Summary
Poly(ADP-ribose) synthetase inhibitor, INO-1001, is known to sensitize cells to radiation in vitro by inhibiting the repair of DNA damage. Recent evidence has suggested that PARP inhibition may also be a way of selectively targeting p53 deficient cancer cells. The present study tested INO-1001 for its in vivo effect on the chemoresponse of two p53 deficient tumors, human breast cancer MDA-MB-231 and murine mammary carcinoma MCa-K. Doxorubicin was used as the DNA damaging agent and tumor growth delay assay was used as the endpoint. Results showed that INO-1001 was highly effective in enhancing the anti-tumor effects of Doxorubicin for both MDA-MB-231 (EF = 1.88) and MCa-K (EF = 1.64). We conclude that PARP inhibitor INO-1001 has high potential for enhancing the anti-tumor effects of chemotherapy agents such as Doxorubicin against p53 deficient breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poly(ADP-ribose) polymerase [PARP, also termed poly(ADP-ribose) synthetase or PARS] is a nuclear enzyme involved in multiple cellular functions including DNA repair, maintenance of genomic integrity, and cell replication and differentiation (reviewed in [1, 2]). PARP functions as a sensor of DNA damage and a signaling molecule, binds to DNA strand breaks and catalyses the cleavage of NAD+ into nicotinamide and ADP-ribose. The role of PARP in improving cell survival after DNA damage is not fully understood, but its binding to DNA may initially stabilize DNA breaks protecting them from nuclease attack or recombination. However, this PARP-DNA binding is then released through auto-ADP ribosylation making DNA lesions available for DNA repair mechanisms.
Because PARP plays an important role in the repair of DNA strand breaks, including those induced by radiation and chemotherapeutic drugs, inhibitors of this enzyme have potential to improve cancer chemotherapy or radiotherapy [2, 3]. A number of PARP inhibitors have been shown to enhance radiation-induced cell killing, the effect of which was particularly pronounced when present in the post-irradiation period [4–11]. Earlier, commercially available PARP inhibitors, such as 3-aminobenzamide or nicotinamide, are characterized by incomplete inhibition of PARP activity and moreover they exhibit various non-specific effects [2], and as such they have limited utility as radiosensitizers. Recently, a number of highly effective and specific PARP inhibitors with low toxicity have been developed [2, 3], and have undergone testing for their radio (chemo) sensitizing effects. Our recent study demonstrated that one of these novel agents, INO-1001, strongly enhanced radiation sensitivity of a number of in vitro cell lines without exerting any intrinsic cytotoxicity on its own [12]. The radiosensitizing effect was higher in combination with fractionated than single dose radiation, which was consistent with the inhibition of repair from radiation damage as an underlying mechanism of radiosensitization.
PARP inhibitors have also been explored for their chemosensitizing activities, notably when combined with DNA damaging drugs such as alkylating agents and topoisomerase-inhibiting agents [13–18]. Most studies have been done in vitro using cancer cell lines of different histology types, where PARP inhibitors demonstrated ability to increase the number of DNA strand breaks and enhance cell cytotoxicity induced by chemotherapeutic agents. Importantly, this enhancing effect of PARP inhibitors appeared to be independent of the p53 status of tumor cells, suggesting that PARP inhibitors could be an efficient way to counteract resistance to chemotherapeutic agents in p53 mutant tumors [17, 18]. An illustrative example of this action is a recent observation that the PARP inhibitor ANI was highly effective in sensitizing p53-deficient cancer cells to doxorubicin-induced apoptosis [17]. Our present study assessed whether these potent in vitro enhancing effects of PARP inhibitors on doxorubicin-induced cell cytotoxicity can be translated to in vivo antitumor activity against p53 mutant tumors. We used the PARP inhibitor INO-1001, that in our earlier study showed strong enhancement of cell radiosensitivity [12], and two p53 mutant mammary carcinoma tumors, one human tumor xenograft and one a syngeneic mouse tumor.
Material and methods
Drugs
The catalytic activity of PARP was inhibited by the potent isoindolinone-based PARP inhibitor INO-1001 provided by Inotek Pharmaceuticals Corporation (Beverly, MA) [19, 20]. The compound was dissolved in 5% dextrose solution to a concentration of 5 mg/ml and injected i.p. at a volume of 1 ml per mouse for a dose of approximately 200 mg/kg. INO-1001 was given for three consecutive days: three times per day at 4-h intervals.Doxorubicin (DOXO; Bedford Labs, Bedford, OH) was obtained as a powder and dissolved in normal saline to a concentration of 0.8 mg/ml. The solution was injected i.v. at a volume of 0.01 ml per gram mouse body weight for a dose of 8 mg/kg.
Tumor cell lines and animals
The human breast cancer MDA-MB-231 was obtained from American Type Culture Collection; tumor cell suspensions were prepared from cells grown as monolayers in vitro. The MCa-K tumor, a mammary carcinoma that spontaneously arose in C3H mice, was in its seventh isotransplant generation when used. Tumor cell suspensions were prepared by mechanical disruption and enzymatic digestion of non-necrotic tumor tissue.
Sixty nude (nu–nu/Ncr) mice were used for the MDA-MB-231 study and 55 C3Hf/KamLaw mice were used for the MCa-K study. Mice were bred in our specific-pathogen free facility and were 3–4 months of age and weighed an average of 32 g at the start of the experiments. They were housed three to five per cage, exposed to 12-h light dark cycles, and given free access to sterilized pelleted food (Prolab Animal Diet, Purina Mills Inc., St. Louis, MO) and sterilized water. Animals were maintained in an American Association for Laboratory Animal Care approved facility, and in accordance with current regulations of the US Department of Agriculture and Department of Health and Human Services. The experimental protocol was approved by, and in accordance with, institutional guidelines established by the Institutional Animal Care and Use Committee.
Tumor implantation and anti-tumor efficacy studies
Solitary tumors were produced by inoculation of 5 × 106 MDA-MB-231 cells into the right hind leg of nude mice or 5 × 105 MCa-K cells into the right hind leg of C3H mice. When tumors grew to an average of 7.2 mm in diameter (range 7.0–7.7 mm), mice were given INO-1001 (200 mg/kg) or 5% dextrose solution only. The agents were injected for three consecutive days: three times per day at 4-h intervals. Doxorubicin was given i.v. as a single dose of 8 mg/kg 1 day after the first dextrose or INO-1001 treatment. On the day both INO-1001 and Doxorubicin were given, the PARP inhibitor was injected 5 min before DOXO. An additional group of mice was treated with Doxorubicin alone when the tumors (MCa-K) were 8 mm in diameter. Groups consisted of seven to eight mice with MCa-K tumors or three to five mice with MDA-MB-231 tumors.
Tumor growth delay was the endpoint used to determine anti-tumor efficacy of INO-1001 and irradiation. To obtain tumor growth curves, three mutually orthogonal diameters of tumors were measured two to three times/week with a vernier caliper, and the mean values were calculated. Mice were sacrificed when tumors grew to 14–15 mm. Regression and regrowth of tumors was assessed from the time of DOXO treatment, i.e. 24 h after initial treatment with dextrose or INO-1001. Tumor growth delay was expressed as the time in days for tumors in the INO-1001- and DOXO-treated groups to grow to 12 mm in diameter minus the time in days for tumors in the dextrose only control group to reach the same size. This was termed absolute growth delay (AGD). For groups treated with both INO-1001 and Doxorubicin, normalized growth delay (NGD) was determined as the time for tumors in the combined therapy group to grow to 12 mm minus time for tumors in the group treated with INO-1001 alone to grow to 12 mm. The enhancement factor (EF) was then determined by dividing NGD for the group receiving INO-1001 plus Doxorubicin therapy by the AGD for the group given Doxorubicin and dextrose only.
Results and discussion
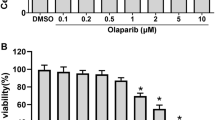
Mice bearing MCa-K or MDA-MB-231 tumors were treated with INO-1001, doxorubicin or both agents, and the effect of these agents on tumor growth was assessed by tumor growth delay shown in Table 1, Figs. 1 and 2. INO-1001 as a single agent had no significant effect on the growth of either MCa-K or MDA-MB-231 tumors. In contrast, doxorubicin significantly delayed the growth of both tumors, but was more effective in the treatment of MDA-MB-231 tumors (AGD of 13.1 ± 2.8 days compared to 4.5 ± 0.7 days for MCa-K tumors). When the two agents were combined, the effect on tumor growth was more than the additive effect of individual agents, implying that synergy had occurred. The AGD was 8.3 ± 0.7 days for MCa-K tumors and 24.3 ± 4.3 for MDA-MB-231 tumors. INO-1001 enhanced the antitumor efficacy of doxorubicin by a factor of 1.64 for MCa-K and by a factor of 1.88 for MDA-MB-231 tumors.
Effect of INO-1001 and Doxorubicin on the growth of MCa-K murine tumors. Mice bearing tumors in the right hind leg were treated with dextrose (open circle), INO-1001 (filled circle), doxorubicin (open diamond), dextrose plus doxorubicin (open triangle), or INO-1001 plus doxorubicin (filled triangle). Treatment with INO-1001 (200 mg/kg) or dextrose was initiated when tumors were an average diameter of 7.2 mm and was given i.p. three times a day for a total of 3 days. Doxorubicin (8 mg/kg i.v.) was administered as a single agent when tumors were 8 mm, or it was given to mice 24 h after the first INO-1001 or dextrose treatment
Effect of INO-1001 and Doxorubicin on the growth of MDA-MB-231 human tumor xenografts. Mice bearing tumors in the right hind leg were treated with dextrose (open circle), INO-1001 (filled circle), dextrose plus doxorubicin (open triangle), or INO-1001 plus doxorubicin (filled triangle). Treatment with INO-1001 (200 mg/kg) or dextrose was initiated when tumors were an average diameter of 7.3mm and was given i.p. three times a day for a total of 3 days. Doxorubicin (8 mg/kg i.v.) was injected 24 h after first INO-1001 or dextrose treatment
Our findings extend the observation of the ability of PARP inhibitors to increase in vitro doxorubicin-induced cell cytoxicity [17] to that of enhancing in vivo tumor response to doxorubicin. Importantly, both in vitro [17] and our in vivo findings showed that PARP inhibitors were effective against p53 mutant tumor cells. Tumor suppressor p53 is important in maintaining genomic instability and suppressing carcinogenesis. Normally functioning p53 gets activated after genotoxic stress and, depending on cell type, nature, and the extent of damage, activates different cellular responses including DNA repair, cellular senescence and apoptosis [21–23]. In malignant tumors, however, p53 is often mutated or functionally inactivated, rendering such tumors resistant to cytotoxic agents [21–23]. This resistance is attributed mainly to the inability of p-53 deficient cells to undergo apoptotic cell death when exposed to cytotoxic agents. The ability of PARP inhibitors to enhance doxorubicin-induced apoptosis in p53 deficient breast cancer cell lines involved other, p53-independent pathways in apoptosis induction [17]. Specifically, the PARP inhibitor ANI-induced apoptosis in these breast cancer cell lines was associated with decrease in mitochondrial potential, increase in cytochrome c release, association of the proapoptotic protein Bax with mitochondria and caspase 3 activation. It is possible that a similar mechanism was involved the enhancement of antitumor efficacy of doxorubicin induced by INO-1001 observed in the present study. Regardless of the mechanisms involved, the results of our study show that combining INO-1001, and likely other PARP inhibitors, with chemotherapeutic agents might be an effective means to treat p53 deficient cancers. However, studies using additional tumors both p53-mutant and -wild-type will be needed to confirm the conclusion derived from this initial investigation.
References
Althaus FR (1985) ADP-Ribosylation of Proteins. Springer, Berlin
Southan GJ, Szabo C (2003) Poly(ADP-ribose) polymerase inhibitors. Curr Med Chem 10(4):321–340
Beneke S, Diefenbach J, Burkle A (2004) Poly(ADP-ribosyl)ation inhibitors: promising drug candidates for a wide variety of pathophysiologic conditions. Int J Cancer 111(6):813–818
Lunee J, George M, Hedges M, Cramp W, Wish W, Hunt B (1984) Post-irradiation sensitization with the ADP-ribosyltransferase inhibitor 3-acetamidobenzamide. Br J Cancer 49:19–25
Brown D, Evans J, Brown J (1984) The influence of inhibitors of poly(ADP)polymerase on X-ray induced potentially lethal damage repair. Br J Cancer 49:27–34
Ben-Hur B, Utsumi H, Elkind M (1984) Inhibitors of poly(ADP-ribose) synthesis enhance X-ray killing of log phase Chinese hamster cells. Radiat Res 97:546–555
Ben-Hur E (1984) Involvement of poly (ADP-ribose) in the radiation response of mammalian cells. Int J Radiat Biol 46(6):659–671
Ueno AM, Tanaka O, Matsudaira H (1984) Inhibition of gamma-ray dose-rate effects by D2O and inhibitors of poly(ADP-ribose) synthetase in cultured mammalian L5178Y cells. Radiat Res 98(3):574–582
Thraves P, Mossman KL, Brennan T, Dritschilo A (1985) Radiosensitization of human fibroblasts by 3-aminobenzamide: An inhibitor of poly(ADP-ribosylation). Radiat Res 104(2 Pt 1):119–127
Kelland LR, Burgess L, Steel GG (1987) Radiation damage repair capacity of a human germ-cell tumour cell line: inhibition by 3-aminobenzamide. Int J Radiat Biol Relat Stud Phys Chem Med 51(2):227–241
Arundel-Suto CM, Scavone SV, Turner WR, Suto MJ, Sebolt-Leopold JS (1991) Effect of PD 128763, a new potent inhibitor of poly(ADP-ribose) polymerase, on X-ray-induced cellular recovery processes in Chinese hamster V79 cells. Radiat Res 126(3):367–371
Brock WA, Milas L, Bergh S, Lo R, Szabo C, Mason KA (2004) Radiosensitization of human and rodent cell lines by INO-1001, a novel inhibitor of poly(ADP-ribose) polymerase. Cancer Lett 205(2):155–160
Bowman KJ, White A, Golding B, Griffin R, Curtin N (1998) Potentiation of anti-cancer agent cytotoxicity by the potent poly(ADP-ribose) polymerase inhibitors NU1025 and NU1064. Br J Cancer 78(10):1269–1277
Delaney CA, Wang LZ, Kyle S, White AW, Calvert AH, Curtin N, Durkacz B, Hostomsky Z, Newell D (2000) Potentiation of temozolomide and topotecan growth inhibition and cytotoxicity by novel poly(adenosine diphosphoribose) polymerase inhibitors in a panel of human tumor cell lines. Clin Cancer Res 6(7):2860–2867
Skalitzky D, Marakovits J, Maegley K, Ekker A, Yu X, Hostomsky Z, Webber S, Eastman B, Almassy R, Li J, Curtin N, Newell D, Calvert A, Griffin R, Golding B (2003) Tricyclic benzimidazoles as potent poly(ADP-ribose) polymerase-1 inhibitors. J Med Chem 46(2):210–213
Calabrese CR, Almassy R, Barton S, Batey MA, Calvert AH, Canan-Koch S, Durkacz BW, Hostomsky Z, Kumpf RA, Kyle S, Li J, Maegley K, Newell DR, Notarianni E, Stratford IJ, Skalitzky D, Thomas HD, Wang LZ, Webber SE, Williams KJ, Curtin NJ (2004) Anticancer chemosensitization and radiosensitization by the novel poly(ADP-ribose) polymerase-1 inhibitor AG14361. J Natl Cancer Inst 96(1):56–67
Munoz-Gamez JA, Martin-Oliva D, Aguilar-Quesada R, Canuelo A, Nunez MI, Valenzuela MT, Ruiz de Almodovar JM, De Murcia G, Oliver FJ (2005) PARP inhibition sensitizes p53-deficient breast cancer cells to doxorubicin-induced apoptosis. Biochem J 386(Pt 1):119–125
Madhusudan S, Middleton M (2005) The emerging role of DNA repair proteins as predictive, prognostic and therapeutic targets in cancer. Cancer Treat Rev 31(8):603–617
Xiao CY, Chen M, Zsengeller Z, Szabo C (2004) Poly (ADP-ribose) polymerase contributes to the development of myocardial infarction in diabetic rats and regulates the nuclear translation of apoptosis-inducing factor. J Pharmacol Exp Ther 310 (2):498–504
Xiao CY, Chen M, Zsengeller Z, Li H, Kiss L, Kollai M, Szabo C (2005) Poly (ADP-Ribose) polymerase promotes cardiac remodeling, contractile failure, and translocation of apoptosis-inducing factor in a murine experimental model of aortic banding and heart failure. J Pharmacol Exp Ther 312(3):891–898
Oren M (2003) Decision making by p53: life, death and cancer. Cell Death Differ 10(4):431–442
Vogelstein B, Lane D, Levine A (2000) Surfing the p53 network. Nature 408(6810):307–310
Wahl GM, Carr AM (2001) The evolution of diverse biological responses to DNA damage: insights from yeast and p53. Nat Cell Biol 3(12):E277–286
Acknowledgement
Sponsored by a Laboratory Study Agreement with Inotek Pharmaceuticals Corp and NIH Grants CA06294 and CA16672.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mason, K.A., Valdecanas, D., Hunter, N.R. et al. INO-1001, a novel inhibitor of poly(ADP-ribose) polymerase, enhances tumor response to doxorubicin. Invest New Drugs 26, 1–5 (2008). https://doi.org/10.1007/s10637-007-9072-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-007-9072-5