Summary
The aim of the present study was to evaluate clinical activity, and the pharmacodynamic and pharmacokinetic profiles, of oral metronomic vinorelbine (VNR) plus dexamethasone (DEX) in metastatic castration-resistant prostate cancer (mCRPC) patients. Fourty-one patients (92 % chemotherapy-resistant) received 30 mg/day VNR p.o. thrice a week plus 1 mg/day DEX p.o. until disease progression. Plasma soluble B cell antigen 7 homolog 3 (sB7-H3), vascular endothelial growth factor (VEGF), and thrombospondin-1 (TSP-1), were measured by ELISA. Plasma VNR was detected using a LC-MS-MS system. The fraction of patients free of progression, defined by criteria of the Prostate Cancer Clinical Trials Working Group 2, at 3 months was 61 %. PSA decrease ≥50 % from baseline was observed in 35 % of patients. Median PFS and OS were 4 months (95 % CI, 2.8–6.9) and 17.5 months (95 % CI, 10.8–24.5), respectively. Toxicity was mild, and no grade 4 toxicities were found. The mean plasma VNR Cmax ranged from 1 to 2.7 ng/ml (Tmax 1.1 h) and no evidence of drug accumulation was found. A moderate relationship was found between plasma sB7-H3 and PSA values (r = 0.565; P = 0.0094) at the baseline. Increased PFS (11.3 vs. 2.8 months; P = 0.0298) was observed in patients with sB7-H3 levels <30.25 ng/mL. Plasma VEGF AUC0-24day increased in non-responders (P < 0.0001), whereas responders maintained higher plasma TSP-1 AUC0-24day (P = 0.0063). In conclusion, metronomic VNR plus DEX showed favourable activity, and a low toxicity profile, in mCRPC patients. Plasma sB7-H3, VEGF and TSP-1 levels are potential pharmacodynamic markers at the reached low plasma concentrations of vinorelbine metronomically administered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metronomic chemotherapy can be defined as the frequent, regular administration of drug doses that maintain a low, prolonged, and active, range of plasma concentrations of drugs with a more favourable toxicity profile [1]. Metronomic chemotherapy is an attractive option for palliative and maintenance treatment of metastatic castration-resistant prostate cancer (mCRPC). That is in part due to its excellent safety profile and the relative low rate of severe toxicities associated with its administration, especially for elderly and frail mCRPC patients [2–4]. In the last few years, mCRPC patients have been enrolled in clinical trials where metronomic oral cyclophosphamide was incorporated into the treatment regimens [4]. Thus, oral cyclophosphamide has been evaluated as a monotherapy [5], combined with corticosteroids [6–9], or given as part of complex combination regimens, which included celecoxib [10, 11], thalidomide [12], methotrexate [13], or docetaxel [2].
The semisynthetic vinka alkaloid vinorelbine (VNR), a cytotoxic microtubule-binding agent, is currently available as an oral formulation, which is suited for chronic and prolonged administration – and therefore for metronomic scheduling [14]. Indeed, metronomic oral vinorelbine at different doses (i.e. 30, 40 and 50 mg/day, three times per week) has produced interesting phase I-II clinical results, both as a monotherapy [15, 16] and given in combination with metronomic capecitabine [17, 18]. Oral VNR has also been combined with cyclophosphamide [19], and with bevacizumab [20], in metastatic breast and in non small cell lung cancer. A preliminary evaluation of the clinical use of metronomic VNR at 30 mg/day in metastatic prostate cancer patients was performed in small subsets of patients in phase I [16] and phase IB [15] studies (n = 6 and n = 8, respectively). Recent additional report includes a small (n = 14) retrospective evaluation of prostate cancer patients [21].
Metronomic VNR has been shown to have anti-endothelial activity in vitro [22, 23], and an antiangiogenic effect in vivo [24]. However, to date, no pharmacodynamic markers for antiangiogenic or immunological mechanisms of action have been studied in prostate cancer patients treated with a metronomic VNR regimen. Vascular endothelial growth factor (VEGF), a proangiogenic factor, and thrombospondin-1 (TSP-1), an endogenous inhibitor of angiogenesis, have been shown to be promising biomarkers of metronomic schedule activity [11, 25], whereas the B cell antigen 7 homolog 3 (B7-H3) have been associated to prostate cancer spread and outcome [26]. The aims of the present study were to evaluate in advanced CRPC patients the clinical activity, as well as the pharmacokinetic and pharmacodynamic profiles, of regimen of oral metronomic VNR plus dexamethasone (DEX).
Patients and methods
Study design and patient selection
This was a multicenter, prospective, non-randomized phase II clinical study (PROMET-3) which was approved by the independent local ethics committee (Sottocomitato Etico per la Sperimentazione Clinica, Azienda USL 6; approval number: scs 2009–0060) and was registered in the European Clinical Trial Database EudraCT (registration number 2009–015116-17). Patients provided their written informed consent to participate in this study, and in the related pharmacokinetic and pharmacodynamic assessments.
Eligibility criteria at baseline included age of ≥18 y, histological diagnosis of prostate adenocarcinoma, failure of prior docetaxel chemotherapy, the inability or unwillingness to receive docetaxel, disease progression according to the criteria of the “Prostate Cancer Clinical Trials Working Group 2” released in 2008 [27] (for trial entry, patients were considered to have disease progression if they had two consecutive increasing PSA level measurement above a reference value, or radiographic evidence of disease progression in either soft tissue or bone), and ongoing androgen deprivation therapy with a serum testosterone level of 50 ng per deciliter or less (≤2.0 nmol per liter). Other inclusion criteria included: PSA of ≥2 ng/mL; Eastern Cooperative Oncology Group (ECOG) performance status of ≤2; adequate bone marrow function (leukocytes, ≥3000/mL; neutrophil count, ≥1500/mL; haemoglobin level, ≥10 g/dL; platelets, ≥100,000/mL); adequate liver function (total serum bilirubin level, <1.5 mg/dL; aspartate aminotransferase and alanine aminotransferase, <3 upper normal limit); adequate renal function (serum creatinine level, <1.5 mg/dL), and life expectancy of ≥3 months. Antiandrogen therapy (flutamide and bicalutamide) was discontinued at least 6 wk. before enrollment, at which point evidence for PSA progression was required. The use of low-dose megestrol acetate for amelioration of symptoms was allowed. LHRH analogues (leuprolide), corticosteroids, and zoledronic acid were allowed if their administration started at least 4 weeks before the beginning of this study, and were associated with rising PSA levels.
Exclusion criteria at baseline included uncontrolled metabolic diseases, active infections, high risk of thromboembolic events without prophylactic treatments, untreated haemorrhagic gastric disease, or the presence of brain metastases.
Treatment
All eligible patients received 30 mg VNR p.o. three times a week plus 1 mg DEX p.o. daily. This treatment was continued without interruption except for the advent of unacceptable toxicity, disease progression, deterioration of performance status, or patient’s refusal to continue. No dose reduction for observed toxicities was applied.
Clinical evaluation
Pretreatment evaluations included a survey of the patient’s medical history, a physical examination that assessed weight, vital signs, and ECOG performance status. Patients also underwent electrocardiogram plus cardiovascular examinations, complete blood count and complete serum biochemistry (creatinine, glycemia, sodium, potassium, calcium, lactate dehydrogenase, aspartate aminotransferase, alanine aminotransferase, γGT, ALP, total bilirubin, PT, aPTT, fibrinogen, and D-dimer) analysis. PSA serum levels were measured, and pain evaluation was conducted according to the visual analogical scale (VAS). Measurable disease evaluation (if applicable) was performed. Every 2 weeks during the course of treatment, patients underwent a physical examination, and toxicity was assessed by the National Cancer Institute-Common Terminology Criteria for Adverse Events (NCI-CTCAE), followed by a blood count, and serum creatinine evaluation. Every 4 weeks the blood count and partial serum biochemistry (creatinine, total bilirubin, calcium, PT, aPTT, fibrinogen, and D-dimer) were repeated. Every 8 weeks an electrocardiogram was taken, alongside a physical and cardiovascular examination. At this time, a toxicity record, blood count, complete serum biochemistry, and measurable disease evaluation were performed. PSA serum levels were measured every 2 weeks throughout the course of this study.
Pharmacodynamic evaluation
Venous blood withdrawals were performed using Vacutainer blood collection tubes containing heparin/EDTA on day 1 (i.e. pretreatment), and on day 28 after initiation of therapy. On day 28, samples were taken prior to VNR administration. Plasma samples were analyzed by immunoenzymatic assays (ELISA) for total concentrations of soluble B cell antigen 7 homolog 3 (sB7-H3), thrombospondin 1 (TSP-1), and vascular endothelial growth factor-A (VEGF-A; R&D Systems, Minneapolis, MN). These ELISAs were carried out according to the manufacturer’s instructions. Optical density was determined using a Multiskan Spectrum microplate reader (Thermo Labsystems, Milan, Italy) set to 450 nm (with a wavelength correction of 540 nm). The results were expressed as nanograms of B7H3, and picograms of TSP-1 or VEGF, per milliliter of plasma.
Pharmacokinetic evaluation
Blood samples (4 ml each) for pharmacokinetic assays were taken from an indwelling i.v. cannula placed in an antecubital vein at baseline, and thereafter at 0.25, 0.5, 0.75, 1, 1.5, and 2 h after VNR oral dose for days 1, 28 and 112, of this study. Blood tubes were centrifuged (5 min; 400 g.; 4 °C) to separate the plasma, which was stored at −80 °C. Plasma concentrations of VNR were quantified using a LC-MS-MS system. Briefly, 500 μl of plasma samples were mixed with 1.1 ml of acetonitrile, with the addition of 50 μl of vinblastine (50 nM) as an internal standard. After agitation and centrifugation (18,620 x g. for 15 min), the supernatant was collected and evaporated under nitrogen flow until it was completely dry. The residue was reconstituted in 200 μl ACN/H2O 30/70 % v/v. An aliquot (20 μl) of the reconstituted extract was then directly injected into a LC-MS-MS system, using a Waters Acquity Ultraperformance Liquid Chromatography (UPLC) coupled with a Waters Xevo TQ-S mass spectrometer (Milford, USA). The flow rate through the column (a Waters Acquity UPLC BEH C18 1.7 μm 2.1 × 50 mm column protected by a Waters Vanguard BEH C18 1.7 μm guard cartridge) was 0.5 ml/min. The MS method was based on positive ion mode Multiple Reaction Monitoring (MRM), and the monitored transitions were 390.3 → 122.2 m/z (quantifier), 390.3 → 658.1, 390.3 → 357.1 m/z (qualifiers) for VNR, and 406.2 → 376.2 (quantifier), 406.2 → 271.6, 406.2 → 255.2 (qualifiers) for vinblastine. The MS parameters were optimized to achieve maximum sensitivity.
Individual plasma concentration profiles of VNR were fitted according to a one-compartment, extravascular with lag-time model by use of nonlinear least squares regression analysis (MwPharm software, version 3.60; MediWare, Groningen, The Netherlands). The area under the curve (AUC0→2h) of VNR was calculated by the trapezoidal method for the area from time 0 to 2 h after VNR administration. The maximum plasma concentration (Cmax) and time to reach Cmax (Tmax) were identified from the inspection of vinorelbine concentration–time plots.
Endpoints and response criteria
The primary endpoint of this study was to evaluate the percentage of patients that did not show progression within the first 3 months of metronomic oral VNR plus DEX therapy. Progression was defined on the basis of changes in PSA, bone metastases, and measurable disease as follows [27]: i) first PSA increase that is >25 % and >2 ng/mL above the nadir, and which is confirmed by a second value 3 or more weeks later, ii) appearance of 2 or more additional lesions for the first reassessment only, iii) use of Response Evaluation Criteria in Solid Tumors (RECIST) criteria in nodal and visceral sites. Secondary end points were the following: a) PSA-based outcome, defined by a decrease of ≥50 % from baseline, and then maintained for at least 12 wk. (in accordance with the consensus guidelines of the Prostate Cancer Clinical Trials Working Group 2), b) objective response rate according to RECIST criteria [28], c) toxicity (NCI-CTCAE), d) duration of PSA response, e) time to PSA progression, f) pain control (VAS), g) overall survival, h) pharmacokinetic parameters of metronomic VNR, and i) ability to modulate plasma sB7-H3, and TSP-1 and VEGF levels.
Statistical analyses
According to single stage design Fleming, as amended by A’Hern [29], with P0 = 35 %, P1 = 55 %, α = 0.05, and β = 0.20, the enrollment of 41 patients was required. The null hypothesis was defined on the basis of a previous study on metronomic chemotherapy conducted by our group [11]. We estimated that if at least 20 patients were free of progression at 3 months of treatment, then that would be indicative of therapeutic efficacy worthy of further investigation.
Response duration was calculated from the time of first objective response to time of progression. Progression free survival (PFS) and overall survival (OS) were calculated from the date of first chemotherapy administration to the date of progression or death/loss to follow-up, respectively. PFS and OS were analyzed by GraphPad Prism software (package version 5.0; Graph- Pad Software Inc., San Diego, CA), using the product limit method of Kaplan and Meier and comparing survival curves using both the log-rank test and the Gehan-Wilcoxon test. The log-rank test was also used to test differences in PFS between subgroups of patients.
Statistical analysis by ANOVA, followed by the Student–Newman–Keuls test, was used to assess any differences in the pharmacokinetic and/or pharmacodynamic data. Correlations between pharmacodynamic and PSA level parameters were investigated by a linear regression analysis. Cut-off values for the pharmacodynamic parameter represented by sB7-H3 levels were found with a nonparametric receiver operating characteristic (ROC) analysis, performed to assess the accuracy of sB7-H3 levels to discriminate between patient responders and non-responders. Statistical analyses were performed using the GraphPad Prism.
Results
Characteristics of enrolled patients and of administered treatment
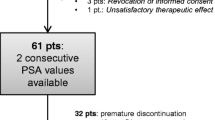
From December 2009 to January 2011, 41 patients from two Italian institutions were enrolled in this study. All patients were clinically assessable. Baseline patient characteristics are listed in Table 1.
Prior hormonal therapy was administered in 39 patients (95 %) and it was represented by antiandrogens (i.e. flutamide, bicalumide) and LHRH agonists (i.e. leuprolide). In two patients this information was not available. Previous docetaxel regimens (i.e. 75 mg/m2 every 3 weeks) had been administered to 35 patients (85 %). Six patients (15 %) were considered unable to receive docetaxel, or they refused docetaxel treatment. Three patients received metronomic oral VNR and DEX as a first line treatment, and the other patients received VNR plus DEX following metronomic oral cyclophosphamide therapy. The mean number of previous regimens was 2.5 (range 0–5) and twenty patients (49 %) received two or more lines of chemotherapy. Previous regimens were as follows: mitoxantrone - 8 patients (20 %), metronomic oral cyclophosphamide - 4 patients (10 %), estramustine - 3 patients (7 %), epirubicin - 2 patients (5 %), sorafenib - 2 patients (5 %), etoposide - 1 patient (2.5 %), carboplatin - 1 patient (2.5 %), sunitinib and gefitinib - 1 patient (2.5 %).
Zoledronic acid was administered to 28 patients (68 %) who had evidence of bone metastases. The median duration of metronomic chemotherapy was 170 days (range, 28–545 days).
Toxicity
All patients were evaluated for treatment associated toxicity (Table 2). Metronomic VNR was generally well tolerated and no NCI-CTCAE grade 4 toxicities were reported in the 41 patients. No major cardiovascular events or toxicity-related deaths were observed. NCI-CTCAE grade 3 toxicities were nonhematologic: these included asthenia (6 patient; 15 %), and anorexia (5 patients; 13 %).
Clinical activity
All patients were evaluated for clinical activity. The fraction of patients free of progression at 3 months was 61 % (n = 25). According to the recommendations of the Prostate Cancer Clinical Trials Working Group 2 [27], a confirmed PSA decrease of ≥50 % from baseline was observed in 14/41 (35 %) patients. In Fig. 1a, a waterfall plot shows the percentage change in PSA levels from baseline to 12 weeks into the study, as well as the maximal PSA decrease. Fourteen patients (35 %) showed a PSA decrease ≥50 %, and 25 (61 %) showed a measurable PSA decrease.
A waterfall plot showing the maximal change from baseline (at 12 wk. or at any time point) of PSA levels after VNR plus DEX therapy a. Actuarial progression-free survival (PFS), and overall survival (OS), curves calculated by the Kaplan-Meier method from the first day of metronomic VNR plus DEX administration b
According to RECIST criteria, nine patients were evaluable: we observed 6 patients with stable disease, 2 with a partial response, and 1 with progression of disease.
Figure 1b shows a median PFS of 4 months (95 % CI, 2.8–6.9 months) and a median OS of 17.5 months (95 % CI, 10.8–24.5 months). Notably, 8/41 patients (20 %) continued to receive metronomic VNR plus DEX treatment beyond PSA or disease progression, due to improvements in their symptoms and in their quality of life, and following discussions with their clinical practitioner. Moreover, 28 patients (68 %) received at least 1 additional anticancer therapy after the end of this study. Of these, eleven patients (27 %) received abiraterone, nine patients (22 %) received mitoxantrone, five patients (12 %) received a re-chellenge with docetaxel, and two patients (5 %) received cabazitaxel, as subsequent treatments.
Pharmacokinetics
Table 3 reports the main pharmacokinetic parameters of the oral 30 mg VNR dose. This dose was rapidly absorbed as indicated by the Tmax that was achieved at 1.1 h (range, 0.25 to 2 h) after VNR oral administration at days 1, 28 and 112. The measured mean plasma Cmax of VNR was not significantly different among the different timepoints analyzed (Table 3). Moreover, the VNR AUC0→2h values at days 1, 28, and 112, were constant during the course of treatment (Table 3). Thus, no evidence was found for accumulation of VNR during the first 16 weeks of treatment.
Pharmacodynamic evaluations
Pharmacodynamic analyses were performed in 20 patients. Plasma samples were collected prior to the first VNR administration (i.e. baseline), and after 28 days of metronomic VNR plus DEX treatment.
A significant, albeit moderate, relationship was found between sB7-H3 plasma levels and serum PSA values (r = 0.565; P = 0.0094; Fig. 2a) at baseline. Thus, in parallel with an increase of PSA levels, a moderately significant increase of plasma sB7-H3 levels was noted. Furthermore, we found a significant increased in PFS (11.3 vs. 2.8 months; P = 0.0298; Fig. 2b) in patients with plasma levels of sB7-H3 below a cutoff value of 30.25 ng/mL, as obtained by ROC analysis.
To interpret the pharmacodynamic parameters in relation to biochemical responses, we defined patients as responders if they showed a decrease in PSA levels of ≥50 % and a PSA stabilization of ≥3 months. Figure 3a shows that plasma levels of TSP-1 (measured by the TSP-1 AUC0–28 day) were significantly higher in responders (n = 15) vs. non-responders (n = 5; Fig. 3a). In contrast, in that same period, plasma VEGF levels (measured by the VEGF AUC0–28 day) significantly increased in non-responders compared to responders (Fig. 3b) in the period day 1 – day 28.
Discussion
This study describes the clinical, pharmacokinetic, and pharmacodynamic, evaluation of oral metronomic VNR given with DEX for the treatment of metastatic CPRC previously treated with docetaxel and other chemotherapeutic drugs.
Our primary objective was to assess the clinical efficacy of a metronomic oral VNR plus DEX regimen. We observed that 61 % of patients (n = 25) were free of progression 3 months into this metronomic study, far beyond our expected target (i.e., of having at least 20 out of 41 treated patients showing such a response), with a confirmed PSA ≥50 % decrease in 35 % of patients, and a median PFS of 4 months. Median OS was 17.5 months. All the enrolled patients were old adults, with nearly half (44 %) of them of age 75 years or older.
When we began this study, there was no standard of care for the second-line setting for CPRC after progression on docetaxel [30]. At that time (i.e. the end of 2009), data from studies on metronomic cyclophosphamide in CRPC were available [6, 11] suggesting a promising role for metronomic chemotherapy in this setting. Therefore we decided that metronomic VNR should be investigated as a palliative treatment after docetaxel treatment. It is important to note that after our study began, numerous phase II-III clinical trials reported on the activity of several second line chemotherapies in mCRPC patients [30]. In some cases, interesting antitumor activity was noted, frequently coupled with a severe toxicity profile (usually high-grade hematological toxicities). Second-generation anti-hormonal agents (abiraterone and enzalutamide) have since been approved for the treatment of mCRPC, on the basis of their ability to improve overall survival and their good safety profiles in men with mCRPC after treatment with docetaxel [31, 32]. Nonetheless, whilst enzalutamide and abiraterone represent breakthroughs in the treatment of mCRPC, there is a substantial proportion of patients (20–40 %) that show no response to these drugs or, after an initial response, who subsequently develop drug resistance [33], typically as a consequence of the acquisition of AR splice variants (i.e. AR-V2, AR-V7). On the other hand, cabazitaxel plus prednisone in the TROPIC phase III clinical trial showed significant prolonged OS compared to mitoxantrone plus prednisone, and has consequently been adopted as one of the standard treatments after docetaxel. The median OS in the cabazitaxel arm was 15.1 months, compared to 12.7 months in the mitoxantrone arm (p < 0.0001), whereas the median time to PSA progression was 6.4 vs. 3.1 months, respectively (P = 0.001). The percentage of patients showing PSA response in the cabazitaxel arm was 39.2 % [34]. However, hematological adverse drug reactions were noted in the majority of enrolled patients, including grade 3 or greater neutropenia (82 % of cases with cabazitaxel) and leucopenia (68 %) [34]. Though cabazitaxel has also demonstrated activity against AR-V7-positive circulating tumor cells [35], new chemotherapeutic strategies are warranted to improve both activity and tolerability profiles, and also to overcome drug resistance [34, 36, 37]. In that regard, our results with metronomic VNR plus DEX given to patients after docetaxel (or following their refusal to take docetaxel) show a good profile of haematological toxicity if compared with other chemotherapeutic regimens, suggesting a possible future role of metronomic VNR 30 mg/day in the palliative treatment of mCRPC patients, especially in older (>75 years) patients.
In a previous phase II trial of metronomic cyclophosphamide (50 mg p.o. daily) with celecoxib and DEX conducted in 28 patients with advanced CRPC, Fontana and colleagues [11] observed a PSA response rate of 32 % and a PSA stabilization of 18 %. Moreover, the median progression-free survival of 4 months (95 % CI, 2.8–6.9 months), observed in the present study, was similar to that observed in a retrospective study by Dickinson et al. [7] with a combined schedule of cyclophosphamide and DEX. These results compare favorably with those noted in other metronomic chemotherapy trials (range 2.8–3 months) involving metronomic cyclophosphamide in combination with celecoxib or methrotrexate [11, 13]. Furthermore, Nelius and colleagues noted in a small study (17 patients) of metronomic cyclophosphamide (50 mg po daily) plus DEX (1 mg po daily) given to patients with taxane-resistant CRPC, that the PSA response was 24 % [9].
The favorable clinical activity, and the related toxicity profile, that we observed with the metronomic 30 mg dose of VNR produced maximum VNR plasma concentrations varying from 1 to 2.7 ng/ml, which were maintained for at least 112 days without any evidence of drug accumulation. Moreover, no significant differences of AUCs were recorded at different timepoints in this study. Previous work by Briasoulis and colleagues [15, 16] described the plasma concentrations of VNR (in the metronomic setting), displaying linear pharmacokinetics with a constant concentration:dose ratio and a proportional increase in concentrations with escalating administered doses [16]. Interestingly, the steady-state concentration of the 30 mg VNR dose was 1.8 ± 1.10 ng/ml [15], a value similar to the ones obtained in this study. This indicates that VNR is clinically active against mCRPC in this range of plasma concentrations.
The prolonged in vitro exposure of VNR, and of its active metabolite, 4-O-deacetylvinorelbine, at pico- and nano-molar concentrations, has been shown to be an effective inhibitor of endothelial cell proliferation, and of endothelial-cell migration [22, 23]. In addition, such doses also inhibit tube formation and in vitro sprouting [22, 23]. Moreover, previous studies showed that the optimal biologic dose of metronomic oral VNR in mice decreases the mobilization and viability of bone marrow–derived circulating endothelial progenitors (CEPs) [24], increases the levels of apoptotic circulating endothelial cells [38], and inhibits the growth of breast cancer in tumor bearing mice [24] [38]. Our pharmacodynamic data in patients is consistent with an antiangiogenic activity of the 30 mg VNR metronomic schedule. Thus we observed an increase in the AUC of plasma TSP-1 - an endogenous antiangiogenic molecule and a mediator of the antiangiogenic effects of metronomic chemotherapy [39] - and a decrease in the AUC of plasma VEGF, a strong pro-angiogenic factor [40], in patients that responded to the metronomic VNR plus DEX regimen used in this study. Similar findings were previously described by our group in colorectal cancer patients treated with metronomic cyclophosphamide plus UFT [25], and also by Camerini and colleagues [41] in NSCL elderly patients treated with metronomic oral VNR.
The pharmacodynamics of metronomic chemotherapy is consistent with the concept that the therapy of cancer is a complex approach involving both tumor cells and their microenvironment, including microvessels and cells of immune system [42]. While anti-angiogenesis is an important mechanism of action of metronomic chemotherapy, other mechanisms, including activation of anti-tumor immunity – mainly through the suppression of regulatory T-cells - have also been identified [43]. Our data in mCRPC patients suggests that metronomic VNR may also promote antitumor immunity. B7-H3 (CD276), a member of the B7 family of molecules, is often induced in human tumors and numerous evidences implicating B7-H3 in tumor immune escape [44]. Indeed, these ligands may act as antigen-specific inhibitors of T-cell-mediated antitumoral immunity [45]. B7-H3 was shown to be highly expressed in prostate cancer and associated with disease spread and poor outcome [26, 46]. High tumor B7-H3 staining in primary prostate cancer has been associated also with increased risk of recurrence measured by PSA after salvage radiation therapy [47] and with clinical relapse [48]. The soluble form of B7-H3 (sB7-H3) was reported to be released from the cell membrane by matrix metalloproteinases cleavage of monocytes, dendritic cells, activated T cells and of tumor cells [49]. Interestingly, our results describe a moderate but significant correlation between sB7-H3 plasma levels and serum PSA concentrations, suggesting that, at least in our study, sB7-H3 plasma levels may be associated with the PSA status. Indeed, although the PSA as a screening marker for prostate cancer is of considerable controversy, its increased expression is an effective indicator for the recurrence of this tumor [50]. Moreover, a significant increased PFS was observed in patients with plasma levels of sB7-H3 < 30.25 ng/mL at day 28 of the metronomic VNR schedule. A similar cut-off of circulating B7-H3 levels (30 ng/ml) was found by Zhang and colleagues [51] and it served to distinguish patients with NSCLC from those with other pulmonary diseases (or healthy volunteers). Thus, lower plasma concentrations of sB7-H3 after 1 month from the beginning of metronomic VNR may be considered as a promising biomarker of effective therapeutic impact, whereas elevated sB7-H3 levels may reflect tumour progression. Furthermore, also the pro-angiogenic factor VEGF has been described as a potent negative regulator of T cell infiltration of tumors, and thus, an inhibitor of the immune control of tumors [52]. Interestingly, TSP-1 has been shown to reverse this immunosoppressive effects of VEGF, inhibiting the VEGF activity on proliferation and T cell activation through the ligation of CD47 [53].
The present prospective phase II clinical trial is a pilot study, and both clinical and pharmacokinetic/pharmacodynamic data are exploratory by nature. The results and the statistical significances we present should be interpreted with caution as they have as yet to be translated to a larger patient population. It must be also acknowledge that low dose DEX alone has shown activity in prostate cancer [54], and could have accounted for some of the cancer control in our study. Indeed, in a recent small phase II study, DEX alone in chemotherapy-naïve mCRPC patients determined a > 50 % PSA decline in 54 % of patients [50]. Nonetheless, the results we present may be useful for the generation of hypotheses on the use of oral VNR metronomic regimens that can be tested in subsequent investigations in docetaxel-resistant patients. Thus, consideration should be given to testing the combination of metronomic VNR plus DEX in a larger patient population (i.e., in a randomized phase II trial of patients that previously received treatment with the second-generation anti-hormonal agents, abiraterone and enzalutamide) in order to better assess its clinical impact. In conclusion, metronomic VNR plus DEX showed a favourable toxicity profile and an interesting activity in elderly adults with mCRPC. Plasma sB7-H3, VEGF and TSP-1 levels, at the reached VNR plasma concentrations of 1–2.7 ng/ml, may represent interesting pharmacodynamic markers for the clinical response of mCRPC patients treated with this schedule.
References
Bocci G, Kerbel R (2016) Pharmacokinetics of metronomic chemotherapy: a neglected but crucial aspect. Nat Rev Clin Oncol. doi:10.1038/nrclinonc.2016.1064
Derosa L, Galli L, Orlandi P, Fioravanti A, Di Desidero T, Fontana A, Antonuzzo A, Biasco E, Farnesi A, Marconcini R, Francia G, Danesi R, Falcone A, Bocci G (2014) Docetaxel plus oral metronomic cyclophosphamide: a phase II study with pharmacodynamic and pharmacogenetic analyses in castration-resistant prostate cancer patients. Cancer 120(24):3923–3931. doi:10.1002/cncr.28953
Fontana A, Falcone A, Derosa L, Di Desidero T, Danesi R, Bocci G (2010) Metronomic chemotherapy for metastatic prostate cancer: a ‘young’ concept for old patients? Drugs Aging 27(9):689–696. doi:10.2165/11537480-000000000-00000
Delos Santos K, Sivanathan L, Lien K, Emmenegger U (2014) Clinical Trials of Low-Dose Metronomic Chemotherapy in Castration-Resistant Prostate Cancer In: Bocci G, Francia G (eds) Metronomic Chemotherapy: Pharmacology and Clinical Applications. Springer-Verlag, Berlin Heidelberg, pp. 119–133
Lord R, Nair S, Schache A, Spicer J, Somaihah N, Khoo V, Pandha H (2007) Low dose metronomic oral cyclophosphamide for hormone resistant prostate cancer: a phase II study. J Urol 177 (6):2136–2140; discussion 2140. doi:10.1016/j.juro.2007.01.143
Glode LM, Barqawi A, Crighton F, Crawford ED, Kerbel R (2003) Metronomic therapy with cyclophosphamide and dexamethasone for prostate carcinoma. Cancer 98(8):1643–1648. doi:10.1002/cncr.11713
Dickinson PD, Peel DN, Sundar S (2012) Metronomic chemotherapy with cyclophosphamide and dexamethasone in patients with metastatic carcinoma of the prostate. Br J Cancer 106 (8):1464–1465; author reply 1466. doi:10.1038/bjc.2012.78
Ladoire S, Eymard JC, Zanetta S, Mignot G, Martin E, Kermarrec I, Mourey E, Michel F, Cormier L, Ghiringhelli F (2010) Metronomic oral cyclophosphamide prednisolone chemotherapy is an effective treatment for metastatic hormone-refractory prostate cancer after docetaxel failure. Anticancer Res 30(10):4317–4323
Nelius T, Klatte T, de Riese W, Haynes A, Filleur S (2010) Clinical outcome of patients with docetaxel-resistant hormone-refractory prostate cancer treated with second-line cyclophosphamide-based metronomic chemotherapy. Med Oncol 27(2):363–367. doi:10.1007/s12032-009-9218-8
Fontana A, Bocci G, Galli L, D’Arcangelo M, Derosa L, Fioravanti A, Orlandi P, Barletta MT, Landi L, Bursi S, Minuti G, Bona E, Grazzini I, Danesi R, Falcone A (2010) Metronomic cyclophosphamide in elderly patients with advanced, castration-resistant prostate cancer. J Am Geriatr Soc 58(5):986–988. doi:10.1111/j.1532-5415.2010.02833.x
Fontana A, Galli L, Fioravanti A, Orlandi P, Galli C, Landi L, Bursi S, Allegrini G, Fontana E, Di Marsico R, Antonuzzo A, D’Arcangelo M, Danesi R, Del Tacca M, Falcone A, Bocci G (2009) Clinical and pharmacodynamic evaluation of metronomic cyclophosphamide, celecoxib, and dexamethasone in advanced hormone-refractory prostate cancer. Clin Cancer Res 15(15):4954–4962. doi:10.1158/1078-0432.ccr-08-3317
Meng LJ, Wang J, Fan WF, XL P, Liu FY, Yang M (2012) Evaluation of oral chemotherapy with capecitabine and cyclophosphamide plus thalidomide and prednisone in prostate cancer patients. J Cancer Res Clin Oncol 138(2):333–339. doi:10.1007/s00432
Gebbia V, Serretta V, Borsellino N, Valerio MR (2011) Salvage therapy with oral metronomic cyclophosphamide and methotrexate for castration-refractory metastatic adenocarcinoma of the prostate resistant to docetaxel. Urology 78(5):1125–1130. doi:10.1016/j.urology.2011.08.010
Cazzaniga ME, Camerini A, Addeo R, Nole F, Munzone E, Collova E, Del Conte A, Mencoboni M, Papaldo P, Pasini F, Saracchini S, Bocci G (2016) Metronomic oral vinorelbine in advanced breast cancer and non-small-cell lung cancer: current status and future development. Future Oncol 12(3):373–387. doi:10.2217/fon.15.306
Briasoulis E, Aravantinos G, Kouvatseas G, Pappas P, Biziota E, Sainis I, Makatsoris T, Varthalitis I, Xanthakis I, Vassias A, Klouvas G, Boukovinas I, Fountzilas G, Syrigos KN, Kalofonos H, Samantas E (2013) Dose selection trial of metronomic oral vinorelbine monotherapy in patients with metastatic cancer: a hellenic cooperative oncology group clinical translational study. BMC Cancer 13:263. doi:10.1186/1471-2407-13-263
Briasoulis E, Pappas P, Puozzo C, Tolis C, Fountzilas G, Dafni U, Marselos M, Pavlidis N (2009) Dose-ranging study of metronomic oral vinorelbine in patients with advanced refractory cancer. Clin Cancer Res 15(20):6454–6461. doi:10.1158/1078-0432.ccr-09-0970
Cazzaniga ME, Torri V, Villa F, Giuntini N, Riva F, Zeppellini A, Cortinovis D, Bidoli P (2014) Efficacy and Safety of the All-Oral Schedule of Metronomic Vinorelbine and Capecitabine in Locally Advanced or Metastatic Breast Cancer Patients: The Phase I-II VICTOR-1 Study. Int J Breast Cancer 2014:769790. doi:10.1155/2014/769790
Saridaki Z, Malamos N, Kourakos P, Polyzos A, Ardavanis A, Androulakis N, Kalbakis K, Vamvakas L, Georgoulias V, Mavroudis D (2012) A phase I trial of oral metronomic vinorelbine plus capecitabine in patients with metastatic breast cancer. Cancer Chemother Pharmacol 69(1):35–42. doi:10.1007/s00280
Launay S, Sabatier R, Brunelle S, Esterni B, Tarpin C, Viret F, Gravis G, Cappiello M, Provansal M, Extra JM, Bertucci F, Viens P, Goncalves A (2016) METRO1: a phase I study of metronomic chemotherapy in adults with advanced refractory solid tumors. Anticancer Res 36(1):293–299
Saloustros E, Kalbakis K, Vardakis N, Kalykaki A, Milaki G, Rovithi M, Agelaki S, Saridaki Z, Georgoulias V, Mavroudis D (2011) Metronomic vinorelbine plus bevacizumab as salvage therapy for patients with metastatic breast cancer. J BUON 16(2):215–218
Tralongo P, Bordonaro S, Di Mari A, Cappuccio F, Rametta Giuliano S (2016) Chemotherapy in frail elderly patients with hormone-refractory prostate cancer: a "real world" experience. Prostate Int 4(1):15–19. doi:10.1016/j.prnil.2015.12.003
Biziota E, Briasoulis E, Mavroeidis L, Marselos M, Harris AL, Pappas P (2016) Cellular and molecular effects of metronomic vinorelbine and 4-O-deacetylvinorelbine on human umbilical vein endothelial cells. Anti-Cancer Drugs 27(3):216–224. doi:10.1097/cad.0000000000000319
Mavroeidis L, Sheldon H, Briasoulis E, Marselos M, Pappas P, Harris AL (2015) Metronomic vinorelbine: anti-angiogenic activity in vitro in normoxic and severe hypoxic conditions, and severe hypoxia-induced resistance to its anti-proliferative effect with reversal by Akt inhibition. Int J Oncol 47(2):455–464. doi:10.3892/ijo.2015.3059
Shaked Y, Emmenegger U, Man S, Cervi D, Bertolini F, Ben-David Y, Kerbel RS (2005) Optimal biologic dose of metronomic chemotherapy regimens is associated with maximum antiangiogenic activity. Blood 106(9):3058–3061. doi:10.1182/blood-2005-04-1422
Allegrini G, Di Desidero T, Barletta MT, Fioravanti A, Orlandi P, Canu B, Chericoni S, Loupakis F, Di Paolo A, Masi G, Fontana A, Lucchesi S, Arrighi G, Giusiani M, Ciarlo A, Brandi G, Danesi R, Kerbel RS, Falcone A, Bocci G (2012) Clinical, pharmacokinetic and pharmacodynamic evaluations of metronomic UFT and cyclophosphamide plus celecoxib in patients with advanced refractory gastrointestinal cancers. Angiogenesis 15(2):275–286. doi:10.1007/s10456-012-9260-6
Zang X, Thompson RH, Al-Ahmadie HA, Serio AM, Reuter VE, Eastham JA, Scardino PT, Sharma P, Allison JP (2007) B7-H3 and B7x are highly expressed in human prostate cancer and associated with disease spread and poor outcome. Proc Natl Acad Sci U S A 104(49):19458–19463. doi:10.1073/pnas.0709802104
Scher HI, Halabi S, Tannock I, Morris M, Sternberg CN, Carducci MA, Eisenberger MA, Higano C, Bubley GJ, Dreicer R, Petrylak D, Kantoff P, Basch E, Kelly WK, Figg WD, Small EJ, Beer TM, Wilding G, Martin A, Hussain M (2008) Design and end points of clinical trials for patients with progressive prostate cancer and castrate levels of testosterone: recommendations of the prostate cancer clinical trials working group. J Clin Oncol 26(7):1148–1159. doi:10.1200/jco.2007.12.4487
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1. Eur J Cancer 45(2):228–247. doi:10.1016/j.ejca.2008.10.026
A’Hern RP (2001) Sample size tables for exact single-stage phase II designs. Stat Med 20(6):859–866. doi:10.1002/sim.721
Altavilla A, Iacovelli R, Procopio G, Cortesi E (2012) Post-docetaxel therapy in castration resistant prostate cancer - the forest is growing in the desert. Ther Adv Urol 4(3):107–111. doi:10.1177/1756287212440302
Fizazi K, Scher HI, Molina A, Logothetis CJ, Chi KN, Jones RJ, Staffurth JN, North S, Vogelzang NJ, Saad F, Mainwaring P, Harland S, Goodman OB Jr, Sternberg CN, Li JH, Kheoh T, Haqq CM, de Bono JS (2012) Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 13(10):983–992. doi:10.1016/s1470-2045(12)70379-0
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, de Wit R, Mulders P, Chi KN, Shore ND, Armstrong AJ, Flaig TW, Flechon A, Mainwaring P, Fleming M, Hainsworth JD, Hirmand M, Selby B, Seely L, de Bono JS (2012) Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 367(13):1187–1197. doi:10.1056/NEJMoa1207506
Antonarakis ES, Armstrong AJ, Dehm SM, Luo J (2016) Androgen receptor variant-driven prostate cancer: clinical implications and therapeutic targeting. Prostate Cancer Prostatic Dis. doi:10.1038/pcan.2016.17
de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, Gravis G, Bodrogi I, Mackenzie MJ, Shen L, Roessner M, Gupta S, Sartor AO (2010) Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet 376 (9747):1147–1154. doi:10.1016/s0140-6736(10)61389-x
Onstenk W, Sieuwerts AM, Kraan J, Van M, Nieuweboer AJ, Mathijssen RH, Hamberg P, Meulenbeld HJ, De Laere B, Dirix LY, van Soest RJ, Lolkema MP, Martens JW, van Weerden WM, Jenster GW, Foekens JA, de Wit R, Sleijfer S (2015) Efficacy of cabazitaxel in castration-resistant prostate cancer is independent of the presence of AR-V7 in circulating tumor cells. Eur Urol 68(6):939–945. doi:10.1016/j.eururo.2015.07.007
Lorente D, Mateo J, Perez-Lopez R, de Bono JS, Attard G (2015) Sequencing of agents in castration-resistant prostate cancer. Lancet Oncol 16(6):e279–e292. doi:10.1016/s1470-2045(15)70033-1
Attard G, Parker C, Eeles RA, Schroder F, Tomlins SA, Tannock I, Drake CG, de Bono JS (2016) Prostate cancer. Lancet 387 (10013):70–82. doi:10.1016/s0140-6736(14)61947-4
Mancuso P, Colleoni M, Calleri A, Orlando L, Maisonneuve P, Pruneri G, Agliano A, Goldhirsch A, Shaked Y, Kerbel RS, Bertolini F (2006) Circulating endothelial-cell kinetics and viability predict survival in breast cancer patients receiving metronomic chemotherapy. Blood 108(2):452–459. doi:10.1182/blood-2005-11-4570
Bocci G, Francia G, Man S, Lawler J, Kerbel RS (2003) Thrombospondin 1, a mediator of the antiangiogenic effects of low-dose metronomic chemotherapy. Proc Natl Acad Sci U S A 100(22):12917–12922. doi:10.1073/pnas.2135406100
Evans I (2015) An overview of VEGF-mediated signal transduction. Methods Mol Biol 1332:91–120. doi:10.1007/978-1-4939-2917-7_7
Camerini A, Puccetti C, Donati S, Valsuani C, Petrella MC, Tartarelli G, Puccinelli P, Amoroso D (2015) Metronomic oral vinorelbine as first-line treatment in elderly patients with advanced non-small cell lung cancer: results of a phase II trial (MOVE trial). BMC Cancer 15:359. doi:10.1186/s12885
Shaked Y (2016) Balancing efficacy of and host immune responses to cancer therapy: the yin and yang effects. Nat Rev Clin Oncol. doi:10.1038/nrclinonc.2016.57
Kareva I, Waxman DJ, Lakka Klement G (2015) Metronomic chemotherapy: an attractive alternative to maximum tolerated dose therapy that can activate anti-tumor immunity and minimize therapeutic resistance. Cancer Lett 358(2):100–106. doi:10.1016/j.canlet.2014.12.039
Wang L, Kang FB, Shan BE (2014) B7-H3-mediated tumor immunology: friend or foe? Int J Cancer 134(12):2764–2771. doi:10.1002/ijc.28474
Loos M, Hedderich DM, Friess H, Kleeff J (2010) B7-h3 and its role in antitumor immunity. Clin Dev Immunol 2010:683875. doi:10.1155/2010/683875
Roth TJ, Sheinin Y, Lohse CM, Kuntz SM, Frigola X, Inman BA, Krambeck AE, McKenney ME, Karnes RJ, Blute ML, Cheville JC, Sebo TJ, Kwon ED (2007) B7-H3 ligand expression by prostate cancer: a novel marker of prognosis and potential target for therapy. Cancer Res 67(16):7893–7900. doi:10.1158/0008-5472.can-07-1068
Parker AS, Heckman MG, Sheinin Y, KJ W, Hilton TW, Diehl NN, Pisansky TM, Schild SE, Kwon ED, Buskirk SJ (2011) Evaluation of B7-H3 expression as a biomarker of biochemical recurrence after salvage radiation therapy for recurrent prostate cancer. Int J Radiat Oncol Biol Phys 79(5):1343–1349. doi:10.1016/j.ijrobp.2010.01.061
Liu Y, Vlatkovic L, Saeter T, Servoll E, Waaler G, Nesland JM, Giercksky KE, Axcrona K (2012) Is the clinical malignant phenotype of prostate cancer a result of a highly proliferative immune-evasive B7-H3-expressing cell population? Int J Urol 19(8):749–756. doi:10.1111/j.1442-2042.2012.03017.x
Zhang G, Hou J, Shi J, Yu G, Lu B, Zhang X (2008) Soluble CD276 (B7-H3) is released from monocytes, dendritic cells and activated T cells and is detectable in normal human serum. Immunology 123(4):538–546. doi:10.1111/j.1365-2567.2007.02723.x
Tonry CL, Leacy E, Raso C, Finn SP, Armstrong J, Pennington SR (2016) The role of proteomics in biomarker development for improved patient diagnosis and clinical decision making in prostate cancer. Diagnostics (Basel) 6(3). doi:10.3390/diagnostics6030027
Zhang G, Xu Y, Lu X, Huang H, Zhou Y, Lu B, Zhang X (2009) Diagnosis value of serum B7-H3 expression in non-small cell lung cancer. Lung Cancer 66(2):245–249. doi:10.1016/j.lungcan.2009.01.017
Chen DS, Mellman I (2013) Oncology meets immunology: the cancer-immunity cycle. Immunity 39(1):1–10. doi:10.1016/j.immuni.2013.07.012
Kaur S, Chang T, Singh SP, Lim L, Mannan P, Garfield SH, Pendrak ML, Soto-Pantoja DR, Rosenberg AZ, Jin S, Roberts DD (2014) CD47 signaling regulates the immunosuppressive activity of VEGF in T cells. J Immunol 193(8):3914–3924. doi:10.4049/jimmunol.1303116
Morioka M, Kobayashi T, Furukawa Y, Jo Y, Shinkai M, Matsuki T, Yamamoto T, Tanaka H (2002) Prostate-specific antigen levels and prognosis in patients with hormone-refractory prostate cancer treated with low-dose dexamethasone. Urol Int 68(1):10–15
Acknowledgments
The authors thank all the patients and their families, and the nurses for their assistance. The authors wish to thank Waters S.p.A. for providing the technical assistance and the UPLC-MS-MS system.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Funding
The present work was supported, in part, by the Italian Association for Cancer Research to GB.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Teresa Di Desidero and Lisa Derosa contributed equally to the study
Rights and permissions
About this article
Cite this article
Di Desidero, T., Derosa, L., Galli, L. et al. Clinical, pharmacodynamic and pharmacokinetic results of a prospective phase II study on oral metronomic vinorelbine and dexamethasone in castration-resistant prostate cancer patients. Invest New Drugs 34, 760–770 (2016). https://doi.org/10.1007/s10637-016-0385-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-016-0385-0