Summary
Background ZD6126 is a novel vascular-targeting agent that disrupts the endothelial tubulin cytoskeleton causing selective occlusion of tumor vasculature and extensive tumor necrosis. This Phase I clinical study was conducted to evaluate the dose and administration schedule of ZD6126. Methods Adult patients with solid tumors refractory to existing treatments received a 10-min, single-dose intravenous infusion of ZD6126 every 14 or 21 days. Subsequent dose escalation was performed, based on the incidence of adverse events (AEs) within the first cycle of drug administration. Blood samples were obtained for pharmacokinetic analysis, and the effects of ZD6126 on tumor vasculature were visualized using DCE-MRI technology. Results Forty-four patients received ZD6126 (5−112 mg/m2 in the 21-day schedule, n = 35; 40−80 mg/m2 in the 14-day schedule, n = 9). Common AEs were similar in both groups and included abdominal pain, nausea and vomiting, which appeared to be dose related. The incidence of abdominal pain at 112 mg/m2 in the 21-day study prevented further dose escalation. Pharmacokinetic studies confirmed that ZD6126 is rapidly hydrolyzed to ZD6126 phenol. There was no difference in the pharmacokinetics of ZD6126 phenol upon repeat administration or between the two dosing regimens. DCE-MRI evaluation has demonstrated the antivascular effects of ZD6126. Conclusions This study identified that ZD6126 administered every 2 or 3 weeks at 80 mg/m2 was well tolerated, with mild but manageable gastrointestinal AEs. In approximately 11% (5 out of 44) of patients, ZD6126 was associated with cardiac events categorized as dose limiting toxicities (one patient with asymptomatic decreased left ventricular ejection fraction (LVEF), two with increased troponin concentrations, one with myocardial ischemia, and one with ECG signs of myocardial ischemia).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The development of a functional vascular system that allows sufficient blood and nutrient supply as well as the effective removal of waste products is essential to the survival of solid tumors [1]. Targeting the tumor vasculature therefore has great potential as a novel therapeutic approach. The clinical value of this approach has been demonstrated with bevacizumab, a recombinant humanized monoclonal antibody that inhibits the biologic activity of vascular endothelial growth factor, thereby preventing angiogenesis. In combination with conventional chemotherapy, bevacizumab therapy has been shown to significantly improve survival in patients with metastatic colon cancer [2]. In contrast to bevacizumab and antiangiogenic agents currently in development, vascular-targeting agents exploit the differences between blood vessels in healthy tissue and those of the tumor, to disrupt the tumor blood flow. The tumor vasculature is characterized by the presence of a rapidly proliferating endothelium and a chaotic network of highly permeable vessels [3, 4]. Unlike stable physiological endothelium with its actin cytoskeleton and supporting pericytes, immature endothelial cells rely to a greater extent on the tubulin cytoskeleton for the maintenance of cell structure [5].
ZD6126 is a novel vascular-targeting agent that is rapidly converted by serum phosphatases to the active agent ZD6126 phenol [6]. ZD6126 phenol binds to tubulin leading to inhibition of tubulin polymerization and subsequent microtubule destabilization [7]. This action results in morphological changes in the immature tumor endothelial cells that are highly dependent on tubulin to maintain their shape. In contrast, the normal vascular endothelium remains unaffected [7]. Sub-toxic doses of ZD6126 have been shown to exhibit significant antitumor activity in a broad range of in vivo rodent carcinoma models [8–10]. In addition, ZD6126 effectively inhibits tumor growth, attenuates endothelial cell proliferation and density as well as eliciting tumor cell necrosis and significant reduction of peritoneal carcinomatosis in an orthotopic human gastric cancer model [11]. All vascular-targeting agents evaluated to date have demonstrated a rim of surviving tissue at the periphery of the tumor, the so-called viable rim, which is thought to arise due to these cells gaining oxygen and nutrients from surrounding normal blood vessels [10, 12]. As both conventional anticancer agents and radiotherapy are particularly effective against these well-vascularized areas, ZD6126 may be of clinical value in combination with existing therapies [13, 14]. For example, in a renal carcinoma model, ZD6126 in combination with cisplatin led to significant enhancement of antitumor activity with no exacerbation of cisplatin toxicity [13]. Of note, however, preclinical safety pharmacology studies showed changes in the cardiovascular system, including reductions in heart rate, increases in blood pressure and reductions in cardiac output [15, 16].
ZD6126 has been investigated in a series of clinical trials, primarily to define the maximum tolerated dose (MTD), to recommend a dose and schedule suitable for further studies, and to determine the safety, tolerability and efficacy [12, 17–19]. Here, we report the results of one of three phase I studies investigating ZD6126 administered every 21 or 14 days in an open-label, non-comparative, dose-escalation study.
Materials and methods
Patient selection
This study recruited adult patients (>18 years of age) at Wayne State University, Karmanos Cancer Institute. All patients were required to have solid tumors refractory to other treatments, a WHO performance status of 0−2, and life expectancy of >12 weeks. Patients with significant hematopoietic, hepatic, renal or cardiac dysfunction, brain metastases or chemotherapy/radiotherapy treatment within 4 weeks of trial commencement were excluded. Concomitant use of any other cancer therapy, rifampicin, phenytoin, carbamazepine, phenobarbitol, ketoconazole, fluconazole or aspirin was not permitted during the trial. The target number of patients was 60, with a minimum of three patients per cohort. The actual number of patients to be recruited depended on the number of dose escalations required to arrive at the MTD. All patients provided written informed consent. The study was approved by the relevant institutional ethical committees or review bodies, and was conducted in accordance with the declaration of Helsinki and the AstraZeneca policy on Bioethics.
Study design
Pre-trial patient assessments were carried out 14 days prior to trial entry, which included physical examination and vital signs, WHO performance status, assessment of tumor markers and objective tumor assessment.
ZD6126 was administered according to two schedules, either once every 21 days or once every 14 days. In each group, patients received a single initial dose of ZD6126 administered as a 10-min intravenous infusion, followed by either a 21- or 14-day observation period. At the end of this period, provided that all toxicities had returned to baseline values, patients went on to receive repeat cycles of ZD6126 at the same dose until withdrawal criteria were reached (occurrence of dose-limiting toxicity [DLT], unresolved Common Toxicity Criteria [CTC] grade 2 toxicity, progressive disease, or patient request). DLTs were defined as any CTC grade 3 or 4 that was not manageable with maximum supportive care; grade 4 neutropenia for more than 5 days; grade 4 thrombocytopenia of any duration; any cardiotoxic event (grade 1 cardiac arrhythmia, change in ejection fraction, blood pressure or heart rate, ECG abnormalities or elevation of cardiac enzymes).
In the 21-day dosing study, ZD6126 was administered at a starting dose of 5 mg/m2. Dose escalation was performed in two phases, phases A and B, and decisions about re-dosing and dose escalation were based on the incidence of adverse events (AEs) observed during treatment and follow up as well as on the overall pattern of toxicity in all patients. In phase A, when less than two patients experienced a grade 2 toxicity and in the absence of DLT, doses were doubled in subsequent cohorts (intra-patient dose escalation was not permitted). A minimum of three patients were evaluated for toxicity at each dose level. In the event of any single occurrence of a drug-related DLT or when two or more patients experienced a grade 2 toxicity, phase B was initiated. This entailed a dose escalation 40% higher than the current dose where dose escalation (up to 112 mg/m2 maximum) was assessed by clinical judgement until the MTD was attained. MTD was defined as the dose at which there is a 33% probability of experiencing a DLT within the first 21 days of drug administration. Patients experiencing a DLT received no further drug administration at the causative dose and either went on to receive a lower dose or were withdrawn from the trial. Patients experiencing a non-DLT went on to receive additional cycles of ZD6126 upon resolution of baseline toxicity values within the 21-day observation period after an additional 14-day period. In the 14-day dosing schedule, three-patient cohorts began with a starting dose of 40 mg/m2 followed by a repeat 14-day cycle upon the resolution of baseline toxicity levels. Following two repeat drug cycles (28 days) dose escalation was implemented to 56 mg/m2 and then to 80 mg/m2 unless two patients within a cohort experienced a drug-related DLT, at which point the MTD was determined. All patients on the 14-day schedule were pre-medicated for abdominal pain, and nausea and vomiting.
Study assessments
The primary objective of this study was to determine the MTD of ZD6126, characterize its DLTs and recommend a dose and schedule suitable for further clinical evaluation. Secondary objectives were to assess the antitumor activity of ZD6126 and determine the pharmacokinetic profile of ZD6126 and ZD6126 phenol (the active metabolite of ZD6126).
Adverse events
Full physical, hematological, neurological and ophthalmic assessments were carried out on trial entry, along with vital signs, urinanalysis and cardiological assessment (troponin levels, ECG and left ventricular ejection fraction [LVEF]) and were repeated at given intervals throughout the trial. 12-lead ECGs were performed within 7 days prior to day 1 and repeated on day 1 within 1 h and 24 h after the dose of ZD6126 and on day 21 (day 14 for the 14-day schedule). For all repeat cycles, ECG was performed on day 1 within 1 h and 24 h after the dose of ZD6126, and on day 21. A follow-up ECG was performed on all patients 60 days after the last dose of medication.
All AEs were defined as the development of a new medical condition or the deterioration of a pre-existing medical condition following or during exposure to ZD6126. When considered drug-induced, AEs were graded according to the National Cancer Institute CTC version 2.0 and recorded at each clinic visit.
Tumor response to treatment
Baseline objective tumor assessments were performed within 14 days of trial commencement. Reassessments were performed at the end of cycle 2 and every even-numbered cycle thereafter and if possible at withdrawal from the trial. For the 14-day schedule, objective tumor assessments were performed every 6 weeks. Tumor response was evaluated according to the revised version of the UICC/WHO criteria.
Patients with soft tissue, liver, fixed pelvic or bone tumor masses suitable for evaluation of blood flow and vascularity were assessed by dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI). This was performed pre dose (within 7 days), 4−6 h from the end of infusion, and then approximately 24 h and 18−21 days after treatment in cycle 1. Subsequent MRIs were performed on day 21 of even-numbered cycles.
MRI acquisition and analysis were performed as described previously [12]. Briefly, MRI data were acquired with a 1.5 Tesla Siemens Visionplus device using body coil excitation and surface coil reception. 3D images were acquired using a spoiled gradient-echo sequence (sixteen 8-mm slices zero-filled to 32 4-mm slices, acquiring a 128 × 256 matrix zero-filled to 256 × 256 with a 40 cm field of view, 1.8-ms echo time, 3.8-ms repetition time, giving an acquisition time of 7.9 s per 3D dataset). Two datasets (number of averages [NA] = 8) were obtained pre-contrast with 2° and 13° flip angles (T1 estimation and pre-contrast background). Continuous (NA = 1, 13° flip angle) images were taken before, during and after bolus intravenous injection of 0.1 mmol/kg Magnevist contrast agent. Voxel-wise analysis of tumor, muscle and spleen regions of interest (ROI) was performed. Signal increases were converted to contrast pseudoconcentrations [20] and the initial area under the contrast agent concentration–time curve (iAUCg) [21] was calculated for the first 60 s after bolus arrival. Median iAUC values were calculated and percentage changes from baseline (pre-treatment) determined for each ROI. The coefficient of variation (CV) was calculated as 100 × √[exp (s 2) − 1], where ‘s’ is the standard deviation of the data on a log scale.
Pharmacokinetic evaluation
Venous blood samples were obtained during cycles 1 and 2 for pharmacokinetic analysis. Samples were collected pre dose; 5, 10, 20 and 30 min from the start of infusion; and 1, 2, 4, 8, 10, 24 and 48 h from the start of infusion. The following pharmacokinetic parameters were determined for ZD6126 phosphate: Maximum plasma concentrations (C max) and the time of maximum plasma concentrations (t max). For ZD6126 phenol, C max, t max, area under the plasma-concentration-versus-time curve from zero to infinity (AUC) and to 6 h after the dose (AUC0-t), clearance, volume of distribution at steady-state (V ss) and terminal half-life were determined using WinNonlin v3.1 (Pharsight Corp, Palo Alto, CA, USA). Comparisons of the parameter values were made following administrations in cycle 1 and cycle 2 to assess any changes upon repeat administration.
Results
Patient characteristics
A total of 44 patients received 14- or 21-day cycles of ZD6126 therapy (Tables 1 and 2). The first patient was enrolled in January 2001, and the last patient completed the study in December 2003. Patient discontinuations were primarily due to disease progression (94.3%).
Safety and tolerability
The AE profile of ZD6126 is summarized in Tables 3, 4 and 5. The total number of AEs, drug-related AEs, and serious AEs (SAEs) were similar in the 14- and 21-day schedules. In the 14-day schedule, SAEs were noted in two patients at the 40 mg/m2 dose. In the 21-day schedule, one, two, three and two patients were noted with SAEs at the 20, 40, 80 and 112 mg/m2 doses respectively. There were two adverse events leading to withdrawal, one each at the 40 and 112 mg/m2 dose groups. Common AEs in the 21-day study included abdominal pain, nausea, constipation and dyspnea. The etiology of abdominal pain was unclear and generally resolved within 12 h. This event did, however, lead to the discontinuation of dose escalation at 112 mg/m2. Pre-medication to manage the pain was adopted during the trial. The majority of reported abdominal pain, nausea and vomiting were considered drug related. As patients on the 14-day schedule were pre-medicated for abdominal pain, nausea and vomiting, the incidence and severity of these events were lower in this group. Overall, 71% of patients in the 21-day schedule and 67% of patients in the 14-day schedule experienced a drug-related AE.
In the 21-day schedule, CTC grade 3 SAEs were seen in five (n = 35) patients (dyspnea, pleural effusion, intestinal obstruction, increased troponin levels and hypotension). This led to withdrawal only in the case of increased troponin levels, which occurred in two patients and were considered DLTs. The hypotension was considered drug-related and also categorized as a DLT. Two patients on the 21-day schedule had abnormal LVEF measurements. One patient had a grade 1 decrease in LVEF measurement (from 61% to 47%) after the first dose of ZD6126 which was categorized as a DLT. LVEF level subsequently improved to 60% after the second dose. The other patient had an abnormal LVEF measurement of 47% associated with grade 2 ventricular hypokinesia occurring approximately 5 weeks following the last dose of ZD6126. LVEF measurements taken 3 weeks following the last dose of ZD6126 were normal, therefore this AE did not occur within the DLT reporting window. These findings contributed to the development of a protocol amendment requiring a repeat LVEF within 5 days if the LVEF was abnormal or had a decrease of 10% or greater from baseline and another amendment requiring a repeat LVEF within 60 days of the final dose. Additional DLTs included one patient with grade 2 myocaridal ischemia and another with ECG signs of myocaridal ischemia (grade 1). All drug-related adverse events categorized as DLTs (occurring within the first 21 days of drug administration) in the 21-day schedule are summarized in Table 5. No significant myelosuppression was noted in the 21-day schedule.
In the 14-day portion of the study (n = 9), three CTC grade 3 SAEs were reported in two patients (thrombocytopenia and two cases of sepsis). The thrombocytopenia was considered to be related to treatment. None of these grade 3 events led to treatment withdrawal and none were considered DLTs. No evidence of increased troponin levels or myocardial ischemia was observed. Three patients had abnormal LVEFs on MUGA scans. However, when the scans were repeated, the abnormalities did not persist and did not meet DLT criteria. Patients on this schedule were evaluated over two 14-day cycles for the occurrence of DLTs and no toxicities meeting the DLT definition were observed within the 28-day reporting timeframe. One death was reported in the 30-day follow-up phase of the study. However, this was attributed to disease progression.
Pharmacokinetic evaluation
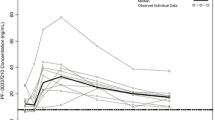
ZD6126 was rapidly hydrolyzed to yield the metabolite ZD6126 phenol. On exposure to ZD6126, a large degree of variability was observed in the C max of ZD6126, and in the C max and AUC of ZD6126 phenol. The mean plasma concentration–time profiles of ZD6126 phenol in cycles 1 and 2 following administration of ZD6126 on the 21-day schedule are presented in Fig. 1. The pharmacokinetic characteristics of ZD6126 phenol appeared linear across the dose groups investigated. Comparison of the cycle 1 and cycle 2 data showed that there were no cycle differences in the pharmacokinetics of ZD6126 phenol. C max, AUC and half-life values were approximately constant across the two treatment schedules (Table 6). Observed cardiac side effects were not found to be associated with any pharmacokinetic aberrancies in drug concentration, exposure, or change in clearance of ZD6126.
Antitumor activity
No objective tumor responses were observed in this study. Of the 34 patients on the 21-day schedule who were evaluated for objective tumor response, two had a best overall response of stable disease, the remainder demonstrating disease progression. In the 14-day dosing schedule, 22.2% of patients had an overall response of stable disease and the remaining 77.8% of patients experienced disease progression.
DCE-MRI was used to measure the effect of ZD6126 on tumor vasculature. DCE-MRI scans were analyzed to derive tumor volume and iAUC60 for liver metastases, muscle and spleen. Analysis was performed for nine patients (four men and five women) who had liver metastases originating from mixed primary solid tumors. Tumor iAUC 6 h after ZD6126 administration was lower than before administration in all tumors, and this effect appeared to increase with higher doses. The within-tumor CV for iAUC was 18%. All patients receiving ZD6126 ≥80 mg/m2 had a decrease in iAUC compared with pre-treatment values of greater than approximately twice the CV. This decrease in tumor iAUC appeared to be maintained in most cases for at least 24 h, although there was some evidence of partial recovery 18−21 days after ZD6126 treatment (Table 7; Fig. 2). No ZD6126-induced changes were apparent in muscle iAUC and no consistent changes were observed in the spleen, a result that has been noted in a previous clinical study with ZD6126 [12].
Discussion
In this phase I study, ZD6126 was generally well tolerated at doses up to 80 mg/m2 in both the 14- and 21-day schedules. Dose-related AEs were primarily abdominal pain, nausea, vomiting and hypertension, all of which were readily managed clinically. In the 21-day schedule, the dose of ZD6126 was escalated from 5 to 112 mg/m2. At 112 mg/m2, abdominal pain precluded further dose escalation. In the 14-day schedule, patients were enrolled at doses of 40, 56 and 80 mg/m2 and no additional toxicities were noted with this schedule. Dose recommendations from this study are therefore ZD6126 administered at 80 mg/m2 once every 2−3 weeks. In approximately 11% (5 out of 44) of patients enrolled in this study, ZD6126 was associated with cardiac events (three patients with asymptomatic decreased LVEF and two with increased troponin concentrations) suggestive of ischemia. A recent study by Gould et al. used a rat preclinical model to examine the underlying mechanisms responsible for cardiac events associated with ZD6126 and found the agent induces acute hemodynamic changes (hypertension and delayed tachycardia) that are prerequisites for cardiac damage in the rat model system [16]. The etiology of this toxicity in humans warrants further investigation. Another vascular targeting agent DMXAA has shown transient, dose-dependent increases in blood pressure [22, 23].
Pharmacokinetic evaluation in this study revealed that ZD6126 was rapidly hydrolyzed to ZD6126 phenol and was generally no longer quantifiable after 10 to 20 min. At lower doses, a terminal half-life of approximately 2 h was observed. At higher doses, the plasma half-life was in the range of 5−10 h. The results also demonstrate no apparent differences in the pharmacokinetics of ZD6126 phenol between cycle 1 and cycle 2, indicating that the drug was cleared between administrations. This was the case when ZD6126 was administered on an accelerated dosing schedule (a single dose every 14 days) or on a longer dosing schedule (a single dose once every 21 days). The data from this study alongside that from other ZD6126 studies has established that there is no relationship between ZD6126 clearance and body surface area; therefore, it is not necessary to adjust the dose according to body size and a unit-dose approach may be adopted [24].
In this phase I study, secondary evaluation of tumor response showed no clinically meaningful improvement. Assessment of the antivascular effects of ZD6126 through DCE-MRI has, however, demonstrated that ZD6126 produced consistent decreases in tumor blood supply at a dose ≥80 mg/m2. ZD6126-induced changes in iAUC were dose related and were selective for the tumor relative to spleen or muscle. DCE–MRI has been widely used in animal and human studies, establishing this simple technique as a robust method of determining the effects of vascular-targeting agents [12, 25–27].
In conclusion, this study has demonstrated the antivascular effects of ZD6126 and identified a dose of 80 mg/m2 administered according to a 2- or 3-week schedule to be a recommended dose.
References
Folkman J (1992) The role of angiogenesis in tumor growth. Semin Cancer Biol 3:65–71
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350:2335–2342
Denekamp J (1993) Review article: angiogenesis, neovascular proliferation and vascular pathophysiology as targets for cancer therapy. Br J Radiol 66:181–196
Denekamp J (1990) Vascular attack as a therapeutic strategy for cancer. Cancer Metastasis Rev 9:267–282
Gotlieb AI (1990) The endothelial cytoskeleton: organization in normal and regenerating endothelium. Toxicol Pathol 18:603–617
Blakey DC, Ashton SE, Westwood FR, Walker M, Ryan AJ (2002) ZD6126: a novel small molecule vascular targeting agent. Int J Radiat Oncol Biol Phys 54:1497–1502
Davis PD, Dougherty GJ, Blakey DC, Galbraith SM, Tozer GM, Holder AL, Naylor MA, Nolan J, Stratford MR, Chaplin DJ, Hill SA (2002) ZD6126: a novel vascular-targeting agent that causes selective destruction of tumor vasculature. Cancer Res 62:7247–7253
Robinson SP, McIntyre DJ, Checkley D, Tessier JJ, Howe FA, Griffiths JR, Ashton SE, Ryan AJ, Blakey DC, Waterton JC (2003) Tumour dose response to the antivascular agent ZD6126 assessed by magnetic resonance imaging. Br J Cancer 88:1592–1597
Micheletti G, Poli M, Borsotti P, Martinelli M, Imberti B, Taraboletti G, Giavazzi R (2003) Vascular-targeting activity of ZD6126, a novel tubulin-binding agent. Cancer Res 63:1534–1537
Blakey DC, Westwood FR, Walker M, Hughes GD, Davis PD, Ashton SE, Ryan AJ (2002) Antitumor activity of the novel vascular targeting agent ZD6126 in a panel of tumor models. Clin Cancer Res 8:1974–1983
McCarty MF, Takeda A, Stoeltzing O, Liu W, Fan F, Reinmuth N, Akagi M, Bucana C, Mansfield PF, Ryan A, Ellis LM (2004) ZD6126 inhibits orthotopic growth and peritoneal carcinomatosis in a mouse model of human gastric cancer. Br J Cancer 90:705–711
Evelhoch JL, LoRusso PM, He Z, DelProposto Z, Polin L, Corbett TH, Langmuir P, Wheeler C, Stone A, Leadbetter J, Ryan AJ, Blakey DC, Waterton JC (2004) Magnetic resonance imaging measurements of the response of murine and human tumors to the vascular-targeting agent ZD6126. Clin Cancer Res 10:3650–3657
Siemann DW, Rojiani AM (2002) Antitumor efficacy of conventional anticancer drugs is enhanced by the vascular targeting agent ZD6126. Int J Radiat Oncol Biol Phys 54:1512–1517
Hoang T, Huang S, Armstrong E, Eickhoff JC, Harari PM (2006) Augmentation of radiation response with the vascular targeting agent ZD6126. Int J Radiat Oncol Biol Phys 64:1458–1465
AstraZeneca Corp (2003) Investigator’s brochure. ZD6126—a vascular targeting agent
Gould S, Westwood FR, Curwen JO, Ashton SE, Roberts DW, Lovick SC, Ryan AJ (2007) Effect of pretreatment with atenolol and nifedipine on ZD6126-induced cardiac toxicity in rats. J Natl Cancer Inst 99:1724–1728
Beerepoot LV, Radema SA, Witteveen EO, Thomas T, Wheeler C, Kempin S, Voest EE (2006) Phase I clinical evaluation of weekly administration of the novel vascular-targeting agent, ZD6126, in patients with solid tumors. J Clin Oncol 24:1491–1498
Gadgeel SM, LoRusso PM, Wozniak AJ, Wheeler C (2002) A dose-escalation study of the novel vascular-targeting agent, ZD6126, in patients with solid tumors. Proc Am Soc Clin Oncol 21 (abstract 438)
DelProposto Z, LoRusso P, Latif Z, Morton P, Wheeler C, Barge A, Evelhoch J (2002) MRI evaluation of the effects of the vascular-targeting agent ZD6126 on tumor vasculature. Proc Am Soc Clin Oncol 21 (abstract 440)
Landis CS, Li X, Telang FW, Coderre JA, Micca PL, Rooney WD, Latour LL, Vetek G, Palyka I, Springer CS Jr (2000) Determination of the MRI contrast agent concentration time course in vivo following bolus injection: effect of equilibrium transcytolemmal water exchange. Magn Reson Med 44:563–574
Leach MO, Brindle KM, Evelhoch JL, Griffiths JR, Horsman MR, Jackson A, Jayson GC, Judson IR, Knopp MV, Maxwell RJ, McIntyre D, Padhani AR, Price P, Rathbone R, Rustin GJ, Tofts PS, Tozer GM, Vennart W, Waterton JC, Williams SR, Workman P (2005) The assessment of antiangiogenic and antivascular therapies in early-stage clinical trials using magnetic resonance imaging: issues and recommendations. Br J Cancer 92:1599–1610
McKeage MJ, Fong P, Jeffery M, Baguley BC, Kestell P, Ravic M, Jameson MB (2006) 5,6-Dimethylxanthenone-4-acetic acid in the treatment of refractory tumors: a phase I safety study of a vascular disrupting agent. Clin Cancer Res 12:1776–1784
Jameson MB, Thompson PI, Baguley BC, Evans BD, Harvey VJ, Porter DJ, McCrystal MR, Small M, Bellenger K, Gumbrell L, Halbert GW, Kestell P (2003) Clinical aspects of a phase I trial of 5,6-dimethylxanthenone-4-acetic acid (DMXAA), a novel antivascular agent. Br J Cancer 88:1844–1850
Oliver R, Wheeler C, Langmuir P, Melezinek I, Stone A (2004) Evaluation of the role of body-surface-area dose adjustment of ZD6126, a novel vascular-targeting agent. Proc Am Soc Clin Oncol 22 (abstract 3065)
Galbraith SM, Maxwell RJ, Lodge MA, Tozer GM, Wilson J, Taylor NJ, Stirling JJ, Sena L, Padhani AR, Rustin GJ (2003) Combretastatin A4 phosphate has tumor antivascular activity in rat and man as demonstrated by dynamic magnetic resonance imaging. J Clin Oncol 21:2831–2842
Galbraith SM, Rustin GJ, Lodge MA, Taylor NJ, Stirling JJ, Jameson M, Thompson P, Hough D, Gumbrell L, Padhani AR (2002) Effects of 5,6-dimethylxanthenone-4-acetic acid on human tumor microcirculation assessed by dynamic contrast-enhanced magnetic resonance imaging. J Clin Oncol 20:3826–3840
Murata R, Overgaard J, Horsman MR (2001) Comparative effects of combretastatin A-4 disodium phosphate and 5,6-dimethylxanthenone-4-acetic acid on blood perfusion in a murine tumour and normal tissues. Int J Radiat Biol 77:195–204
Acknowledgement
This study was supported by AstraZeneca, Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Previous presentations of study: Preliminary data from this study were presented at: 2001 AACR-NCI-EORTC (poster); 2002 American Society of Clinical Oncology (poster).
Rights and permissions
About this article
Cite this article
LoRusso, P.M., Gadgeel, S.M., Wozniak, A. et al. Phase I clinical evaluation of ZD6126, a novel vascular-targeting agent, in patients with solid tumors. Invest New Drugs 26, 159–167 (2008). https://doi.org/10.1007/s10637-008-9112-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-008-9112-9