Summary
Background The prognosis of patients with metastatic carcinoma of the biliary tract (mBTC) is poor and a systemic therapy with gemcitabine and platinum-based is the gold standard. The addition of bevacizumab to the chemotherapy might increase patients’ survival. Our aim was to assess and compare the efficacy of GEMOX (gemcitabine and oxaliplatin regimen) plus bevacizumab to GEMOX alone in mBTC. Methods Patients with mBTC who received the GEMOX-bevacizumab (n = 32; Group A) or GEMOX (n = 25; Group B) regimen as first-line treatment were compared. Treatment was repeated every two weeks until disease progression or unacceptable adverse effects occurred. The primary evaluation criterion was the progression-free survival (PFS). Results A quarter of patients (8/32) from Group A and a fifth of patients (13/25) from Group B had an objective response. The median PFS was 6.48 months and 3.72 months in Group A and B, respectively (p = 0.049). The median OS was 11.31 months and 10.34 months in Group A and B, respectively. Grade 3/4 sepsis was identified in 9.4% and 12% in Group A and B, respectively, (p = 0.64). Conclusion In mBTC, the addition of bevacizumab to GEMOX increased the progression-free survival and was associated with manageable toxicity. These data pave the way for further evaluation of antiangiogenic agents in mBTC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Backgrounds
Biliary tract cancers (BTC) are the second most common primary liver cancer after hepatocellular carcinoma [1]. They rise from the epithelial lining of the gallbladder or from the bile ducts, and carry a poor prognosis. BTC include gallbladder carcinoma, intrahepatic perihilar and extrahepatic cholangiocarcinoma. BTC, intrahepatic cholangiocarcinoma excluded, represent more than 11.000 new cases per year in the United States [2]. BTC are more frequently diagnosed at an advanced stage, characterized by a vascular invasion, extensive regional lymph node metastases and/or the presence of distant metastases. Locations of metastases are the liver, the lungs, the bones and the peritoneum. Surgery appears as the only curative treatment in BTC [3]. In advanced disease, surgery is abandoned in favor of chemotherapy [4].
Based on a pooled analysis of 104 trials which included more than 2800 patients, the combination of gemcitabine and platinum drugs has been considered as the “gold standard” in first-line treatment for patients with metastatic cholangiocarcinoma (mBTC) [5]. The addition of a platinum therapy to gemcitabine was reinforced by the ABC-02 study which confirmed the superiority of GEMCIS (gemcitabine plus cisplatin regimen) to gemcitabine alone in locally-advanced or mBTC [6]. No differences between platinum drugs have been raised from the pooled analysis, suggesting the non-inferiority of oxaliplatin compared to cisplatin. Nevertheless, the combination of gemcitabine to the oxaliplatin regimen (GEMOX) has already been identified as a well-tolerated association even in frail patients [7]. In mBTC, phase II studies confirmed the feasibility of the combination and identified an anti-tumor activity with an objective response rate (stable disease + tumor response) allowing a median overall survival of 12 months in up to 50% of patients [8, 9]. These data paved the way for new therapeutic agents, which would improve the survival of patients.
Vascular endothelial growth factor (VEGF) is one of the most important factors of angiogenesis and also a key regulator in pathological angiogenesis. VEGF expression has been detected in mBTC, and correlates with advanced disease stage and poor prognosis [10]. The addition of an antiangiogenic therapy to the chemotherapy resulted in a synergistic effect. There is an overexpression of neoangiogenesis in mBTC. Human BTC express both b-Fibroblast Growth Factor (b-FGF) and VEGF but not as autocrine growth factors but as angiogenic factors [11]. The hyperactivation of the angiogenic pathway highlighted the hypothetical usefulness of an antiangiogenic therapy being associated with the chemotherapy. Bevacizumab, a recombinant humanised monoclonal antibody against VEGF, is an important therapeutic agent in cancers [12, 13]. The normalization of the tumor vascularization has been suggested as a new objective to improve survival [14, 15]. In a phase II non-comparative study, the addition of bevacizumab to GEMOX was associated with a 7-month median PFS with tolerable safety in mBTC [15]. The aim of our study was to assess and compare the efficacy of GEMOX plus bevacizumab to GEMOX alone in mBTC.
Methods
The medical records of patients with mBTC having received the GEMOX regimen with or without bevacizumab as first-line treatment between July 2006 and January 2016 in our institution were retrospectively reviewed. This exploratory analysis was approved by the local ethical committee and complies with the standards of the Declaration of Helsinki.
Study design and participants
In this open-label retrospective study, we recruited patients with mBTC from Cochin Teaching Hospital, France. Patients were eligible if they were 18 years of age; had a histologically- or cytologically- confirmed mBTC, including gallbladder, intrahepatic and extrahepatic bile ducts, measurable or assessable disease according to Response Evaluation Criteria in Solid Tumors (RECIST 1.1) [16], and adequate renal function (creatinine clearance <40 ml/min) as well as bone marrow function. Biliary tract obstruction was adequately treated over the course of the study. Patients were excluded if they had any contraindications to receive bevacizumab, such as clinically significant cardiovascular disease, uncontrolled hypertension, recent myocardial infarction, unstable angina, or congestive heart failure assessed as a grade II or above according to the New York Heart Association. From September 2011 to January 2016, 32 patients with mBTC received the GEMOX plus bevacizumab regimen as first-line treatment (Group A). In a retrospective analysis, from July 2006 to August 2011, 29 patients with mBTC who received the GEMOX regimen as first-line treatment were identified (Fig. 1). Of these patients, 25 would have been able to receive bevacizumab and were considered as the control group (Group B).
Treatment schedule and toxicity assessment
Patients received 1.000 mg/m2 gemcitabine as a 30-min infusion on day 1, followed by 100 mg/m2 oxaliplatin as a 2-h infusion on the same day (GEMOX regimen). The treatment was repeated every 2 weeks until disease progression or unacceptable toxicity. In Group A, the bevacizumab was added to the GEMOX regimen at a fixed dose of 5 mg/kg every 2 weeks. In patients with mBTC, the choice of giving GEMOX plus bevacizumab as a first-line palliative therapy was related to a multidisciplinary decision based on phase II studies [8, 9].
As per previously published, chemotherapy was administered at reduced doses if any severe adverse events related to the study drug occurred, and in frail patients [17]. At baseline, patients had a physical examination, a laboratory assessment (haematological analysis, hepatic and renal function, and baseline serum concentrations of CA 19–9) and radiological studies including contrast-enhanced CT scans of the chest, abdomen, and pelvis. Tolerance was assessed at each cycle and tumor response every 6 cycles. Body weight, performance status and toxicities were recorded at each cycle or visit. Response and progression were assessed using the RECIST 1.1. Treatment was continued until disease progression, unacceptable toxicity, or patient refusal. Toxicity was assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0 (NCI-CTCAE v4.0) and the oxaliplatin-specific scale for peripheral neuropathy [18]. None of the patients received granulocyte colony-stimulating factor or erythropoietin as primary prevention. If non-neurological grade 3–4 toxicity occurred, the subsequent cycle was administered only after recovery and the treatment dose was adjusted (gemcitabine dose was reduced to 800 mg/m2 and oxaliplatin dose was reduced to 85 mg/m2). Furthermore, the oxaliplatin dose was reduced in case of prolonged (14 days or longer) paresthesia, temporary (7–14 days) painful paresthesia and/or functional impairment. In the event of persistent (14 days or longer) painful paresthesia and/or functional impairment, oxaliplatin was omitted from the regimen until recovery. Bevacizumab was maintained at 5 mg/kg every cycle. In the case of proteinuria, treatment with GEMOX-bevacizumab was interrupted until protein quantity was lower than 2 g per day. Bevacizumab was discontinued in patients who developed uncontrolled grade 3 hypertension or any grade 4 hypertension, proteinuria, bleeding, thromboembolic event, or bowel perforation. If toxicities were related to gemcitabine or oxaliplatin, patients could receive bevacizumab alone.
Efficacy assessment
Tumor evaluation was performed every four or six cycles of treatment, or before if clinically indicated, according to RECIST v1.1 [16]. Progression-Free Survival (PFS) was measured from the date of first treatment administration to the date of evidence of disease progression or death. Overall Survival (OS) was measured from the date of first treatment administration to the date of death or last follow-up.
Statistical analysis
Descriptive statistics [median, ranges, 95% confidence intervals (95%CI)] were used to report patients baseline characteristics, and treatment-induced adverse events. Comparisons between Group A and B were performed using Fisher’s exact test, Chi-square test with Yates correction, or Wilcoxon’s test when appropriate. Survival analyses were performed using the Kaplan–Meier method with the log-rank test. A p value below 0.05 was considered statistically significant. Calculations were performed using the NCCS™ 2007 software (NCCS, Kaysville, UT).
Results
A total of 57 patients with mBTC were enrolled in the study, among whom 32 received GEMOX plus bevacizumab (Group A) and 25 GEMOX alone (Group B). Median age was 59.7 years (range: 54.1–66.7) and 62.9 years (range: 55.7–71.4) in Group A and B, respectively. Patients’ and disease clinical characteristics at baseline are summarized in Table 1. No statistical differences between the two groups were identified considering the age, gender, ECOG performance status, body mass index, primary tumor site, or the tumor extension except for peritoneum extensions which were more frequently observed in Group A (28% versus 4%; p = 0.04). Patients’ biological characteristics at baseline are summarized in Table 2. No statistical differences between the two groups were identified considering the biological results, ACE or CA 19–9. One patient from each group had undergone local treatment (radiofrequency) before initiation of chemotherapy. Nineteen per cent and 32% of patients had initial surgery at the primary site in Group A and B, respectively (p = 0,349).
Patients from Group A and B completed a median of 10 (range: 4–28) and 6 cycles (range: 1–44), respectively. The median follow-up duration was 12.97 months (range: 4–32) and 14.45 months (range: 2–52) in Group A and B, respectively. At the time of analysis, 4 patients were still receiving treatment in Group A and none in Group B. Patients experienced grade 1–4 asthenia in 97% and 100% in Group A and B, respectively. Asthenia grade 3–4 affected 12.5% of patients in Group A and 24% in Group B (p = 0.31). Treatment-induced grade > 1 toxicities are summarized in Table 3. No toxic death occurred. The overall incidence of grade 3–4 adverse events was 34.4% and 40% in Group A and B, respectively (p = 0.78). Specific grade 3–4 bevacizumab-related adverse events included grade 3 hypertension (6%), grade 4 cardiac ischaemia (3%), grade 3 proteinuria (6%), perforation (6%), grade 3 thrombosis (3%) and grade 3 bleeding events (3%). All patients with a perforation had a gallbladder adenocarcinoma and experienced a gallbladder perforation.
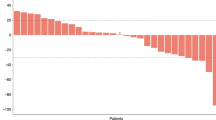
The proportions of patients who achieved an objective response (complete or partial response) and disease control were similar between the two treatment groups (69% and 52%; p = 0.532). A quarter of patients (8/32) from Group A and a fifth of patients (13/25) from Group B had an objective response. Tumor response and survival rates are indicated in Table 4. Forty one per cent of patients from Group A and 32% from Group B achieved a disease control. The median PFS was 6.48 months (range: 3–32) and 3.72 months (range: 1–39) in Group A and B, respectively (p = 0.049; Fig. 2a). The median OS was 11.31 months (range: 3–32) and 10.34 months (range: 2–52) in Group A and B, respectively (p = 0.44; Fig. 2b). Patients discontinued the treatment for disease progression in 89% and 93% of cases in Group A and B, respectively. Fifty percent of patients from Group A and 40% from Group B received second-line therapy after disease progression.
Discussion
In the present study, we identified that the addition of an antiangiogenic therapy improved PFS in mBTC despite the absence of any significant improvement in OS. The addition of bevacizumab was not associated with a significant additional toxicity. The prognosis of patients with mBTC deserved further study to improve overall survival. Our study pinpointed an increased toxicity in patients with gallbladder adenocarcinoma in Group A and reinforced the idea of the heterogeneity of BTC as previously reported in the work of Lee [19]. The addition of bevacizumab was associated with a trend for an improved survival. In our study, the overall survival was higher than those of previously published studies [7] [20]. In non-sarcopenic patients receiving the GEMOX regimen, the median PFS and OS were significantly lower than the ones we observed in Group B [7]. Furthermore, the addition of a tyrosine kinases inhibitor with an antiangiogenic effect, erlotinib, failed to improve OS associated with the GEMOX regimen (9.5 months) [20]. In our study, we identified a two-month longer survival than Lee et al.
In our study, the primary endpoint was significantly longer in Group A than in Group B (6.48 versus 3.72 months; p = 0.049). The benefit in PFS of the addition of bevacizumab in Group A was not associated with a significant benefit in OS. However, Mancuso et al. identified that tumor blood vessels undergo rapid regression when VEGF signaling is inhibited [21]. This study also reports a phenomenon of rapid revascularization of tumors after removal of anti-VEGF therapy that may explain the non-significant benefit in OS [21]. Similar hypothesis was proposed by Cacheux et al. who identified that the discontinuation of an antiangiogenic agent may induce a reversible tumor growth acceleration in colorectal patients [22].
In our study, mBTC patients from Group B presented a shorter PFS than those reported in other studies [23, 20]. In the BINGO trial, median PFS was 5.5 months. This extended PFS could be due to the inclusion in the BINGO trial of patients with locally-advanced carcinoma with a better ECOG performance status at baseline and smaller tumor burden [23]. In line with our data, André et al. study reported a 3.4 months median PFS in patients with gemcitabine combined with oxaliplatin (GEMOX) in advanced biliary tract adenocarcinoma [24]. Other targeted therapies have been evaluated in mBTC. Notably, Malka et al. reported in a phase II study the feasibility of GEMOX plus cetuximab, a chimeric anti-Epidermal Growth Factor Receptor antibody, without a survival advantage [23].
In our study, bevacizumab is associated with an increased and manageable toxicity, with 34.4% grade 3–4 adverse events. The incidence rate of side effects identified in our study was in line with those identified in hepatocellular carcinoma patients receiving GEMOX plus bevacizumab. Dose adaptation following a toxic effect occurring in patients helps to continue therapy for a long period. Side effects induced by GEMOX or bevacizumab are known and their management as well. In Zhu et al. study, patients treated with the combination of GEMOX plus bevacizumab seemed to benefit from bevacizumab, with an acceptable toxicity profile [15]. Valle et al. study was in line with our study confirming that the association of gemcitabine plus cisplatin was associated with a significant survival advantage without the addition of substantial toxicity compared to gemcitabine alone [6]. From a more general point of view, the present study confirmed that a GEMOX plus bevacizumab regimen is feasible and associated with some toxicities that should be stressed. Our unit previously reported our experience on the feasibility of oxaliplatin plus gemcitabine in frail patients such as hepatocellular carcinoma patients with an acceptable toxicity profile [17]. In the present cohort, only one case of grade 3 neuropathy was observed in each group.
Our study presented some limitations considering that it is a retrospective analysis based on patients who received bevacizumab plus GEMOX or GEMOX at two different time periods. In addition, the size of the samples is not sufficient to identify a significant overall benefit. Our study paves the way for larger studies to validate the usefulness of the addition of an antiangiogenic agent to the chemotherapy in first-line advanced biliary tract carcinoma.
In the Group A of our study, 33% of patients (2 out of 6) experienced a colo-vesical fistula. These patients had a gallbladder carcinoma and one of them presented peritoneal metastasis. Cases of cholecystocolic fistula caused by gallbladder carcinoma have been reported 2526. Bevacizumab is associated with an additional risk of fistula. Based on our study, we consider that the addition of an antiangiogenic agent should be avoided in gallbladder carcinoma. Furthermore, fistula aside, there was no discontinuation of bevacizumab due to toxicity in our study. In Group A, treatment was stopped due to tumor progression in only 3% of cases.
Conclusion
In conclusion, the GEMOX plus bevacizumab regimen showed an antitumor efficacy in terms of progression-free survival. The addition of bevacizumab was associated with a manageable toxicity. Our study stressed the usefulness to evaluate the addition of an antiangiogenic agent to the GEMOX regimen in first-line treatment of mBTC.
Abbreviations
b-FGF, b-Fibroblast Growth Factor; GEMCIS, Gemcitabine plus cisplatin regimen; GEMOX, Gemcitabine and oxaliplatin; mBTC, metastatic carcinoma of the biliary tract; NCI-CTCAE, National Cancer Institute Common Terminology Criteria for Adverse Events; OS, the Overall Survival; PFS, the progression-free survival; RECIST, Response Evaluation Criteria in Solid Tumors; VEGF, Vascular endothelial growth factor.
References
Bergquist A, von Seth E (2015) Epidemiology of cholangiocarcinoma. Best Pract Res Clin Gastroenterol 29:221–232
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66:7–30
Vauthey JN, Blumgart LH (1994) Recent advances in the management of cholangiocarcinomas. Semin Liver Dis 14:109–114
Hezel AF, Zhu AX (2008) Systemic therapy for biliary tract cancers. Oncologist 13:415–423
Eckel F, Schmid RM (2007) Chemotherapy in advanced biliary tract carcinoma: a pooled analysis of clinical trials. Br J Cancer 96:896–902
Valle J, Wasan H, Palmer DH et al (2010) ABC-02 trial investigators. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 362:1273–1281
Mir O, Coriat R, Dhooge M et al (2012) Feasibility of gemcitabine and oxaliplatin in patients with advanced biliary tract carcinoma and a performance status of 2. Anti-Cancer Drugs 23:739–744
Harder J, Riecken B, Kummer O et al (2006) Outpatient chemotherapy with gemcitabine and oxaliplatin in patients with biliary tract cancer. Br J Cancer 95:848–852
Riechelmann RP, Townsley CA, Chin SN et al (2007) Expanded phase II trial of gemcitabine and capecitabine for advanced biliary cancer. Cancer 110:1307–1312
Hida Y, Morita T, Fujita M et al (1999) Vascular endothelial growth factor expression is an independent negative predictor in extrahepatic biliary tract carcinomas. Anticancer Res 19:2257–2260
Ogasawara S, Yano H, Higaki K et al (2001) Expression of angiogenic factors, basic fibroblast growth factor and vascular endothelial growth factor, in human biliary tract carcinoma cell lines. Hepatol Res Off J Jpn Soc Hepatol 20:97–113
Hurwitz H, Fehrenbacher L, Novotny W et al (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Giantonio BJ, Catalano PJ, Meropol NJ et al (2007) Eastern cooperative oncology group study E3200. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the eastern cooperative oncology group study E3200. J Clin Oncol Off J Am Soc Clin Oncol 25:1539–1544
Jain RK (2001) Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med 7:987–989
Zhu AX, Meyerhardt JA, Blaszkowsky LS et al (2010) Efficacy and safety of gemcitabine, oxaliplatin, and bevacizumab in advanced biliary-tract cancers and correlation of changes in 18-fluorodeoxyglucose PET with clinical outcome: a phase 2 study. Lancet Oncol 11:48–54
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer Oxf Engl 1990 45:228–247
Dhooge M, Coriat R, Mir O et al (2013) Feasibility of gemcitabine plus oxaliplatin in advanced hepatocellular carcinoma patients with child-Pugh B cirrhosis. Oncology 84:32–38
Caussanel JP, Lévi F, Brienza S et al (1990) Phase I trial of 5-day continuous venous infusion of oxaliplatin at circadian rhythm-modulated rate compared with constant rate. J Natl Cancer Inst 82:1046–1050
Lee H, Wang K, Johnson A et al (2016) Comprehensive genomic profiling of extrahepatic cholangiocarcinoma reveals a long tail of therapeutic targets. J Clin Pathol 69:403–408
Lee J, Park SH, Chang H-M et al (2012) Gemcitabine and oxaliplatin with or without erlotinib in advanced biliary-tract cancer: a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 13:181–188
Mancuso MR, Davis R, Norberg SM et al (2006) Rapid vascular regrowth in tumors after reversal of VEGF inhibition. J Clin Invest 116:2610–2621
Cacheux W, Boisserie T, Staudacher L et al (2008) Reversible tumor growth acceleration following bevacizumab interruption in metastatic colorectal cancer patients scheduled for surgery. Ann Oncol Off J Eur Soc Med Oncol ESMO 19:1659–1661
Malka D, Cervera P, Foulon S et al (2014) BINGO investigators. Gemcitabine and oxaliplatin with or without cetuximab in advanced biliary-tract cancer (BINGO): a randomised, open-label, non-comparative phase 2 trial. Lancet Oncol 15:819–828
André T, Tournigand C, Rosmorduc O et al (2004) GERCOR group. Gemcitabine combined with oxaliplatin (GEMOX) in advanced biliary tract adenocarcinoma: a GERCOR study. Ann Oncol Off J Eur Soc Med Oncol ESMO 15:1339–1343
Authors’ information
All authors work at the Cochin University Hospital, Paris Descartes Medical School, Sorbonne Paris cite university in Paris. MB, OM and FG are oncologists working on drug optimization in the oncology unit. MD, JD, BB, MAG, CB, RC are gastrointestinal oncologists in charge of patients’ care in the digestive oncology unit.
Author information
Authors and Affiliations
Contributions
MB, MD and RC conceived the study, MB participated in the design of the study, MB, MD, JD, BB, MAG, CB, OM, FG, RC helped to draft the manuscript. RC coordinated to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethical Review Committee for publications of the Cochin University Hospital (CLEP) has examined the present research and gave an ethical approval (Decision number: AOOO-2016-026012).
Consent for publication
Not applicable.
Availability of data and materials
All clinical data is available at the Cochin University Hospital in Paris. Please contact the corresponding author for data requests.
Competing interests
Prof. Coriat has acted as paid consultant for Bayer Healthcare, Sanofi, Novartis, and Pfizer. Dr. Mir has acted as consultant for Amgen, Astra-Zeneca, Bayer, BMS, Lilly, Netcancer, Novartis, Pfizer and Roche. Prof. Goldwasser has acted as paid consultant for Freisenius Kabi. The other authors have no conflict of interests to declare.
Funding
None.
Rights and permissions
About this article
Cite this article
Bréchon, M., Dior, M., Dréanic, J. et al. Addition of an antiangiogenic therapy, bevacizumab, to gemcitabine plus oxaliplatin improves survival in advanced biliary tract cancers. Invest New Drugs 36, 156–162 (2018). https://doi.org/10.1007/s10637-017-0492-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-017-0492-6