h, 25.5 h, and 49.5 h. Furthermore, 11 blood samples were collected before the first cycle of the repeated-dose treatment and after the first cycle: 1.5 h later on days 1 and 4, before the dose administration on day 7 as well as 1.5 h, 3 h, 6 h, 12 h, 25.5 h, and 49.5 h later. Urine samples were collected before the single-dose treatment and at intervals of 0–3 h, 3–6 h, 6–12 h, and 12–25.5 h. The concentrations of JPH203 and Nac-JPH203 in both sample types were determined using a validated liquid chromatography-mass spectrometry method.
Blood samples for the PFAA analysis were collected before the single-dose treatment and 25.5 h later.
Efficacy analyses
Computed tomography was performed after the first cycle and then every 6 weeks after the end of the first cycle. Tumor responses were evaluated in accordance with the Response Evaluation Criteria in Solid Tumors version 1.1. The response rate (RR) was defined as the proportion of patients who experienced a complete response (CR) or partial response (PR). The disease control rate was defined as the proportion of patients with CR, PR, or stable disease (SD).
NAT2 SNP analysis
The NAT2 SNP analysis was performed by BML Inc. (Tokyo). The patients’ blood samples were subjected to DNA extraction and analysis to identify SNPs and the NAT2 phenotype. The presence of rs1495741 was determined using the TaqMan® SNP Genotyping Assay, in accordance with the manufacturer’s instructions. The two-SNP inferred NAT2 acetylator phenotype was identified based on the presence of rs1041983 (282C > T) and rs18011280 (341T > C). The three-SNP inferred NAT2 acetylator phenotype was identified based on the presence of rs1799929 (481C > T), rs1799930 (590G > A), and rs1799931 (857G > A). The four-SNP inferred NAT2 acetylator phenotype was identified based on the presence of rs1801279 (191G > A), rs1801280 (341T > C), rs1799930 (590G > A), and rs1799931 (857G > A). In these assays, the rapid acetylator phenotype was defined as the homozygous presence of all normal versions, the intermediate acetylator phenotype was defined as the heterozygous presence of any one of the SNPs, and the slow acetylator phenotype was defined as the homozygous presence of one or more SNPs or the heterozygous presence of two or more SNPs.
Statistical analysis
The PK parameters were expressed as mean ± standard deviation values. The blood ratio of Nac-JPH203/JPH203 was calculated for individual patients based on the AUC∞. The urine ratio of Nac-JPH203/JPH203 was also calculated for individual patients, using the amounts of JPH203 and Nac-JPH203 accumulated in the urine at 0–25.5 h after the single-dose treatment. The amino acid data were expressed as mean ± standard deviation values, with statistical significance evaluated using Student’s t test. For all tests, significant differences were identified based on a P value of <0.05. All analyses were performed using IBM SPSS software (version 22.0; IBM Corp., Armonk, NY).
Results
Patient characteristics
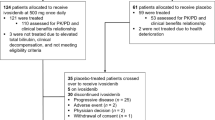
Seventeen patients were enrolled between January 2015 and August 2016. The patients’ characteristics are shown in Table 1. Most patients had gastrointestinal cancers, with the most common types being colorectal cancer (35%), biliary tract cancer (BTC, 29%), and pancreatic cancer (24%). All patients had received previous treatments, with a median number of 3 previous chemotherapy regimens (range: 2–6).
Follow-up and safety outcomes
The median follow-up time was 3.7 months (range: 1.5–26.8 months). The dose escalation summary (12–85 mg/m2) is shown in Table 2. Grade 3 liver dysfunction occurred in 1 of 6 patients receiving the 60 mg/m2 dose, as well as in the first patient who received the 85 mg/m2 dose. Although the AEs in these 2 patients resolved rapidly, further enrollment was terminated because the grade 3 liver dysfunction was deemed a DLT at the 85 mg/m2 dose. Therefore, the MTD was defined as 60 mg/m2.
The treatment-related AEs (TRAEs) are summarized in Table 3. The most common TRAEs were generally grade 1 or 2 elevated ALT, elevated AST, elevated γ-GTP, malaise, nausea, hypertension, and fever. Grade 3 elevations of ALT, AST, and γ-GTP were observed in the 60 mg/m2 and 85 mg/m2 groups, which were considered DLTs. There were no cases of grade 4 TRAEs or death. The treatment was eventually discontinued because of tumor progression in 14 of the 17 patients, and because of the grade 3 liver dysfunction in the other 2 patients. The remaining patient is continuing JPH203 treatment without disease progression for 2 years.
Pharmacokinetics and pharmacodynamics
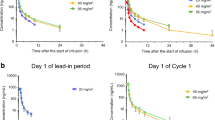
The PK parameters for JPH203 are shown in Fig. 1. The maximum plasma concentrations (Cmax) of JPH203 were observed at 1.0 h after a single-dose administration for the 12 mg/m2 and 25 mg/m2 doses, and at 1.5 h for the 40 mg/m2, 60 mg/m2, and 85 mg/m2 doses. The Cmax values after a single dose increased between the 12 mg/m2 and 85 mg/m2 dose levels (Fig. 1a). Although the Cmax values also increased between the 12 mg/m2 and 85 mg/m2 dose levels after repeated treatments, JPH203 did not accumulate in the plasma (Fig. 1b). The AUC∞ values after single-dose and repeated-dose administrations are shown Fig. 1c. The AUC∞ values increased between the 12 mg/m2 and 85 mg/m2 dose levels after a single dose (12 mg/m2: 463.1 ± 64.5 ng・h /mL, 25 mg/m2: 887.8 ± 338.4 ng・h/mL, 40 mg/m2: 1460.5 ± 317.1 ng・h/mL, 60 mg/m2: 2094.3 ± 932.7 ng・h/mL, 85 mg/m2 [1 patient]: 3022.5 ng・h/mL). While the AUC∞ values after repeated-dose administrations increased between the 12 mg/m2 and 25 mg/m2 dose levels, no difference was observed between the 25 mg/m2 and 40 mg/m2 dose levels (12 mg/m2: 183.1 ± 57.1 ng・h/mL, 25 mg/m2: 1426.4 ± 285.1 ng・h/mL, 40 mg/m2: 1290.2 ± 351.5 ng・h/mL, 60 mg/m2: 1948.5 ± 763.5 ng・h/mL).
There were several patients who exhibited broad variations in their ratio of the Nac-JPH203 and JPH203 concentrations, regardless of the JPH203 dose level. The Nac-JPH203/JPH203 ratio in blood exhibited a roughly linear relationship with the ratio in urine (Fig. 2). Individuals with the rapid phenotype had higher Nac-JPH203/JPH203 ratios (i.e., higher production of Nac-JPH203), while patients with the non-rapid phenotype (slow + intermediate) had lower ratios.
Associations between Nac-JPH203/JPH203 in blood and urine and the NAT2 phenotypes. There was roughly linear relationship between the Nac-JPH203/JPH203 ratio in the blood and urine. Patients with the rapid NAT2 phenotype (8/16 patients) were predominantly distributed toward the upper right corner of the graph, while patients with the slow and intermediate phenotypes (8/16 patients) were predominantly distributed toward the lower left corner of the graph. Nac-JPH203, N-acetyl-JPH203; NAT2, N-acetyltransferase 2; DLT, dose-limiting toxicity; γ-GTP, γ-glutamyl transpeptidase; ALP, alkaline phosphatase
We observed an increase in the LAT1-substrate PFAA levels at the 12 mg/m2 dose level, but not at the other dose levels, after single-dose administration (Table 4).
Efficacy
Sixteen of the 17 patients were considered evaluable for treatment response. The remaining patient had pancreatic cancer and discontinued treatment before starting repeated-dose treatment at the 12 mg/m2 dose level because of tumor progression. The waterfall plots for response to JPH203 and time from enrollment are shown Figs. 3 and 4. The RR was 6.3% and the disease control rate was 31.3%. One patient with BTC achieved PR, and that patient continued treatment for 2 years without evidence of disease progression at the cut-off date (May 2017). Disease control was observed in 3 of 5 patients with BTC and in 2 of 6 patients with colorectal cancer. The patient who achieved PR was receiving the 12 mg/m2 dose level, and disease control was observed in 2 of the 3 patients at this level. No cases of PR were observed at the higher dose levels. Disease control was observed in 1 of 3 patients at the 25 mg/m2 dose, 1 of 3 patients at the 40 mg/m2 dose, and 1 of 6 patients at the 60 mg/m2 dose.
NAT2 SNP analyses
Sixteen patients provided blood samples for analysis of the 7 major SNPs (481C > T, 282C > T, 857G > A, 803A > G, 341T > C, 590G > A, and 191G > A). We observed that 4 SNPs (481C > T, 803A > G, 341T > C, and 191G > A) exhibited homozygous normal versions, and 3 SNPs (282C > T, 857G > A, and 590G > A) exhibited heterozygous versions or homozygous variants. The allele frequencies for those SNPs were consistent with those in the National Center for Biotechnology Information database. Based on the SNP panel results, all patients were classified according to their NAT2 acetylator phenotype (rapid, intermediate, or slow), and these classifications were consistent for each patient across all combinations of SNPs (2-SNP, 3-SNP, and 4-SNP) and regardless of the primary tumor site.
Association between the NAT2 phenotypes and clinical outcomes
Among the 8 patients with the rapid NAT2 phenotype, 4 patients exhibited liver dysfunction and had the highest Nac-JPH203/JPH203 ratios in the blood and urine, with 2 of these 4 patients judged to have experienced DLTs (Fig. 2). Disease control was re-analyzed in terms of the rapid and non-rapid phenotypes (intermediate or slow), which revealed disease control rates of 50% for the non-rapid phenotype (4/8 patients) and of 12.5% for the rapid phenotype (1/8 patients). Among the 5 patients with BTC, 3 of the 4 patients with the non-rapid phenotype experienced disease control (75%), while the 1 patient with the rapid phenotype had progressive disease (Tables 5 and 6).
Discussion
To the best of our knowledge, this is the first-in-human study of JPH203, which is a potent selective inhibitor of LAT1. The LAT1 protein was identified and named in 1998 [4], with an increasing number of reports identifying a relationship between LAT1 activity and various cancers. For example, several studies have evaluated LAT1 as an anti-cancer target [26, 27], evaluated its regulatory and functional role in cancer [28], and examined its structure, function, and ligand [29]. Thus, inhibitors of LAT1 may be a useful class of anti-cancer agents, with JPH203 potentially being the first-in-class compound to be tested in clinical studies.
The LAT1 protein has several unique properties in this setting. First, LAT1 has 12 transmembrane non-glycosylated segments, and requires a glycosylated chaperon (4F2hc or CD98) for its membrane trafficking [4], making it a heteromeric amino acid transporter. Second, LAT1 is an oncofetal protein that supports embryological growth through its high-capacity transport of large and essential amino acids, as well as during a limited period after gestation [30]. Third, LAT1 is upregulated when carcinogenesis is induced experimentally, and its high expression in cancer cells is related to high mortality among cancer patients [13,14,15,16,17,18,19,20,21]. Fourth, in vitro and in vivo models have indicated that cancer cell growth is dramatically reduced in LAT1-knockout cells or cells that are treated using a LAT1 inhibitor [31, 32]. Fifth, although LAT1 is expressed in some human adult tissues (e.g., the bone marrow, brain, reproductive organs, and skin), cancer tissues exhibit substantially higher LAT1 expression based on immunohistochemical testing and amino acid positron emission tomography using an LAT1 tracer (L-[3-18F]-α-methyltyrosine or 18F-FMT) [33].
This first-in-human study of JPH203 aimed to determine whether an LAT1-inhibiting small molecule could be used as a novel anticancer treatment. The results indicate that some solid tumors reacted well to JPH203 treatment, including BTC and colorectal cancer. This is likely because JPH203 was developed as a very potent LAT1 inhibitor [34], with tremendously high LAT1 selectivity, and it does not appear to have functional and/or biological activity against LAT2, which is a normal neutral amino acid transporter [34]. The JPH203 drug is formulated for intravenous injection in a sulfobutylether-β-cyclodextrin complex (JPH203-SBECD), which appears to be well tolerated as previously predicted, based on the sufficient safety margin between the MTD (60 mg/m2) and the RP2D (25 mg/m2). Furthermore, given that JPH203 is metabolized into N-acetyl-JPH203 by hepatic NAT2, the plasma concentrations of JPH203 should depend on hepatic enzyme activity. Nevertheless, it is important to note that 2 of 17 patients were removed from the study because they developed liver dysfunction as a DLT. This may be related to the metabolism of JPH203 into N-acetyl-JPH203 in the liver, with N-acetyl-JPH203 being excreted in the bile [23, 24]. Therefore, further studies are needed to directly evaluate how N-acetyl-JPH203 might be related to these episodes of liver dysfunction.
Although the MTD of JPH203 was determined to be 60 mg/m2, the PK profile of JPH203 did not support setting the RP2D at >25 mg/m2. This is because the plasma levels of LAT1-substrate PFAAs increased significantly, as expected, after single-dose administration at the 12 mg/m2 dose level, with disease control (PR + SD) observed for 3 of 6 patients at the 12 mg/m2 and 25 mg/m2 dose levels. However, we only detected SD in 2 of 10 cases at the ≥40 mg/m2 dose levels. Thus, we recommend 25 mg/m2 as the RP2D, as we suspect that high-dose JPH203 administration might have a negative feedback effect on the LAT1 pathway [11].
The present study revealed that JPH203 has promising activity in patients with BTC. Interestingly, LAT1 overexpression is associated with poor outcomes in various cancers [13,14,15,16,17,18,19,20,21], with the proportions of overexpression being 22% for prostate cancer, 29% for lung adenocarcinoma, 43% for gastric cancer, 43% for breast cancer, and 52.6% for pancreatic cancer [14,15,16,17,18]. Two recent studies have also revealed that LAT1 overexpression was related to a poor prognosis in patients with BTC [20, 21], with Kaira et al. reporting that LAT1 expression was elevated in 64.0% of resected BTC specimens. Thus, it appears that LAT1 expression is more likely to be elevated in BTC than in other cancers. Furthermore, several in vitro and in vivo studies have demonstrated that LAT1 inhibitors, including JPH203, are effective against BTC [11, 35, 36]. Therefore, based on the elevation of LAT1 expression in resected samples, the in vivo and in vitro efficacies of LAT1 inhibitors, and our preliminary efficacy data, it appears that JPH203 might have promising activity against BTC.
The JPH203 molecule is predominantly metabolized into Nac-JPH203 by NAT2 in liver cells. Furthermore, the metabolic clearance of JPH203 is longer than that of influx clearance, and eventually becomes passive clearance. Thus, JPH203 uptake appears to be the rate-limiting step for overall hepatic elimination in rats, while in human hepatocytes the intrinsic clearance is predicted to be rate-limiting [24]. The SNP panel assay results for the NAT2 phenotypes were consistent for all 16 individuals and across all combinations of SNPs. Hein et al. demonstrated that the accuracies for inferring the NAT2 phenotype were 98.4% for the 7-SNP panel, 92.2% for the 2-SNP panel, 92.2% for the 3-SNP panel, and 98.4% for the 4-SNP panel [25], and our results also support this conclusion. Furthermore, the allele frequencies for each of the 7 SNPs were consistent with those in the National Center for Biotechnology Information database, with more than one-half of the Japanese population having the non-rapid phenotype. According to Sabbagh et al., the slow-acetylator type of NAT2 may represent a genetic adaptation to dietary habits and lifestyle changes throughout the long history of human evolution. The authors also reported that the rapid phenotype is predominantly distributed in Asia, while the slow phenotype is predominantly distributed in Western Europe, based on data from 128 groups and 14,679 samples [37]. In the present study, 4 of 8 patients with the rapid phenotype developed liver dysfunction, and 2 of 4 patients had DLTs, while none of the patients with the non-rapid phenotype experienced these effects. Thus, it is possible that the NAT2 phenotype may help predict the development of AEs, especially liver dysfunction, after JPH203 treatment. We also speculate, based on our results, that the non-rapid phenotype is more likely to be linked to treatment efficacy. This suggests that a lower Nac-JPH203/JPH203 ratio is critical for maximizing the anti-tumor effect of JPH203, in which the acetylation of JPH203 into inactive Nac-JPH203 is slow because of non-rapid NAT2 activity.
This study had some limitations. First, the sample size was small and only 5 patients had BTC, despite our promising results in this patient subset. While there are few options for previously treated BTC, the FOLFOX regimen (5-FU, leucovorin, and oxaliplatin) plus active symptom control provided prolonged overall survival among patients previously treated using gemcitabine plus cisplatin [38]. On the other hand, a recent clinical trial of immune checkpoint anti-PD-1 monotherapy revealed modest activity in BTC patients who were refractory to or could not tolerate gemcitabine-based treatment, although its combination with gemcitabine and cisplatin provided a better outcome [39]. Thus, it may be prudent to carefully consider the use of JPH203 in patients with previously treated BTC. Second, all patients who were enrolled in the present study had already failed multiple treatment lines, and prolonged follow-up was difficult because of their poor prognosis. Third, we enrolled a heterogeneous group of patients with different cancer types and previous cancer treatments.
In conclusion, the PK/PD findings and the antitumor effects of JPH203 at each dose level indicate that an appropriate RP2D is 25 mg/m2. Furthermore, we found that JPH203 was well-tolerated at lower doses and provided promising activity against BTC. Moreover, the findings suggest that the NAT2 phenotype, which can be evaluated based on SNP panels, might be useful for predicting the safety and efficacy of JPH203. Therefore, we are conducting a placebo-controlled randomized phase II study of patients with BTC and the non-rapid NAT2 phenotype (UMIN000034080).
References
Ganapathy V, Thangaraju M, Prasad PD (2009) Nutrient transporters in cancer: relevance to Warburg hypothesis and beyond. Pharmacol Ther 121:29–40
Hosios AM, Hecht VC, Danai LV, Johnson MO, Rathmell JC, Steinhauser ML, Manalis SR, Vander Heiden MG (2016) Amino acids rather than glucose account for the majority of cell mass in proliferating mammalian cells. Dev Cell 36:540–549
Christensen HN (1990) Role of amino acid transport and countertransport in nutrition and metabolism. Physiol Rev 70:43–77
Kanai Y, Segawa H, Miyamoto K, Uchino H, Takeda E, Endou H (1998) Expression cloning and characterization of a transporter for large neutral amino acids activated by the heavy chain of 4F2 antigen (CD98). J Biol Chem 273:23629–23632
Segawa H, Fukasawa Y, Miyamoto K, Takeda E, Endou H, Kanai Y (1999) Identification and functional characterization of a Na+−independent neutral amino acid transporter with broad substrate selectivity. J Biol Chem 274:19745–19751
Babu E, Kanai Y, Chairoungdua A, Kim DK, Iribe Y, Tangtrongsup S, Jutabha P, Li Y, Ahmed N, Sakamoto S, Anzai N, Nagamori S, Endou H (2003) Identification of a novel system L amino acid transporter structurally distinct from heterodimeric amino acid transporters. J Biol Chem 278:43838–43845
Bodoy S, Martin L, Zorzano A, Palacín M, Estévez R, Bertran J (2005) Identification of LAT4, a novel amino acid transporter with system L activity. J Biol Chem 280:12002–12011
Yanagida O, Kanai Y, Chairoungdua A, Kim DK, Segawa H, Nii T, Cha SH, Matsuo H, Fukushima J, Fukasawa Y, Tani Y, Taketani Y, Uchino H, Kim JY, Inatomi J, Okayasu I, Miyamoto K, Takeda E, Goya T, Endou H (2001) Human L-type amino acid transporter 1 (LAT1): characterization of function and expression in tumor cell lines. Biochim Biophys Acta 1514:291–302
Liu XM, Reyna SV, Ensenat D, Peyton KJ, Wang H, Schafer AI, Durante W (2004) Platelet-derived growth factor stimulates LAT1 gene expression in vascular smooth muscle: role in cell growth. FASEB J 18:768–770
Kim CS, Moon IS, Park JH, Shin WC, Chun HS, Lee SY, Kook JK, Kim HJ, Park JC, Endou H, Kanai Y, Lee BK, Kim DK (2010) Inhibition of L-type amino acid transporter modulates the expression of cell cycle regulatory factors in KB oral cancer cells. Biol Pharm Bull 33:1117–1121
Yothaisong S, Dokduang H, Anzai N, Hayashi K, Namwat N, Yongvanit P, Sangkhamanon S, Jutabha P, Endou H, Loilome W (2017) Inhibition of L-type amino acid transporter 1 activity as a new therapeutic target for cholangiocarcinoma treatment. Tumor Biol 39:1010428317694545
Kobayashi H, Ishii Y, Takayama T (2005) Expression of L-type amino acid transporter 1 (LAT1) in esophageal carcinoma. J Surg Oncol 90:233–238
Nakanishi K, Ogata S, Matsuo H, Kanai Y, Endou H, Hiroi S, Tominaga S, Aida S, Kasamatsu H, Kawai T (2007) Expression of LAT1 predicts risk of progression of transitional cell carcinoma of the upper urinary tract. Virchows Arch 451:681–690
Kaira K, Oriuchi N, Imai H, Shimizu K, Yanagitani N, Sunaga N, Hisada T, Tanaka S, Ishizuka T, Kanai Y, Endou H, Nakajima T, Mori M (2008) Prognostic significance of L-type amino acid transporter 1 expression in resectable stage I-III nonsmall cell lung cancer. Br J Cancer 98:742–748
Sakata T, Ferdous G, Tsuruta T, Satoh T, Baba S, Muto T, Ueno A, Kanai Y, Endou H, Okayasu I (2009) L-type amino-acid transporter 1 as a novel biomarker for high-grade malignancy in prostate cancer. Pathol Int 59:7–18
Ichinoe M, Mikami T, Yoshida T, Igawa I, Tsuruta T, Nakada N, Anzai N, Suzuki Y, Endou H, Okayasu I (2011) High expression of L-type amino-acid transporter 1 (LAT1) in gastric carcinomas: comparison with non-cancerous lesions. Pathol Int 61:281–289
Furuya M, Horiguchi J, Nakajima H, Kanai Y, Oyama T (2012) Correlation of L-type amino acid transporter 1 and CD98 expression with triple negative breast cancer prognosis. Cancer Sci 103:382–389
Kaira K, Sunose Y, Arakawa K, Ogawa T, Sunaga N, Shimizu K, Tominaga H, Oriuchi N, Itoh H, Nagamori S, Kanai Y, Segawa A, Furuya M, Mori M, Oyama T, Takeyoshi I (2012) Prognostic significance of L-type amino-acid transporter 1 expression in surgically resected pancreatic cancer. Br J Cancer 107:632–638
Toyoda M, Kaira K, Ohshima Y, Ishioka NS, Shino M, Sakakura K, Takayasu Y, Takahashi K, Tominaga H, Oriuchi N, Nagamori S, Kanai Y, Oyama T, Chikamatsu K (2014) Prognostic significance of amino-acid transporter expression (LAT1, ASCT2, and xCT) in surgically resected tongue cancer. Br J Cancer 110:2506–2513
Kaira K, Sunose Y, Ohshima Y, Ishioka NS, Arakawa K, Ogawa T, Sunaga N, Shimizu K, Tominaga H, Oriuchi N, Itoh H, Nagamori S, Kanai Y, Yamaguchi A, Segawa A, Ide M, Mori M, Oyama T, Takeyoshi I (2013) Clinical significance of L-type amino acid transporter 1 expression as a prognostic marker and potential of new targeting therapy in biliary tract cancer. BMC Cancer 13:482
Yanagisawa N, Hana K, Nakada N, Ichinoe M, Koizumi W, Endou H, Okayasu I, Murakumo Y (2014) High expression of L-type amino acid transporter 1 as a prognostic marker in bile duct adenocarcinomas. Cancer Med 3:1246–1255
Oda K, Hosoda N, Endo H, Saito K, Tsujihara K, Yamamura M, Sakata T, Anzai N, Wempe MF, Kanai Y, Endou H (2010) L-type amino acid transporter 1 inhibitors inhibit tumor cell growth. Cancer Sci 101:173–179
Wempe MF, Rice PJ, Lightner JW, Jutabha P, Hayashi M, Anzai N, Wakui S, Kusuhara H, Sugiyama Y, Endou H (2012) Metabolism and pharmacokinetic studies of JPH203, an L-amino acid transporter 1 (LAT1) selective compound. Drug Metab Pharmacokinet 27:155–161
Toyoshima J, Kusuhara H, Wempe MF, Endou H, Sugiyama Y (2013) Investigation of the role of transporters on the hepatic elimination of an LAT1 selective inhibitor JPH203. J Pharm Sci 102:3228–3238
Hein DW, Doll MA (2012) Accuracy of various human NAT2 SNP genotyping panels to infer rapid, intermediate and slow acetylator phenotypes. Pharmacogenomics 13:31–41
Häfliger TP, Charles RP (2019) The L-type amino acid transporter LAT1—an emerging target in Cancer. Int J Mol Sci 20:2428
Wang Q, Holst J (2015) L-type amino acid transport and cancer: targeting the mTORC1 pathway to inhibit neoplasia. Am J Cancer Res 5:1281–1294
Salisbury TB, Arthur S (2018) The regulation and function of the L-type amino acid transporter 1 (LAT1) in Cancer. Int J Mol Sci 19:2373
Singh N, Ecker GF (2018) Insights into the structure, function, and ligand discovery of the large neutral amino acid transporter 1, LAT1. Int J Mol Sci 19:1278
Nakada N, Mikami T, Hana K, Ichinoe M, Yanagisawa N, Yoshida T, Endou H, Okayasu I (2014) Unique and selective expression of L-amino acid transporter 1 in human tissue as well as being an aspect of oncofetal protein. Histol Histopathol 29:217–227
Cormerais Y, Giuliano S, LeFloch R, Front B, Durivault J, Tambutte E, Massard PA, de la Ballina LR, Endou H, Wempe M, Palacin M, Parks SK, Pouyssegur J (2016) Genetic disruption of the key role of essential amino acid transport in the control of mTORC1 and tumor growth. Cancer Res 76:4481–4492
Rosilio C, Nebout M, Imbert V, Griessinger E, Neffati Z, Benadiba J, Hagenbeek T, Spits H, Reverso J, Ambrosetti D, Michiels JF, Bailly-Maitre B, Endou H, Wempe MF, Peyron JF (2015) L-type amino acid transporter 1 (LAT1): a therapeutic target supporting growth and survival of t-cell lymphoblastic lymphoma/t-cell acute lymphoblastic leukemia. Leukemia 29:1253–1266
Kaira K, Oriuchi N, Shimizu K, Ishikita T, Higuchi T, Imai H, Yanagitani N, Sunaga N, Hisada T, Ishizuka T, Kanai Y, Endou H, Nakajima T, Endo K, Mori M (2009) Evaluation of thoracic tumors with (18)F-FMT and (18)F-FDG PET-CT: a clinicopathological study. Int J Cancer 124:1152–1160
Wempe MF, Jutabha P, Kumar V, Fisher JA, Waers K, Holt MD, Dodson AM, Bautista J, Gehr DT, Backos DS, Kumar A, Rice PJ, Anzai N, Saito K, Oda K, Kanai Y, Endou H (2019) Developing selective L-Amino Acid Transport 1 (LAT1) inhibitors: A Structure-Activity Relationship overview. Med Res Arch. https://doi.org/10.18103/mra.v7i12.2014
Janpipatkul K, Suksen K, Borwornpinyo S, Jearawiriyapaisarn N, Hongeng S, Piyachaturawat P, Chairoungdua A (2014) Downregulation of LAT1 expression suppresses cholangiocarcinoma cell invasion and migration. Cell Signal 26:1668–1679
Yothaisong S, Namwat N, Yongvanit P, Khuntikeo N, Puapairoj A, Jutabha P, Anzai N, Tassaneeyakul W, Tangsucharit P, Loilome W (2017) Increase in L-type amino acid transporter 1 expression during cholangiocarcinogenesis caused by liver fluke infection and its prognostic significance. Parasitol Int 66:471–478
Sabbagh A, Darlun P, Crouau-Roy B, Poloni ES (2011) Arylamine N-acetyltransferase (NAT2) genetic diversity and traditional subsistence: a worldwide population survey. PLoS One 6:e18507
Lamarca A, Palmer DH, Wasan HS, Ross PJ, Ma YT, Arora A, Falk S, Gillmore R, Wadsley J, Patel K, Anthoney A, Maraveyas A, Waters JS, Hobbs C, Barber S, Ryder D, Ramage JK, Davies LM, Bridgewater JA, Valle JW (2019) ABC-06 | a randomised phase III, multi-Centre, open-label study of active symptom control (ASC) alone or ASC with oxaliplatin / 5-FU chemotherapy (ASC+mFOLFOX) for patients (pts) with locally advanced / metastatic biliary tract cancers (ABC) previously-treated with cisplatin/gemcitabine (CisGem) chemotherapy. J Clin Oncol 37:4003 (abstract)
Ueno M, Ikeda M, Morizane C, Kobayashi S, Ohno I, Kondo S, Okano N, Kimura K, Asada S, Namba Y, Okusaka T, Furuse J (2019) Nivolumab alone or in combination with cisplatin plus gemcitabine in Japanese patients with unresectable or recurrent biliary tract cancer: a non-randomised, multicentre, open-label, phase 1 study. Lancet Gastroenterol Hepatol 4:611–621
Acknowledgments
The authors thank Masuhiro Yoshitake and Yoshinori Bamba for their support in the NAT2 analysis.
Funding
This study was sponsored by J-Pharma Co., Ltd.
Author information
Authors and Affiliations
Contributions
Conception and design, N.O., H.E., and J.F.; Administrative support, H.E.; Provision of study materials or patients, N.O., D.N., K.K., T.K., F.N., and J.F.; Collection and assembly of data, N.O., D.N., K.K., T.K., F.N., and J.F.; Data analysis and interpretation, N.O., D.N., F.N., H.E., and J.F.; Manuscript writing, All authors.; Final approval of manuscript, All authors.
Corresponding author
Ethics declarations
Conflict of interest
Okano N. received personal fees from Merck Serono, Taiho, Eisai and J-Pharma. Naruge D. declares that he has no conflict of interest. Kawai K. declares that he has no conflict of interest. Kobayashi T. declares that he has no conflict of interest. Nagashima F. received personal fees from Taiho, Chugai, Yakult, Sumitomo Dainippon, Merck Serono, Takeda, Kyowa Hakko Kirin, Sanofi Mochida, Janssen and Nestle. Endou H. received salary from J-Pharma, and has pending patents for LAT1, JPH203 and application of JPH203 in Phase I study of solid tumors. Furuse J. received grants from J-Pharma, Taiho, Sumitomo Dainippon, Janssen, Daiichi Sankyo, MSD, Yakult, Takeda, Chugai, Ono, Astellas, Zeria, Novartis, Nanocarrier, Shionogi, Onco Therapy Science, Eli Lilly Japan, Bayer, Bristol-Myers Squibb, Merck Serono, Kyowa Hakko Kirin, Eisai, NanoCarrier, Mochida, Baxalta and Sanofi, and received personal fees from Taiho, Chugai, Yakult, Sumitomo Dainippon, Eli Lilly Japan, Astellas, Ono, Pfizer, Bayer, Novartis, Merck Serono, Takeda, Eisai, MSD, Shionogi, J-Pharma, Daiichi Sankyo, Kyowa Hakko Kirin, Sanofi, Sandoz, Otsuka, Zeria, Fujifilm, Astra Zeneca, Asahi Kasei, Shire, Mochida, Nippon Kayaku, EA pharma, Sawai and Teijin Pharma.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board and with the 1964 Helsinki declaration and its later amendments. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okano, N., Naruge, D., Kawai, K. et al. First-in-human phase I study of JPH203, an L-type amino acid transporter 1 inhibitor, in patients with advanced solid tumors. Invest New Drugs 38, 1495–1506 (2020). https://doi.org/10.1007/s10637-020-00924-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-020-00924-3