Abstract
Purpose
Objective assessment of visual acuity (VA) is possible with VEP methodology, but established with sufficient precision only for vision better than about 1.0 logMAR. We here explore whether this can be extended down to 2.0 logMAR, highly desirable for low-vision evaluations.
Methods
Based on the stepwise sweep algorithm (Bach et al. in Br J Ophthalmol 92:396–403, 2008) VEPs to monocular steady-state brief onset pattern stimulation (7.5-Hz checkerboards, 40% contrast, 40 ms on, 93 ms off) were recorded for eight different check sizes, from 0.5° to 9.0°, for two runs with three occipital electrodes in a Laplace-approximating montage. We examined 22 visually normal participants where acuity was reduced to ≈ 2.0 logMAR with frosted transparencies. With the established heuristic algorithm the “VEP acuity” was extracted and compared to psychophysical VA, both obtained at 57 cm distance.
Results
In 20 of the 22 participants with artificially reduced acuity the automatic analysis indicated a valid result (1.80 logMAR on average) in at least one of the two runs. 95% test–retest limits of agreement on average were ± 0.09 logMAR for psychophysical, and ± 0.21 logMAR for VEP-derived acuity. For 15 participants we obtained results in both runs and averaged them. In 12 of these 15 the low-acuity results stayed within the 95% confidence interval (± 0.3 logMAR) as established by Bach et al. (2008).
Conclusions
The fully automated analysis yielded good agreement of psychophysical and electrophysiological VAs in 12 of 15 cases (80%) in the low-vision range down to 2.0 logMAR. This encourages us to further pursue this methodology and assess its value in patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A very frequent referral diagnosis to many electrodiagnostic laboratories in ophthalmology is unexplained visual loss, possibly with a non-organic component [1]. This represents a multifaceted and complex gamut, from malingering to conversion syndrome (historically called hysterical vision loss), and is referred to neutrally as “functional visual loss.” While visual evoked potentials (VEPs) were previously employed to assist in the assessment of these cases via the estimation of an objective visual acuity (VA) measure (e.g., [2, 3] reviewed in [4, 5]), these were mainly directed at an VA range better than ≈ 1.0 logMAR, exception: [6]. However, visual acuities markedly worse than that are of particular interest, as VA values in this range of visual impairment include categories with implications for legal consequences and social support. For example (arranged by increasing “laxness”),
-
In Germany the VA threshold for “legal blindness” is ≤ 0.02VAdecimal ≡ ≤ 1/50VASnellen ≡ ≥ 1.7 logMAR
-
The American foundation for the Blind [7] defines “legal blindness” as a VA of ≤ 20/200VASnellen ≡ ≤ 0.1VAdecimal ≡ ≥ 1.0 logMAR
-
The World Health Organization (WHO) defines the following H54.x thresholds [8]:
“Moderate visual impairment” < 20/70VASnellen ≡ < 0.3VAdecimal ≡ > 0.5 logMAR
“Severe visual impairment” < 20/200VASnellen ≡ < 0.1VAdecimal ≡ > 1.0 logMAR
Such classifications would benefit from an objective assessment of VA in the low-vision range, e.g., based on visual evoked potentials. Previously, the Bach group devised a VEP-based VA estimation (“Freiburg Acuity VEP,” [5]) based on a fully automated analysis of responses to stimuli progressing stepwise through different check sizes that yields an estimate of VA with confidence limits. They arrived at an algorithm (the “stepwise heuristic algorithm”) that automatically selects appropriate values from the check size tuning function which accommodates the frequent occurrence of an “amplitude notch” for some combinations of spatial and temporal frequencies [9,10,11,12]. The algorithm derives a limiting spatial frequency (SF0) via an appropriate scaling factor, which serves as a surrogate measure of VA (VAdecimal ≈ SF0/17.6 cpd). One important feature of their approach is the derivation of a noise-corrected “true” response amplitude [13,14,15] and the automatic assessment of the significance of each response [13]. This removes the effect of interindividual noise variability and may explain that a constant scaling factor holds for the entire range (more on this in Discussion). While this approach covered a fairly wide VA range [from decimal 0.2VAdecimal to 2.0VAdecimal (= 0.7 logMAR to −0.3 logMAR)], it omitted visual acuities below 0.2VAdecimal (0.7 logMAR).
As there is a lack of systematic investigations in the range of legal blindness, the current study was designed to probe the possibility to obtain VEP correlates of VA in the low-vision range, down to a VA of 0.02VAdecimal (= 1.7 logMAR), i.e., legal blindness in Germany. Specifically, we aimed to test whether the range of the “Freiburg Acuity VEP” could be extended accordingly. For a proof of principle the study population would ideally be required to meet the following rather specific criteria: (1) It should cover a narrow VA range around 1.7 logMAR, (2) the affected individuals should have the same cause of VA reduction, in order to reduce potentially confounding disease-specific effects, and (3) it should have good compliance. We here addressed this challenge by simulating reduced VA in participants with healthy vision and normal VA by viewing through diffusers.
Methods
Participants
In total 24 participants with normal (corrected) VA (≥ 1.0VAdecimal) were included in the experiment (see Table 1). Only one eye of each participant was assessed, in two participants without artificial visual acuity reduction and in the remaining 22 with acuity reduction. The study followed the tenets of the Declaration of Helsinki [19]. The protocol was approved by the Ethics Committee of the University of Magdeburg, Germany, and informed consent was obtained from the participants.
Only two participants were measured with their normal visual acuity as sufficient reference data were available from our previous study [5]. For 22 participants visual acuity was artificially reduced by scatter transparencies [image degradation by Bangerter occlusion foils was not sufficient, so we used frosted document transparencies (Art Nr. 10916997, Herlitz PBS AG, Berlin, Germany)] for part of the recordings. One disadvantage of scatter transparencies is some inhomogeneity across the transparency, so care was taken that the same head posture was kept for VA and VEP measurements. Uncrowded psychophysical VA was measured using the automated “Freiburg Visual Acuity and Contrast Test (FrACT)” [20], a Landolt-C-based test whose results are equivalent to ETDRS [21], at the same distance as the VEP stimulation (114 cm for clear vision and 57 cm for degraded vision). Psychophysical visual acuities were measured at least twice for each participant. For degraded vision the decimal acuities (average across both repetitions) ranged from 1.92 to 2.18 logMAR, average across subjects 2.06 logMAR (0.01VAdecimal).
Stimuli
Checkerboard stimuli were presented in brief onset mode, three frames = 40 ms on and seven frames = 93 ms off, corresponding to 7.5 Hz. Space-averaged mean luminance was 45 cd/m2. The contrast was set to 40% by the following rationale: The contrast transfer function of the VEP typically saturates early (e.g., [22]), so a medium contrast is sufficient to evoke full amplitude. Furthermore, with this rather low contrast the luminance values do not approach extreme values and gamma correction of the display [23] is easily achieved. Thus, luminance artifacts, always a danger with onset stimuli, are more easily avoided [24].
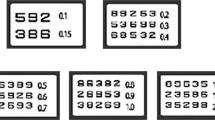
Two sets of check sizes were used: one for the normal VA range (“Acuity_1”) and one for the low-vision range (“Acuity_3”). For Acuity_1 the check sizes were selected in six logarithmically equidistant steps from 0.048° to 0.385°, constrained by monitor resolution: 2 × 2 pixels for the smallest check size, then 3 × 3, 4 × 4, 7 × 7, 10 × 10, and 16 × 16, the latter corresponding to 0.385° at the observation distance of 114 cm. For Acuity_3 the check sizes were selected in eight logarithmically equidistant steps from 0.52° to 8.9°; again the values originate from integer pixel numbers nearest to the log scale. For seven participants (recording numbers #195 and higher, see Table 1) a small ninth check size was added (0.087°), which should be invisible in low vision. This enabled us to assess the possibility of a luminance artifact, as no significant responses should be obtained for this condition in low vision. The exact check sizes are given in Fig. 1, left of the traces.
Three participants in three columns. Left per column: VEP traces, right: frequency spectra (1–100 Hz). Check size increases from top to bottom and is given in bold left of the traces. The left column represents data from participant #99 with full VA (−0.26 logMAR). For the participants in the center and right column VA was artificially reduced to 2.09 and 2.16 logMAR. The right column is one of the seven cases, participant #210, with an additional small check size to assess possible luminance artifacts. Amplitude scales are constant along columns, but differ between subjects. The vertical gray bar between columns 1 and 2 indicates that the check sizes differ; otherwise, the traces are aligned for check size. Significant responses are indicated by yellow highlighting. #99 shows strong responses (eight peaks in the 1066-ms epoch), corresponding to a strong 7.5-Hz line in the spectrum for all check sizes. For the two low-vision examples (#52 and #210) only the three or two largest check sizes evoke significant responses. The responses frequently contain alpha activity and some of 50-Hz (mains) interference, which is not visible in the traces as they have been filtered with a digital 45 Hz low pass for display purposes
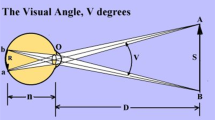
For analysis, the check size was converted to spatial frequency, considering that the dominant spatial frequency is at 45° to the check orientation, using the formula [25]:
Thus, the smallest check size of 0.048° contains the dominant spatial frequency of 14.7 cpd. Each check size was presented for ten sweeps of 1066 ms length each; then, the next check size was followed. After the largest check size, the stimulus sequence repeated. Six such cycles thus resulted in 60 sweeps or 480 onsets per check size. This interleaved presentation for the stepwise sweep reduces the influence of sequential artifacts (e.g., fatigue). The timing of the stimulation frequency and the sweep length was designed to contain only integer relations. There were an integer number of onsets per sweep (eight onsets), and this prevented frequency overspill in the subsequent Fourier analysis [26].
Recording
The EEG was recorded with gold cup electrodes at Oz, LO and RO, referenced to FPz. LO and RO were 15% (of the half-head circumference) left and right of Oz, following Mackay et al. [27]. Signals were amplified (50,000×), analog filtered in the range of 1–100 Hz, and digitized at a rate of 1 kHz with 12-bit resolution. Averaging was arranged to capture exactly eight onsets in 1066-ms epochs. Stimulation and recording employed the “EP2000” Evoked Potentials System [28]. This program presented the stimuli while it stepped through the check size sequence, acquired the signals, displayed them online, checked for and discarded artifacts (beyond an amplitude window of ± 140 µV), repeated discarded trials, displayed online averages and online Fourier analysis results, and saved the records for off-line processing. To ensure subject alertness random digits from 0 to 9 appeared in random intervals of the screen and were reported via button press by the subjects. When the VA was low, the participants could not recognize the digit, but could perceive an event at the fixation position, which they reported. In order to assess the reproducibility of the electrophysiological measures obtained the protocol was run twice for each participant.
Analysis
The resulting steady-state VEPs were subjected to Fourier analysis. For each check size (spatial frequency SF) the following measures were obtained: the magnitude A(SF) at the stimulation frequency (7.5 Hz) and a noise estimate, i.e., the average of the response of the two neighboring frequencies (6.5 and 8.5 Hz). Based on these the noise-corrected “true” amplitude A *(SF) [13,14,15] and the significance of this response p(SF) [13] were calculated. The resultant data set of A *(SF) and p(SF) constitutes the input to an algorithm that calculates a measure that can be related to the VA obtained by psychophysical means by means of a stepwise heuristic algorithm as described previously [5]. This stepwise heuristic algorithm is designed to find an optimal range for a regression of A * versus log(SF) to be extrapolated to zero, thus yielding SF0 (for details and the rule set for the algorithm see [5]). It must be noted that, due to the nature of the algorithm, there can be failures to determine SF0. Thus, the stepwise heuristic algorithm yields a value for SF0, or failure for each recording. The SF0 values were previously correlated with the respective psychophysically derived VA [5]. Ultimately, for VA assessment, this correlation was applied inversely and appropriate confidence bands were calculated. As a consequence, VEP acuity is obtained by dividing SF0 by 17.6. Using this dimensionless number 17.6 (a rounded value of the actual result) the resulting dimension is “one over degrees,” which, expressed in minutes of arc, immediately yields a decimal VA. In logMAR terms the VEP acuity is calculated as log10(17.6/SF0).
Results
For a qualitative assessment of the check size dependence of the VEPs typical sets of recordings are shown in Fig. 1. Using the 2008 acuity VEP parameters [5] data from subject #99, i.e., with clear vision, are depicted; for the extended acuity VEP parameters, i.e., with larger check sizes, data from two participants with degraded vision (#52 and #210) are shown. The traces on the left represent amplitude versus time, and to their right the corresponding magnitude spectra after Fourier transform are shown. For subject #99, i.e., with clear vision, the response at the stimulation frequency of 7.5 Hz is clearly visible and significant (p < 5%) for all check sizes. For the subjects #52 and #210 only the three or two largest check sizes, respectively, evoke significant responses at 7.5 Hz.
The tuning curves for the responses at 7.5 Hz from Fig. 1 are presented in Fig. 2. In addition to the data in Fig. 1 the tuning curves are shown for a repeat run in each participant (run 2) to give an impression of the reproducibility. The VEP-based visual acuities are derived from these tuning curves as the point where the linear regression line crosses the abscissa, SF0, multiplied with a previously determined conversion factor (17.6) [5]. Following the stepwise heuristic algorithm, for #99 the regression starts on the right with the rightmost point and extends to low spatial frequencies. The zero crossing for #99 (clear vision) is at SF0 = 32.1 and 28.2 cpd. Applying the above conversion factor, as detailed in Methods, these SF0 result in a VEP visual acuity of −0.2 logMAR (1.6 VAdecimal) for both runs. For #52 and #210 (degraded vision) the check range tested is, in adaptation to the smaller psychophysical VA, shifted to larger checks than for #99. The zero crossing is at SF0 = 0.3 and 0.4 cpd for #52 and at 0.2 and 0.3 cpd for #210, for runs 1 and 2, respectively. This results in a VA of 1.75 and 1.61 logMAR (0.018 and 0.025 VAdecimal) for #52, and a VA of and 1.92 and 1.81 logMAR (0.012 and 0.015 VAdecimal) for #210.
Tuning curves for the VEPs shown in Fig. 1 (run 1) and a repetition (run 2). The noise-corrected response magnitude at 7.5 Hz is plotted versus the logarithm of the dominant spatial frequency of the checkerboard stimulus. A significant response is indicated by stars, circles otherwise. The thick regression lines are based on the “stepwise heuristic algorithm” [5]. In these examples the extrapolation to zero amplitude yields a spatial frequency (SF0) of 32.1 and 28.2 cpd for #99 (runs 1 and 2, respectively) corresponding, in both cases, to a VA of −0.2 logMAR; for the degraded condition lower SF0s are determined, corresponding to a VA of 1.75 and 1.61 logMAR (#52), and 0.2 and 0.3, corresponding to a VA of 1.92 and 1.81 logMAR (#210)
Beyond these examples we found the following in our experimental group with reduced VA: In 15 of 22 (68%) participants with artificially degraded visual acuity both runs of the heuristic algorithm indicated a “valid” VA, and in 20 of 22 (91%) participants at least one run resulted in a valid VA. An account of the reproducibility of these results and the corresponding psychophysical VAs is given in Fig. 3, where psychophysical and VEP visual acuities are plotted for the two consecutive runs. As expected the two participants with clear vision reached clearly better VAs for both psychophysics and VEPs than the participants with degraded vision. While it is evident that the reproducibility is greater for the psychophysical than for the electrophysiological measures, it should be noted that all VA measures for the degraded condition clearly fall in the low-vision range.
Test–retest plot for psychophysical (green dots) and VEP-based VA (red stars). The two participants with clear vision reached high visual acuities (smaller logMAR values, note inverted axis) for both psychophysics and VEPs. There is less scatter for the psychophysical than for the electrophysiological measures. The lines parallel to the gray identity line represent the 95% limits of agreement (LOA) for the two VA approaches (psychophysical: dotted green, and VEP: dashed red)
Finally, the relation of the psychophysical and electrophysiological VAs was analyzed for the 15 participants with degraded vision (i.e., VAs around 2 logMAR) for whom VEP-based VA estimates were obtained for both repetitions. These results are based on the average measures from both repetitions and are given in Fig. 4. For comparison the results reported in [5] are added (with smaller symbols). In total, 12 (80%) of the 15 reduced vision VAs lie within the 95% confidence interval determined in [5] for their higher VA range. There appears to be a slight overall shift to higher acuities for the VEP compared to the psychophysics by about 0.2 logMAR.
Relation of psychophysical and electrophysiological VAs (large blue symbols, average of two runs; n = 15) in comparison with previously published data [5], small gray symbols. In total 12 of the 15 participants with a VA degraded to ≈ 2 logMAR lie within the 95% CI determined in [5], three are outside, with a VEP-based VA that is better than the psychophysical VA
Discussion
We extended the Freiburg paradigm for VEP-based objective VA assessment to lower acuity ranges by using a set of larger check sizes without any other changes. Indeed, even for an acuity as poor as ≈ 2.0 logMAR a significant brief onset VEP can be evoked if check sizes up to 9° are employed. Thus, in 20 of 22 eyes (91%) the automatic analysis procedure indicated a “valid” result in at least one of the two runs per eye, and in 15 of 22 (68%) both runs returned a valid result. In 12 of the 15 eyes with artificially reduced acuity the VEP result lay within the 95% confidence interval established for the original paradigm. Those three that lay outside represented better VA reported by the VEP analysis than obtained psychophysically.
Operating range of the heuristic VEP algorithm
We were surprised by the robustness of the heuristic VEP algorithm in largely coping with acuities that are more than a factor of 10 lower than the range for which it was originally designed (see Fig. 4). However, the data suggest that the linear relation between log(dominant spatial frequency) and logMAR acuity seen for acuities better than 0.5 logMAR (upper right in Fig. 4) is partially lost for really low acuities (Fig. 4, bottom left). Maybe this is not so surprising, given that at 2.0 logMAR the corresponding optotype has a diameter of ≈ 8°, challenging the very concept of acuity. Obviously, given enough calibration data, the correction factor might be made variable across the acuity range. However, as yet we see no strong reason why the linear relationship between check size and VA should vary and plan further experiments to explore this region.
Nomenclature in VEP-based objective acuity assessment and acuity calculation
The term “sweep VEP” seems to have been coined first by Tyler et al. [16] where indeed a continuous sweep of a square wave grating’s spatial frequency was presented on an oscilloscope type of display. These and other authors later replaced this with a “stepwise sweep” of discrete spatial frequencies or check size, usually keeping the term “sweep VEP.” The term still implies a monotonous succession of the spatial parameter. Other authors used “bracketing” based on online response analysis [6] and avoided the term “sweep.” We here avoid the term “sweep” as well, although the interleaved check size sequences are monotonic.
Another issue in the nomenclature of VEP acuity is the relation of the (dominant) spatial frequency of the stimulus to the psychophysical acuity. In psychophysics 30 cpd is equated to an acuity 20/20 Snellen or 1.0 decimal so that VA[logMAR] = log10(threshold spatial frequency/30 cpd) [1]. For VEP-based thresholds using 30 cpd as denominator sometimes seems to fit, but frequently not. For a nice literature discussion of this aspect see [4, Fig. 4], which shows that the factor for converting VEP threshold to VA changes across the acuity range. The latter is undesirable and requires extensive reference data to determine VA acuities. In the present paper we confirmed a roughly constant factor across the wide range of 2.5 log units, i.e., a factor of ≈ 17.6, clearly smaller than 30. However, we are unsurprised that the denominator in equation [1] is smaller than 30, and reasons for this include:
-
Lower contrast for the VEP stimulus (rationale in Methods, Stimuli), whereas psychophysical acuity is assessed with full contrast.
-
Instability of accommodation. Accommodation tends to vary markedly on a tenths of seconds time scale with high interindividual variability, ± 1–3 D were found during mfVEP recording [17]. With a typical summation time for 100 ms for psychophysical acuity [18] brief perfect accommodation can serve psychophysical acuity, whereas the prolonged recording time of several minutes averages perfect and suboptimal accommodation, leading on average to a degraded stimulus and consequent lower acuity estimates.
Transfer to patient applications
It must be noted that, to provide proof of principle in the present study, we simulated low vision in the study participants with normal vision to guarantee fully controlled conditions. As evident from tests with the original acuity VEP paradigm for the upper acuity range [5], the correlation of VEP acuity and psychophysical acuity becomes less tight for data from patients as compared to healthy controls with simulated acuity reductions. Consequently the next step to establish objective low visual acuity testing for clinical use is to test our low-vision acuity VEP adaptation in relevant patient groups. Our pilot measurements targeting this issue indicate that the two acuity estimates, i.e., from VEP and from psychophysics, might correspond better in some patients, but less in others, with a tendency of an overestimation of the VEP acuities in the latter. Such variability might be due to different disease mechanisms causing the visual acuity loss as already reported for the initial acuity VEP [29]. Finally, it must be underscored that the VEP paradigm described here is specifically adapted to the low-vision range. Consequently it is expected to mis-estimate, likely underestimate, higher acuities, i.e., those that fall outside the low-vision range (> 0.3VAdecimal, i.e., < 0.5 logMAR). Systematic studies addressing these issues will help to identify the application spectrum of the low-vision acuity VEP and to ultimately provide a comprehensive framework of objective low-vision assessment.
All in all, we see our findings as a promising result, suggesting that even around 2.0 logMAR a low VEP-based VA outcome indeed can be taken as evidence that acuity is low indeed, and after having made sure that optics, especially accommodation, and fixation are not a cause of concern.
References
Holder GE (2006) Electrodiagnostic testing in malingering and hysteria. In: Heckenlively J, Arden G (eds) Principles and practice of clinical electrophysiology of vision. MIT Press, Cambridge, London, pp 637–641
Katsumi O, Arai M, Wajima R et al (1996) Spatial frequency sweep pattern reversal VER acuity vs Snellen visual acuity: effect of optical defocus. Vis Res 36:903–909
Arai M, Katsumi O, Paranhos FR et al (1997) Comparison of Snellen acuity and objective assessment using the spatial frequency sweep PVER. Graefes Arch Clin Exp Ophthalmol 235:442–447
Ridder WH III (2004) Methods of visual acuity determination with the spatial frequency sweep visual evoked potential. Doc Ophthalmol 109:239–247
Bach M, Maurer JP, Wolf ME (2008) Visual evoked potential-based acuity assessment in normal vision, artificially degraded vision, and in patients. Br J Ophthalmol 92:396–403. doi:10.1136/bjo.2007.130245
Mackay AM, Bradnam MS, Hamilton R et al (2008) Real-time rapid acuity assessment using VEPs: development and validation of the step VEP technique. Investig Ophthalmol Vis Sci 49:438–441
American Foundation for the Blind (2008) Key definitions of statistical terms—American Foundation for the Blind. http://www.afb.org/info/blindness-statistics/key-definitions-of-statistical-terms/25. Accessed 17 Dec 2016
World Health Organisation (2016) ICD-10 Version:2016. http://apps.who.int/classifications/icd10/browse/2016/en#/H54.3. Accessed 3 Jun 2017
Tyler C, Apkarian P (1982) Properties of localized pattern evoked potentials. In: Bodis-Wollner I (ed) Evoked Potentials. The New York Academy of Sciences, New York
Strasburger H (1987) The analysis of steady state evoked potentials revisited. Clin Vision Sci 1:245–256
Bach M, Joost W (1989) VEP vs spatial frequency at high contrast: Subjects have either a bimodal or single-peaked response function. In: Kulikowski J, Dickinson C, Murray I (eds) Seeing contour and colour. Pergamon Press, Oxford, pp 478–484
Parry NR, Murray IJ, Hadjizenonos C (1999) Spatio-temporal tuning of VEPs: effect of mode of stimulation. Vis Res 39:3491–3497
Meigen T, Bach M (1999) On the statistical significance of electrophysiological steady-state responses. Doc Ophthalmol 98:207–232
Norcia AM, Tyler CW, Hamer RD, Wesemann W (1989) Measurement of spatial contrast sensitivity with the swept contrast VEP. Vis Res 29:627–637
Norcia AM, Clarke M, Tyler CW (1985) Digital filtering and robust regression techniques for estimating sensory thresholds from the evoked potential. IEEE Eng Med Biol Mag 4:26–32
Tyler CW, Apkarian P, Levi DM, Nakayama K (1979) Rapid assessment of visual function: an electronic sweep technique for the pattern visual evoked potential. Investig Ophthalmol Vis Sci 18:703–713
Jägle H, Zobor D, Brauns T (2010) Accommodation limits induced optical defocus in defocus experiments. Doc Ophthalmol 121:103–109. doi:10.1007/s10633-010-9237-y
Heinrich SP, Krüger K, Bach M (2010) The effect of optotype presentation duration on acuity estimates revisited. Graefes Arch Clin Exp Ophthalmol 248:389–394. doi:10.1007/s00417-009-1268-2
World Medical Association (2000) Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Med Assoc 284:3043–3045
Bach M (2007) The freiburg visual acuity test—variability unchanged by post hoc re-analysis. Graefes Arch Clin Exp Ophthalmol 245:965–971
Bach M (1996) The freiburg visual acuity test—automatic measurement of visual acuity. Optom Vis Sci 73:49–53
Heinrich TS, Bach M (2001) Contrast adaptation in human retina and cortex. Investig Ophthalmol Vis Sci 42:2721–2727
Bach M, Meigen T, Strasburger H (1997) Raster-scan cathode-ray tubes for vision research—limits of resolution in space, time and intensity, and some solutions. Spat Vis 10:403–414
Odom JV, Bach M, Brigell M et al (2016) ISCEV standard for clinical visual evoked potentials: (2016 update). Doc Ophthalmol 133:1–9. doi:10.1007/s10633-016-9553-y
Fahle M, Bach M (2006) Basics of the VEP. In: Heckenlively J, Arden G (eds) Principles and Practice of clinical electrophysiology of vision. MIT Press, Cambridge, London, pp 207–234
Bach M, Meigen T (1999) Do’s and don’ts in Fourier analysis of steady-state potentials. Doc Ophthalmol 99:69–82
Mackay AM, Hamilton R, Bradnam MS (2003) Faster and more sensitive VEP recording in children. Doc Ophthalmol 107:251–259
Bach M (2007) Freiburg evoked potentials. http://www.michaelbach.de/ep2000.html. Accessed 19 Aug 2013
Wenner Y, Heinrich SP, Beisse C et al (2014) Visual evoked potential-based acuity assessment: overestimation in amblyopia. Doc Ophthalmol 128:191–200. doi:10.1007/s10633-014-9432-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent–licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Statement of human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Hoffmann, M.B., Brands, J., Behrens-Baumann, W. et al. VEP-based acuity assessment in low vision. Doc Ophthalmol 135, 209–218 (2017). https://doi.org/10.1007/s10633-017-9613-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-017-9613-y