Summary
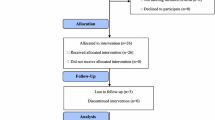
The purpose of this study was to evaluate the efficacy (progression free survival (PFS) and response rate) and safety of vinorelbine and trastuzumab combination chemotherapy in patients with HER2-overexpressing, metastatic breast cancer as a first line chemotherapy regimen. Patients with histologically confirmed, HER2-positive (immunohistochemistry (ICH) 3+, or 2+ and FISH+) metastatic breast cancer who had nor received prior vinorelbine or anti-HER2 therapy in the adjuvant setting, received at least eight weeks of vinorelbine i.v. (25 mg/g weekly) and trastuzumab (4 mg/kg on day 1 followed by 2 mg/kg weekly). Forty-one women from six participating centers were enrolled into the trial. The overall response rate, was 43.9% (18 of 41 patients), (CI 28–60.3%), 30% of patients were progression free after 1 year. Four patients reached complete remission, 14 partial remission and five had stable disease for at least 18 weeks. Six patients developed primary progression. 35 patients (85%) experienced progression after a median time of 235 days. Therapy was in general well-tolerated. There were two CTC grade 4 infusion syndromes and two patients experienced cardiotoxicity at least grade 2. This phase II trial of vinorelbine and trastuzumab demonstrated an effective and well-tolerated regimen with a favourable safety profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Advances in understanding breast cancer biology have led to a therapy guided by the biologic features of the tumour. HER-2/neu overexpressing is detected in about 25% to 30% of invasive breast cancers and is associated with an aggressive tumour phenotype and reduced survival rates [2–4]. The development of trastuzumab, a humanized monoclonal antibody directed against the human epidermal growth factor receptor-2 (HER-2) protein, has been a major achievement in the management of breast cancer. Trastuzumab was approved for clinical use by the Food and Drug Administration in 1998 and by the European authorities in 2000. In the pivotal trials of single agent trastuzumab in the metastatic setting, response rates of 30% and 15% have been reported in previously untreated [5] and treated HER2-positive patients [6], respectively. Single agent trastuzumab is generally well tolerated and not associated with the typical side effects seen with chemotherapeutic agents. Most side effects are mild to moderate and infusion-related reactions can usually be managed without withdrawal of trastuzumab [6, 7]. The benefits of trastuzumab in women with HER2-overexpressing breast cancer include response rates of 50% in combination with chemotherapy, improved time to progression and time to treatment failure and a significant 25% increase in survival duration at a 35 months of follow up [8]. The clinical benefits and tolerability of trastuzumab have been shown to maintain quality of life (QoL) of the patients [8, 9].
Preclinical studies indicated synergistic or additive interactions of trastuzumab with different chemotherapy agents [10, 11]. These investigations indicate that combinations of trastuzumab with vinorelbine, docetaxel and docetaxel plus platinum agents may have synergistic activity against breast cancer. These in vitro results have been confirmed by studies using mouse xenograft models [12]. Because of the improvement in survival, trastuzumab-based therapy has become a standard of care for women with HER2-positive advanced breast cancer and since 2 to 3 years in the adjuvant situation, too.
For vinorelbine anti-tumour-activity in metastatic breast cancer has been demonstrated in the first-line treatment setting. It appears to be similar to that reported for taxanes in phase II trials with 30–40% when used as first line therapy [13, 14]. However, taxanes are associated with a significant higher toxicity compared to vinorelbine. We performed a clinical study to determine the efficacy and safety of the combination of vinorelbine and trastuzumab in patients with HER-2/neu positive metastatic breast cancer as first line chemotherapy treatment.
Patients and methods
Patient eligibility
Eligible patients had histological confirmed HER2-overexpressing (ICH 3+ or 2+ and FISH+) metastatic breast cancer with measurable lesions in at least one site that has not been irradiated. Any previous adjuvant or neoadjuvant chemotherapy was permitted except vinorelbine or anti-HER2 therapy. Treatment with anthracyclines should have been finished at least six months ago and the cumulative dose should not have exceeded 360 mg/m2 of doxorubicin or 720 mg/m2 epirubicin. Prior hormone therapy for metastatic breast cancer was permitted. Any radiation therapy had to be completed at least three weeks before enrollment.
Other eligibility requirements included age ≥18 and ≤75 years, Karnofsky Index ≥70%, life expectancy ≥16 weeks, adequate hepatic, renal as well as bone marrow function defined by serum bilirubin ≤1.5× upper limit of normal, ALT and AST ≤2.5× upper limit of normal (unless related to liver metastasis), serum creatinine ≤1.5 upper limit of normal, haemoglobin ≥10 g/dl, neutrophils ≥1.5 × 109/l and platelets ≥100 × 109/l. Patients had to have normal cardiac function, with a LVEF not more than 10% below the normal limit.
Patients with pre-existing neuropathy in excess of WHO grade 2 were ineligible as well as patients with serious illness or a medical or psychiatric condition that might influence their ability to provide informed consent or to receive protocol-based therapy and patients with symptoms susceptible of cerebral or meningeal metastases. All patients had provided written informed consent before entering the study. The protocol was reviewed and approved by the institutional review boards of all participating centers.
Patients were enrolled between February 2002 and February 2003.
Treatment regimen
Treatment was administered in an outpatient setting. The initial trastuzumab infusion was 4 mg/kg intravenously (IV), administered over 60 min. Subsequently, trastuzumab was given weekly at 2 mg/kg i.v., administered over 30 min. Vinorelbine was given weekly on the same days as trastuzumab, after trastuzumab administration. At first application, vinorelbine and trastuzumab had to be given with a time interval of 2 h. The dose of vinorelbine was 25 mg/m2 administered in between 250 ml of saline solution prior and after the infusion. Patients were assessed with weekly complete blood count plus differential, and liver function tests every 4 weeks. The protocol called for the vinorelbine dose to be adjusted every week on the day of therapy, on the basis of haematologic toxicity and hepatotoxicity. Neutrophils less than 1 × 109/l required a delay of vinorelbine administration of 1 week. If vinorelbine could not have been given in 3 subsequent weeks due to toxicity, the treatment with vinorelbine was discontinued. Patients had LVEF measured at baseline and every 8 weeks during the study. Trastuzumab was withheld in patients experiencing absolute declines in LVEF of greater than 10% below the normal limit until a reevaluation 1 month later. In case of LVEF-stabilisation treatment with trastuzumab was continued again if further decrease of left ventricular function was noted, the patient was put off treatment. For patients experiencing a cardiac dysfunction of NYHA grade 3 or 4 trastuzumab was stopped immediately.
Any neurological toxicity greater than WHO grade 2 led to a discontinuation of vinorelbine.
Study analysis
Patients received weekly therapy and were assessed every 8 weeks. Tumour response was defined according to the Response Evaluation Criteria in Solid Tumours (RECIST). Patients with stable disease or with either complete response (CR) or partial response (PR) received ongoing treatment. After 24 weeks of combined treatment patients continued on trastuzumab only. Patients with progressive disease were taken off study. The primary endpoint of this study was best overall response rate on the basis of all eligible patients who received al least 8 weeks of protocol therapy. Secondary endpoints were time to tumour progression, median survival and assessment of tolerability. Calculation of the required patients to be enrolled in this study resulted from the two-stage minimax-design according to Simon [1].
Results
Patient characteristics
A total of 41 patients from six participating centers in Germany suffering from HER-2/neu overexpressing (ICH 3+[95%] or 2+ and FISH+) metastatic breast cancer were included in this evaluation. Patient characteristics are shown in Table 1.
Chemotherapy
Protocol therapy called for ongoing weekly trastuzumab treatment without dose modification and administration regardless of vinorelbine dosing. The average treatment duration was 120 days (median 138 days range 1 to 205 days; N = 41) and almost half of the patients received 24 applications of chemotherapy (N = 20). Eighteen patients (44%) completed the protocol. Reasons for going off study before completion of the protocol was progression (26%; N = 11), five patients (12%) withdrew consent for physician or patient preference; another five patients went off study due to serious adverse events, which were as follows: infection, allergic reaction, surgical intervention, pathological fracture and decline in LVEF.
Clinical efficacy
Objective response, either CR or PR, was seen in 18 of 41 patients (43.9%, CI 28–60.3%). Four patients reached CR, 14 PR and an additional five patients had stable disease for 18 weeks or longer, for details see Table 2.
Response rates were analyzed among clinical subsets of patients, defined by hormone-receptor status, prior adjuvant chemotherapy or hormone therapy treatment and menopausal status. Patients were analysed in different subsets: hormone-receptor-positive tumours versus hormone-receptor-negative tumours, patients who had received adjuvant chemotherapy or hormone therapy and patients who had not, or patients who were postmenopausal compared with patients who were not. These result are shown in Table 3.
Time to progression analysis
Six patients (15%) developed primary progression during the first 6 weeks of treatment, or within less than six applications, at a median time of 23 days after registration. Thirty-five patients (85%) experienced progression of disease after a median time to progression of 235 days. About 30% of patients were without disease progression at 1 year (see Fig. 1).
There was no statistically significant difference in time to progression with regard to different locations of metastases, hormone receptor status, adjuvant chemotherapy, palliative hormone therapy or menopausal status, as shown in Table 4.
About half of the patients died (21 of 41 patients, 51%) with an average overall survival of 429 days (33–850 days) from registration, with a median of 411 days (Fig. 2).
Tolerability analysis
The incidence and severity of acute toxicity associated with combined trastuzumab–vinorelbine therapy was quite low. All treatment-related toxicities that occurred in more than 10% of patients on study or were in excess of CTC grade 2 are shown in Table 5. We documented 14 serious adverse events (SAEs), nine of them clearly not associated with the study drugs (vinorelbine or trastuzumab).
Discussion
For women with Her-2/neu overexpressing metastatic breast cancer, treatment with trastuzumab combined with chemotherapy is the standard of care.
While in vitro studies were able to demonstrate an additive anti-tumour effect of docetaxel plus trastuzumab, other substances (vinorelbine, docetaxel, and cisplatin) showed a synergistic effect. In vivo, it was possible to demonstrate, that vinorelbine plus trastuzumab regimens are not only superior to paclitaxel containing regimens in terms of toxicity [15], but also in terms of response and survival [16, 17]. For example the TRAVIOTA study showed 51% remission rate for vinorelbine plus trastuzumab versus 40% for the taxane-containing regimen and a median time to progression of 8.5 versus 6.0 months for the vinorelbine combination [18].
This is in the line with the current phase II trial of vinorelbine and trastuzumab in patients with HER2-neu positive metastatic breast cancer which demonstrated high response rates of clinical activity achieved with limited acute toxicities.
Almost half of the patients had an objective response with 10% CR and 34% PR. About 30% of patients were without disease progression at 1 year. The clinical outcome was not significantly affected by other factors.
This confirms the results of other recent clinical studies of this combination both in untreated and in heavily pre-treated patients with HER-2/neu positive metastatic breast tumours. Different phase II trials have shown high objective response rates (44–78%) [16, 18, 19–22]. The slightly lower objective response rate may be due to the intent-to-treat-analysis and the high number of not evaluable patients in the current trial (n = 8).
The haematologic and non-haematologic toxicities were well within the range expected from different other trials. Cardiotoxicity, a side effect of particular concern in trastuzumab treatment, was acceptably low; only one patient experienced cardiotoxicity of grade 3 (grade 3 arrhythmia), which is not known as caused by trastuzumab, and another patient developed asymptomatic grade 2 decrease of LVEF (<50%).
The favourable safety profile of the vinorelbine/trastuzumab combination has consistently been shown in other trials and the rates of cardiomyopathy were not higher than those reported with trastuzumab as single agent [6]. In the study by Jahanzeb et al. [20] no grade 3–4 cardiac toxicity was seen and Burstein et al. [16] described only one patient with grade 3 cardiac toxicity.
Compared to combination therapy with taxanes, vinorelbine causes only mild alopecia. Docetaxel induced distracting onycholysis is not observed by the vincaalkaloid. Cumulative neurotoxicity observed using vinorelbine is less marked than with other vincaalkaloids such as vincristine and vindesine and less common than using a taxane-containing regimen. Concerning haematologic toxicities vinorelbine is comparable to a taxane regimen. However docetaxel/trastuzumab offers the advantage of a three weeks schedule over the weekly application of vinorelbine combined with the antibody. As many patients with relapsing breast cancer received taxane containing therapy regimens in the adjuvant setting, vinorelbine is a relevant combination partner for trastuzumab in first line treatment. Capecitabine, a potential alternative, offering similar advantages concerning oral administration and non-causing alopezia as vinorelbine, is right now the only compound tested as a chemotherapy partner for lapatinib in patients with advanced HER-2/neu positive breast cancer in case of disease progression in patients receiving trastuzumab and should therefore not be used as a first line substance. Nowadays the oral application of vinorelbine enables a 3 weeks application schedule of trastuzumab, too, and may be preferable to the i.v. administration: The oral regimen showed comparable results in overall response rates (43–68%) and median time to progression (8.9–9.0 months) to our herein presented study [23, 24].
In conclusion, weekly vinorelbine/trastuzumab may be considered an acceptable option for HER2-overexpressing patients as it represents an effective and well-tolerated therapy. At last, the decision which combination therapy is favoured, should always made together with the patient, taking her individual living conditions into consideration.
References
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10. doi:10.1016/0197-2456(89)90015-9
Berger MS et al (1988) Correlation of c-erbB-2 gene amplification and protein expression in human breast carcinoma with nodal status and nuclear grading. Cancer Res 48(5):1238–1243
Slamon DJ et al (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235(4785):177–182. doi:10.1126/science.3798106
Slamon DJ et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244(4905):707–712. doi:10.1126/science.2470152
Vogel CL et al (2002) Efficacy and safety of trastuzumab as a single agent in first-line treatment of HER2-overexpressing metastatic breast cancer. J Clin Oncol 20(3):719–726. doi:10.1200/JCO.20.3.719
Cobleigh MA et al (1999) Multinational study of the efficacy and safety of humanized anti-HER2 monoclonal antibody in women who have HER2-overexpressing metastatic breast cancer that has progressed after chemotherapy for metastatic disease. J Clin Oncol 17(9):2639–2648
Baselga J et al (1999) Phase II study of weekly intravenous trastuzumab (Herceptin) in patients with HER2/neu-overexpressing metastatic breast cancer. Semin Oncol 26(4 Suppl 12):78–83
Slamon DJ et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344(11):783–792. doi:10.1056/NEJM200103153441101
Osoba D et al (1999) Health-related quality of life in women with metastatic breast cancer treated with trastuzumab (Herceptin). Semin Oncol 26(4 Suppl 12):84–88
Pegram MD et al (1999) Inhibitory effects of combinations of HER-2/neu antibody and chemotherapeutic agents used for treatment of human breast cancers. Oncogene 18(13):2241–2251. doi:10.1038/sj.onc.1202526
Pegram MD et al (2004) Rational combinations of trastuzumab with chemotherapeutic drugs used in the treatment of breast cancer. J Natl Cancer Inst 96(10):739–749
Pietras RJ et al (1998) Remission of human breast cancer xenografts on therapy with humanized monoclonal antibody to HER-2 receptor and DNA-reactive drugs. Oncogene 17:2235–2249. doi:10.1038/sj.onc.1202132
Gianni L et al (1995) Paclitaxel in metastatic breast cancer: a trial of two doses by a 3-hour infusion in patients with disease recurrence after prior therapy with anthracyclines. J Natl Cancer Inst 87(15):1169–1175. doi:10.1093/jnci/87.15.1169
Seidman AD et al (1995) Phase II trial of paclitaxel by 3-hour infusion as initial and salvage chemotherapy for metastatic breast cancer. J Clin Oncol 13(10):2575–2581
Suzuki Y et al (2003) Combination of trastuzumab and vinorelbine in metastatic breast cancer. Jpn J Clin Oncol 33(10):514–517. doi:10.1093/jjco/hyg101
Burstein HJ et al (2003) Trastuzumab and vinorelbine as first-line therapy for HER2-overexpressing metastatic breast cancer: multicenter phase II trial with clinical outcomes, analysis of serum tumour markers as predictive factors, and cardiac surveillance algorithm. J Clin Oncol 21(15):2889–2895. doi:10.1200/JCO.2003.02.018
Winer EP, Burstein HJ (2001) New combinations with Herceptin in metastatic breast cancer. Oncology 61(Suppl 2):50–57. doi:10.1159/000055402
Burstein HJ et al (2007) Trastuzumab plus vinorelbine or taxane chemotherapy for HER2-overexpressing metastatic breast cancer: the trastuzumab and vinorelbin or taxane study. Cancer 110(5):965–972. doi:10.1002/cncr.22885
Franquesa R, Centelles M, Villadiego K (2005) A multicenter study of trastuzumab (H) and vinorelbine (N) as first and second line therapy for patients with HER2-positive metastatic breast cancer (HER2+ MBC). ASCO Meeting Abstracts, 868
Jahanzeb M et al (2002) Phase II trial of weekly vinorelbine and trastuzumab as first-line therapy in patients with HER2(+) metastatic breast cancer. Oncologist 7(5):410–417
Burstein HJ et al (2001) Clinical activity of trastuzumab and vinorelbine in women with HER2-overexpressing metastatic breast cancer. J Clin Oncol 19(10):2722–2730
Porta V, Martin M, Gil M (2004) Evaluation of vinorelbine (N) and trastuzumab (H) as first line therapy for HER2-positive metastatic breast cancer (HER2+ MBC): impact on clinical response and cardiac function. ASCO Meeting Abstracts: 636
Bartsch R, Wenzel C, Altorjai G (2007) Results from an observational trial with oral vinorelbine and trastuzumab in advanced breast cancer. Breast Cancer Res Treat 102(3):375–381. doi:10.1007/s10549-006-9342-5
Catania C, Medici M, Magni E (2007) Optimizing clinical care of patients with metastatic breast cancer: a new oral vinorelbine plus trastuzumab combination. Ann Oncol 18(12):1969–1975. doi:10.1093/annonc/mdm372
Acknowledgments
We thank all participating patients and attending medical staff in the different centers, Klaus Pahnke, Büro für Statistik, Reinheim, Germany for statistical analyses and the monitors of GSO-Gesellschaft für Studienmanagement und Onkologie mbH, Hamburg, Germany. Financial support was provided by Pierre Fabre Pharma GmbH, Freiburg, Germany and Hoffmann-La Roche AG, Grenzach-Wyhlen, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schilling, G., Bruweleit, M., Harbeck, N. et al. Phase II trial of vinorelbine and trastuzumab in patients with HER2-positive metastatic breast cancer. A prospective, open label, non-controlled, multicenter phase II trial (to investigate efficacy and safety of this combination chemotherapy). Invest New Drugs 27, 166–172 (2009). https://doi.org/10.1007/s10637-008-9166-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-008-9166-8