Abstract
Color vision was examined by psychophysical tests and photopic color full-field electroretinography (ERG) in formerly preterm children, and compared with those of full-term children. In a prospective case–control study, 25 patients with a history of preterm birth 7–14 years of age were divided into three groups: group I, laser-treated retinopathy of prematurity [ROP] (n = 7); group II, spontaneously regressed ROP (n = 8); group III, no ROP (n = 10). Age-matched full-term born children comprised the control group (n = 8). Color vision was assessed by Fansworth D15 and Lanthony desaturated D15 tests. The cone function was tested using photopic full-field ERG. Besides the ISCEV standard stimuli, blue light on amber background was also used (S-cone ERG). The correlation between ERG parameters and prematurity or ROP was determined. We found no significant differences between any patient group and the control group in the results of the psychophysical tests, and implicit times of the ERG responses. The ERG b-wave amplitudes were significantly lower in group I (laser-treated ROP) compared to controls, for 2 of 4 stimulus conditions i.e. the standard (P = 0.028) and S-cone (P = 0.017) single flash ERGs. The general estimating equation model statistics found a significant effect of prematurity on the b-wave amplitudes (P = 0.025, standard, P = 0.014, S-cone ERG). A slightly reduced photopic ERG b-wave amplitude may be associated with prematurity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infants born at less than 32 weeks’ gestation are at high risk of retinopathy of prematurity (ROP), myopia, amblyopia, strabismus, and optic nerve abnormalities [1–3] related to the degree of prematurity [4] and the presence of cerebral damage. [5] These children have also been reported to have an increased long-term incidence of color vision [6] and contrast sensitivity impairments [3] unrelated to major ocular disease or cerebral damage.
Since the first hypothesis of tritan defects in preterm born infants by Abramov [6] several studies investigated color vision in children with history of preterm birth. The results of the psychophysical tests are controversial [6–9]. However in the CRYO-ROP study, with pseudoisochromatic plates, the investigators found an increased occurrence of blue-yellow deficits in children born before term, which was not related to birth weight, gestational age or severity of ROP, and showed no correlation with cryotherapy treatment. A relationship was observed only with visual acuity [10].
ERG studies have shown that ROP has an effect on the photoreceptors and post receptoral retina that persist even after its active phase. The late-maturing central retina and particularly the rod outer segments in the macula, appear to be vulnerable to these effects. Subtle deficits also occur in peripheral retinal function and persist into adolescence and early adulthood [11–14]. According to Fulton et al., ROP has less effect on the cone than on the rod photoresponses suggesting that cones are more resistant to the ROP disease process [15].
In this study, we examined whether an objective method (photopic full-field ERG with blue light stimuli on amber background), can detect a selective alteration in the functioning of the blue-cone system in preterm born children compared to age matched full term born controls.
Methods
This study was approved by the local human research ethics committee (TUKEB 101/2006; Semmelweis University, Budapest, Hungary) and is in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants’ parents or guardians. Parents or guardians stayed with their children throughout the procedure. This prospective case–control study included formerly preterm children 7–14 years of age who had received treatment and follow-up at our department. Their data were then compared to those collected from healthy, age–matched children born at full term. Both eyes of each control and each formerly preterm subject were examined. When both eyes of a subject were eligible for the study, one eye was randomly selected for statistical analysis. An eye was eligible for this study if it had a normal-appearing posterior pole and its best corrected visual acuity was 1.0 (decimal scale). The birth weight and the gestational age at birth for the groups are presented in Table 1.
Subjects
Subjects with a history of preterm birth
Patients were excluded from the study if they had nystagmus, or a history of cerebral damage. Eyes with residua of ROP (i.e., macular dragging, macular fold, partial retinal detachment involving the macula, or total retinal detachment), amblyopia, or myopia higher than –3.5 D spherical equivalent were also excluded. Patients were divided into three groups following the stage of ROP found during the acute phase [16]. One eligible eye from each subject chosen at random was selected and enrolled in each group.
Group I: Laser-treated patients
Both eyes of the patients underwent argon blue-green or 810-nm diode laser treatment for stage-3 threshold ROP. Laser coagulation was performed by using indirect binocular ophthalmoscopy. 14 eyes of 7 children were examined, 10 eyes were eligible, and 7 eyes were included after randomization.
Group II: Patients with spontaneously regressed ROP
Higher stages than stage 1 or 2 ROP were not documented in the acute phase within a few months of birth. 8 patients responded, 12 eyes matched with the enrollment criteria, 8 eyes were included after randomization.
Group III: Patients without ROP
No ROP was documented during the neonatal period. Twenty eyes of 10 patients were checked; 18 eyes were eligible, 10 eyes were included after randomization.
Term born control subjects
Group IV
All control subjects were born at full term, 7–14 years of age, generally healthy, with no ocular disease. (8 children, 16 eligible eyes, 8 randomly selected eyes).
Ophthalmic assessment included the following steps in order. Best corrected visual acuity was measured with Snellen chart adjusted at 5 m. The Lang test was used to screen amblyopia. Refraction and keratometry readings were obtained after cycloplegia (3*Tropicamid 1%) with a calibrated autokeratorefractometer (model Accuref-K 9001; Shin Nippon, Tokyo, Japan). Slit lamp biomicroscopy and ophthalmoscopy were performed
Color vision tests
Color vision was assessed using the Fansworth D15, and the Lanthony desaturated D15 tests (LUNEAU Ophthalmologie). Each eligible eye was tested and the child was asked to place the 15 colored caps in order. The Lanthony desaturated test was always performed twice to check for repeatability [17]. The color vision tests were performed under daylight conditions obtained by a D65 (illuminant D) light source at 270 lux. The results were evaluated with a WEB-based scoring software (http://www.torok.info/colorvision/d15.htm) for the Farnsworth-Munsell 100-Hue, Roth 28-Hue, Farnsworth D-15, and the Lanthony D-15 desaturated color tests. This scoring software compares results to age matched normative data.
ERG measurements
Cone function was objectively tested for both eyes after pupil dilation (mentioned above), using full-field electroretinography under photopic conditions (RETIport System, Roland Consult GmbH, Wiesbaden, Germany). DTL electrodes were placed on the cornea after oxybuprocain 0.4%/proparacaine 0.5% instillation. A ground electrode was placed on the skin near the temporal orbital rim. Single flashes and 30 Hz flicker were presented for both the “standard” ERG (white light) and for the “S-cone” ERG (blue light on amber background). To get more cone specific responses, 30 Hz flicker was applied first, followed by 3 single flashes. We followed procedures proposed by the International Society for Clinical Electrophysiology of Vision (ISCEV) [18]. The interstimulus interval was 5 s for flash. The strength of white flash and flicker was 3 cd*s/m2 (on 25 cd/m2 background). The S-cone ERGs were performed with similar values to the proposed ISCEV extended protocol to assess S-cone responses The background illumination was amber (585 nm) at 85 cd/m2, to bleach the M- and L-cones. The stimuli were 6 cd*s/m2 blue (430 nm) flashes, reacting on S-cones only (Ref: http://www.iscev-wiki.org/twiki/bin/view/Main/SCone) All stimulus conditions (white flicker, white flash, blue flicker, blue flash) were produced by LEDs and were presented three times each, with flicker presented first. White stimuli were always presented before blue stimuli. Signals were bandpass filtered (low cut: 1 Hz, high cut: 300 Hz) and amplified (gain: 100,000) with artefact rejection at 95%. The amplitudes and implicit times were compared for the four groups.
Statistical analysis
Statistical analysis was performed with commercial software (GraphPad Prism 3.0 and SPSS ver. 15.0 for Windows; Chicago, IL). P ≤ 0.05 was considered statistically significant, with a 95% CI. The Shapiro-Wilks W test showed that the data were not normally distributed; therefore nonparametric tests were applied, and data were expressed as medians with the corresponding interquartile range (IQR). The Kruskal–Wallis test was used to evaluate differences among the four groups. For parameters showing significant difference between the groups Dunns Post Test was used, to compare each group to others
Receiver operating characteristic (ROC) curves were plotted to determine the cutoff point of b-wave amplitudes of standard ERG S-cone ERG with blue flash, respectively. The amplitudes were the test variables, prematurity was the static variable, with the category 0 used for full-term subjects (group IV) and 1 for the preterm children (group’s I–III). The null hypothesis was that there was no difference between the preterm and full-term subjects.
General estimating equations (GEE) were calculated for all selected eye and eligible fellow eyes (40 eyes of 25 preterm children and 16 eyes of 8 full-term subjects), to investigate whether prematurity or ROP was responsible for effects in the preterm group. The working correlation matrix was independent. A logit link function was applied. The patients’ identity numbers were used to designate the subjects. The patients’ eyes were compared to determine the within subject effects. The cutoff point calculated by ROC was the dependent parameter. The following factors were analyzed: stages of ROP (1. laser treatment, 2. ROP stages 1 to 2; 3. no ROP), birth weight ≤1,250 g and gestational age at birth ≤30 weeks as indices of prematurity. These two latter parameters were considered together, i.e. both values had to be below the respective values.
Results
No significant differences were found for any parameters between the left and right eyes of the patients.
The Kruskal–Wallis test showed no significant differences between the four groups for the following parameters: age, refraction (Table 1), the results of the psychophysical color vision tests, and the implicit time of the ERG waves for any stimulus condition (Table 2).
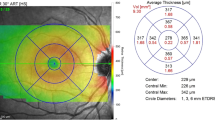
The b-wave amplitudes were smaller in the preterm groups compared to controls. The lowest amplitudes were found in laser treated preterm group (Fig. 1). However the differences were significant only for standard single flash ERG amplitude and for S-cone single flash ERG amplitude (Table 2).
Although amplitude appears to decrease with increasing severity of retinopathy, we found no significant differences for any parameters among the three premature groups. The comparison with Dunns post test of the groups for parameters showing significant difference are summarised in Table 3.
GEE statistics were performed to determine the relationship of prematurity and ROP in the reduced ERG amplitudes found in the preterm subjects compared with the full-term subjects. At first, the cutoff point of b-wave amplitude was determined by ROC curve analysis only for the two stimulus conditions that showed a significant difference on the Kruskal–Wallis test. The cutoff point of standard single flash ERG b-wave amplitudes was 99.8 μV (sensitivity: 0.825; specificity: 1.0; area under the curve [AUC] = 0.743 ± 0.076, mean ± SD, P = 0.009; 95% CI: 0.594–0.893). For S-cone ERG flash amplitude, the cutoff point = 81.05 μV (sensitivity: 0.85; specificity: 1.0), area under the curve [AUC] = 0.763 ± 0.061, (mean ± SD), P = 0.005; 95% CI: 0.638–0.889. (Fig. 2)
The general estimating equation indicated P = 0.025 and P = 0.014 for the effect of prematurity (birth weight ≤1,250 g and gestational age ≤30 weeks) on the b-wave amplitudes obtained by standard single flash ERG and S-cone ERG with single blue light stimuli, respectively. The analysis of effect of severity of retinopathy or laser treatment on the subtle cone dysfunction resulted in P values of 0.095 and 0.422 under conditions mentioned above.
Discussion
We found a subtle cone pathway dysfunction, that was present for ERG b-wave amplitude, but not latency, in formerly preterm children with normal appearing posterior pole. Comparing the preterm groups (group I–III) to a control group, significant differences in the b-wave amplitudes obtained with standard and S-cone electroretinography using single flash light stimuli were found, in subjects with a history of preterm birth who had laser-treated ROP.
Plausible explanations for the b-wave amplitude decrease could be the severe ROP that required laser treatment, or the premature birth. For the cones the first possibility could include loss of the cells, while the second one could include cellular dysfunction due to the disruption of normal development.
The first possibility is unlikely, as recent data gained with adaptive optics Fourier domain optical coherence tomography offered no evidence of cone loss in the central retina of the subjects with ROP [19] The ablation of the periphery could also be an explanation of cone loss but at present we have very few data on cone distribution in the periphery. Spatial cone density was investigated mostly in the foveal or parafoveal area, because in the periphery rods are known to be the dominant type of photoreceptors [20, 21].
Cellular dysfunction is more probable; as high vulnerability of the developing foveal cones is previously described, and these are the immature photoreceptors which appear to be particularly vulnerable to retinal oxygen level fluctuation [22]. The results of the GEE statistics in our study are also in accordance with this second hypothesis. It was the degree of prematurity characterized with birth weight ≤1,250 g and gestational age at birth ≤30 weeks, and not the severity of ROP or laser treatment, that predicted the long-term cone impairment.
This cone dysfunction seems to be a really subtle alteration, as significant decrease can be detected only in the b-wave amplitude, but the b-wave implicit times did not differ from those of controls. (A-waves could not be analysed in all cases, due to the small amplitudes and thus weak signal-to-noise ratio in all groups.) On one hand, earlier maturation may protect the cones. On the other hand, cones have twice as many mitochondria and greater aerobic ATP production which protects against metabolic insults and apoptosis [23]. Furthermore, cones, in contrast to rods, have the capability of utilizing endogenous glycogen, affording protection against the adverse effects of hypoxia and attendant hypoglycemia. [24]. Patient selection can also be an explanation for this finding, because in this study we examined preterm born children with perfect vision, and nomal appearing posterior pole. A previous study of Fulton et al. reported that cone function is only minimally reduced in mild ROP, but it is below the normal mean in all subjects with severe ROP [15].
The observed b-wave alteration can also imply that inner retinal cone pathways were affected in our subjects. Our previous morphological research with OCT, and other multifocal ERG findings support this hypothesis, suggesting that the developmental organization of the central retina is altered in ROP. The decrease or absence of inner retinal cell migration in preterm infants can be an explanation for the diminution of foveal depression and the continuity of bipolar and amacrine cell layer, seen on OCT scans [25], and the decreased amplitude of ERG waves in the central rings with multifocal ERG [26].
For the investigation of selective blue cone dysfunction, we tried to apply blue cone specific stimuli. At the time of our investigations there had been several reports that the human S-cone ERG can be separately detected, but this S-cone ERG was not standardized for age or methodology. [27–30]. We chose a strong amber background light to desensitize the L and the M cones as well as the rods, and to leave the S-cones much less light-adapted and consequently more responsive [30].
We found a reduction in b-wave amplitude for both ISCEV standard stimulus flashes and our S-cone stimuli and therefore we thought that besides S-cones, M- and L-cones might also be altered. This finding is supported by previous experimental studies describing cone differentiation in humans. S-opsin is expressed first at 12th gestational week, and it is followed by L/M opsin some weeks later in the central region. [31, 32]. At the time of oxygen induced injury probably S-cones are in a more mature so less vulnerable state than L/M cones. At the same time, our S-cone responses did not correspond with those reported previously in the literature. Their latency was earlier than published S-cone ERGs, and their b-wave amplitude was greater and more similar to standard cone ERGs. It raised the possibility; that we could not separate the S-cones totally from the L/M cones with our stimuli.
In accordance with the ERG results we couldn’t detect any selective color vision defect in preterm born children; compared to controls with the Fansworth D15 and the Lantony desaturated (L15) tests. We chose these two color vision tests because they are rather short, so relatively easy for children, and L15 was found to be the most suitable test for screening of early color vision abnormalities in uncomplicated juvenile diabetes [33]. It is only the Fansworth-Munsell 100-Hue test that has the same clinical reliability and sensitivity, but its results are affected—particularly in children—by the much longer execution time [33, 34]. The increased prevalence of impaired color vision, reported earlier in the CRYO-ROP study with the Standard Pseudoisochromatic Plates (SPP) in a big population [10], was not detected in several smaller studies with psychophysical methods [5–9]. The CryoROP Study described yellow-blue color vision deficits in a large preterm population. All of the children were younger than our patients. The birth weigth was less than it was in our study and all neonates had some stage of ROP. According to the literature, the SPP test used in the CRYO-ROP study demonstrated low sensitivity in early color vision defects in diabetes patients [33].
Limitations of the present study are the small sample size, and the moderate selectivity of the S-cone stimulation which precluded a definitive conclusion. However our study shows that a subtle dysfunction of the cone pathways is possible and it could be related to the degree of prematurity. The dysfunction represented by the photopic b-waves amplitude could mean that in addition to, or instead of the cone photoreceptors themselves, but the inner retinal cone pathways were affected. The alteration found is in accordance with previous anatomic and electrophysiological data showing lower vulnerability of cones than rods to ROP [15].
References
Gallo JE, Lennerstrand G (1991) A population based study of ocular abnormalities in premature children aged 5 to 10 years. Am J Ophthalmol 111:539–547
Keith CG, Kitchen WH (1983) Ocular morbidity in infants of very low birth weight. Br J Ophthalmol 67:302–305
Dowdeswell HJ, Slater AM, Broomhall J, Tripp J (1995) Visual deficits in children born at less than 32 weeks’ gestation with and without major ocular pathology and cerebral damage. Br J Ophthalmol 79:447–452
Snir M, Nissenkorn I, Sherf I, Cohen S, Sira IB (1988) Visual acuity, strabismus and amblyopia in preterm babies with and without retinopathy of prematurity. Ann Ophthalmol 20:256–258
Hungerford J, Stewart A, Hope P (1986) Ocular sequel of preterm birth and their relation to ultrasound evidence of cerebral damage. Br J Ophthalmol 70:463–468
Abramov I, Hainline L, Lennerise E, Brown A (1985) Changes in visual functions of children exposed as infants to prolonged illumination. J Am Optometric Assoc 56:614–619
O’Connor AR, Stephenson T, Johnson A, Tobin MJ, Moseley MJ, Ratib S, Ng Y, Fielder AR (2002) Long-term ophthalmic outcome of low birth weight children with and without retinopathy of prematurity. Pediatrics 109:12–18
O’Connor AR, Stephenson T, Johnson A, Tobin MJ, Moseley MJ, Ratib S, Fielder AR (2004) Visual outcome in low birth weight children. Br J Ophthalmol 88:1149–1153
Mcloone E, O’Keefe M, Mcloone S, Lanigan B (2006) Long term functional and structural outcomes of laser therapy for retinopathy of prematurity. Br J Ophthalmol 90:754–759
Dobson V, Quinn GE, Abramov I, Hardy RJ, Tung B, Siatkowski RM, Phelps DL (1996) Color vision measured with pseudoisochromatic plates at five and-a-half years in eyes of children from the CRYO-ROP study. Invest Ophth Vis Sci 37:2467–2474
Reisner DS, Hansen RM, Findl O, Petersen RA, Fulton AB (1997) Dark-adapted thresholds in children with histories of mild retinopathy of prematurity. Invest Ophth Vis Sci 38:1175–1183
Hansen RM, Fulton AB (2000) Background adaptation in children with a history of mild retinopathy of prematurity. Invest Ophth Vis Sci 46:3458–3462
Fulton AB, Hansen RM, Petersen RA, Vanderveen DK (2001) The rod photoreceptors in retinopathy of prematurity: an electroretinographic study. Arch Ophthalmol 119:499–505
Moskowitz A, Hansen RM, Fulton AB (2005) Early ametropia and ROD photoreceptor function in retinopathy of prematurity. Optom Vis Sci 82:307–317
Fulton AB, Hansen RM, Moskowitz A (2008) The cone electroretinogram in retinopathy of prematurity. Invest Opht Vis Sci 49:814–819
An International Committee for Classification of retinopathy of prematurity (2005) The International Classification of retinopathy of prematurity. Arch Ophthalmol 123:991–999
Good GW, Schepler A, Nichols JJ (2005) The reliability of the Lanthony Desaturated D-15 test. Optom Vis Sci 82:1054–1059
Marmor MF, Fulton AB, Holder GE, Miyake Y, Brigell M, Bach M (2009) Standard for clinical electroretinography (2008 update). Doc Ophthalmol 118:69–77
Hammer XD, Iftimia NV, Ferguson RD, Bigelow CE, Ustun TE, Barnaby AM, Fulton AB (2008) Foveal fine structure in retinopathy of prematurity:An Adaptive Optics Fourier Domain Optical Coherence Tomography study. Invest Ophht Vis Sci 49:2061–2070
Curcio CA, Sloan KR, Kalina RE, Hendrickson AE (1990) Human photoreceptor topography. J Comp Neurol 292:497–523
Curcio CA, Kimberly AA, Sloan KR, Lerea CL, Hurley JB, Klkock IB, Milam AH (1991) Distribution and morphology of human cone photoreceptors stained with anti-blue-opsin. J Comp Neurol 312:610–624
Wellard J, Lee D, Valter K, Stone J (2005) Photoreceptors in the rat retina are specifically vulnerable to both hypoxia and hyperoxia. Vis Neurosci 22:501–507
Perkins GA, Ellisman MH, Fox DA (2003) Three-dimensional analysis of mouse rod and cone mitochondrial cristae architecture: bioenergetic and functional implications. Mol Vis 9:60–73
Nihira M, Anderson K, Gorin FA, Burns MS (1995) Primate rod and cone photoreceptors may differ in glucose accessibility. Invest Opht Vis Sci 36:1259–1270
Ecsedy M, Szamosi A, Karko C, Zubovics L, Varsanyi B, Nemeth J, Recsan Zs (2007) Comparison of Macular Structure Imaged by Optical Coherence Tomography in Preterm and Full-Term Children. Invest Opht Vis Sci 48:5207–5211
Fulton AB, Hansen RM, Moskowitz A, Barnaby AM (2005) Multifocal ERG in subjects with a history of retinopathy of prematurity. Doc Ophthalmol 111:7–13
Padmos P, Norren D, Jaspers Faijer JW (1978) Blue cone function in a family with an inherited tritan defect tested with electroretinography and psychophysics. Invest Ophthalmol Vis Sci 17:436–441
Sawusch M, Pokorny J, Smith VC (1987) Clinical electroretinography for short wavelength sensitive cones. Invest Ophthalmol Vis Sci 28:966–974
Miyake Y, Yagasaki K, Ichikawa H (1985) Differential diagnosis of congenital tritanopia and dominantly inherited juvenile optic atrophy. Arch Ophthalmol 103:1496–1501
Gouras P, MacKay CJ (1990) Electroretinographic responses of the short-wavelength-sensitive cones. Invest Ophthalmol Vis Sci 31:1203–1209
Xiao M, Hendrickson A (2000) Spatial and temporal expression of short long/medium, or both opsins in human fetal cones. J Comp Neurol 425:545–559
Bumsted-O’Brien KM, Shulte D, Hendrickson AE (2003) Expression of photoreceptors-associated molecules during fetal eye development. Mol.Vis 9:401–409
Giusti C (2001) Lanthony 15-Hue Desturated Test for screening of early color vision defects in uncomplicated juvenile diabetes. Jpn J Ophthalmol 45:607–611
Verriest G, Lethem JV, Uvijls A (1982) A new assessment of the normal ranges of the Farnsworth-Munsell 100-Hue test scores. Am J Ophthalmol 93:635–642
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ecsedy, M., Varsányi, B., Szigeti, A. et al. Cone function in children with a history of preterm birth. Doc Ophthalmol 122, 141–148 (2011). https://doi.org/10.1007/s10633-011-9268-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-011-9268-z