Summary
Vascular endothelial growth factor (VEGF) overexpression and increased angiogenesis have been proposed as having biologic importance in germ cell tumors (GCT). We conducted a single-institution phase II trial of sunitinib, an oral inhibitor of the VEGF receptor, in patients with relapsed or refractory GCT. A Simon’s two-stage design was used to determine the number of patients for enrollment. Responses were assessed using a modified version of Response Evaluation Criteria in Solid Tumors (RECIST), taking into account tumor marker changes. Dose modifications were made according to a nomogram for adverse events. Ten patients were enrolled. The first five received sunitinib 50 mg for four consecutive weeks, followed by a two-week break (4/2). Since four of five treated on this schedule had some tumor marker decline during the four-week “on” period, with subsequent rise during the two-week break, the dose was changed to 37.5 mg continuously for patients six to ten. However, only marker stabilization (no declines) was seen. Overall, there were no objective responses: Five had stable disease and five progressive disease (PD). Sunitinib was well tolerated; only one patient required a dose reduction due to grade 3 mucositis. Two patients experienced tumor-related hemorrhage (grade 3 and grade 1). All patients developed PD within three cycles. Sunitinib is well tolerated, but at standard doses, does not demonstrate significant activity in highly refractory GCT. Correlation between sunitinib treatment and tumor marker changes on the 50 mg 4/2 schedule suggest some pathways targeted by sunitinib (ie, angiogenesis) may be important to GCT biology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While the overall prognosis for patients with advanced germ cell tumors (GCT) is excellent, up to 30% with disseminated disease fail to achieve a durable complete response (CR) following initial treatment with cisplatin plus etoposide with or without bleomycin chemotherapy (EP, BEP) [1]. Second-line treatment options include cisplatin plus ifosfamide in combination with vinblastine or paclitaxel (VeIP, TIP), or high-dose therapy with stem-cell support [1]. However, a subset of patients will also be refractory to or ineligible for these salvage treatments [1]. Certain patient groups such as those with mediastinal nonseminomatous GCT or primary refractory GCT may be especially difficult to cure with these salvage approaches [1, 2]. Therefore, a goal of phase I and phase II clinical trials is to identify new active agents for patients with GCT who are resistant to conventional therapies.
Angiogenesis is considered to be a key factor in tumor growth and progression for a variety of malignancies, often by increased activation of the vascular endothelial growth factor (VEGF) pathway. Antineoplastic drugs designed to target the VEGF pathway have risen out of this recognition, and in some cancers (ie, renal cell carcinoma), they have become the new standard of care [3]. As with other neoplasms, recent evidence has also suggested a role for angiogenesis in the pathobiology of GCT. Viglietto et al observed that as compared with the normal testis, testicular neoplasms have greater expression of VEGF and VEGFR expression and higher microvessel density [4]. Subsequently, Fukuda et al demonstrated that increased angiogenesis and VEGF expression within orchiectomy specimens of GCT patients predicted for the presence of metastatic disease [5].
Sunitinib is an oral inhibitor of multiple receptor tyrosine kinases including VEGFR, and has been demonstrated in preclinical models to impair angiogenesis [6]. It has been approved in the United States for use in patients with renal cell carcinoma (RCC) and gastrointestinal stromal tumour (GIST), and is currently being studied in a variety of other malignancies. We sought to evaluate the efficacy of sunitinib in patients with GCT resistant to standard platinum-based treatment options.
Patients and methods
Patient eligibility
Eligibility criteria included GCT histology; evidence of measurable metastatic disease and/or elevation of tumor markers (alpha-fetoprotein [AFP] >15 ng/mL and/or elevation of β-human chorionic gonadotropin [β-HCG] >2.2 mIU/L); age ≥18 years; Karnofsky performance status ≥70%; absolute neutrophil count (ANC) ≥1500 cells/mm3; platelet count ≥100,000/mm3; hemoglobin ≥10 g/dl; bilirubin ≤1.5 times the upper limit of normal; serum glutamic oxaloacetic transaminase ≤2.0 times the upper limit of normal; and creatinine ≤2.2. All patients were either clinically refractory to standard platinum-based salvage therapy with progression or relapsed after high-dose chemotherapy with autologous stem cell rescue, or they had declined or were not candidates for high-dose therapy. All patients gave informed consent, and the trial was reviewed and approved by the Institutional Review Board at Memorial Sloan-Kettering Cancer Center.
Treatment
Based on the experience in other malignancies, the initial dosing schedule of sunitinib was selected to be 50 mg, administered daily for four consecutive weeks followed by a two-week break (4/2 schedule), constituting one six-week cycle. Sunitinib dosing was changed to 37.5 mg continuously after patients on the 50 mg 4/2 schedule were observed to have tumor marker declines during the four-week “on” period, with subsequent rise during the two-week break. This schedule had previously been reported in patients taking sunitinib for RCC as well as GIST [7, 8]. Sunitinib was provided by Pfizer Inc. (New York, NY), the sponsor of this single-institution, investigator-initiated phase II trial.
Toxicity and response criteria
All toxicities were evaluated based on the National Cancer Institute Common Toxicity Criteria for Adverse Events (CTCAE, v 3.0). The starting dose level (dose level 0) for the first five patients was 50 mg administered on a four-weeks-on and 2-weeks-off schedule (50 mg; 4/2), whereas the starting dose level 0 for patients six to ten was 37.5 mg administered continuously. Additional dose levels are illustrated in Table 1. Grade 4 neutropenia, grade ≥3 thrombocytopenia, grade ≥3 fatigue, or grade 4 hand-foot skin reaction resulted in a dose reduction of one level. In addition, patients were instructed to withhold sunitinib for grade 3 hand-foot skin reaction and any other nonhematologic grade 3 or 4 toxicity until the toxicity had reached grade ≤1, with reinstitution at either the same dose level or a one dose level reduction at the discretion of the investigator. No dose escalation was allowed for patients treated on the 50 mg, 4/2 schedule, whereas the dose for patients on the 37.5 mg continuous schedule could be increased to 50 mg (dose level +1) after cycle two if they did not experience any grade 3 or 4 toxicities.
Interim assessment of tumor status was performed by radiographic imaging at baseline and then every six weeks. Responses were evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST). In addition, patients had serum tumor marker levels and complete blood counts drawn at baseline, day 14, and day 28 of the first cycle; and on day 0 and 28 of subsequent cycles. Treatment was continued until disease progression (≥20% increase in tumor size or rising serum tumor markers), unacceptable toxicity, or patient withdrawal of consent.
Statistical stipulation
The sample size and stopping rules were determined according to a Simon two-stage design in which a response rate of ≥20% was considered promising, and a response rate of ≤5% was considered unacceptable [9]. With a Type I error of 5% and a Type II error of 20%, ten patients would initially be enrolled, with enrollment expanded to 29 patients if at least one patient responded.
Results
Patient characteristics are shown in Table 2. The majority had unfavorable characteristics; all patients had received at least two lines of prior therapy (median 3, range 2–7), and 80% had undergone prior high-dose chemotherapy. All patients had received prior ifosfamide and paclitaxel. Four patients had late relapses and three had mediastinal primary tumors.
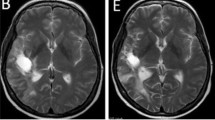
Seventeen cycles of sunitinib were administered to ten patients. The best response was stable disease (SD) in five patients and progressive disease (PD) in five patients. Based on RECIST, no objective responses were observed, and all patients developed progressive disease within three cycles of sunitinib. The first five patients were treated on the 50 mg 4/2 dosing schedule. Four of these patients experienced some tumor marker decline (without radiographic progression) during the four-week “on” period, with subsequent marker rise during the two-week break (Fig. 1a). These four patients had SD as their best response, while the remaining patient experienced PD. The observed marker changes prompted alteration in the dosing schedule of sunitinib to 37.5 mg continuously for patients six to ten in an attempt to prevent tumor progression from occurring during the two-week break. However, this did not result in any meaningful difference in response, with only one patient achieving marker stabilization (Fig. 1b) and no marker declines noted. The patient with marker stabilization achieved an overall best response of SD, while the other four patients treated on this schedule experienced PD with only one cycle of treatment.
Changes in serum tumor markers (AFP, HCG, or LDH) during treatment with sunitinib for a Patients treated on the 50 mg 4/2 schedule. Sunitinib treatment was administered from day 1–28 and held from day 29–42; and b Patients treated on the 37.5 mg continuous schedule in which there were no breaks in treatment until patients were withdrawn from the study. For patients with >1 elevated marker, the most specific (AFP/HCG > LDH) and most highly elevated marker at baseline was chosen. Abbreviations: C, cycle; D; day
In general, sunitinib was well tolerated; only one patient (on the 50 mg, 4/2 schedule) required a dose reduction (to 37.5 mg) for grade 3 mucositis, and there were no grade 4 toxicities. Other notable toxicities included grade 3 lymphopenia in six, grade 3 neutropenia in two, and grade 3 hemorrhage into a progressive splenic metastasis in one. Two other patients experienced bleeding, one experienced grade 2 epistaxis, and the other experienced grade 1 hemorrhage into a progressive liver metastasis. The most commonly occurring toxicities are listed in Table 3. Since all of the patients treated on the 37.5 mg continuous schedule developed PD prior to cycle three, there were no dose escalations on this trial.
Discussion
This phase II study is the first trial to evaluate a targeted antiangiogenesis agent specifically in patients with GCT. Although sunitinib demonstrated good tolerability, no significant clinical activity was observed at standard doses in patients with multiply relapsed or refractory GCT. The most serious toxicities were grade 3 mucositis, resulting in the single dose reduction required, and grade 3 hemorrhage within a progressive splenic metastasis. Both of these adverse effects have been previously observed during studies of sunitinib in other malignancies [10, 11].
Although activity was insufficient to induce objective responses, the mild declines in tumor markers observed during the four-week “on” period and re-elevation during the two-week break suggest that pathways inhibited by sunitinib such as VEGF may still be important to GCT biology. An alternate explanation would be that an off-target effect of sunitinib is to impair pathways involved in either marker production or secretion by tumor, thereby leading to a decline in serum tumor marker values without affecting tumor growth. Inhibition of a marker production pathway independent of anti-tumor effect is felt to be unlikely however, since both HCG and AFP were noted to decline with sunitinib.
Nevertheless, based on the correlation between sunitinib treatment and tumor marker changes, we elected to alter the dosing schedule midway through the trial. We chose to dose sunitinib at 37.5 mg continuously, since it had previously demonstrated efficacy in both RCC [8] and GIST [7], and we hoped to eliminate tumor progression during the two-week break period. However, this change did not improve outcomes, and overall, none of the ten patients achieved an objective response. Based on the results of this trial, we could not identify a rationale for continued study of sunitinib in patients with progressive GCT. No further trials of sunitinib in GCT are planned. Whether other more potent inhibitors of VEGFR such as axitinib could have activity in GCT, remains to be seen.
References
Kondagunta GV, Motzer RJ (2006) Chemotherapy for advanced germ cell tumors. J Clin Oncol 24:5493–5502
Beyer J, Kramar A, Mandanas R, Linkesch W, Greinix A, Droz JP, Pico JL, Diehl A, Bokemeyer C, Schmoll HJ, Nichols CR, Einhorn LH, Siegert W (1996) High-dose chemotherapy as salvage treatment in germ cell tumors: a multivariate analysis of prognostic variables. J Clin Oncol 14:2638–2645
Feldman DR, Motzer RJ (2006) Novel targets and therapies for metastatic renal cell carcinoma. Oncology 20:1745–1753. Williston Park, N.Y, discussion 1756
Viglietto G, Romano A, Maglione D, Rambaldi M, Paoletti I, Lago CT, Califano D, Monaco C, Mineo A, Santelli G, Manzo G, Botti G, Chiappetta G, Persico MG (1996) Neovascularization in human germ cell tumors correlates with a marked increase in the expression of the vascular endothelial growth factor but not the placenta-derived growth factor. Oncogene 13:577–587
Fukuda S, Shirahama T, Imazono Y, Tsushima T, Ohmori H, Kayajima T, Take S, Nishiyama K, Yonezawa S, Akiba S, Akiyama S, Ohi Y (1999) Expression of vascular endothelial growth factor in patients with testicular germ cell tumors as an indicator of metastatic disease. Cancer 85:1323–1330
Mendel DB, Laird AD, Xin X, Louie SG, Christensen JG, Li G, Schreck RE, Abrams TJ, Ngai TJ, Lee LB, Murray LJ, Carver J, Chan E, Moss KG, Haznedar JO, Sukbuntherng J, Blake RA, Sun L, Tang C, Miller T, Shirazian S, McMahon G, Cherrington JM (2003) In vivo antitumor activity of SU11248, a novel tyrosine kinase inhibitor targeting vascular endothelial growth factor and platelet-derived growth factor receptors: determination of a pharmacokinetic/pharmacodynamic relationship. Clin Cancer Res 9:327–337
George S, Blay JY, Casali PG, Le Cesne A, Stephenson P, Deprimo SE, Harmon CS, Law CN, Morgan JA, Ray-Coquard I, Tassell V, Cohen DP, Demetri GD (2009) Clinical evaluation of continuous daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib failure. Eur J Cancer. doi:10.1016/j.ejca.2009.02.011
Srinivas S, Roigas J, Gillessen S, Harmenberg U, De Mulder PH, Fountzilas G, Vogelzang N, Peschel C, Flodgren P, Escudier B (2007) Continuous daily administration of sunitinib in patients (pts) with cytokine-refractory metastatic renal cell carcinoma (mRCC): Updated results. Journal of Clinical Oncology, ASCO Annual Meeing Proceedings Part I 25:Abstract 5040
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, Baum CM, Figlin RA (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356:115–124
Socinski MA, Novello S, Brahmer JR, Rosell R, Sanchez JM, Belani CP, Govindan R, Atkins JN, Gillenwater HH, Pallares C, Tye L, Selaru P, Chao RC, Scagliotti GV (2008) Multicenter, Phase II Trial of Sunitinib in Previously Treated, Advanced Non-Small-Cell Lung Cancer. J Clin Oncol 26:650-656
Acknowledgments
Supported by Pfizer Inc. (New York, NY) and the Sidney Kimmel Center for Prostate and Urologic Cancers. The authors would like to thank Carol Pearce, BA, MFA, writer/editor, editorial unit, Department of Medicine, Memorial Sloan-Kettering Cancer Center, for her critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Feldman, D.R., Turkula, S., Ginsberg, M.S. et al. Phase II trial of sunitinib in patients with relapsed or refractory germ cell tumors. Invest New Drugs 28, 523–528 (2010). https://doi.org/10.1007/s10637-009-9280-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-009-9280-2