Summary
Background RO4929097 is an oral inhibitor of γ -secretase that results in Notch signaling inhibition. Prior work has demonstrated that Notch signaling inhibition enhances chemotherapy sensitivity of cancer cells. This phase I study was conducted to determine maximum tolerated dose (MTD), toxicities and efficacy of RO4929097 and capecitabine in advanced solid tumors. Methods Patients with refractory solid tumors received capecitabine at a fixed dose of 1,000 mg/m2 twice daily with escalating doses of RO4929097 on a 21-day cycle in a 3 + 3 design. Capecitabine was administered for 14 days and the RO49029097 once daily, 3 days per week, both for a 21 day cycle. Results Thirty patients were treated on six dose levels (20 to 150 mg). The maximally tolerated dose was not reached. One dose limiting toxicity was observed at each level 3 through 6 (hypophosphatemia, fatigue, and nausea/vomiting). Three confirmed partial responses were observed: two patients with fluoropyrimide-refractory colon cancer and one patient with cervical cancer. Autoinduction of RO4929097 was demonstrated with increasing dose levels and duration. Conclusions The recommended phase 2 dose is capecitabine 1,000 mg/m2 orally twice daily on days 1 through 14 with RO4929097 20 mg orally once daily on days 1–3, 8–10 and 15–17 with a 21 day cycle. Clinical benefit was observed in cervical and colon cancer. Autoinduction of RO4929097 was seen both with increasing cycle number and increasing dose. Plasma concentrations of RO4929097 were above those needed for Notch inhibition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Notch is a cell surface protein receptor involved in transmitting growth and proliferation signals to the cell [1]. Activation of Notch occurs through ligand binding. Two Notch ligand families, Jagged and Delta, have been described in mammals with five ligands identified to date (Jagged 1, 2, and Delta 1, 3, 4). After ligand binding, two successive proteolytic cleavage steps occur. The first step is mediated by ADAM/TACE (a disintegrin and metalloprotease/tumor-necrosis factor α converting enzyme) and occurs at the S2 cleavage site. The second step occurs at the S3 cleavage site and is mediated by the γ-secretase complex. The γ-secretase complex is involved in cleaving and activating the cell surface protein receptor of Notch [2].
Increased activation of Notch signaling is associated with several tumors, including T-cell acute lymphoblastic leukemia [3, 4], breast cancer [5–7], melanoma [8–10], lung cancer [11–13] and colon cancer [14]. In colon cancer, increasing expression of Notch-1 genes occurs as tumors progress through the adenoma to carcinoma sequence and is even greater in metastases [14]. Blocking Notch signaling via γ-secretase inhibition produces a slower growing, less transformed phenotype in human cancer cells in vivo. Notch inhibitors also enhance chemotherapy sensitivity and decrease the production of prosurvival factors by colon cancer cells [14].
RO4929097 is a potent and selective oral inhibitor of γ-secretase that shows antitumor activity in multiple animal models [15]. RO4929097 is active when dosed orally using either an intermittent or continuous daily dosing schedule. Efficacy is maintained for up to 90 days post-dosing with histological analysis showing a phenotype indicative of Notch signaling inhibition. In the first-in-human phase 1 study, multiple schedules were found to be tolerated [16]. Common side effects were fatigue, myelosuppression, fever, rash, chills, anorexia and hypophosphatemia. Radiographic responses by RECIST were seen in colorectal cancer, sarcoma and melanoma [16].
Capecitabine is an oral prodrug, which is approved by the United States Food and Drug Administration (FDA) for breast and colorectal cancer. Wide ranges of doses, schedules, and concomitant medications have been studied, but a dose of 1,000 mg/m2 orally twice daily on days 1 through 14 of a 21 day cycle as monotherapy has demonstrated efficacy in breast and colorectal cancers [17–19]. Extrapolating from the results of Meng et al. [14] showing γ -secretase inhibitors enhanced the chemotherapy sensitivity of colon cancer cells and decrease prosurvival factors, we hypothesized that RO4929097 would increase chemotherapy sensitivity to capecitabine in otherwise chemotherapy resistant metastatic colorectal and breast cancer. The presence of autoinduction and cytochrome P450 (CYP) interactions was also explored via correlate studies. The goal of this study was to establish the recommended phase 2 dose of the combination of RO4929097 and capecitabine.
Materials and methods
Patient selection
Eligible patients had a histologically documented, advanced solid malignancy refractory to standard therapy or for which no curative therapy existed. Other inclusion criteria included: age of at least 18 years; Eastern Cooperative Oncology Group (ECOG) performance status of 0 to 2; adequate hematologic, hepatic and renal functions (total white blood cell count ≥3,000/μl, absolute neutrophil count ≥1,500/μl, platelets ≥100,000/μl, total bilirubin within institutional normal limit, aspartate transaminase/alanine transaminase ≤2.5 x the institutional upper limit of normal, creatinine ≤1.5 mg/dl or creatinine clearance ≥60 ml/min/1.73 m2 for patients with creatinine levels above institutional normal); and life expectancy greater than 12 weeks.
Exclusion criteria included untreated brain metastasis; chemotherapy or radiation therapy within 4 weeks; anti-epileptics metabolized by cytochrome P450 history of cirrhosis or uncontrolled electrolyte abnormalities; active infection; HIV, baseline prolonged corrected QT interval on ECG (defined as baseline QTcF (QT interval using Fridericia’s formula) >450 msec [male] or QTcF >470 msec [female]), and known dihydropyrimidine dehydrogenase (DPD) deficiency. Patients were required to practice effective birth control.
All patients provided written informed consent. The protocol was approved by the Institutional Review Board of both institutions.
Dose escalation
This was a phase I dose escalation study using a standard 3 + 3 schema (see Table 1). The starting dose of capecitabine was 1,000 mg/m2 BID for 14 days of a 21 day cycle and was not escalated throughout the study. The RO4929097 dose was initiated at 20 mg orally daily for three consecutive days followed by 4 days off (days 1–3, 8–10 and 15–17), and escalated as seen in Table 1. This starting dose was selected because of preliminary results from pharmacokinetic andpharmacodynamic studies, showing minimal toxicities at a dose of up to 40 mg, but with auto-induction likely seen at doses of 60 mg or higher. This inducible effect appeared to be dependent upon both exposure and duration. Thus, to optimize patient safety and minimize autoinduction, dose escalation was begun at 20 mg of RO4929097 daily. The maximum tolerated dose (MTD) was defined as the highest dose at which there were less than two of six patients with a dose-limiting toxicity (DLT).
Definition of dose limiting toxicities
Adverse events were evaluated using the National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. DLT was defined as a toxicity that was considered at least possibly related to RO4929097 in combination with the planned dose of capecitabine. DLTs were defined as one of the following adverse events occurring during the first cycle: absolute neutrophil countless than500 for at least 7 days; febrile neutropenia or grade 3 or greater neutropenic infection; platelets less than 25,000 or thrombocytopenic bleeding; nonhematologic toxicity grade 3 or greater except nausea, vomiting, or diarrhea associated with suboptimal premedication and/or management; aspartate transaminase/alanine transaminase elevations grade 3 or higher for more than 7 days; toxicity leading to two or more missed doses per cycle; and toxicity resulting in the delay of the subsequent cycle by 14 days or greater.
Follow-up assessments
Imaging was required every three cycles (9 weeks) with laboratory evaluations prior to each cycle of therapy every 3 weeks. Disease status was assessed with the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1 [20]. Electrocardiograms were performed as clinically indicated, including with electrolyte disturbances.
Pharmacokinetics
Sample collection
Blood samples for evaluation of RO4929097 pharmacokinetics were collected at baseline and 1, 2, 3, 4, 8, 12, 16 and 24 h after oral administration of RO4929097 on day 3 and day 10 of cycle 1. Samples for evaluation of capecitabine and its metabolites were obtained at baseline, 1, 2, 3, 4 and 8 h after capecitabine administration during cycle 1. Whole blood was centrifuged to obtain plasma by standard methods and stored at −70° Celsius until analysis. Concentrations of RO4909927 and capecitabine were quantitated with a liquid chromatography-electrospray ionization tandem mass spectrometric method as previously described [21].
Sample preparation
Samples contained 50 μL of subject plasma. After microfuge, samples were quantitated by linear regression from a six-point standard curve ranging from 3.91 to 1,000 ng/mL with a trend line (r2) of 0.990 over the range. This quantitative method’s lower limit of quantitation (LLOQ) was 15.62 ng/ mL, and the lower limit of detection (LOD) was 3.91 ng/ mL. Recovery of RO4909927 from plasma was greater than 99 % compared to water standards. Intraday variability was 0.62 % for low-standard triplicates and 1.46 % for middle-standard triplicates and 0.36 % for high-standard triplicates. The interday variability over 35 days was 6.48 % for a low standard, 4.32 % for the middle standard, and 1.68 % for a high standard. 5-fluorouracil (5FU), capecitabine, 5′-deoxy-5-fluorocytidine (DFCR) and 5-flurouradine (DFUR) plasma concentrations were evaluated with a Spectra Physics P2000 HPLC as previously described [21].
Statistical analysis
The primary outcome measure of this study was assessment of toxicity. The number and severity of toxicity incidents determined the level of tolerance for RO4909927 and capecitabine were categorization via Common Terminology Criteria for Adverse Events standard toxicity grading. The number of treatment anti-tumor responses served as the secondary outcome measure and were summarized by simple descriptive summary statistics delineating complete and partial responses as well as stable and progressive disease.
Pharmacokinetic parameters were determined by noncompartmental methods with WinNonlin Pro version 5.3 (Pharsight Corporation, Cary, N.C.). Area under the plasma concentration–time curve was estimated using the trapezoidal rule from time 0 to peak concentration and the log-trapezoidal rule from the peak concentration to the last measurable plasma concentration (AUClast). AUC (0– ∞) was then calculated from the time of dosing and extrapolated to infinity. Dose adjusted Cmax and AUC values were calculated by dividing Cmax and AUC by the dose administered (in mg). Dose adjusted Css was calculated by dividing the cycle 2, day 1 plasma concentration prior to dosing by the dose administered. All pharmacokinetic parameters were summarized by standard descriptive statistics in terms of means and standard deviations. A two-sample t-test was used to evaluate changes in the pharmacokinetic parameters between the day 3 and the day 10 assessments. Analysis of variance was conducted to compare pharmacokinetic parameters between dose levels. AUC and Cmax values were log-transformed before conducting the comparisons. Due to the exploratory nature of the pharmacokinetic analysis, no adjustments for multiple comparisons were used. All p-values were two-tailed and p < 0.05 was used for defining statistical significance. Data analyses were performed using SAS® (SAS Institute Inc., Cary, North Carolina) version 9.2.
Results
Patients
Thirty patients were accrued at two large academic cancer centers, the University of Wisconsin Carbone Cancer Center (Madison, Wisconsin) and Princess Margaret Cancer Centre (Toronto, Ontario, Canada). Baseline patient characteristics are summarized in Table 2.
Dose escalation
Dose escalation began at level 1 and continued to dose level 6. The MTD was not reached. One DLT was observed at each level from 3 through 6. Observed DLTs were grade 3 hypophosphatemia with prolonged QT interval, intolerable grade 2 fatigue which resulted in getting less than 75 % of planned doses, grade 3 hypophosphatemia which took greater than 72 h to resolve despite supplementation, and grade 2 nausea and vomiting which resulting in delivery of less than 75 % of planned doses. At each level, the dose cohort was expanded, and no further DLTs were seen. At dose level 6, the study was closed when the clinical development of RO4929097 was stopped by the manufacturer.
Tolerability
Common side effects thought to be at least possibly related to the study drug, and experienced by at least 10 % of patients included nausea (70 %), vomiting (47 %), hypophosphatemia (47 %), diarrhea (47 %), and fatigue (53 %) (Table 3). One episode of hypophosphatemia was associated with ECG changes (QT interval prolongation) and one episode took longer than 72 h to resolve, despite holding the study drugs.
Pharmacokinetics
The primary pharmacokinetic endpoint was to compare day 3 and day 10 cycle 1 pharmacokinetic parameters. Pharmacokinetic parameters for RO4929097 by dose level as well as dose adjusted AUC and Cmax for all cycles are depicted in Table 4. Statistical comparisons were not performed within the dose levels given the small sample sizes in each dose level, however, AUC and Cmax were dose adjusted, and pharmacokinetic parameters across dose levels were combined and are also presented in Table 4. The combined data demonstrates a significant decrease in both dose adjusted RO4929097 AUC, declining from 666 ± 444 ng*hr/mg on day 3 to 296 ± 256 ng*hr/mg on day 10, and dose adjusted Cmax, declining from 23.5 ± 11.8 ng/mL/mg on day 3 to 14.3 ± 8.5 ng/mL/mg on day 10 (p < 0.0001 for both comparisons). The half-life declined between days 3 and 10, decreasing from 28.2 ± 42.9 h on day 3 to 16.7 ± 10.6 h on day 10 (p < 0.0001) with a corresponding increase in clearance, suggesting autoinduction of metabolism occurs by day 10 of cycle 1 with this schedule.
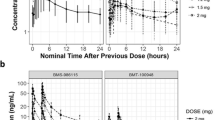
The dose-adjusted steady-state concentrations on cycle 2, day 1, prior to RO4929097 administration, were also evaluated by dose level with results shown in Fig. 1a. While RO4929097 concentration tended to decrease at higher dose levels, there is no significant correlation between concentration and dose (R2 = −0.17 (95 % CI: −0.53–0.24, p = 0.4136), also supporting autoinduction of metabolism by RO4929097.
As an additional assessment of dose linearity and as a correction for induction seen between day 7 and day 10, the ratio of day 10/day 7 non-dose adjusted Cmax and AUC were compared across dose levels. (See Fig. 1b and 2c) While the overall trend was a decrease with increasing doses, there were no significant changes in Cmax or AUC with increasing dose.
Pharmacokinetic parameters of capecitabine and metabolites were similar to previously reported parameters (data not shown).
Antitumor activity
Three confirmed partial responses were seen in two patients with previously heavily treated, fluoropyrimidine-refractory colorectal cancer, and one patient with previously treated cervical cancer (10 %). The response time ranged from approximately 4 to 5 months. There were also nine patients (30 %) with stable disease as their best response, with stable disease defined as per RECIST [17] and after three or more cycles. The response time ranged from 4 to 7.5 months. Stable disease was seen in at least one patient with colorectal cancer, carcinoid (low grade neuroendocrine carcinoma), cholangiocarcinoma and head and neck cancer. Eighteen patients (60 %) had progressive disease as their best response.
Discussion
This phase I study evaluated the combination of the oral γ secretase inhibitor RO4929097 along with capecitabine. The intent of combining these two drugs was that the addition of RO4929097 was to possibly overcome chemotherapy resistance in refractory solid tumors. Consequently, the responses and prolonged periods of stable disease that were seen in 5-FU refractory colorectal cancer patients may be clinically meaningful, but the inability to dose escalation the RO4929097 due to autoinduction with increasing doses limits our ability to fully evaluate this observation.
Relatively infrequent and expected grade 3 and 4 toxicities were seen, including nausea, vomiting, diarrhea, hypophosphatemia and fatigue. No MTD was reached, but increasing levels of autoinduction of RO4929097 were seen at escalating doses. The plasma concentrations of RO4929097 also decreased with increasing duration of dosing. Thus, the highest serum levels of RO4929097 were seen at dose level 1. The recommended phase 2 doses for this combination are capecitabine 1,000 mg/m2 orally twice daily for days 1–14 plus RO4909297 20 mg daily days 1–3, 8–10 and 15–17 of a 21-day cycle.
Prior studies have demonstrated autoinduction of RO4929097 [2], but not all pharmacokinetic studies of this agent have identified this effect [24]. We demonstrated that RO4929097 induces its own metabolism with increasing dose level and with increasing duration of treatment. Although a linear increase was expected, we observed a decrease in half-life, with decreased or stabilized Cmax/dose with each increasing dose level. Trough (Css) levels similarly decreased with each increasing dose level with some patients having no detectable RO4929097 prior to the first day of the second cycle. Additionally, the RO4929097 AUC decreased with increasing drug dose, suggesting futility of further dose escalation at achieving higher levels of RO4929097. The volume of distribution similarly increased with increasing dose and frequency, but did not entirely explain the change in AUC, Cmax, or Css. This autoinduction makes dose escalation challenging. However, in spite of this autoinduction, at all dose levels, the Cmax appeared to be above the level required for Notch inhibition in the plasma. Thus, the initial dose appeared to be enough to have on-target effects.
Promising partial responses were seen in two patients with fluoropyrimidine-refractory colorectal cancer and one patient with cervical cancer. Typically, capecitabine as a monotherapy should not be as effective after progression on fluoropyrimidine therapy. Although it is challenging to draw many conclusions from a phase I study due to the inherently small sample sizes and dose escalation design, these responses support manipulation of the Notch pathway as a potentially meaningful route for treating cancers, in particular colorectal cancer. This also supports the hypothesis that RO4929097 may have accentuated the chemotherapy sensitivity of the cancer cells and enhanced the effectiveness of capecitabine. This response presumably is not just unique to RO4929097, but should be seen with other γ –secretase inhibitors and warrants future clinical trials. There are other Notch and γ –secretase inhibitors still in clinical development, including MK-0752, LY-411 and PF-03084014, among others [22]. The logical next step in targeting of this pathway will be in developing a γ –secretase inhibitor which does not have autoinduction and can successfully be paired with either 5-fluorouracil or capecitabine. Prior evidence of RO4929097’s ability to enhance VEGF pathway blockade activity after resistance may be another logical pathway to exploit for bevacizumab and/or regorafenib refractory colorectal cancers [23].
In conclusion, the combination of RO4929097 and capecitabine is well tolerated and showed some promising tumor activity in fluoropyrimidine-refractory metastatic colorectal cancer. RO4929097 did demonstrate autoinduction at all dose levels which limited the ability to dose escalate the doses. Activity was seen in colorectal cancer supporting the development of γ –secretase inhibitors further in this disease.
References
Purow B (2012) Notch inhibition as a promising new approach to cancer therapy. Adv Exp Med Biol 727:305–19
Tolcher AW, Messersmith WA, Mikulski SM et al (2012) Phase I study of RO4929097, a gamma secretase inhibitor of Notch signaling, in patients with refractory metastatic or locally advanced solid tumors. J Clin Oncol 30:2348–2353
Aster JC, Pear WS, Blacklow SC (2008) Notch signaling in leukemia. Annu Rev Pathol 3:587–613
Staal FJ, Langerak AW (2008) Signaling pathways involved in the development of T-cell acute lymphoblastic leukemia. Haematologica 93:493–497
Dickson BC, Mulligan AM, Zhang H et al (2007) High-level JAG1 mRNA and protein predict poor outcome in breast cancer. Mod Pathol 20:685–693
Reedijk M, Odorcic S, Chang L et al (2005) High-level coexpression of JAG1 and NOTCH1 is observed in human breast cancer and is associated with poor overall survival. Cancer Res 65:8530–8537
Reedijk M, Pinnaduwage D, Dickson BC et al (2008) JAG1 expression is associated with a basal phenotype and recurrence in lymph node-negative breast cancer. Breast Cancer Res Treat 111:439–448
Massi D, Tarantini F, Franchi A et al (2006) Evidence for differential expression of Notch receptors and their ligands in melanocytic nevi and cutaneous malignant melanoma. Mod Pathol 19:246–254
Okuyama R, Tagami H, Aiba S (2008) Notch signaling: its role in epidermal homeostasis and in the pathogenesis of skin diseases. J Dermatol Sci 49:187–194
Pinnix CC, Herlyn M (2007) The many faces of Notch signaling in skin-derived cells. Pigment Cell Res 20:458–465
Chen Y, De Marco MA, Graziani I et al (2007) Oxygen concentration determines the biological effects of NOTCH-1 signaling in adenocarcinoma of the lung. Cancer Res 67:7954–7959
Konishi J, Kawaguchi KS, Vo H et al (2007) Gamma-secretase inhibitor prevents Notch3 activation and reduces proliferation in human lung cancers. Cancer Res 67:8051–8057
Peacock CD, Watkins DN (2008) Cancer stem cells and the ontogeny of lung cancer. J Clin Oncol 26:2883–2889
Meng RD, Shelton CC, Li YM et al (2009) Gamma-secretase inhibitors abrogate oxaliplatin-induced activation of the Notch-1 signaling pathway in colon cancer cells resulting in enhanced chemosensitivity. Cancer Res 69(2):573–82
Luistro L, He W, Smith M et al (2009) Preclinical profile of a potent gamma-secretase inhibitor targeting notch signaling with in vivo efficacy and pharmacodynamic properties. Cancer Res 69(19):7672–80
Tolcher AW, Messersmith WA, Mikulski SM et al (2012) Phase I study of RO4929097, a gamma secretase inhibitor of notch signaling, in patients with refractory metastatic or locally advanced solid tumors. J Clin Oncol 30(19):2348–2353
O’Shaughnessy JA, Blum J, Moiseyenko V et al (2001) Randomized, open-label, phase II trial of oral capecitabine (Xeloda) vs. a reference arm of intravenous CMF (cyclophosphamide, methotrexate and 5-flurouracil) as first-line therapy for advanced/metastatic breast cancer. Ann Oncol 12(9):1247–54
Twelves C, Scheithauer W, McKendrick J et al (2012) Capecitabine versus 5-fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results from the X-ACT trial with analysis by age and preliminary evidence of a pharmacodynamic marker of efficacy. Ann Oncol 23(5):1190–7
Van Cutsem E, Twelves C, Cassidy J et al (2001) Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: results of a large phase III study. J Clin Oncol 19(21):4097–106
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumors: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–47
Mulkerin D, LoConte NK, Holen KD et al (2009) A phase I study of an oral simulated FOLFOX with high dose capecitabine. Invest New Drugs 27(5):461–8
Olsauskas-Kuprys R, Zlobin A, Osipo C (2013) Gamma secreatase inhbitors of Notch signaling. Onco Targets Ther 6:943–955
Sahebjam S, Bedard PL, Castonguay V et al (2013) A phase I study of the combination of RO4929097 and cediranib in paitnets with advanced solid tumors. Br J Cancer 109:943–949
Acknowledgments
The investigators gratefully acknowledge the patients and families who participated in this study. Funding was provided by the National Cancer Institute Grant U01 CA062491 (University of Wisconsin) and U01-CA132123 (Princess Margaret Hospital). Further support is provided by the University of Wisconsin Carbone Cancer Center Core Grant P30 CA014520 and the Princess Margaret Hospital Phase I Consortium. Amye Tevaarwerk is supported by the National Institutes of Health Clinical and Translational Science Awards program 9U54TR000021.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
LoConte, N.K., Razak, A.R.A., Ivy, P. et al. A multicenter phase 1 study of γ -secretase inhibitor RO4929097 in combination with capecitabine in refractory solid tumors. Invest New Drugs 33, 169–176 (2015). https://doi.org/10.1007/s10637-014-0166-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-014-0166-6