Summary
Purpose Preclinical data indicate that combination HER2-directed and anti-VEGF therapy may bypass resistance to trastuzumab. A phase I trial was performed to assess safety, activity, and correlates. Experimental design Patients with advanced, refractory malignancy were enrolled (modified 3 + 3 design with expansions for responding tumor types). Patients received lapatinib daily for 21 days, and bevacizumab and trastuzumab every 3 weeks. Correlates included HER2 extracellular domain levels (ECD) and single nucleotide polymorphisms (SNPs). Results Ninety-four patients were treated (median = four prior systemic therapies). The most common related adverse events ≥ grade 2 were diarrhea (n = 33, 35 %) and hypertension (n = 10, 11 %). The recommended phase 2 dose was trastuzumab 6 mg/m2 (loading = 8 mg/m2) and bevacizumab 15 mg/kg every 3 weeks, with lapatinib 1,250 mg daily (full FDA-approved dose of each drug). One patient (1 %) achieved a complete response (CR); eight (9 %), a partial response (PR) (includes breast (n = 7, one of which was HER2 2+ by IHC) and salivary ductal carcinoma (n = 1); and 14 (15 %), stable disease (SD) ≥6 months (total SD ≥ 6 months/PR/CR =23 (25 %). All patients with PR/CR received prior trastuzumab +/− lapatinib. SD ≥ 6 months/PR/CR rate and time to treatment failure (TTF) correlated with elevated baseline HER2 ECD (N = 75 patients tested) but not with HER2 SNPs. Conclusions Combination trastuzumab, lapatinib, and bevacizumab was well-tolerated and demonstrated antitumor activity in heavily pretreated patients with advanced malignancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human epidermal growth factor receptor 2 (HER2) is a protein in the epidermal growth factor receptor (EGFR) family. Overexpression of HER2 promotes neoplastic transformation of cells making it a popular therapeutic target. HER2 overexpression is seen in multiple tumor types, including breast (25–30 %) [1], gastric/esophageal (22 %) [2], pancreatic (16 %) [3], salivary gland (17 %) [4], cholangiocarcinoma (29 %) [5], gallbladder (10 %) [6], non-small cell lung (11 %) [7], and ovarian (5–15 %) [8]. HER2 correlates with poor prognosis and decreased overall survival in many tumor types, including breast, bladder, ovarian, endometrial, non-small cell lung cancer, and gastric cancer [9–14]. Inhibition of HER2 is an established therapy for HER2-positive breast and gastric cancer and is a promising therapy for other malignancies.
Trastuzumab, a monoclonal antibody that is Food and Drug Agency (FDA) approved for HER2 overexpressed breast cancer and gastric or gastroesophageal (GE) junction patients, binds to the extracellular domain of the HER2/neu protein and inhibits the proliferation of human tumor cells that overexpress HER2 [2, 15]. While trastuzumab improves overall survival and response rate, resistance has been shown to develop in metastatic breast cancer patients [16]. Therefore, the need to inhibit HER2 via alternate pathways exists. Lapatinib, also FDA approved for breast cancer patients, is a tyrosine kinase inhibitor of both epidermal growth factor receptor (EGFR) and HER2 [17]. In combination with capecitabine, lapatinib has been shown to improve time to progression in metastatic breast cancer patients who progressed on prior therapy, including trastuzumab [18]. Combining lapatinib and trastuzumab provides the opportunity to target two members of the HER subfamily simultaneously and both the extracellular and intracellular domains. Combining lapatinib and trastuzumab may be clinically more effective than either drug alone [19], perhaps because some tyrosine kinase receptors act through both kinase dependent and independent pathways [20, 21].
Vascular endothelial growth factor (VEGF) plays an important role in cancer development and metastases [22]. Bevacizumab was the first VEGF monoclonal antibody approved by the FDA to target tumor angiogenesis, and is now approved for colorectal, renal cell, non-small cell lung cancer, and glioblastoma [23–26], as well as demonstrates activity in ovarian and other cancers [27–29].
Overexpression of HER2 has been associated with upregulation of VEGF in breast and lung cancer cell lines [30, 31]. Preclinical data has shown that combining HER2 inhibition therapy and anti-VEGF therapy, bevacizumab, may bypass resistance to trastuzumab [32]. Clinically, two different phase II studies have shown responses in advanced HER2-postive breast cancer patients on combination trastuzumab and bevacizumab [33] and combination lapatinib and bevacizumab [34]. Phase II and III studies have also shown increased clinical efficacy of combination trastuzumab and lapatinib [35, 36]. These findings suggest combination HER2 and VEGF therapy may be a promising strategy to increase efficacy and overcome resistance.
We performed a phase I trial administering combination bevacizumab, trastuzumab, and lapatinib based on our hypothesis that this combination of concurrent HER2, EGFR, and VEGF inhibition could be given safely and would demonstrate antitumor activity in patients with varied tumor types. The primary objective of this study was to assess safety and tolerability as well as to define the maximum tolerated dose (MTD) of combination bevacizumab, trastuzumab, and lapatinib. Secondary objectives were to establish a preliminary assessment of anti-tumor activity and correlation of surrogate markers.
Materials and methods
Study design
The study was conducted at The University of Texas M. D. Anderson Cancer Center (MDACC) per Institutional Review Board guidelines. A modified 3 + 3 study design was used (Supplementary Methods). The treatment arm reported herein included all patients who started therapy between 11/19/2007 and 7/19/2012 as part of a dose-escalation study conducted in patients with advanced cancer. The treatment cycle repeated once every 21 days until prohibitive toxicity, tumor progression, or patient withdrawal. Patients were treated at variable dose levels, depending on the time of study entry (Table 1). Once the maximum tolerated dose (MTD) was determined, the dose level was expanded to include up to 14 additional patients per specific tumor type that had complete response (CR), partial response (PR), or stable disease (SD) >4 cycles. These tumor types included breast, gallbladder/cholangiocarcinoma, gastric/esophageal, ovarian/fallopian tube, pancreatic, salivary duct, and non-melanoma skin cancers.
Patients
Patients had metastatic or advanced cancer not amenable to standard therapy, an Eastern Cooperative Oncology Group (ECOG) performance status of 0–2 [37], and adequate hematologic, hepatic, and renal function. Exclusion criteria included hemoptysis, unexplained bleeding, significant cardiovascular disease, intercurrent uncontrolled illness, significant gastrointestinal bleeding within 28 days, hemorrhagic brain metastases, prior abdominal surgery within 30 days, pregnancy, and a history of hypersensitivity to bevacizumab, trastuzumab, lapatinib, Chinese hamster ovary cell proteins and/or any component of the formulations of these drugs. Treatment with prior cytotoxic therapies must have ended at least 3 weeks prior to enrollment, and biologic therapy must have ended at least 2 weeks or five drug half-lives prior to enrollment (whichever was shorter).
Patients with left ventricular ejection fraction of less than 50 % were excluded unless the individual was receiving an angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blocker (ARB) and a beta blocker. In addition, patients with prolonged QTc defined as greater than 440 milliseconds (males) and greater than 460 milliseconds (females) were excluded.
Safety
Clinically significant adverse events were assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE), version 3.0 [38]. History, physical exam, hematology, blood chemistry, and urinalysis were performed at baseline and regular intervals while receiving treatment.
Evaluation of efficacy
Treatment efficacy was evaluated by diagnostic imaging per Response Evaluation Criteria in Solid Tumors (RECIST) 1.0 [39]. Radiologic assessments were conducted at baseline and about every 6 weeks thereafter.
Molecular testing
Molecular testing was performed in the Clinical Laboratory Improvement Amendments (CLIA)-approved MDACC laboratory for patients with available archived tissue. BRAF, c-KIT, K/NRAS, c-MET, PIK3CA, and p53 mutation analysis were performed, as well as c-MET amplification by fluorescent in-situ hybridization (FISH) and PTEN expression by standard immunohistochemistry.
For BRAF (codons 468–474 in exon 11 and codons 595–600 in exon 15), c-KIT (exons 9, 11, 13, and 17), K/NRAS (codons 12, 13 and 61), PIK3CA (codons 532–554 in exon 9 and codons 1011–1062 in exon 20), EGFR (exons 18–21), and p53 mutation (exons 4–9) testing, polymerase chain reaction (PCR)-based sequencing analysis was performed on DNA extracted from paraffin-embedded tumor tissue. The lower limit of detection was approximately one cell bearing the mutation per five to ten normal cells. PTEN expression was determined by immunohistochemistry using anti-PTEN monoclonal mouse antibody (Dako, Carpinteria, CA).
Tissue was evaluated for HER-2/neu gene amplification by interphase FISH technique using the PathVysion HER-2/neu DNA Probe Kit (LSI HER-2/neu Spectrum Orange/CEP17 Spectrum Green).
Single Nucleotide Polymorphism (SNP)
Genomic DNA from 56 patients were isolated from white blood cell (WBC) fraction (also called buffy coat or PBMC) using a QIAamp DNA Blood Mini Kit (Qiagen, Germany). Then the region of interest of the five annotated single-nucleotide polymorphisms (SNPs) in the HER2 gene (−3444C > T, −1985 G > T, I655A A > G, P1170A C > G, rs1810132 STR C > T) was amplified using custom polymerase chain reaction (PCR) primers. Sanger sequencing was performed on a 3730xl DNA Analyzer (Applied Biosystems) using BigDye™ Terminator v3 chemistry (Applied Biosystems). Mutation analysis was performed using SeqScape®Software v2.5 (Applied Biosystems).
HER2 Extracellular Domain (ECD)
Plasma samples from 75 patients were obtained at baseline, 24–48 h post-dose, and end of cycle 1. Plasma circulating ECD/HER-2 was determined using a sandwich enzyme-linked immunosorbent assay (ELISA c-erbB2/c-neu Rapid Format Elisa kit QIA10™ Calbiochem®) for the extracellular domain of p185 to determine whether a soluble oncoprotein fragment can be detected in the plasma of cancer patients. A cutoff value of 5 ng/mL was used to distinguish individuals with elevated levels versus normal.
Statistical analysis
Analyses were descriptive and exploratory. Within-patient comparisons were analyzed using paired t-tests and Wilcoxon signed rank tests. Between-patient comparisons were analyzed using unpaired t-tests and Mann–Whitney tests. Correlations were assessed using either Pearson or Spearman correlation analyses. Non-parametric analyses were chosen when data were clearly not normally distributed and/or had clear outliers. Survival analysis was performed using Kaplan-Meier. Analysis of VEGF SNPs was performed using SPSS 19 computer software (SPSS Chicago, IL). Many of the analyses were based on small numbers of patients, and care must be taken when interpreting non-statistically-significant results. Due to the exploratory nature of the analyses, no adjustment was made for multiple testing.
Results
Demographics
Ninety-four patients with advanced metastatic cancer were enrolled (Table 2), 58 of which were women (61.7 %). All patients were pretreated, with a median of four prior systemic therapies (range 1–18). The median age was 60 years. Seventy-four patients (79 %) had archived tissue available for one or more molecular tests. None of 45 patients (0 %) tested demonstrated EGFR mutation; seven of 22 patients (32 %) demonstrated KRAS mutation; one of 10 patients (10 %) demonstrated c-MET mutation; three of 24 patients (13 %) demonstrated PIK3CA mutation; forty-four of 66 patients (67 %) demonstrated HER2 amplification; nineteen of 38 patients (50 %) demonstrated positive ER expression; ten of 35 patients (29 %) demonstrated positive PR expression; two of 11 patients (18 %) tested had loss of PTEN expression.
Adverse events
Thirty patients (32 %) did not experience a drug-related toxicity, and 44 patients (47 %) experienced no drug-related toxicity higher than grade 1. The most common treatment-related grade 2 or higher adverse events were diarrhea (n = 33, 35 %) and hypertension (n = 10, 11 %) (Table 1). Eight patients experienced dose-limiting toxicity (DLT) due to diarrhea (n = 8, dose levels 7, 10, 11, 12), and nausea and vomiting (n = 1, dose level 12). Twenty patients (21 %) required dose reduction for toxicity and eight patients (9 %) withdrew due to toxicity. No deaths resulted from adverse events.
Dose reduction was required in 20 out of 94 patients (21 %) due to one or more toxicities. Toxicities requiring dose reduction included diarrhea (n = 17), hypertension (n = 1), fatigue (n = 1), rash (n = 1), nausea (n = 1), skin fissure (n = 1), decreased left ventricular ejection fraction (n = 1), and hand and foot syndrome (n = 1).
There were no DLTs experienced at dose levels 1 through 6. At dose level 7, one out of six patients experienced grade 3 diarrhea. There were no DLTs experienced at dose levels 8 and 9. At dose level 10, one out of eight patients experienced grade 3 diarrhea. At dose level 11, one out of nine patients experienced grade 3 diarrhea. At dose level 12, five out of 38 patients experienced grade 3 diarrhea, one out of 38 patients experienced grade 3 nausea and grade 3 vomiting. The full FDA-approved doses were reached without identifying an MTD. Therefore, the recommended phase 2 dose (RP2D) was determined to be level 12 [40], which includes bevacizumab (15 mg/kg IV every 3 weeks), trastuzumab (loading dose =8 mg/m2 IV every 3 weeks; maintenance dose =6 mg/m2 IV every 3 weeks), and lapatinib (1,250 mg daily). Once the RP2D was determined, dose level 12 was further expanded to include up to 14 additional patients per specific tumor type that had CR, PR, or SD >4 cycles. These tumor types included breast, gallbladder/cholangiocarcinoma, gastric/esophageal, ovarian/fallopian tube, pancreatic, salivary duct, and non-melanoma skin cancers.
Antitumor activity
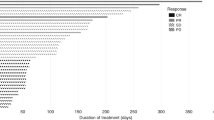
Ninety-four patients are included in the response data (Fig. 1). Three patients withdrew before the first restaging assessment due to toxicity. These three patients and any patients with early clinical progression are depicted as 21 % increase by RECIST (Fig. 1) and are considered treatment failures. Patients with non-measurable disease that achieved best response of stable disease are depicted on the figure as +0.5 %.
3D-Waterfall plot showing best response as determined by RECIST and time on study in 94 patients. The x-axis represents each patient. The y-axis indicates percent change in tumor size by RECIST. Patients who experienced at least 15 % tumor regression are color coded by tumor type. Patients with early clinical progression or new lesions and those that withdrew early due to toxicity are indicated arbitrarily as +21 % and are denoted with a star (*) and a “Ұ”, respectively. Additional information, including HER2 aberrations and non-measurable stable disease are also noted. The treatment duration (months) for each patient is depicted by the grey bars on the z-axis. The patient still on study at the time of submission is denoted with an arrow
A CR was observed in one patient (1 %) with breast cancer lasting 11 months. Eight patients (9 %) achieved a PR, one of which was unconfirmed. The patients with a confirmed PR had breast cancer (n = 6; 4, 5, 6, 8, 11, and 15 months) and HER2-amplified salivary duct cancer (n = 1; 27+ months). The salivary duct cancer patient with a PR for 27+ months was still on study at the time of submission. The patient with unconfirmed PR had HER2-positive breast cancer. One patient with HER2-negative breast cancer achieved partial response and had 2+ HER2 expression on immunohistochemistry. A patient with non-small cell lung cancer and a HER2 exon 20 mutation (insertion 774–775 AYVM) achieved disease stability lasting 8 months, including marked cavitation of some lung metastases [41]. An additional 13 patients (15 %) achieved SD lasting at least 6 months. The diagnoses of these patients were gallbladder (n = 1), pancreatic (n = 4), cholangiocarcinoma (n = 1), skin (n = 1), breast (n = 5), and ovarian (n = 1) cancers.
Prior antiangiogenic and HER2 inhibitor therapy and response
Of all 94 patients on study, 42 patients (45 %) did not receive prior bevacizumab, lapatinib, or trastuzumab. Thirteen patients (14 %) had received prior bevacizumab but no prior lapatinib or trastuzumab; 12 patients (13 %) had received prior trastuzumab but no prior bevacizumab or lapatinib; 24 patients (26 %) had received prior trastuzumab and lapatinib (seven in combination, 17 sequential treatment); two patients (2 %) had received prior bevacizumab and trastuzumab (one in combination, one sequential treatment); and one patient (1 %) received sequential bevacizumab and lapatinib.
Of the 42 patients who did not receive prior bevacizumab, lapatinib, or trastuzumab, five (12 %) had SD ≥6 months. Of the 24 patients who received prior trastuzumab and lapatinib, four (17 %) had SD ≥6 months, four (17 %) had a PR, and one (1 %) had a CR. These patients received prior trastuzumab and lapatinib in combination and in sequential treatments. Of the 12 patients that received prior trastuzumab but no prior bevacizumab or lapatinib, two (2 %) had SD ≥6 months and four (17 %) had a PR. Of the 13 patients who had received prior bevacizumab but no prior lapatinib or trastuzumab, no significant responses were seen. This was the same for the two patients (2 %) who received prior bevacizumab and trastuzumab and one patient (1 %) who received sequential bevacizumab and lapatinib.
Of the 8 patients with PR, four (50 %) had received prior trastuzumab and lapatinib. The remaining four patients with PR (50 %) had received prior trastuzumab. The one patient with a CR had received prior trastuzumab and lapatinib. Therefore, prior treatment did not preclude PR or CR.
Brain metastases and response
Of the 18 patients with brain metastases, 5 (28 %) achieved PR and 3 (17 %) achieved SD ≥6 months, with the longest duration being 27+ months and 18 months respectively. Therefore, the presence of brain metastases did not preclude PR or SD ≥6 months.
Dosing and response
Of the 55 patients on dose levels 10 to 12 (Table 1), 14 (25 %) achieved SD ≥6 months/PR. For the 39 patients treated at dose levels one to nine, nine (23 %) achieved SD ≥6 months/PR/CR. Response rate and SD ≥6 months was the same for dose levels 1–9 versus dose levels 10–12 (23 % vs. 25 % respectively, p = 1.00).
Molecular aberrations and response
Of the 94 patients on study, 43 (46 %) were HER2-positive by FISH. One HER2-positive patient (2 %) with breast cancer achieved a CR, seven HER2-positive patients (16 %) (six with breast cancer and one with salivary duct cancer) achieved a PR, and ten patients (23 %) (five with breast cancer and one each with non-melanoma skin, pancreatic, ovarian, gallbladder, and cholangiocarcinoma) achieved SD ≥6 months. One patient with non-small cell lung cancer had a HER2 mutation at exon 20 and achieved SD for 9 months. Twenty-two patients (23 %) were HER2-negative and 28 patients (30 %) were not tested for HER2 amplification or mutation. One HER2-negative breast cancer patient (5 %) achieved a PR, and one HER2-negative pancreatic cancer patient (5 %) achieved SD ≥6 months. Two patients (7 %) who were not tested for HER2 amplification achieved SD ≥6 months, both with pancreatic cancer.
Of the 45 patients tested, all were EGFR wild type, and 15 (33 %) achieved SD ≥ 6 months/PR/CR.
The tumors of 20 patients (51 %) were estrogen receptor positive and/or progesterone receptor positive including breast (n = 15), ovarian/fallopian tube (n = 3), pancreatic (n = 1), and melanoma (n = 1), while 17 patients (49 %) were negative for both. Achievement of SD ≥ 6 months/PR/CR was observed in six of the 20 patients (30 %) that had estrogen receptor positive and/or progesterone receptor positive tumors, versus ten of the 17 patients (59 %) that had tumors that were both estrogen and progesterone receptor negative (p = 0.10).
HER2 correlates and response
HER2 extracellular domain (ECD) levels were evaluated in 75 patients, and HER2 single nucleotide polymorphisms (SNPs) were evaluated in 56 patients. A significant difference was observed between baseline HER2 ECD levels of responders (SD ≥ 6 months/PR) (n = 20) and nonresponders (n = 55) (59 ng/mL vs. 10 ng/mL, p = 0.005). In addition, a significant difference was observed in percent decrease of HER2 ECD levels at 24–48 h between SD ≥ 6 months/PR and nonresponders (93 % vs. 82 %, p = 0.049). In contrast, no significant difference was observed in HER2 ECD levels or percent change at end of cycle 1 between SD ≥ 6 months/PR and nonresponders. SD ≥ 6 months/PR rate was higher in patients with elevated baseline HER2 ECD (>5 ng/mL) (n = 25) vs. normal baseline HER2 ECD (≤5 ng/mL) (n = 50) (48 % vs. 16 %, p = 0.003). Time to treatment failure (TTF) was also longer in patients with elevated baseline HER2 ECD (>5 ng/mL) vs. normal baseline HER2 ECD (≤5 ng/mL) (4.2 months vs. 1.4 months, p = 0.038). No significant difference in SD ≥ 6 months/PR/CR rate or TTF was observed when compared with each of the five HER2 SNPs.
Discussion
In this study, we report the results of a phase I dose-escalation trial of combination trastuzumab, lapatinib, and bevacizumab. The combination was well-tolerated, with successful escalation to the FDA-approved doses of all three drugs without reaching a maximum tolerated dose (MTD). The most common toxicity observed at the recommended phase 2 dose (RP2D) was diarrhea (35 %), which attributed primarily to the lapatinib. This diarrhea was managed easily in most patients with anti-diarrhea medication but required dose reduction (18 %) or treatment discontinuation (1 %) in a minority of patients. The prevalence and severity of diarrhea was similar to what has been reported previously in lapatinib monotherapy studies [42]. Although previous studies combining trastuzumab with lapatinib demonstrated poor tolerance of lapatinib doses above 1,000 mg, patients in our study tolerated 1,250 mg, possibly because of earlier and more aggressive intervention [35, 36].
Response (SD ≥6 months/PR/CR) was achieved in 50 % of heavily pretreated breast cancer patients in this study. These patients had all received prior trastuzumab and the majority prior lapatinib [43]. Despite failing prior concurrent or sequential trastuzumab and lapatinib treatment, these patients continued to achieve SD ≥ 6 months/PR/CR with the addition of bevacizumab to the treatment combination. Overcoming resistance to prior concurrent trastuzumab and lapatinib and achieving longer treatment duration with combination trastuzumab, lapatinib, and bevacizumab suggests that bevacizumab contributes to this HER2 treatment combination. Recent data suggests that bevacizumab is not effective in breast cancer, as demonstrated in well-designed randomized trials of unselected patients [44, 45]. However, it is conceivable that specific combinations such as those used herein might have activity or that subsets of patients may benefit. Prospective trials would need to address this issue.
Responses in non-breast cancer patients with HER2 aberrations were notable. A HER2-amplified salivary duct cancer patient in this study achieved resolution of measurable disease and minimal residual nonmeasurable disease for 27+ months. This patient was heavily pretreated with trastuzumab used in combination with radiation therapy or cytotoxic chemotherapy after which his tumor progressed suggesting that the combination overcame prior resistance to trastuzumab [46]. A HER2-mutant non-small cell lung cancer patient also achieved prolonged stable disease on this study combination, after progressing on prior systemic chemotherapy [41]. Combining bevacizumab and lapatinib with trastuzumab yielded salutary effects in these patients and suggests the activity of this treatment combination is not isolated to HER2-positive breast cancer patients alone.
Brain metastases are common in many HER2-positive cancers, and unfortunately, more effective treatments for brain metastases are needed. In a preclinical study, an anti-VEGFR2 antibody was combined with trastuzumab and lapatinib and significantly slowed growth and increased necrosis in brain metastases [47]. In our study, one of the four patients with progressing brain metastases at the time of enrollment achieved an unconfirmed PR and received treatment for 6 months. Overall, eight of 18 patients with brain metastases attained SD ≥ 6 months/PR, demonstrating that the presence of brain lesions did not preclude response.
Previous studies have demonstrated an association between HER2 single nucleotide polymorphisms (SNPs) and the risk of developing breast, lung, and gastric cancer [48, 49]. Our analysis revealed no association between these HER2 SNPs and SD ≥ 6 months/PR/CR rate or time to treatment failure. Our study is limited by small sample size and heterogeneous patient population, but future studies may consider exploring HER2 SNPs for potential prognostic value.
Consistent with previous studies [50], we found that elevated baseline plasma circulating HER2 extracellular domain (ECD) was associated with SD ≥ 6 months/PR rate and time to treatment failure. Further study of the value of this assay across tumor types is warranted.
Our study has several important limitations. Patients received different doses of drug, consistent with an early phase trial. On the other hand, we did not see a difference in the rate of SD ≥ 6 months/CR/PR at higher versus lower doses. The number of patients with each tumor type was small, and larger studies will need to be done to ascertain if response signals observed herein translate to meaningful efficacy. Finally, the analysis of the biologic correlates was retrospective and also limited by sample size.
In conclusion, the combination of trastuzumab, lapatinib, and bevacizumab is well-tolerated at full FDA-approved doses of each drug, and the combination has demonstrated clinical activity in patients with heavily pre-treated, advanced malignancy. HER2 ECD levels correlated with SD ≥ 6 months/PR and time to treatment failure. Most patients who achieved SD ≥ 6 months/CR/PR had HER2 positive breast cancer and showed salutary effects despite previous treatment with trastuzumab +/− lapatinib. Other disease categories also achieved SD ≥ 6 months/PR including a patient with non-small cell lung cancer harboring a HER2 mutation at exon 20, a patient with HER2+ salivary duct cancer, and patients with HER2-negative breast and pancreatic cancer (n = 1 of each). On this basis and the observation that the regimen was well tolerated and that heavily-pretreated patients who had previously progressed on anti-HER2 and anti-angiogenic treatment strategies attained SD ≥ 6 months/CR/PR, further evaluation of this combination is warranted.
References
Slamon DJ, Godolphin W, Jones LA, Holt JA, Wong SG, Keith DE, Levin WJ, Stuart SG, Udove J, Ullrich A et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244(4905):707–712
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Ruschoff J, Kang YK (2010) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376(9742):687–697. doi:10.1016/S0140-6736(10)61121-X
Safran H, Iannitti D, Ramanathan R, Schwartz JD, Steinhoff M, Nauman C, Hesketh P, Rathore R, Wolff R, Tantravahi U, Hughes TM, Maia C, Pasquariello T, Goldstein L, King T, Tsai JY, Kennedy T (2004) Herceptin and gemcitabine for metastatic pancreatic cancers that overexpress HER-2/neu. Cancer Invest 22(5):706–712
Glisson B, Colevas AD, Haddad R, Krane J, El-Naggar A, Kies M, Costello R, Summey C, Arquette M, Langer C, Amrein PC, Posner M (2004) HER2 expression in salivary gland carcinomas: dependence on histological subtype. Clin Cancer Res 10(3):944–946
Kim HJ, Yoo TW, Park DI, Park JH, Cho YK, Sohn CI, Jeon WK, Kim BI, Kim MK, Chae SW, Sohn JH (2007) Gene amplification and protein overexpression of HER-2/neu in human extrahepatic cholangiocarcinoma as detected by chromogenic in situ hybridization and immunohistochemistry: its prognostic implication in node-positive patients. Ann Oncol 18(5):892–897. doi:10.1093/annonc/mdm006
Pignochino Y, Sarotto I, Peraldo-Neia C, Penachioni JY, Cavalloni G, Migliardi G, Casorzo L, Chiorino G, Risio M, Bardelli A, Aglietta M, Leone F (2010) Targeting EGFR/HER2 pathways enhances the antiproliferative effect of gemcitabine in biliary tract and gallbladder carcinomas. BMC Cancer 10:631. doi:10.1186/1471-2407-10-631
Clamon G, Herndon J, Kern J, Govindan R, Garst J, Watson D, Green M (2005) Lack of trastuzumab activity in nonsmall cell lung carcinoma with overexpression of erb-B2: 39810: a phase II trial of cancer and leukemia group B. Cancer 103(8):1670–1675. doi:10.1002/cncr.20950
Yan M, Parker BA, Schwab R, Kurzrock R (2014) HER2 aberrations in cancer: implications for therapy. Cancer Treat Rev 40(6):770–780. doi:10.1016/j.ctrv.2014.02.008
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235(4785):177–182
Kolla SB, Seth A, Singh MK, Gupta NP, Hemal AK, Dogra PN, Kumar R (2008) Prognostic significance of Her2/neu overexpression in patients with muscle invasive urinary bladder cancer treated with radical cystectomy. Int Urol Nephrol 40(2):321–327. doi:10.1007/s11255-007-9283-x
Berchuck A, Kamel A, Whitaker R, Kerns B, Olt G, Kinney R, Soper JT, Dodge R, Clarke-Pearson DL, Marks P et al (1990) Overexpression of HER-2/neu is associated with poor survival in advanced epithelial ovarian cancer. Cancer Res 50(13):4087–4091
Hetzel DJ, Wilson TO, Keeney GL, Roche PC, Cha SS, Podratz KC (1992) HER-2/neu expression: a major prognostic factor in endometrial cancer. Gynecol Oncol 47(2):179–185
Tan D, Deeb G, Wang J, Slocum HK, Winston J, Wiseman S, Beck A, Sait S, Anderson T, Nwogu C, Ramnath N, Loewen G (2003) HER-2/neu protein expression and gene alteration in stage I-IIIA non-small-cell lung cancer: a study of 140 cases using a combination of high throughput tissue microarray, immunohistochemistry, and fluorescent in situ hybridization. Diagn Mol Pathol 12(4):201–211
Gravalos C, Jimeno A (2008) HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol 19(9):1523–1529. doi:10.1093/annonc/mdn169
Baselga J, Tripathy D, Mendelsohn J, Baughman S, Benz CC, Dantis L, Sklarin NT, Seidman AD, Hudis CA, Moore J, Rosen PP, Twaddell T, Henderson IC, Norton L (1996) Phase II study of weekly intravenous recombinant humanized anti-p185HER2 monoclonal antibody in patients with HER2/neu-overexpressing metastatic breast cancer. J Clin Oncol 14(3):737–744
Tripathy D, Slamon DJ, Cobleigh M, Arnold A, Saleh M, Mortimer JE, Murphy M, Stewart SJ (2004) Safety of treatment of metastatic breast cancer with trastuzumab beyond disease progression. J Clin Oncol 22(6):1063–1070. doi:10.1200/JCO.2004.06.557
Wood ER, Truesdale AT, McDonald OB, Yuan D, Hassell A, Dickerson SH, Ellis B, Pennisi C, Horne E, Lackey K, Alligood KJ, Rusnak DW, Gilmer TM, Shewchuk L (2004) A unique structure for epidermal growth factor receptor bound to GW572016 (Lapatinib): relationships among protein conformation, inhibitor off-rate, and receptor activity in tumor cells. Cancer Res 64(18):6652–6659. doi:10.1158/0008-5472.CAN-04-1168
Geyer CE, Forster J, Lindquist D, Chan S, Romieu CG, Pienkowski T, Jagiello-Gruszfeld A, Crown J, Chan A, Kaufman B, Skarlos D, Campone M, Davidson N, Berger M, Oliva C, Rubin SD, Stein S, Cameron D (2006) Lapatinib plus capecitabine for HER2-positive advanced breast cancer. N Engl J Med 355(26):2733–2743. doi:10.1056/NEJMoa064320
Blackwell KL, Burstein HJ, Storniolo AM, Rugo HS, Sledge G, Aktan G, Ellis C, Florance A, Vukelja S, Bischoff J, Baselga J, O’Shaughnessy J (2012) Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 Study. J Clin Oncol 30(21):2585–2592. doi:10.1200/JCO.2011.35.6725
Weihua Z, Tsan R, Huang WC, Wu Q, Chiu CH, Fidler IJ, Hung MC (2008) Survival of cancer cells is maintained by EGFR independent of its kinase activity. Cancer Cell 13(5):385–393. doi:10.1016/j.ccr.2008.03.015
Janku F, Huang HJ, Angelo LS, Kurzrock R (2013) A kinase-independent biological activity for insulin growth factor-1 receptor (IGF-1R): implications for inhibition of the IGF-1R signal. Oncotarget 4(3):463–473
Holash J, Maisonpierre PC, Compton D, Boland P, Alexander CR, Zagzag D, Yancopoulos GD, Wiegand SJ (1999) Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF. Science 284(5422):1994–1998
Ferrara N, Hillan KJ, Gerber HP, Novotny W (2004) Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat Rev Drug Discov 3(5):391–400. doi:10.1038/nrd1381
Yang JC, Haworth L, Sherry RM, Hwu P, Schwartzentruber DJ, Topalian SL, Steinberg SM, Chen HX, Rosenberg SA (2003) A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med 349(5):427–434. doi:10.1056/NEJMoa021491
Johnson DH, Fehrenbacher L, Novotny WF, Herbst RS, Nemunaitis JJ, Jablons DM, Langer CJ, DeVore RF 3rd, Gaudreault J, Damico LA, Holmgren E, Kabbinavar F (2004) Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol 22(11):2184–2191. doi:10.1200/JCO.2004.11.022
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27(28):4733–4740. doi:10.1200/JCO.2008.19.8721
Burger RA, Sill MW, Monk BJ, Greer BE, Sorosky JI (2007) Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a gynecologic oncology group study. J Clin Oncol 33:5165–5171. doi:10.1200/JCO.2007.11.5345
Wright JD, Viviano D, Powell MA, Gibb RK, Mutch DG, Grigsby PW, Rader JS (2006) Bevacizumab combination therapy in heavily pretreated, recurrent cervical cancer. Gynecol Oncol 103(2):489–493. doi:10.1016/j.ygyno.2006.03.023
Miller KD, Chap LI, Holmes FA, Cobleigh MA, Marcom PK, Fehrenbacher L, Dickler M, Overmoyer BA, Reimann JD, Sing AP, Langmuir V, Rugo HS (2005) Randomized phase III trial of capecitabine compared with bevacizumab plus capecitabine in patients with previously treated metastatic breast cancer. J Clin Oncol 23(4):792–799. doi:10.1200/JCO.2005.05.098
Yen L, You XL, Al Moustafa AE, Batist G, Hynes NE, Mader S, Meloche S, Alaoui-Jamali MA (2000) Heregulin selectively upregulates vascular endothelial growth factor secretion in cancer cells and stimulates angiogenesis. Oncogene 19(31):3460–3469. doi:10.1038/sj.onc.1203685
Konecny GE, Meng YG, Untch M, Wang HJ, Bauerfeind I, Epstein M, Stieber P, Vernes JM, Gutierrez J, Hong K, Beryt M, Hepp H, Slamon DJ, Pegram MD (2004) Association between HER-2/neu and vascular endothelial growth factor expression predicts clinical outcome in primary breast cancer patients. Clin Cancer Res 10(5):1706–1716
du Manoir JM, Francia G, Man S, Mossoba M, Medin JA, Viloria-Petit A, Hicklin DJ, Emmenegger U, Kerbel RS (2006) Strategies for delaying or treating in vivo acquired resistance to trastuzumab in human breast cancer xenografts. Clin Cancer Res 12(3 Pt 1):904–916. doi:10.1158/1078-0432.CCR-05-1109
Hurvitz S, Pegram M, Lin L, Chan D, Allen H, Dichmann R, et al. (2009) Final results of a phase II trial evaluating Trastuzumab and Bevacuzumab as first line treatment of HER2-amplified advanced breast cancer. Thirty-Second Annual Cancer Therapy & Research Center-American Association for Cancer Research San Antonio Breast Cancer Symposium 2009 San Antonio, TX: American Association for Cancer Research; 2009
Rugo HS, Chien AJ, Franco SX, Stopeck AT, Glencer A, Lahiri S, Arbushites MC, Scott J, Park JW, Hudis C, Nulsen B, Dickler MN (2012) A phase II study of lapatinib and bevacizumab as treatment for HER2-overexpressing metastatic breast cancer. Breast Cancer Res Treat 134(1):13–20. doi:10.1007/s10549-011-1918-z
Blackwell KL, Burstein HJ, Storniolo AM, Rugo H, Sledge G, Koehler M, Ellis C, Casey M, Vukelja S, Bischoff J, Baselga J, O’Shaughnessy J (2010) Randomized study of Lapatinib alone or in combination with trastuzumab in women with ErbB2-positive, trastuzumab-refractory metastatic breast cancer. J Clin Oncol 28(7):1124–1130. doi:10.1200/JCO.2008.21.4437
Baselga J, Bradbury I, Eidtmann H, Di Cosimo S, de Azambuja E, Aura C, Gomez H, Dinh P, Fauria K, Van Dooren V, Aktan G, Goldhirsch A, Chang TW, Horvath Z, Coccia-Portugal M, Domont J, Tseng LM, Kunz G, Sohn JH, Semiglazov V, Lerzo G, Palacova M, Probachai V, Pusztai L, Untch M, Gelber RD, Piccart-Gebhart M (2012) Lapatinib with trastuzumab for HER2-positive early breast cancer (NeoALTTO): a randomised, open-label, multicentre, phase 3 trial. Lancet 379(9816):633–640. doi:10.1016/S0140-6736(11)61847-3
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern cooperative oncology group. Am J Clin Oncol 5(6):649–655
Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, Rubin P (2003) CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol 13(3):176–181. doi:10.1016/S1053-4296(03)00031-6
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European organization for research and treatment of cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Falchook G S, Wheler JJ, Naing A, Hong DS, Moulder SL, Piha-Paul SA, Ng CS, Jackson E, Kurzrock R (2010) A phase I study of bevacizumab in combination with sunitinib, sorafenib, and erlotinib plus cetuximab, and trastuzumab plus lapatinib. Paper presented at the American Society of Clinical Oncology Annual Meeting, Chicago, IL
Falchook GS, Janku F, Tsao AS, Bastida CC, Stewart DJ, Kurzrock R (2013) Non-small-cell lung cancer with HER2 exon 20 mutation: regression with dual HER2 inhibition and anti-VEGF combination treatment. J Thorac Oncol 8(2):e19–20. doi:10.1097/JTO.0b013e31827ce38e
Burris HA 3rd (2004) Dual kinase inhibition in the treatment of breast cancer: initial experience with the EGFR/ErbB-2 inhibitor lapatinib. Oncologist 9(Suppl 3):10–15
Falchook GS, Moulder SL, Wheler JJ, Jiang Y, Bastida CC, Kurzrock R (2013) Dual HER2 inhibition in combination with anti-VEGF treatment is active in heavily pretreated HER2-positive breast cancer. Ann Oncol 24(12):3004–3011. doi:10.1093/annonc/mdt395
Robert NJ, Dieras V, Glaspy J, Brufsky AM, Bondarenko I, Lipatov ON, Perez EA, Yardley DA, Chan SY, Zhou X, Phan SC, O’Shaughnessy J (2011) RIBBON-1: randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2-negative, locally recurrent or metastatic breast cancer. J Clin Oncol 29(10):1252–1260. doi:10.1200/JCO.2010.28.0982
Cameron D, Brown J, Dent R, Jackisch C, Mackey J, Pivot X, Steger GG, Suter TM, Toi M, Parmar M, Laeufle R, Im YH, Romieu G, Harvey V, Lipatov O, Pienkowski T, Cottu P, Chan A, Im SA, Hall PS, Bubuteishvili-Pacaud L, Henschel V, Deurloo RJ, Pallaud C, Bell R (2013) Adjuvant bevacizumab-containing therapy in triple-negative breast cancer (BEATRICE): primary results of a randomised, phase 3 trial. Lancet Oncol 14(10):933–942. doi:10.1016/S1470-2045(13)70335-8
Falchook GS, Lippman SM, Bastida CC, Kurzrock R (2014) Human epidermal receptor 2-amplified salivary duct carcinoma: regression with dual human epidermal receptor 2 inhibition and anti-vascular endothelial growth factor combination treatment. Head Neck 36(3):E25–27. doi:10.1002/hed.23429
Kodack DP, Chung E, Yamashita H, Incio J, Duyverman AM, Song Y, Farrar CT, Huang Y, Ager E, Kamoun W, Goel S, Snuderl M, Lussiez A, Hiddingh L, Mahmood S, Tannous BA, Eichler AF, Fukumura D, Engelman JA, Jain RK (2012) Combined targeting of HER2 and VEGFR2 for effective treatment of HER2-amplified breast cancer brain metastases. Proc Natl Acad Sci U S A 109(45):E3119–3127. doi:10.1073/pnas.1216078109
Frank B, Hemminki K, Wirtenberger M, Bermejo JL, Bugert P, Klaes R, Schmutzler RK, Wappenschmidt B, Bartram CR, Burwinkel B (2005) The rare ERBB2 variant Ile654Val is associated with an increased familial breast cancer risk. Carcinogenesis 26(3):643–647. doi:10.1093/carcin/bgh342
Kallel I, Kharrat N, Al-fadhly S, Rebai M, Khabir A, Boudawara TS, Rebai A (2010) HER2 polymorphisms and breast cancer in Tunisian women. Genet Test Mol Biomark 14(1):29–35. doi:10.1089/gtmb.2009.0069
Kostler WJ, Schwab B, Singer CF, Neumann R, Rucklinger E, Brodowicz T, Tomek S, Niedermayr M, Hejna M, Steger GG, Krainer M, Wiltschke C, Zielinski CC (2004) Monitoring of serum Her-2/neu predicts response and progression-free survival to trastuzumab-based treatment in patients with metastatic breast cancer. Clin Cancer Res 10(5):1618–1624
Acknowledgments
We would like to thank the patients and their families for their participation in this clinical trial. We would also like to thank Adrienne Howard for regulatory protocol assistance. This work was supported by the Paul Calabresi Career Development Award for Clinical Oncology K12 CA088084.
Conflict of interest
Dr. Falchook receives research funding and travel reimbursement from GlaxoSmithKline. The other authors declare that they have no conflict of interest.
Financial support
Paul Calabresi Career Development Award for Clinical Oncology K12 CA088084
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 23 kb)
Rights and permissions
About this article
Cite this article
Falchook, G.S., Moulder, S., Naing, A. et al. A phase I trial of combination trastuzumab, lapatinib, and bevacizumab in patients with advanced cancer. Invest New Drugs 33, 177–186 (2015). https://doi.org/10.1007/s10637-014-0173-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-014-0173-7