Summary
Background This phase Ib study used a parallel, multi-arm design to examine tasisulam-sodium (hereafter tasisulam), a drug with complex pharmacology, combined with standard chemotherapies in patients with advanced solid tumors, with the ultimate goal of accelerating drug development. Methods Patients received escalating doses of tasisulam (3 + 3 schema; target Cmax 300–400 μg/mL) every 28 days plus 1,000 mg/m2 gemcitabine HCl (days 1 and 15), 60 mg/m2 docetaxel, 200 mg/m2/day temozolomide, 75 mg/m2 cisplatin, or 150 mg/day erlotinib. Following dose-escalation, patients were enrolled into specific tumor subtype arms, chosen based on the established activity of the standard agent. Because tasisulam is highly albumin-bound, patients in the tumor-specific confirmation arms were dosed targeting specific albumin-corrected exposure ranges (AUCalb) identified during dose-escalation (3,500 h*μg/mL [75th percentile] for docetaxel, temozolomide, and cisplatin; 4,000 h*μg/mL for gemcitabine and erlotinib). Results A total of 234 patients were enrolled. The safety profile of tasisulam with standard chemotherapies was sufficient to allow enrollment into the dose-confirmation phase in all arms. The primary dose-limiting toxicities were hematologic (thrombocytopenia and neutropenia). The most common grade ≥3 drug-related treatment-emergent adverse event was neutropenia, with the highest incidence in the docetaxel arm. Conclusions The multi-arm design allowed the efficient determination of the maximum tolerated dose of tasisulam across multiple combinations, and a preliminary characterization of pharmacokinetics, safety, and potential efficacy. Although enrollment into all planned groups was not completed due to termination of compound development, these data support the feasibility of this approach for accelerated cancer drug development, even for drugs with complex pharmacology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many agents, particularly cancer chemotherapies, are eventually used in combination with other agents. For this reason, in addition to traditional phase I monotherapy trials, the clinical development plan of an investigational agent sometimes includes combination (phase Ib) trials, which are usually run as individual trials. Although preclinical studies provide initial direction, identifying active combination regimens in humans can be a lengthy process, particularly for compounds with complex pharmacology or a novel mechanism of action. As proposed by Von Hoff [1] and others [2, 3], a more efficient approach is the “Complete Phase 1b Study,” which tests various drug combinations in one trial with multiple combination treatment arms running in parallel.
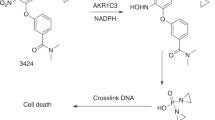
The study described in this report applied the “Complete Phase 1b Study” design to investigate tasisulam, a novel acylsulfonamide antineoplastic agent, in combination with standard of care chemotherapeutic agents in patients with advanced solid tumors. At the time this study was designed, tasisulam was being evaluated as a single agent in several tumor types [4–9]. However, preclinical studies suggested that it might have even greater activity at more modest doses in combination with other chemotherapeutic agents, an attractive strategy given the potential for greater pharmacokinetic (PK) and safety variability at higher doses due to high-affinity albumin binding. First, tasisulam demonstrated a unique anti-tumor dual mechanism of action, involving mitotic catastrophe and antiangiogenesis [10]. Second, in the National Cancer Institute Comparative Assay for Regulatory Elements (COMPARE) analysis, the activity profile of tasisulam could not be matched with any other cytotoxic compound with a known mechanism of action [11].
The design of the present study allowed for the parallel investigation of tasisulam in combination with five standard of care chemotherapies—gemcitabine HCl [12, 13], docetaxel [14, 15], temozolomide [16, 17], cisplatin [18, 19], and erlotinib [20]—selected on the basis of their toxicity profiles, potential mechanism of action-related synergy, and opportunity for future clinical development in specific tumor types. The rationale for studying tasisulam in combination was based on mouse xenograft studies that demonstrated greater activity when tasisulam was combined with dacarbazine, cisplatin, docetaxel, or gemcitabine than when it was administered alone (Eli Lilly and Company, data on file). In addition, tasisulam and erlotinib have been investigated in a panel of non-small cell lung cancer (NSCLC) cell lines with mutant or wild-type epidermal growth factor receptor (EGFR), in addition to Chinese Hamster Ovary cells transfected with mutant EGFR, with greatest activity noted when the 2 agents were given together (Eli Lilly and Company, data on file).
This study included a dose-escalation phase to determine the maximum tolerated dose of tasisulam when used in combination with gemcitabine, docetaxel, temozolomide, cisplatin, or erlotinib. Following successful dose-escalation, patients were enrolled into specific tumor subtype arms, chosen based on the established activity of the standard agent partner. Thus, this study added something new to the “Complete Phase 1b Study” design because it included a dose-confirmation phase. Ultimately, we aimed to determine the feasibility of this innovative “Complete Phase 1b Study” approach for simultaneously investigating several different drug combinations with tasisulam, especially given its complex pharmacology, and to ascertain whether our results supported the broader use of this study design for cancer drug development.
Methods
The primary objective of this non-randomized, open-label, phase Ib study (sponsored by Eli Lilly and Company, Indianapolis, IN, USA; Lilly Trial: H8K-MC-JZAK; ClinicalTrials.gov Identifier: NCT01284335) was to determine the recommended dose of tasisulam given concurrently with standard doses of gemcitabine HCl (arm A), docetaxel (arm B, later split into arms B1 and B2 in which docetaxel and tasisulam administration was separated by 3 days using alternate sequences [see the Results section]), temozolomide (arm C), cisplatin (arm D), or erlotinib (arm E) in patients with advanced solid tumors. Secondary objectives were to characterize the safety profiles of the five combinations, estimate tasisulam PK parameters, and document best overall response rates in specific tumor types. The study was conducted in accordance with ethical principles, including the Declaration of Helsinki, and was approved by local ethical review boards. The investigators enrolled patients onto one of the five treatment combinations guided by clinical factors, such as tumor type and prior therapies. Patient enrollment was stopped in November 2011. However, patients were allowed to continue active treatment if, in the opinion of the investigator, the patient was benefiting from treatment.
Eligibility criteria
Patients enrolled in the study were ≥18 years of age with histologically confirmed unresectable or metastatic solid malignancy or lymphoma for which monotherapy with gemcitabine HCl, docetaxel, temozolomide, cisplatin, or erlotinib was deemed appropriate by the investigator. Eligible patients also had tumor progression after receiving standard therapeutic agents or were appropriate for combination therapy because of limited treatment options. Additional eligibility criteria included evaluable disease per Response Evaluation Criteria in Solid Tumors (RECIST version 1.0) [21] or the International Working Group’s Criteria for Malignant Lymphoma [22]; Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0 or 1; normal hematologic, renal, and liver function; an estimated life expectancy of ≥12 weeks; serum albumin ≥3.0 g/dL; and signed informed consent. Patients did not receive chemotherapy, radiotherapy, immunotherapy, or other investigational therapy within 30 days before enrollment (6 weeks for mitomycin C or nitrosoureas) or any experimental agent for noncancer indications (or previous treatment with tasisulam). Because of the potential for drug interactions, patients receiving the following treatments were excluded: warfarin, amiodarone, quinidine, propofol, clozapine, or strong or moderate inhibitors of CYP2C19, including proton-pump inhibitors (esomeprazole and pantoprazole were allowed if not administered 72 h before or after tasisulam). Primary exclusion criteria included any other serious medical condition, active central nervous system or brain metastasis, current hematologic malignancy (other than lymphoma), hypersensitivity to any of the combination drugs, or positive tests for HIV, hepatitis B, or hepatitis C. Pregnant or lactating women were also excluded.
Treatment plan and dose-escalation schema
Tasisulam was administered as a 2-h IV infusion on day 1 (day 4 in treatment arm B1, see Results) of the treatment cycle concurrently with standard doses of gemcitabine HCl (30-min IV infusion of 1,000 mg/m2 on days 1 and 15; Eli Lilly and Company, Indianapolis, Indiana), docetaxel (60-min IV infusion of 60 mg/m2; Sanofi-Aventis, Bridgewater, New Jersey), temozolomide (200 mg/m2/day orally; Schering Corp., Kenilworth, New Jersey), cisplatin (60-min IV infusion of 75 mg/m2; Bristol-Myers Squibb, New York, New York), and erlotinib (150 mg/day orally; Genentech, South San Francisco, California) (Fig. 1).
Study flow diagram. Arm A, tasisulam administered on day 1 and gemcitabine HCl (GEM) administered on days 1 and 15 of a 28-day cycle (n = 58); Arm B, tasisulam administered on day 1 and docetaxel (DTX) administered on day 1 of a 21-day cycle; Arm B1, DTX administered on day 1 and tasisulam administered on day 4 of a 28-day cycle; Arm B2, tasisulam administered on day 1 and DTX administered on day 4 of a 28-day cycle (total Arms B, B1, and B2, n = 60); Arm C, tasisulam administered on day 1 and temozolomide (TMZ) administered on days 1–5 of a 28-day cycle (n = 25); Arm D, tasisulam administered on day 1 and cisplatin (CIS) administered on day 1 of a 21-day cycle, later modified to a 28-day cycle (n = 63); Arm E, tasisulam administered on day 1 and erlotinib (ERL) administered on days 1–28 of a 28-day cycle (n = 28). AUCalb, area under the curve above an albumin threshold; NSCLC, non-small cell lung cancer; SCLC, small cell lung cancer; STS, soft tissue sarcoma. a In the dose-confirmation phase, the goal was to treat a minimum of 10 patients in each treatment arm for each specific tumor type; b The regimen was amended because of hematologic toxicity noted at the lowest tasisulam dose level when tasisulam and docetaxel were administered together on day 1; c GEM-naïve; d DTX-naïve; e TMZ-naïve
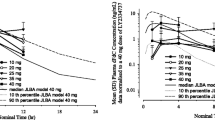
Tasisulam is highly bound to albumin (>99.7 %), with a relatively long half-life (median terminal half-life of 10 days) [6], consistent with the turnover of albumin (9–12 days) [23]. Analysis of early phase tasisulam studies suggested that the area under the curve (AUC) of total tasisulam above a certain threshold was positively correlated with toxicity [6, 24]. This certain threshold was related to patient’s pre-dose albumin levels, likely because drug toxicity is related to free tasisulam concentrations. Thus, AUC-above-the-albumin-corrected-threshold (AUCalb) (Fig. 2) was used as a surrogate of the AUC of free tasisulam concentration, which had not been possible to reliably measure in the clinical trial setting prior to initiation of this study.
In the dose-escalation phase, escalating doses of tasisulam, based on specific target maximum concentration (Cmax) values, were administered concurrently with fixed doses of each standard chemotherapeutic agent using a conventional 3 + 3 dose-escalation schema [25]. Tasisulam doses targeted Cmax values ranging from 300 to 400 μg/mL (300, 320, 340, 360, 380, and 400). This Cmax range was chosen on the basis of phase I clinical toxicity and PK data [4, 5, 11], as well as on safety data from completed and ongoing phase II single-agent clinical trials [6–8].
A dose-limiting toxicity (DLT) was defined as an adverse event (AE) that occurred during cycle 1 that was likely drug-related and met any of the following criteria: Common Terminology Criteria for Adverse Events (CTCAE) grade 4 neutropenia lasting more than 5 days; CTCAE grade 4 neutropenia with fever, regardless of duration; CTCAE grade 4 thrombocytopenia, regardless of duration; CTCAE grade ≥3 thrombocytopenia with bleeding, regardless of duration; or CTCAE grade ≥3 nonhematologic toxicity. In addition, the investigator, together with the sponsor’s medical personnel, could declare a DLT if a patient experienced increasing toxicity during treatment that posed excessive risk to the patient. The maximum tolerated dose (MTD) was the highest dose level with <33 % of patients having DLT in cycle 1. Thus, if none of the 3 treated patients experienced a DLT at a given dose level, dosing proceeded to the next higher dose level. If 1 of 3 patients experienced a DLT at any dose level during cycle 1, then the cohort was expanded to include up to 6 patients. If ≥2 patients experienced a DLT, the MTD was considered exceeded and dose escalation was stopped. Intrapatient dose escalations were not allowed.
Dose-confirmation phase
Once the MTD was exceeded for a particular combination treatment arm, PK, albumin levels, and safety from the escalation phase were analyzed to identify the albumin corrected exposure range (AUCalb) of tasisulam that would optimize safety and potential antitumor activity of the combination. The dose-confirmation phase for that combination was then opened, using the identified AUCalb of tasisulam. Each combination treatment arm was expanded to include a total of 20 to 30 patients per arm, enriched for specific tumor subtypes by enrolling at least 10 patients for each specific tumor subtype of interest (Fig. 1). Specific tumor types planned for the dose-confirmation phase were as follows: arm A (gemcitabine), gemcitabine-naïve metastatic pancreatic cancer and gemcitabine-naïve metastatic soft tissue sarcoma; arm B (docetaxel), docetaxel-naïve NSCLC and docetaxel-naïve metastatic breast cancer, prior docetaxel given in an adjuvant setting was allowed; arm C (temozolomide), temozolomide-naïve metastatic melanoma and temozolomide-naïve glioblastoma; arm D (cisplatin), metastatic NSCLC and small cell lung cancer (SCLC), previous cisplatin treatment was allowed; and arm E (erlotinib), metastatic NSCLC.
Safety and antitumor assessments
Physical examinations, performance status assessment, and tumor measurement of palpable or visual lesions were completed at baseline and at each cycle. Treatment-emergent adverse events (TEAEs), along with their toxicity ratings per CTCAE, version 3 [26], vital signs, and standard laboratory tests were collected at baseline, before each cycle, and post-therapy. Tumor response was determined by the investigator according to RECIST (version 1.0) guidelines [21], as measured by radiological imaging performed at baseline, prior to day 1 of cycle 3, and every other cycle thereafter.
Pharmacokinetic assessments
PK analyses were conducted on all patients who received at least 1 dose of study treatment and had plasma samples collected. Tasisulam concentrations were analyzed by a validated liquid chromatography/mass spectrometry/mass spectrometry (LC-MS/MS) method by Advion BioServices, Inc. (Ithaca, New York). Details of the calibration, interassay accuracy, and interassay precision of the LC-MS/MS method have been previously reported [9].
The tasisulam PK dataset was analyzed using first-order conditional estimation with interaction in NONMEM (version 7). The final tasisulam PK model was a 2-compartment model, with lean body weight as a covariate on the volume of the central compartment. AUCalb was computed using the log-linear trapezoidal rule and the individual predicted concentrations.
Statistical analysis
All patients who received at least 1 dose of combination therapy were evaluated for safety and antitumor activity. No hypothesis tests were conducted for this study; parameter estimates and summary statistics are reported.
Results
Patient characteristics
A total of 234 patients were enrolled by a clinical oncology network (US Oncology Group; 211 patients, 14 sites) and 5 other individual sites (23 patients) within the United States. The study was initiated in 2008 and closed for enrollment in November 2011. The majority (84 %) of patients were Caucasian, with a mean age of 62.2 ± 12.3 years (Table 1). Equal numbers of men and women were enrolled. The predominant histologic tumor type was NSCLC (26.5 %), with the majority (63.2 %) of patients having an ECOG PS of 1. Of the 4 patients with glioblastoma in arm C (temozolomide) who completed the confirmation phase, 3 patients had prior radiation therapy (unknown for 1 patient).
At the time of this report, 2 patients remain on active treatment. One of these patients is an 87-year-old woman with SCLC and liver metastases in the cisplatin arm (arm D) who has been on treatment since 30 March 2011 (3 years) and who has maintained stable disease (SD). She has been on single-agent tasisulam since cycle 10 (currently on cycle 37) due to discontinuation of cisplatin because of neurotoxicity. The other patient is a 64-year-old woman with breast cancer, liver metastases, and paraaortic adenopathy in the docetaxel arm (arm B2) who has been on treatment since 28 October 2011 (30 months) and who achieved partial response (PR). She has been on single-agent tasisulam since cycle 11 (currently on cycle 29) due to discontinuation of docetaxel because of grade 3 thrombocytopenia.
Dosing
Treatments were given as described in the methods section for arms A (gemcitabine), C (temozolomide), and E (erlotinib) (Fig. 1). As initially planned, in arm B docetaxel was given on day 1 of a 21-day cycle, followed by tasisulam on the same day. However, hematologic toxicity (neutropenia) was observed in 3 patients at the lowest dose of tasisulam (Cmax 300 μg/mL) in combination with docetaxel (Table 2). Therefore, the regimen was amended for subsequent dose levels as follows: arm B1, docetaxel was given on day 1 and tasisulam on day 4; and arm B2, tasisulam was given on day 1 and docetaxel on day 4 (Fig. 1). Cycle length was extended to 28 days for both arms. Enrollment to arm B1 was later closed due to treatment-related hematologic toxicities (Table 2). In arm D (cisplatin), all 3 patients in the Cmax 300 μg/mL group and 1 patient in the 320 μg/mL group were on a 21-day cycle; the remainder were on a 28-day cycle.
On the basis of a safety (Table 2) and PK analysis of the dose-escalation phase data, the tasisulam dosing algorithm for the dose-confirmation phase was designed such that 75 % of the population would have an AUCalb of less than either 3,500 or 4,000 h*μg/mL. The tasisulam AUCalb target ranges identified for each combination are shown in Table 3. Despite the complexity of tasisulam dosing, the dosing approach accurately achieved the specified target in the dose-confirmation arm. An AUCalb target range of 3,500 h*μg/mL (75th percentile) was selected for arms B2 (docetaxel), C (temozolomide), and D (cisplatin); 63 % of patients in cycle 1 and 74 % in cycle 2 had an AUCalb of less than 3,500 h*μg/mL (Fig. 3). An AUCalb target range of 4,000 h*μg/mL was selected for arms A (gemcitabine) and E (erlotinib); 68 % of patients in cycle 1 and 81 % in cycle 2 had an AUCalb of less than 4,000 h*μg/mL (Fig. 3). For arm E (erlotinib), the AUCalb target was later decreased to AUCalb 3,500 h*μg/mL after 13 patients were enrolled and 1 patient developed grade 1 gastrointestinal hemorrhage and grade 4 thrombocytopenia, although the case was confounded by concomitant clopidogrel use. The dose-escalation phase was completed for arm C (temozolomide), but the dose-confirmation phase was closed early because of limited enrollment (6 patients entered the dose-confirmation phase), early signs of insufficient benefit versus risk, and for strategic reasons.
Overall safety
Of the 234 patients who received at least 1 dose of combination treatment and were evaluable for safety, 29 discontinued because of a possibly study drug-related TEAE; 13 during the dose-escalation phase and 16 during the dose-confirmation phase (Table 4). Seven deaths occurred during the study or within 30 days of discontinuation in the setting of a possibly study drug-related TEAE (neutropenic sepsis, sepsis, and gastrointestinal hemorrhage); 2 during the dose-escalation phase (1 each in arm B [docetaxel] and arm C [temozolomide]) and 5 during the dose-confirmation phase (2 in arm C [temozolomide] and 1 each in arms B [docetaxel], D [cisplatin], and E [erlotinib]).
For both study phases and across all treatment cycles, the most common TEAE that was possibly study drug-related and had a severity of grade ≥3 was neutropenia (40.6 %; 95/234 patients) (Table 5), with the highest incidence (70 %; 42/60 patients) observed in arm B (docetaxel). Over half of the patients in arm C (temozolomide) experienced thrombocytopenia. Overall, the most common nonhematologic AE was hypophosphatemia, with the highest incidence (15 %; 9/60 patients) observed in arm B (docetaxel). In addition to the most common TEAEs, 2 patients in arm C (temozolomide) reported possibly study drug-related grade ≥3 sepsis.
Dose-confirmation phase antitumor activity
The treatment arms that attained a minimum of 10 patients for a specific tumor type were arm A (gemcitabine) for gemcitabine-naïve metastatic pancreatic cancer (n = 15), arm B2 (docetaxel) for docetaxel-naïve NSCLC (n = 10), and arm D (cisplatin) for NSCLC (n = 20) and SCLC (n = 14). Best overall response for these patients is shown in Table 6. The clinical benefit rate was 50 % or over for each of these groups.
Accrual and cost analysis
Over 40 months, 234 patients were enrolled. The time from protocol approval to first patient visit for this multi-arm, phase Ib study was 109 days, which was similar to the mean of 98 days for all phase I oncology clinical trials conducted by the sponsor (Eli Lilly and Company, data on file).
A cost analysis was conducted to examine whether a 5-arm, phase 1b clinical trial, such as the current study, might be more cost effective than 5 comparable single-arm trials. Assumptions for the 5-arm study were as follows: 5 dose levels, with 5 patients at each dose level in the dose-escalation phase (25 patients per arm) and 25 patients per arm in the dose-confirmation phase (total of 250 patients), all patients completing 6 cycles, and 10 sites participating. Assumptions for the single-arm studies were as follows: 5 dose levels, with 5 patients at each dose level in the dose-escalation phase and 25 patients in the dose-confirmation phase (total of 50 patients in each study), all patients completing 6 cycles, 4 sites participating per study (typical for a single-arm study). Given these assumptions and typical grant spend related to start-up fees, investigator budget, laboratory and diagnostic testing, and monitoring, it is estimated that cost savings for a single 5-arm study over 5 single-arm individual studies would amount to approximately 20 %.
Discussion
The multi-arm, phase 1b design of this study allowed a broad, preliminary characterization of the safety and antitumor activity of tasisulam across multiple combinations of standard therapeutic agents in specific tumor subtypes. The design of this study was based on the “Complete Phase 1b Study” outlined by Von Hoff [1]. This approach offers several potential advantages over the traditional multiple phase Ib study approach, including: (1) several different treatment arms the investigator can choose from, informed by individual patient treatment history and tumor subtype; (2) multiple parallel paths for MTD determination and preliminary efficacy and safety read-outs in specific tumor subtypes; (3) greater operational efficiency and cost savings; (4) greater shared learning about the safety and PK profile of an investigational agent within a broader investigative clinical setting; and (5) the ability to close or prioritize a combination arm for strategic purposes.
There are several resource and operational aspects of this type of trial that are worthy of further discussion. First, although enrollment comparisons across different investigative agents can be highly confounded, the enrollment rate of the current multi-arm study of 0.25 patients/site/month was similar to historical data from 5 individual advanced solid tumor phase I oncology trials run in sequence showing an enrollment rate of approximately 0.5 patients/site/month (Eli Lilly and Company, data on file). The lower enrollment metrics of the current study were likely due to factors related to the complex pharmacology and dosing of tasisulam rather than to operational trial design differences. This possibility is supported by data showing that our study enrolled 234 patients to 5 arms in 40 months, similar to the time course of three other individual tasisulam phase Ib combination studies (approximately 28 to 43 months; Eli Lilly and Company, data on file). Importantly, the similar enrollment rate of this study compared to individual tasisulam phase Ib studies was accomplished with only one start-up date and consolidated investigator and staff training. Second, our cost analysis estimated potential cost savings of approximately 20 % by conducting a single multiple-arm trial rather than 5 individual single-arm trials. The primary drivers for cost savings are fewer start-up/training fees and lower monitoring costs. A single multiple-arm study also offers an advantage of greater consistency and efficiency because the protocol is carried out by the same sites instead of multiple sites for each study, features that are particularly important for early phase studies. Finally, the fact that most patients (211 of 234) were from a clinical network with centralized data management and administrative services (e.g., investigational review board and pharmacy) suggests that this design might be most efficient in the centralized clinical trial setting rather the individual study site setting.
Compared to the earlier “Complete Phase 1b Study” design [1], our study has further extended the patient population suitable for this type of approach. Patients in the dose-escalation phase of our study were extensively pretreated and therefore more typical of a traditional oncology phase I study compared to the mostly standard of care drug-naïve population enrolled in the earlier study. The dose-confirmation phase of our study was a hybrid of the earlier design, with some tumor-specific sub-arms being standard of care drug-naïve (gemcitabine, docetaxel, and temozolomide) and others not being standard of care drug-naïve (cisplatin and erlotinib). Additionally, our trial design differed from the recent phase Ib study of cediranib [27] in that our study allowed the investigator to choose the appropriate treatment arm on the basis of tumor subtype and prior therapy. To the best of our knowledge, our study is the largest phase Ib study to date that has used this multi-arm design.
Lastly, the present trial provided some preliminary evidence of antitumor activity for several of the tasisulam combinations. In the gemcitabine-naïve pancreatic cancer cohort (n = 15), a median of 4 cycles of tasisulam and gemcitabine was given (range 1–20), with 2 patients achieving PR and 6 maintaining SD (Table 6), and a median progression-free survival of approximately 3.3 months (95 % CI: 1.6 to 8.5; data not shown). In contrast, in previous studies, single-agent gemcitabine for metastatic pancreatic cancer had a median time to tumor progression of 2.1 months (95 % confidence interval 1.9–3.4 months) [28]. The findings associated with the cisplatin combination in metastatic SCLC in this study were also of interest, considering that this cohort consisted of heavily pretreated patients with a median of 2 prior treatment regimens (range 1–6; 93 % of patients received previous cisplatin or carboplatin). Patients received a median of 3 cycles (range 1–21), with 1 patient achieving PR and 7 maintaining SD. The AE profile of the cisplatin combination (possibly study drug-related grade ≥3 neutropenia and thrombocytopenia of 36.5 % and 31.7 %, respectively) and the clinical benefit rate seen in SCLC patients in this sub-arm were similar to findings from single-agent topotecan as second-line treatment in relapsed SCLC [29]. The NSCLC cohort of the cisplatin combination (n = 20) also consisted of a heavily pretreated population, with a median of 3.5 prior regimens (range 1–7; 75 % of patients received previous cisplatin or carboplatin). A median of 2 cycles (range 1–10) was given, with 1 patient achieving PR and 9 maintaining SD. The patients on the tasisulam-docetaxel NSCLC arm (n = 10) had received a median of 2.5 prior treatment regimens (range 1–4) and a median of 5.5 cycles (range 1–13), with 2 patients achieving PR and 5 maintaining SD. This combination, however, was significantly more myelosuppressive, with approximately 70 % of these patients experiencing possibly study drug-related grade ≥3 neutropenia.
In conclusion, the multi-arm, phase Ib design of this study allowed a reasonable preliminary characterization of the safety and anti-tumor activity of tasisulam across multiple combinations of standard therapeutic agents in specific tumor subtypes. Although enrollment into all planned tumor-subtype groups was not completed due to termination of compound development, sufficient numbers of patients were enrolled in the confirmation phase of three tumor/therapy-specific combinations (gemcitabine for metastatic pancreatic cancer, docetaxel for NSCLC, and cisplatin for NSCLC and SCLC). The enrollment and operational efficiency of this study over multiple phase Ib studies was particularly noteworthy given the additional challenge of one of the combination arms (docetaxel) requiring further breakdown into separate inverted drug sequence arms and the complex pharmacology and novel mechanism of action of tasisulam. Overall, the results of this study indicate that this “Complete Phase 1b Study” design was an efficient way to gather data on a complex molecule, such as tasisulam, and support the broader use of this design for early cancer drug development.
References
Von Hoff DD, Nieves JA, Vocila LK, Weitman SD, Cvitkovic E (2007) The complete phase Ib clinical trial: a method to accelerate new agent development. J Clin Oncol 25(18S):2562
LoRusso PM, Boerner SA, Seymour L (2010) An overview of the optimal planning, design, and conduct of phase I studies of new therapeutics. Clin Cancer Res 16(6):1710–1718. doi:10.1158/1078-0432.CCR-09-1993
George S, Desai J, Paul Eder J, Manola J, Ryan DP, Appleman LJ, Demetri GD (2006) Selective kinase inhibition with daily imatinib intensifies toxicity of chemotherapy in patients with solid tumours. Eur J Cancer 42(7):864–870. doi:10.1016/j.ejca.2005.12.010
Fujiwara Y, Ando Y, Mukohara T, Kiyota N, Chayahara N, Mitsuma A, Inada-Inoue M, Sawaki M, Ilaria R Jr, Kellie Turner P, Funai J, Maeda K, Minami H (2013) A phase I study of tasisulam sodium using an albumin-tailored dose in Japanese patients with advanced solid tumors. Cancer Chemother Pharmacol. doi:10.1007/s00280-013-2092-2
Gordon MS, Ilaria R Jr, de Alwis DP, Mendelson DS, McKane S, Wagner MM, Look KY, Lorusso PM (2013) A phase I study of tasisulam sodium (LY573636 sodium), a novel anticancer compound, administered as a 24-h continuous infusion in patients with advanced solid tumors. Cancer Chemother Pharmacol 71(1):21–27. doi:10.1007/s00280-012-1917-8
Kirkwood JM, Gonzalez R, Reintgen D, Clingan PR, McWilliams RR, de Alwis DP, Zimmermann A, Brown MP, Ilaria RL Jr, Millward MJ (2011) A phase 2 study of tasisulam sodium (LY573636 sodium) as second-line treatment for patients with unresectable or metastatic melanoma. Cancer 117:4732–4739. doi:10.1002/cncr.26068
Ryan CW, Matias C, Agulnik M, Lopez-Pousa A, Williams C, de Alwis DP, Kaiser C, Miller MA, Ermisch S, Ilaria R Jr, Keohan ML (2013) A phase II study of tasisulam sodium (LY573636 sodium) as second-line or third-line treatment for patients with unresectable or metastatic soft tissue sarcoma. Investig New Drugs 31(1):145–151. doi:10.1007/s10637-012-9819-5
Scagliotti GV, Ilaria R Jr, Novello S, von Pawel J, Fischer JR, Ermisch S, de Alwis DP, Andrews J, Reck M, Crino L, Eschbach C, Manegold C (2012) Tasisulam sodium (LY573636 sodium) as third-line treatment in patients with unresectable, metastatic non-small-cell lung cancer: a phase-II study. J Thorac Oncol 7(6):1053–1057. doi:10.1097/JTO.0b013e3182519d79
Simon GR, Ilaria RL Jr, Sovak MA, Williams CC, Haura EB, Cleverly AL, Sykes AK, Wagner MM, de Alwis DP, Slapak CA, Miller MA, Spriggs DR (2011) A phase I study of tasisulam sodium (LY573636 sodium), a novel anticancer compound in patients with refractory solid tumors. Cancer Chemother Pharmacol 68(5):1233–1241. doi:10.1007/s00280-011-1593-0
Meier T, Uhlik M, Chintharlapalli S, Dowless M, Van Horn R, Stewart J, Blosser W, Cook J, Young D, Ye X, Evans G, Credille K, Ballard D, Huber L, Capen A, Chedid M, Ilaria R Jr, Smith MC, Stancato L (2011) Tasisulam sodium, an antitumor agent that inhibits mitotic progression and induces vascular normalization. Mol Cancer Ther 10(11):2168–2178. doi:10.1158/1535-7163.MCT-11-0323
Paull KD, Shoemaker RH, Hodes L, Monks A, Scudiero DA, Rubinstein L, Plowman J, Boyd MR (1989) Display and analysis of patterns of differential activity of drugs against human tumor cell lines: development of mean graph and COMPARE algorithm. J Natl Cancer Inst 81:1088–1092
Burris HA 3rd, Moore MJ, Andersen J, Green MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM, Tarassoff P, Nelson R, Dorr FA, Stephens CD, Von Hoff DD (1997) Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J Clin Oncol 15(6):2403–2413
Hartmann JT, Oechsle K, Huober J, Jakob A, Azemar M, Horger M, Kanz L, Bokemeyer C (2006) An open label, non-comparative phase II study of gemcitabine as salvage treatment for patients with pretreated adult type soft tissue sarcoma. Investig New Drugs 24(3):249–253. doi:10.1007/s10637-005-3537-1
Burris HA 3rd (1999) Single-agent docetaxel (Taxotere) in randomized phase III trials. Semin Oncol 26(3 Suppl 9):1–6
Shepherd FA, Dancey J, Ramlau R, Mattson K, Gralla R, O’Rourke M, Levitan N, Gressot L, Vincent M, Burkes R, Coughlin S, Kim Y, Berille J (2000) Prospective randomized trial of docetaxel versus best supportive care in patients with non-small-cell lung cancer previously treated with platinum-based chemotherapy. J Clin Oncol 18(10):2095–2103
Patel PM, Suciu S, Mortier L, Kruit WH, Robert C, Schadendorf D, Trefzer U, Punt CJ, Dummer R, Davidson N, Becker J, Conry R, Thompson JA, Hwu WJ, Engelen K, Agarwala SS, Keilholz U, Eggermont AM, Spatz A (2011) Extended schedule, escalated dose temozolomide versus dacarbazine in stage IV melanoma: final results of a randomised phase III study (EORTC 18032). Eur J Cancer 47(10):1476–1483. doi:10.1016/j.ejca.2011.04.030
Yung WK, Prados MD, Yaya-Tur R, Rosenfeld SS, Brada M, Friedman HS, Albright R, Olson J, Chang SM, O’Neill AM, Friedman AH, Bruner J, Yue N, Dugan M, Zaknoen S, Levin VA (1999) Multicenter phase II trial of temozolomide in patients with anaplastic astrocytoma or anaplastic oligoastrocytoma at first relapse. Temodal Brain Tumor Group. J Clin Oncol 17(9):2762–2771
Evans WK, Shepherd FA, Feld R, Osoba D, Dang P, Deboer G (1985) VP-16 and cisplatin as first-line therapy for small-cell lung cancer. J Clin Oncol 3(11):1471–1477
Sandler AB, Nemunaitis J, Denham C, von Pawel J, Cormier Y, Gatzemeier U, Mattson K, Manegold C, Palmer MC, Gregor A, Nguyen B, Niyikiza C, Einhorn LH (2000) Phase III trial of gemcitabine plus cisplatin versus cisplatin alone in patients with locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol 18(1):122–130
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S, Smylie M, Martins R, van Kooten M, Dediu M, Findlay B, Tu D, Johnston D, Bezjak A, Clark G, Santabarbara P, Seymour L (2005) Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 353(2):123–132. doi:10.1056/NEJMoa050753
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Cheson BD (2007) The international harmonization project for response criteria in lymphoma clinical trials. Hematol Oncol Clin North Am 21(5):841–854. doi:10.1016/j.hoc.2007.06.011
Sterling K (1951) The turnover rate of serum albumin in man as measured by I131-tagged albumin. J Clin Invest 30:1228–1237
de Alwis D, Cleverly A, Chow K, Troconiz I, Ilaria R (2010) Tailored dosing of tasisulam sodium (LY573636 sodium) to reduce hematological toxicity and improve therapeutic index. EJC Suppl 8(7):92–93
Ratain MJ, Mick R, Schilsky RL, Siegler M (1993) Statistical and ethical issues in the design and conduct of phase I and II clinical trials of new anticancer agents. J Natl Cancer Inst 85(20):1637–1643
Cancer Therapy Evaluation Program, Common Terminology Criteria for Adverse Events. (2006) National Cancer Institute. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. Accessed 7 Apr 2014
Lorusso P, Shields AF, Gadgeel S, Vaishampayan U, Guthrie T, Puchalski T, Xu J, Liu Q (2011) Cediranib in combination with various anticancer regimens: results of a phase I multi-cohort study. Investig New Drugs 29(6):1395–1405. doi:10.1007/s10637-010-9484-5
Gemzar [package insert] (2013). Eli Lilly and Company, Indianapolis, Indiana
von Pawel J, Schiller JH, Shepherd FA, Fields SZ, Kleisbauer JP, Chrysson NG, Stewart DJ, Clark PI, Palmer MC, Depierre A, Carmichael J, Krebs JB, Ross G, Lane SR, Gralla R (1999) Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol 17(2):658–667
Acknowledgments
The authors wish to thank the Study JZAK investigators for their participation in the study: Drs Stephen Anthony, Thaddeus Beck, Thomas Boyd, Gabriela Chiorean, Maria Flores, Beth Hellerstedt, Pam Kaiser, Robert Raju, Rachel Sanborn, and Hillary Wu. We also thank Cindy C. Taylor of ClinGenuity LLC for assistance with the preparation of the manuscript, Dinesh P. De Alwis formerly of Eli Lilly and Company for assistance with the pharmacokinetics analyses, and Baha Alkuzweny of Inventiv for statistical analyses. We are grateful to the patients who participated in this trial.
This study was funded by Eli Lilly and Company.
Drs Chen, Turner, Chow, Tai, and Ilaria Jr. are employees and minor stockholders of Eli Lilly and Company. Drs Smith and Jotte were on the speaker’s bureau for Eli Lilly and Company when the current study was conducted. Dr Von Hoff has received institutional funding for ongoing clinical trials on hedgehog pathway inhibitor Eli Lilly and Company. The other authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jotte, R.M., Von Hoff, D.D., Braiteh, F. et al. An innovative, multi-arm, complete phase 1b study of the novel anti-cancer agent tasisulam in patients with advanced solid tumors. Invest New Drugs 33, 148–158 (2015). https://doi.org/10.1007/s10637-014-0160-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-014-0160-z