Summary
As HER2 is a client protein of the molecular chaperone Hsp90, targeting Hsp90 may be beneficial in HER2-positive breast cancer. In this study, the activity of the Hsp90 inhibitor NVP-AUY922 was assessed in HER2 overexpressing breast cancer cell lines, including two cell line models of acquired trastuzumab-resistance. The seven HER2-positive breast cancer cell lines tested showed significant sensitivity to NVP-AUY922 in vitro, with IC50 values between 6 and 17 nM. Combining NVP-AUY922 with chemotherapy did not improve response. NVP-AUY922 in combination with trastuzumab, significantly enhanced growth inhibition in three of the seven cell lines tested. In conclusion, our data shows that NVP-AUY922 displays potent anti-cancer activity in HER2-positive and trastuzumab-resistant breast cancer cells, and supports further testing of NVP-AUY922 in patients with HER2-positive breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HER2 is a member of the transmembrane receptor tyrosine kinase ErbB family. The HER2 protein is over-expressed or the gene amplified in approximately 20–25% of breast cancers [1], resulting in the HER2-positive clinical phenotype which is associated with a poor prognosis [1, 2]. Targeting HER2 with trastuzumab, a recombinant humanized monoclonal antibody, is clinically effective in the treatment of early and metastatic HER2 over-expressing breast cancer [3, 4]. Although many patients respond to trastuzumab, approximately 90% of patients with metastatic HER2 positive breast cancer develop progressive disease [5]. Resistance to trastuzumab may be mediated by one or more of the following mechanisms (a) compensatory signalling – increased signalling from HER family members [6] or other receptors (IGFIR) [7, 8], (b) activation of downstream signalling, such as the PI3K/Akt pathway [9,10,11] and (c) deletion of tumour supressors (PTEN) [12], suggesting that trastuzumab resistant tumour cells are still heavily dependent on signalling downstream of HER2.
Hsp90 is involved in the folding, assembly, stabilization and activation of more than 200 proteins, referred to as “clients”, including kinase signalling proteins, mutated signalling proteins, transcription factors, and cell cycle-regulators [13, 14]. Oncoproteins, such as HER2, Akt, and EGFR, can use the Hsp90 chaperone machinery to protect mutated and over-expressed proteins from misfolding and degradation, promoting cancer cell survival [15, 16]. Hsp90, along with co-chaperone proteins, has been reported to regulate degradation of HER2 and can interact with the kinase domain of HER2 where it is responsible for maintaining the mature protein in a state competent for dimerization and activation [17]. Thus, Hsp90 is an attractive target for anti-cancer therapies [18,19,20]. A phase II trial of tanespimycin (17-AAG) plus trastuzumab showed significant anti-cancer activity in patients with HER2-positive, metastatic breast cancer who progressed on trastuzumab [21]. Tanespimycin also showed either additive or synergistic activity in combination with a variety of chemotherapeutic agents, including docetaxel, cisplatin and irinotecan, in preclinical studies [22] and phase I clinical trials [23,24,25]. However, the development of tanespimycin as a cancer therapy has been suspended by the sponsor for non-clinical reasons [21, 26]. NVP-AUY922, a novel resorcinylic isoxazole amide, is a more potent inhibitor of Hsp90 than 17-AAG and has strong anti-tumour activity [27, 28] against gastric cancer [29], non-small cell lung cancer [30] and breast cancer in vitro and in vivo [31]. In addition, NVP-AUY922 showed anti-tumour activity in phase I studies in patients with advanced solid tumours [32] and in a phase I/II trial in patients with HER2-positive or ER-positive breast cancer [33]. Wainberg and collaborators reported that NVP-AUY922 showed a synergistic effect with trastuzumab in HER2-positive breast and gastric cancer cell lines, including in trastuzumab-conditioned models [34].
In this study, we investigated the effect of NVP-AUY922 in a panel of HER2-positive trastuzumab-sensitive and trastuzumab-resistant breast cancer cell lines.
Methods
Cells and reagents
HER2-positive breast cancer cell lines BT474, EFM-192A, SKBR3, MDA-MB-361 and HCC1954 were obtained from the American Tissue Culture Collection (Manassas, VA). BT474/Trastuzumab resistant (BT474/Tr) and SKBR3/Trastuzumab resistant (SKBR3/Tr), which were developed following continuous exposure to trastuzumab (100 μg/ml) for 9 months, were kindly provided by Dr. Dennis Slamon, UCLA [35]. All cell lines were cultured in RPMI (Sigma-Aldrich) containing 10% FCS.
NVP-AUY922 (provided by Novartis) was prepared as a 10 mM stock in dimethyl sulfoxide (DMSO). Trastuzumab (Herceptin, Genentech Inc.), docetaxel (Taxotere, Aventis), and cisplatin were obtained from the Pharmacy Department, St Vincent’s University Hospital, Dublin. 5′-deoxy-5′-fluoruridine (5’-DFUR, Sigma-Aldrich) was prepared as a 10 mM stock in DMSO.
Protein extraction
The cells, untreated or treated with 0.1, 0.5 or 1 μM NVP-AUY922 for 24 h, were washed with cold phosphate buffered saline (PBS) and lysed in RIPA buffer (Sigma-Aldrich) containing protease inhibitors (Sigma-Aldrich), 1 mM phenylmethylsulfonyl fluoride (PMSF) and 1 mM sodium orthovanadate. After 20 min incubation on ice, lysate was passed through a 21-gauge needle and centrifuged at 10000 rpm for 5 min at 4 °C. Protein quantification was carried out using the bicinchoninic acid assay (Pierce Biotechnology).
Western blotting
40 μg of proteins were solubilised in sample buffer (250 mM Tris–HCl; 10% sodium dodecyl sulfate (SDS); 5% beta-mercaptoethanol; 30% glycerol; 0.02% bromophenol blue), heated to 95 °C for 5 min and proteins were separated using Novex 4–12% polyacrylamide gels (Life Technologies). Proteins were transferred to nitrocellulose membrane (Life Technologies). The membrane was blocked with NET buffer (1.5 M NaCl; 0.05 M EDTA; 0.5 M Tris pH 7.8; 0.5% Triton X100; 2.5 g/l gelatin) at room temperature for 1 h. After overnight incubation at 4 °C with primary antibody, three washes with NET buffer were carried out, followed by incubation at room temperature with secondary antibody (anti-mouse, Sigma; anti-rabbit, Pierce Biotechnology) for 1 h. Primary antibodies used were anti-HER2 (Calbiochem), anti-Hsp90 (Santa Cruz Biotechnology), anti-Akt (Cell Signalling Technology) and anti-α-tubulin (Sigma-Aldrich). Following three washes with NET buffer and one PBS wash, protein bands were detected using Luminol (Santa Cruz Biotechnology) or ECL™ Advance western blotting detection kit (GE Healthcare). Bands were quantified using ImageJ software.
Proliferation assays
Cell proliferation assays were performed using the acid phosphatase assay. Briefly, 5 × 104 cells/well for BT474, BT474/Tr and MDA-MB-361 and 3 × 104 cells/well for EFM-192A, SKBR3, SKBR3/Tr and HCC1954 were seeded in 96-well plates. Following overnight incubation at 37 °C, drugs were added at the appropriate concentrations and incubated for 5 days at 37 °C. media was removed and cells were washed once with PBS. Acid phosphatase substrate (10 mM p-nitrophenyl-phosphate (Sigma-Aldrich) in sodium acetate buffer) was added to each well and incubated at 37 °C for 1 h. The reaction was stopped by adding 1 M NaOH. Absorbance was read at 405 nm with 620 nm as the reference wavelength. Inhibition of proliferation was calculated relative to untreated controls. IC50 values, the effective concentration of drug that inhibits 50% of growth, were determined using the Chou and Talalay equation on CalcuSyn software [36].
Statistical analysis
For NVP-AUY922 and trastuzumab combination assays, the Student’s t-test (two-tailed) was used to compare the effect of the combination with each of the single agents alone (at 10 nM each). Relationships between response to NVP-AUY922 in combination with trastuzumab and signalling pathways (from [10]), and ER status were examined using the Mann Whitney U, Spearmann Rank or Fisher’s test on StatView for Windows (version 5.0.1) (SAS Institute, Inc). P < 0.05 was considered statistically significant.
Results
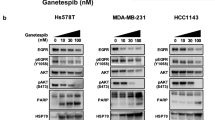
NVP-AUY922 decreases HER2 and Akt levels in HER2 positive breast cancer cell lines
The five parental HER2-positive breast cancer cell lines and the two trastuzumab resistant cell lines expressed detectable levels of HER2 and Hsp90 (Fig. 1a). Treatment with increasing doses of NVP-AUY922 resulted in a dose-dependent decrease in HER2 and Akt levels in BT474 and SKBR3 cell lines (Fig. 1b). NVP-AUY922 treatment also decreased the level of these proteins in the trastuzumab resistant cell lines, BT474/Tr and SKBR3/Tr. Hsp90 protein levels were not reduced by the inhibitor (Fig. 1b).
a Baseline expression of HER2, Hsp90, Akt, pAkt (S473/T308) and α-tubulin was measured by western blotting in six parental and two trastuzumab-resistant HER2-postive breast cancer cell lines. b Expression of HER2, Akt, Hsp90 and α-tubulin was determined following 24 h incubation with increasing doses of NVP-AUY922 (0, 0.1, 0.5 and 1 μM) in BT474, BT474/Tr, SKBR3 and SKBR3/Tr. Data is representative of triplicate experiments
NVP-AUY922 inhibits proliferation of HER2-positive breast cancer cell lines
Sensitivity to trastuzumab in the panel of HER2-positive breast cancer cell lines was assessed at 20 nM (approx 3 μg/ml) trastuzumab (Table 1). Four cell lines, BT474, EFM-192A, SKBR3 and MDA-MB-361 showed 32–48% inhibition of growth and were classified as trastuzumab sensitive. Trastuzumab did not reduce proliferation of HCC1954 cells and this cell line was classified as innately resistant to trastuzumab. Finally, we confirmed that the trastuzumab-conditioned cell lines, BT474/Tr and SKBR3/Tr, show reduced response to trastuzumab compared to the parental cell lines, with 8 and 25% growth inhibition at 20 nM, respectively.
NVP-AUY922 inhibited the growth of the 7 HER2-positive breast cancer cell lines tested, at clinically achievable concentrations (IC50 values ranging from 6 to 17 nM, Table 1), including the innately resistant HCC1954 cells and the two trastuzumab-conditioned cell lines, BT474/Tr and SKBR3/Tr. We also tested combinations of NVP-AUY922 with standard chemotherapy agents. The combination of NVP-AUY922 with each of the chemotherapy agents (docetaxel, cisplatin, 5-DFUR) did not improve response compared to NVP-AUY922 alone in BT474 cells (Fig. 2). Similiar results were obtained for SKBR3, HCC1954 and MDA-MB-361 cells (Supplementary figure 1).
Enhanced anti-proliferative effect of NVP-AUY922 in combination with trastuzumab
To investigate the impact of NVP-AUY922 on trastuzumab response, proliferation assays were performed with NVP-AUY922 or trastuzumab alone, and in combination in the panel of cell lines. In 3 of the 7 cell lines tested, the combination of NVP-AUY922 and trastuzumab produced enhanced response compared to the single agents, including both the parental BT474 and the trastuzumab-resistant model BT474/Tr, and the EFM-192A cells (Fig. 3, Table 2). In the other 4 cell lines, combined treatment did not enhance response, compared to NVP-AUY922 alone.
a SKBR3, b SKBR3/Tr, c MDA-MB-361, d HCC1954, e BT474, f BT474/Tr, g EFM-192A were incubated with increasing doses of NVP-AUY922 (starting dilution at 20 nM), trastuzumab (starting dilution at 20 nM), or the combination of both drugs (1:1) for 5 days. Cell viability was determined using the acid phosphatase method. Data represents the mean +/− SD of triplicate independent experiments. * P < 0.05
Response to NVP-AUY922 and trastuzumab and Hsp90 client proteins
Levels of Hsp90 protein did not correlate with response to NVP-AUY922 (p = 0.43) or combined treatment with trastuzumab and NVP-AUY922 (Supplementay table 1). Based on the known client proteins of Hsp90 and their potential interaction with HER2 signalling, we examined the relationship between response to NVP-AUY922 alone or in combination with trastuzumab, and ER expression status, HER protein levels, IGF1R expression levels, and the PI3K/Akt signalling pathway. Data was available for 5 of the 7 cell lines [10]. Although all of the cell lines were sensitive to NVP-AUY922, greater sensitivity correlated with lower levels of HER2 (p = 0.045, r = 0.995). Total HER2 levels did not correlate with response to combined trastuzumab and NVP-AUY922 treatment. No other correlations were observed with response to NVP-AUY922 alone or in combination with trastuzumab (Supplementary table 1).
Discussion
The prognosis for HER2-positive breast cancer has significantly improved since the introduction of trastuzumab [37] and more recently lapatinib [38], pertuzumab [39] and T-DM1 [40]. Despite these advances, resistance to HER2-targeted therapies remains a clinical problem, particularly for metastatic disease. Hsp90 is an emerging target with potential in HER2-positive breast cancer as it is responsible for protein stabilization of multiple proteins involved in oncogenesis, including HER2. Hsp90 inhibition results in degradation of HER2 via ubiquitinylation and lysosomal pathways [41].
In this study, we analyzed the effect of combining NVP-AUY922, an Hsp90 inhibitor already described as having potent anti-tumour activity [27,28,29,30,31,32, 42], with trastuzumab or standard chemotherapy agents in HER2-positive breast cancer cell lines. Consistent with a previously published study [34], we showed that NVP-AUY922 has potent anti-proliferative effects in five HER2-positive breast cancer cell lines (trastuzumab-sensitive BT474, EFM-192A, SKBR3, MDA-MB-361 and the innately trastuzumab-resistant HCC1954 cells), displaying activity in the nanomolar range which is within the achievable range of plasma concentrations reported clinically. In patients administered 70 mg/m2, the mean plasma levels of NVP-AUY922 after 24 h were approximately 60 ng/mL (approx. 130 nM) [32].
We further investigated whether Hsp90 inhibition with NVP-AUY922 would have activity in two trastuzumab-resistant variants of the HER2-positive breast cancer cell lines BT474 (BT474/Tr) and SKBR3 (SKBR3/Tr) [35]. In agreement with other studies [43,44,45], acquired trastuzumab-resistant cell lines were also highly sensitive to Hsp90 inhibition. Consistent with previously published results [44], we found that NVP-AUY922 decreased the levels of HER2 in both trastuzumab sensitive and - resistant cell lines. Scaltriti and collaborators suggested that the trastuzumab-resistant cells were still dependent on the HER2 signalling pathway, which may in part explain the observed sensitivity to Hsp90 inhibition by IPI-504 as shown in their study [44] and NVP-AUY922 in our study. In addition, the combination of NVP-AUY922 with trastuzumab enhanced response in both BT474 and BT474/Tr cell lines as previously observed [34]. We also found enhanced response to the combination in EFM-192A cells but not in SKBR3, SKBR3/Tr, MDA-MB-361 and HCC1954 cell lines. In an attempt to uncover the differential response to combined treatment with trastuzumab plus NVP-AUY922 we examined the relationship between response and a number of known Hsp90 charperones. However, no correlations were observed between enhanced response to the combination and expression of ER, HER family proteins, IGF1R or Akt. Extending the analysis to a larger panel of HER2-positive breast cell lines may help to elucidate potential predictive biomarkers of enhanced response to combined trastuzumab and NVP-AUY922 treatment.
Previous studies have shown that NVP-AUY922 inhibits the growth of BT474 xenograft tumours in mice [27]. Combined NVP-AUY922 and trastuzumab produces enhanced anti-tumour activity in vivo in HER2-amplified gastric cancer xenografts, including a trastuzumab-conditioned model [34]. However, in xenografts generated with BT474 trastuzumab-resistant cells, combining trastuzumab with the Hsp90 inhibitor IPI-504 did not enhance tumour regression compared to IPI-504 alone [44]. NVP-AUY922 has not yet been tested in combination with trastuzumab in vivo in an acquired trastuzumab-resistant breast cancer model. A phase Ib/II study of NVP-AUY922 in combination with trastuzumab, in trastuzumab-refractory breast cancer, reported an overall response rate (complete or partial responses) of 22.0% (9/41) while 48.8% (20/41) of patients had stable disease [46].
Combining NVP-AUY922 with chemotherapy provided no additional anti-proliferative benefit compared to NVP-AUY922 alone in any of the cell lines tested. However, as NVP-AUY922 has been shown to induce G1 and/or G2-M phase cell cycle arrest in breast cancer cells [27, 34], the sequence of administration of NVP-AUY922 and chemotherapy is likely to influence the effects of combined treatment. Munster and collaborators previously showed that Hsp90 inhibition by 17-AAG, sensitized breast cancer cells to chemotherapy but the effect was schedule dependent and also concentration dependent, with lower concentrations required to sensitze HER2-positive breast cancer cells [22]. A phase I study of NVP-AUY922 in combination with trastuzumab and paclitaxel in patients with trastuzumab-refractory HER2-positive metastatic breast cancer, reported an overall response rate of 22% (2/9) and stable disease was observed in 56% (5/9) of patients [47].
In summary, our results support the clinical development of NVP-AUY922 as a potent anti-cancer therapy in HER2-positive and trastuzumab-resistant breast cancer. In addition, combined targeting of HER2 with Hsp90 inhibition and trastuzumab represents a promising treatment option. The lack of synergy observed for combinations of NVP-AUY922 with chemotherapy does not favour clinical evaluation of concurrent administration of NVP-AUY922 with chemotherapy. Alternative scheduling or combinations with other targeted therapies warrants further investigation.
References
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235(4785):177–182
Menard S, Fortis S, Castiglioni F, Agresti R, Balsari A (2001) HER2 as a prognostic factor in breast cancer. Oncology 61(Suppl 2):67–72
Buzdar AU, Ibrahim NK, Francis D, Booser DJ, Thomas ES, Theriault RL, Pusztai L, Green MC, Arun BK, Giordano SH, Cristofanilli M, Frye DK, Smith TL, Hunt KK, Singletary SE, Sahin AA, Ewer MS, Buchholz TA, Berry D, Hortobagyi GN (2005) Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol 23(16):3676–3685
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C, Cameron D, Dowsett M, Barrios CH, Steger G, Huang CS, Andersson M, Inbar M, Lichinitser M, Lang I, Nitz U, Iwata H, Thomssen C, Lohrisch C, Suter TM, Ruschoff J, Suto T, Greatorex V, Ward C, Straehle C, McFadden E, Dolci MS, Gelber RD (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353(16):1659–1672
Gullo G, Zuradelli M, Sclafani F, Santoro A, Crown J (2012) Durable complete response following chemotherapy and trastuzumab for metastatic HER2-positive breast cancer. Ann Oncol Off J Eur Soc Med Oncol/ESMO 23(8):2204–2205. https://doi.org/10.1093/annonc/mds221
Agus DB, Akita RW, Fox WD, Lewis GD, Higgins B, Pisacane PI, Lofgren JA, Tindell C, Evans DP, Maiese K, Scher HI, Sliwkowski MX (2002) Targeting ligand-activated ErbB2 signaling inhibits breast and prostate tumor growth. Cancer Cell 2(2):127–137
Lu Y, Zi X, Zhao Y, Mascarenhas D, Pollak M (2001) Insulin-like growth factor-I receptor signaling and resistance to trastuzumab (Herceptin). J Natl Cancer Inst 93(24):1852–1857
Nahta R, Yuan LX, Zhang B, Kobayashi R, Esteva FJ (2005) Insulin-like growth factor-I receptor/human epidermal growth factor receptor 2 heterodimerization contributes to trastuzumab resistance of breast cancer cells. Cancer Res 65(23):11118–11128
Chan CT, Metz MZ, Kane SE (2005) Differential sensitivities of trastuzumab (Herceptin)-resistant human breast cancer cells to phosphoinositide-3 kinase (PI-3K) and epidermal growth factor receptor (EGFR) kinase inhibitors. Breast Cancer Res Treat 91(2):187–201
O'Brien NA, Browne BC, Chow L, Wang Y, Ginther C, Arboleda J, Duffy MJ, Crown J, O'Donovan N, Slamon DJ Activated phosphoinositide 3-kinase/AKT signaling confers resistance to trastuzumab but not lapatinib. Mol Cancer Ther 9(6):1489–1502
Yakes FM, Chinratanalab W, Ritter CA, King W, Seelig S, Arteaga CL (2002) Herceptin-induced inhibition of phosphatidylinositol-3 kinase and Akt is required for antibody-mediated effects on p27, cyclin D1, and antitumor action. Cancer Res 62(14):4132–4141
Nagata Y, Lan KH, Zhou X, Tan M, Esteva FJ, Sahin AA, Klos KS, Li P, Monia BP, Nguyen NT, Hortobagyi GN, Hung MC, Yu D (2004) PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell 6(2):117–127
Messaoudi S, Peyrat JF, Brion JD, Alami M Heat-shock protein 90 inhibitors as antitumor agents: a survey of the literature from 2005 to 2010. Expert Opin Ther Pat 21(10):1501–1542
Wandinger SK, Richter K, Buchner J (2008) The Hsp90 chaperone machinery. J Biol Chem 283(27):18473–18477
Whitesell L, Lindquist SL (2005) HSP90 and the chaperoning of cancer. Nat Rev Cancer 5(10):761–772
Pratt WB, Toft DO (2003) Regulation of signaling protein function and trafficking by the hsp90/hsp70-based chaperone machinery. Exp Biol Med (Maywood) 228(2):111–133
Citri A, Gan J, Mosesson Y, Vereb G, Szollosi J, Yarden Y (2004) Hsp90 restrains ErbB-2/HER2 signalling by limiting heterodimer formation. EMBO Rep 5(12):1165–1170
Hahn JS (2009) The Hsp90 chaperone machinery: from structure to drug development. BMB Rep 42(10):623–630
Richardson PG, Mitsiades CS, Laubach JP, Lonial S, Chanan-Khan AA, Anderson KC Inhibition of heat shock protein 90 (HSP90) as a therapeutic strategy for the treatment of myeloma and other cancers. Br J Haematol 152(4):367–379
Trepel J, Mollapour M, Giaccone G, Neckers L Targeting the dynamic HSP90 complex in cancer. Nat Rev Cancer 10(8):537–549
Modi S, Stopeck A, Linden H, Solit D, Chandarlapaty S, Rosen N, D'Andrea G, Dickler M, Moynahan ME, Sugarman S, Ma W, Patil S, Norton L, Hannah AL, Hudis C HSP90 inhibition is effective in breast cancer: a phase II trial of tanespimycin (17-AAG) plus trastuzumab in patients with HER2-positive metastatic breast cancer progressing on trastuzumab. Clin Cancer Res 17(15):5132–5139
Munster PN, Basso A, Solit D, Norton L, Rosen N (2001) Modulation of Hsp90 function by ansamycins sensitizes breast cancer cells to chemotherapy-induced apoptosis in an RB- and schedule-dependent manner. See: Sausville EA Combining cytotoxics and 17-allylamino, 17-demethoxygeldanamycin: sequence and tumor biology matters. Clin Cancer Res 7(8):2228–2236
Hubbard J, Erlichman C, Toft DO, Qin R, Stensgard BA, Felten S, Ten Eyck C, Batzel G, Ivy SP, Haluska P Phase I study of 17-allylamino-17 demethoxygeldanamycin, gemcitabine and/or cisplatin in patients with refractory solid tumors. Invest New Drugs 29(3):473–480
Iyer G, Morris MJ, Rathkopf D, Slovin SF, Steers M, Larson SM, Schwartz LH, Curley T, DeLaCruz A, Ye Q, Heller G, Egorin MJ, Ivy SP, Rosen N, Scher HI, Solit DB A phase I trial of docetaxel and pulse-dose 17-allylamino-17-demethoxygeldanamycin in adult patients with solid tumors. Cancer Chemother Pharmacol 69(4):1089–1097
Tse AN, Klimstra DS, Gonen M, Shah M, Sheikh T, Sikorski R, Carvajal R, Mui J, Tipian C, O'Reilly E, Chung K, Maki R, Lefkowitz R, Brown K, Manova-Todorova K, Wu N, Egorin MJ, Kelsen D, Schwartz GK (2008) A phase 1 dose-escalation study of irinotecan in combination with 17-allylamino-17-demethoxygeldanamycin in patients with solid tumors. Clin Cancer Res 14(20):6704–6711
Arteaga CL Why is this effective HSP90 inhibitor not being developed in HER2+ breast cancer? Clin Cancer Res 17(15):4919–4921
Eccles SA, Massey A, Raynaud FI, Sharp SY, Box G, Valenti M, Patterson L, de Haven BA, Gowan S, Boxall F, Aherne W, Rowlands M, Hayes A, Martins V, Urban F, Boxall K, Prodromou C, Pearl L, James K, Matthews TP, Cheung KM, Kalusa A, Jones K, McDonald E, Barril X, Brough PA, Cansfield JE, Dymock B, Drysdale MJ, Finch H, Howes R, Hubbard RE, Surgenor A, Webb P, Wood M, Wright L, Workman P (2008) NVP-AUY922: a novel heat shock protein 90 inhibitor active against xenograft tumor growth, angiogenesis, and metastasis. Cancer Res 68(8):2850–2860
Oude Munnink TH, Korte MA, Nagengast WB, Timmer-Bosscha H, Schroder CP, Jong JR, Dongen GA, Jensen MR, Quadt C, Hooge MN, Vries EG (89)Zr-trastuzumab PET visualises HER2 downregulation by the HSP90 inhibitor NVP-AUY922 in a human tumour xenograft. Eur J Cancer 46(3):678–684
Lee KH, Lee JH, Han SW, Im SA, Kim TY, Oh DY, Bang YJ Antitumor activity of NVP-AUY922, a novel heat shock protein 90 inhibitor, in human gastric cancer cells is mediated through proteasomal degradation of client proteins. Cancer Sci 102(7):1388–1395
Garon EB, Finn RS, Hamidi H, Dering J, Pitts S, Kamranpour N, Desai AJ, Hosmer W, Ide S, Avsar E, Jensen MR, Quadt C, Liu M, Dubinett SM, Slamon DJ The HSP90 inhibitor NVP-AUY922 potently inhibits non-small cell lung cancer growth. Mol Cancer Ther 12(6):890–900
Jensen MR, Schoepfer J, Radimerski T, Massey A, Guy CT, Brueggen J, Quadt C, Buckler A, Cozens R, Drysdale MJ, Garcia-Echeverria C, Chene P (2008) NVP-AUY922: a small molecule HSP90 inhibitor with potent antitumor activity in preclinical breast cancer models. Breast Cancer Res 10(2):R33
Sessa C, Shapiro GI, Bhalla KN, Britten C, Jacks KS, Mita M, Papadimitrakopoulou V, Pluard T, Samuel TA, Akimov M, Quadt C, Fernandez-Ibarra C, Lu H, Bailey S, Chica S, Banerji U First-in-human phase I dose-escalation study of the HSP90 inhibitor AUY922 in patients with advanced solid tumors. Clin Cancer Res 19(13):3671–3680
Gaykema SB, Schroder CP, Vitfell-Rasmussen J, Chua S, Oude Munnink TH, Brouwers AH, Bongaerts AH, Akimov M, Fernandez-Ibarra C, Lub-de Hooge MN, de Vries EG, Swanton C, Banerji U (2014) 89Zr-trastuzumab and 89Zr-bevacizumab PET to evaluate the effect of the HSP90 inhibitor NVP-AUY922 in metastatic breast cancer patients. Clin Cancer Res 20(15):3945–3954. https://doi.org/10.1158/1078-0432.CCR-14-0491
Wainberg ZA, Anghel A, Rogers AM, Desai AJ, Kalous O, Conklin D, Ayala R, O'Brien NA, Quadt C, Akimov M, Slamon DJ, Finn RS Inhibition of HSP90 with AUY922 induces synergy in HER2-amplified trastuzumab-resistant breast and gastric cancer. Mol Cancer Ther 12(4):509–519
Konecny GE, Pegram MD, Venkatesan N, Finn R, Yang G, Rahmeh M, Untch M, Rusnak DW, Spehar G, Mullin RJ, Keith BR, Gilmer TM, Berger M, Podratz KC, Slamon DJ (2006) Activity of the dual kinase inhibitor lapatinib (GW572016) against HER-2-overexpressing and trastuzumab-treated breast cancer cells. Cancer Res 66(3):1630–1639
Reynolds CP, Maurer BJ (2005) Evaluating response to antineoplastic drug combinations in tissue culture models. Methods Mol Med 110:173–183
Slamon D, Pegram M (2001) Rationale for trastuzumab (Herceptin) in adjuvant breast cancer trials. Semin Oncol 28(1 Suppl 3):13–19
Geyer CE, Forster J, Lindquist D, Chan S, Romieu CG, Pienkowski T, Jagiello-Gruszfeld A, Crown J, Chan A, Kaufman B, Skarlos D, Campone M, Davidson N, Berger M, Oliva C, Rubin SD, Stein S, Cameron D (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355(26):2733–2743
Baselga J, Cortes J, Kim SB, Im SA, Hegg R, Im YH, Roman L, Pedrini JL, Pienkowski T, Knott A, Clark E, Benyunes MC, Ross G, Swain SM Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med 366(2):109–119
Krop IE, Beeram M, Modi S, Jones SF, Holden SN, Yu W, Girish S, Tibbitts J, Yi JH, Sliwkowski MX, Jacobson F, Lutzker SG, Burris HA Phase I study of trastuzumab-DM1, an HER2 antibody-drug conjugate, given every 3 weeks to patients with HER2-positive metastatic breast cancer. J Clin Oncol 28(16):2698–2704
Raja SM, Clubb RJ, Bhattacharyya M, Dimri M, Cheng H, Pan W, Ortega-Cava C, Lakku-Reddi A, Naramura M, Band V, Band H (2008) A combination of Trastuzumab and 17-AAG induces enhanced ubiquitinylation and lysosomal pathway-dependent ErbB2 degradation and cytotoxicity in ErbB2-overexpressing breast cancer cells. Cancer Biol Ther 7(10):1630–1640
Stingl L, Stuhmer T, Chatterjee M, Jensen MR, Flentje M, Djuzenova CS Novel HSP90 inhibitors, NVP-AUY922 and NVP-BEP800, radiosensitise tumour cells through cell-cycle impairment, increased DNA damage and repair protraction. Br J Cancer 102(11):1578–1591
Leow CC, Chesebrough J, Coffman KT, Fazenbaker CA, Gooya J, Weng D, Coats S, Jackson D, Jallal B, Chang Y (2009) Antitumor efficacy of IPI-504, a selective heat shock protein 90 inhibitor against human epidermal growth factor receptor 2-positive human xenograft models as a single agent and in combination with trastuzumab or lapatinib. Mol Cancer Ther 8(8):2131–2141
Scaltriti M, Serra V, Normant E, Guzman M, Rodriguez O, Lim AR, Slocum KL, West KA, Rodriguez V, Prudkin L, Jimenez J, Aura C, Baselga J Antitumor activity of the Hsp90 inhibitor IPI-504 in HER2-positive trastuzumab-resistant breast cancer. Mol Cancer Ther 10(5):817–824
Zsebik B, Citri A, Isola J, Yarden Y, Szollosi J, Vereb G (2006) Hsp90 inhibitor 17-AAG reduces ErbB2 levels and inhibits proliferation of the trastuzumab resistant breast tumor cell line JIMT-1. Immunol Lett 104(1–2):146–155
Kong A, Rea D, Ahmed S, Beck JT, Lopez Lopez R, Biganzoli L, Armstrong AC, Aglietta M, Alba E, Campone M, Hsu Schmitz SF, Lefebvre C, Akimov M, Lee SC Phase 1B/2 study of the HSP90 inhibitor AUY922 plus trastuzumab in metastatic HER2-positive breast cancer patients who have progressed on trastuzumab-based regimen. Oncotarget 7(25):37680–37692
Jhaveri K, Wang R, Teplinsky E, Chandarlapaty S, Solit D, Cadoo K, Speyer J, D'Andrea G, Adams S, Patil S, Haque S, O'Neill T, Friedman K, Esteva FJ, Hudis C, Modi S A phase I trial of ganetespib in combination with paclitaxel and trastuzumab in patients with human epidermal growth factor receptor-2 (HER2)-positive metastatic breast cancer. Breast Cancer Res 19(1):89
Funding
This research was supported by funding from the Health Research Board (CSA/2007/11), Science Foundation Ireland (08/SRC/B1410), the Cancer Clinical Research Trust/The Caroline Foundation and the Irish Cancer Society Collaborative Cancer Research Centre Breast-Predict (CCRC13GAL). “The opinions, findings and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the Irish Cancer Society.”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Alexandra Canonici, Zulfiqar Qadir, Neil T. Conlon, Alex J. Eustace, Neil A. O’Brien and Naomi Walsh declare that they have no conflicts of interest in regard to this article. John Crown, Denis M. Collins and Norma O’Donovan have recieved research funding from Roche Pharmaceuticals. This article does not contain any studies with either human or animal participants performed by any of the authors.
Electronic supplementary material
Supplementary fig 1
Effect of NVP-AUY922 in combination with chemotherapy on proliferation of HER2-positive breast cancer cell lines. HER2-positive breast cancer cell lines were incubated with increasing doses of NVP-AUY922 (starting dilution at 20 nM) in combination with chemotherapy agents (docetaxel (50:1), cisplatin (1:500) or 5-DFUR (1:500)) for 5 days. Data represents the mean +/− SD of triplicate independent experiments. (GIF 148 kb)
Supplementary Table 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Canonici, A., Qadir, Z., Conlon, N.T. et al. The HSP90 inhibitor NVP-AUY922 inhibits growth of HER2 positive and trastuzumab-resistant breast cancer cells. Invest New Drugs 36, 581–589 (2018). https://doi.org/10.1007/s10637-017-0556-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-017-0556-7