Abstract
The aim of this study was to investigate the relationship between stimulus intensity and response amplitude for the photopic negative response (PhNR) of the flash ERG. Specific aims were (i) to determine whether a generalized Naka–Rushton function provided a good fit to the intensity–response data and (ii) to determine the variability of the parameters of the best-fitting Naka–Rushton models. Electroretinograms were recorded in 18 participants, on two occasions, using both DTL fibre and skin active electrodes, in response to Ganzfeld red stimuli (Lee filter “terry red”) ranging in stimulus strength from −1.30 to 0.53 log cd.s.m−2 (0.28–2.11 log phot td.s) presented over a steady blue background (Schott glass filter BG28; 3.9 log scot td). PhNR amplitude was measured from b-wave peak and from pre-stimulus baseline. The Naka–Rushton function was fitted to all intensity–response data, and parameters, ‘n’, ‘Vmax’ and ‘K’ were obtained. Coefficients of variation (CoV), and inter-ocular and inter-session limits of agreement (LoA) were calculated for both Naka–Rushton parameters. A generalized Naka–Rushton function was found to provide a good fit to the intensity–response data, except at the highest stimulus intensity, where a reduction in amplitude occurred in many individuals. The ‘Vmax’ parameter was less variable than ‘K’ for all intensity–response data. Variability was lower for DTL than skin electrodes, and for peak-to-trough PhNR measurements, compared to baseline-to-trough. This study has demonstrated for the first time that the Naka–Rushton model provides a useful means of quantifying the intensity–response relationship of the PhNR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The flash electroretinogram (ERG) has historically been used principally to assess the function of the outer retinal layers. In 1999, however, Viswanathan et al. reported on a newly identified negative wave following the b-wave of the flash ERG, which they termed the photopic negative response (PhNR) [1]. There is now substantial evidence to suggest that this response originates principally from the spiking activity of inner retinal neurones, predominantly the retinal ganglion cells [1–13]. Previously, the electrophysiological assessment of inner retinal function had been largely dependent on the pattern electroretinogram (PERG) [14–18], a response which requires considerable averaging and is susceptible to reduction by refractive blur and media opacities [19], so the possibility of assessing ganglion cell function with the flash ERG is an attractive one.
Evidence suggests that the amplitude, but not the implicit time, of the PhNR is affected in primary open-angle glaucoma [2, 3, 13]. Unfortunately, however, amplitudes of the subcomponents of the ERG tend to vary more between individuals than implicit times, and this is true of the PhNR [4, 20]. This inter-individual variation may be attributed to differences in anatomical factors such as fundus pigmentation [21] and axial length [22], or to technical factors such as electrode position or contact impedance, as well as to variation in retinal function. A wide spread of responses within the normal population makes it more difficult to detect disease-related changes. It may, therefore, be more appropriate to consider alternative analytical approaches whereby the variations in absolute amplitude are rendered less important.
In a previous report, investigating measurement protocols aimed at minimising amplitude variation, we determined that the calculation of a ratio of the b-wave amplitude to the PhNR amplitude resulted in a lower level of variability than absolute PhNR amplitude within a population of normal participants [20]. Another means of assessing function, which may reduce the impact of variability of absolute amplitudes, is the analysis of change in response amplitude with varying stimulus intensity. An increase in PhNR amplitude with increasing stimulus strength has been described, with saturation occurring at around 2.0 log phot td.s [9, 10, 13, 23]; however, no attempt has been made to fit this intensity–response data with a mathematical model, thereby allowing a quantitative analysis of the parameters of the intensity–response relationship. The generalised “Naka–Rushton” function (see Eq. 1) is a sigmoidal curve, which has been shown to describe the increase in b-wave amplitude, measured from the minimum point of the a-wave, with increasing stimulus intensity [24–26]. This reportedly provides a good fit to data across a range of intensities, although the relationship breaks down at high intensities for both light- [27] and dark-adapted [28] b-waves. The intensity–response data of the d-wave of the flash ERG have also been fitted with the generalized (hyperbolic) Naka–Rushton function [29].
where V = response amplitude; Vmax = the maximum amplitude; I = stimulus intensity; K = the semi-saturation constant i.e. the stimulus intensity at which the amplitude is at a half of Vmax; and n = an exponent describing the slope of the function, at the point where stimulus strength = the exponent, K.
This study aimed to determine whether the generalised Naka–Rushton function could provide a good fit to PhNR intensity–response data and to investigate the inter-subject, inter-ocular and inter-session variability of the parameters of the best-fitting model. The intensity–response data of the photopic b-wave were also analysed for comparison.
Methods
Participants
A total of 18 participants aged 20–33 years were recruited from within the staff and students at the School of Optometry and Vision Sciences at Cardiff University. All participants returned for a second visit within 2 weeks of the primary visit to assess inter-session repeatability. All participants had normal corrected visual acuity (0.1 logMAR or better) and good ocular health. Participants with a refractive error > ± 6.00D mean sphere or a family history of glaucoma were excluded.
All participants gave signed consent after a full explanation of the study. The study was conducted within the tenets of the Declaration of Helsinki and had been reviewed by the ethical committee of the School of Optometry and Vision Sciences.
Electroretinography
Pupils were dilated with 1 drop of 1.0% tropicamide prior to ERG recording, with a minimum pupil diameter of 7 mm obtained for all participants. Binocular ERGs were recorded simultaneously using skin and DTL fibre active electrodes. DTL fibre active electrodes [30] (Unimed electrode supplies, Surrey, UK) were positioned in each eye, in the lower fornix to maximise stability during recording [31], and the loose end fastened using medical tape at the inner canthus (Blenderm, Viasys Healthcare Ltd., Warwick, UK). Silver–silver chloride, 9 mm diameter, ‘touchproof’ skin electrodes (Viasys Healthcare Ltd., Warwick, UK) were placed on the orbital rim directly below the pupil in primary position. Both DTL and skin active electrodes were referred to a skin electrode placed about 3 cm behind the ipsilateral outer canthus; the earth electrode was a skin electrode placed in the mid-frontal position. Skin preparation reduced impedance to below 5 kΩ. All ERGs were recorded without local anaesthetic or methylcellulose solution.
The PhNR was elicited to Ganzfeld stimulation (GS2000, LACE Elettronica, Italy) of long wavelength light (Lee Filter “Terry Red”, Lee Filters, Hampshire, UK; transmittance <5% at wavelengths shorter than 575 nm, and above 85% from 625–700 nm) presented at 4 Hz (max 300 μs flash duration) over a continuous blue background (Schott Glass filter BG28, Schott AG, Mainz, Germany; peak transmittance 450 nm) of 3.9 log scot td.s (sufficient strength to saturate the s-cones and rods [32]). Participants were pre-adapted to the background for a minimum of 5 min prior to testing.
Electroretinograms were recorded to a series of flashes of increasing intensity, ranging from −1.30 to 0.53 log cd.s.m−2 (0.28–2.11 log phot td.s, assuming a 7-mm pupil and making no allowance for the Stiles Crawford effect), using a Medelec Synergy EP unit (Viasys Healthcare Ltd., Warwick, UK). All stimuli were calibrated using the ILT1700 microprocessor-controlled digital radiometer, with SED033/Y/R luminance detector (Able Instruments and Controls, Reading, UK). The PhNR was recorded in sets of 10 averages, with timebase (recording period) of 200 ms. A total of 40–200 responses (depending on stimulus intensity) were averaged over four channels; these four traces were superimposed to confirm signal repeatability and averaged off-line. All responses were bandpass filtered from 1 to 100 Hz. An automatic rejection system removed signals containing large eye movements and blink artefacts.
Signal analysis
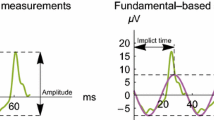
The amplitudes of the PhNR and b-wave were measured from the averaged ERG trace, uncorrected for baseline drift. The i-wave obscured the negative trough of the PhNR for stimulus strengths above around 0.91 log phot td.s (as reported by others [5, 6]), and for this reason, we measured the PhNR at the minimum point directly before or after the i-wave to ensure that we identified the most negative location. The position of the minimum point varied between individuals, but in most cases, it was after the i-wave at stimulus strengths above 1.21 log phot td.s, whilst at lower intensities, the waveform was more symmetrical and the most negative point could be before or after the peak of the i-wave. On the basis of a previous analysis of the inter-individual, inter-session and inter-ocular variability of the PhNR, measurements from the peak of the b-wave to the minimum before or after the i-wave (PT) were considered to be less variable than measurements relative to the pre-stimulus baseline (BT) [20]. However, in assessing the relationship between stimulus intensity and the amplitude of the PhNR, it was also considered important to assess the amplitude of response independent of the b-wave amplitude, so responses were also measured from baseline. The amplitude of the b-wave was measured from the minimum point of the a-wave to the maximum point of the b-wave.
Statistical analysis
The amplitude data were plotted as a function of log stimulus intensity and were fitted with the Naka–Rushton model (see Eq. 1), with parameters Vmax, K and n modified on a ‘least squares’ basis using Microsoft Excel version 2003. Whilst the exponent n is close to unity in the healthy eye and it has been suggested that this may be omitted to simplify the equation [24], we adopted the approach that a number of investigators have taken in modelling the intensity–response function of the b-wave [26–29, 33–35], and allowed ‘n’ as a freely adjustable variable in the equation. This maximised the goodness of fit of the model. The goodness of fit of the model was assessed by calculating the root mean squared error (RMSE), expressed as a percentage of Vmax to provide a normalised index comparable between components with different absolute amplitudes. It was decided to assess the variability of Vmax and K as these are the Naka–Rushton parameters most commonly affected by retinal disease [34, 36]. The Vmax and K parameters of the best-fitting Naka–Rushton model were obtained for all participants, for both visits, for all 3 amplitude measures: b-wave, PhNR measured from b-wave peak (PT) and PhNR measured from pre-stimulus baseline (BT).
The coefficient of variation, expressed as a percentage, was calculated for Vmax and K, for right and left eyes, for both DTL and skin electrodes for visit 1 of all participants. This is a measure of the spread of data, where a lower quotient indicates a narrower distribution of data within the group i.e. less inter-individual variation.
The distribution of the data was checked for normality using the Shapiro–Wilk test, and then Bland–Altman plots were constructed to assess inter-ocular variability of Vmax and K within the first session and inter-session repeatability (of the right eye) [37]. As in Fortune et al. [4], limits of agreement (LoA) were also calculated as a percentage of the mean value to allow between-eye and between-session findings to be compared across techniques (see Eq. 2) [4].
As described by Bland and Altman [37], 95% confidence intervals were constructed to assess the precision of the LoA. To summarise, the standard error of the LoA was calculated using the formula √(3s2/n), where s = standard deviation of differences and n = number of participants. This value was multiplied by the t-value for n-1 degrees of freedom (P = 0.05), and the confidence intervals were calculated as LoA ±(t × SE). These confidence intervals were then expressed as a percentage of the mean amplitude.
One-way ANOVA and paired t tests, with P-values Bonferroni-corrected for multiple comparisons [38], were carried out to determine whether there were statistically significant differences in Vmax and K between parameters and electrode type. All statistics were performed using SPSS 16 (IBM).
Results
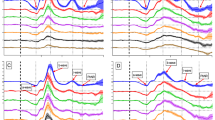
At the lower flash intensities, there was an increase in both b-wave and PhNR amplitudes with increasing stimulus intensity for all participants. The b-wave was approaching saturation by 2.11 log phot td.s and, analysing the data from visit 1, a slight reduction in b-wave amplitude was visible at the highest intensity in 8 of the 18 participants. The PhNR measured from the peak of the b-wave (PT) showed saturation in all individuals at either 1.51 or 1.81 log phot td.s and showed a more marked reduction in amplitude at the highest stimulus intensities than the b-wave. This reduction in amplitude occurred at 1.81 log phot td.s in 3 individuals, and at 2.11 log phot td.s in a further 12 participants. The amplitude of the PhNR measured from pre-stimulus baseline (BT) showed either saturation at the highest stimulus intensity (N = 8) or a slight reduction in amplitude at 2.11 log phot td.s (N = 10).
Representative data from the first visit of one individual can be seen in Fig. 1, where the reduction in the amplitude of the response at the highest stimulus intensity is marked for the peak-to-trough PhNR measurement (PT) and smaller, but still present, for the baseline-to-trough (BT) measurement, but absent for the b-wave intensity–response series. The rising/saturating portion of the intensity–response data was fitted well by the Naka–Rushton function for both b-wave and PhNR data (when there was a reduction in amplitude at the final data points, these were excluded from the model fitting procedure). The normalised RMSE was between 2.79 and 3.96% of Vmax for all parameters.
To investigate the general shape of the intensity–response function within the group, the amplitudes of the b-wave, PT and BT PhNR measurements of all 18 subjects at visit 1 were averaged at each intensity to produce a mean intensity–response series, which can be seen in Fig. 2. This approach has been demonstrated in previous publications [39, 40]. For the b-wave and the PT PhNR intensity–response data, it can be seen that there is an increase in amplitude, following the sigmoidal shape of the Naka–Rushton function, up until the highest stimulus intensity, where there is a small reduction in amplitude for the b-wave, and a larger reduction for the PT PhNR data. The BT PhNR data showed a similar pattern, although the reduction in amplitude at the highest intensity was less. For both DTL and skin active electrodes, there was an increase in the variability of the responses with increasing amplitude, which is reflected in the larger error bars (±SEM) shown at the higher intensities. This variability for large amplitude responses is also apparent in that the right eye and left eye data are more divergent at the highest intensities, although the error bars are overlapping.
The data points show the averaged amplitudes of all 18 participants at visit 1 (error bars show SEM) as a function of stimulus illuminance, with black points relating to the right eye, and left eye data shown in grey for comparison. The solid lines show the best-fitting Naka–Rushton function for each averaged data set. a shows b-wave amplitude data, b shows PhNR data measured from the peak of the b-wave (PT), c shows PhNR data measured from pre-stimulus baseline (BT)
To ensure that the reduction in amplitude at the highest stimulus intensity was not due to insufficient time for retinal recovery between flashes, intensity–response series were recorded from two individuals using a 0.5 Hz stimulus and compared to the results using the 4 Hz stimulus. The data still showed a reduction in b-wave and PhNR amplitude (PT and BT) at the highest stimulus intensity (see Fig. 3 for sample data from one individual), suggesting that the 4 Hz stimulus frequency did not cause an artefactual reduction in amplitude at the highest intensities.
The 4 Hz intensity–response data of individual participants were modelled, and the parameters of the best-fitting Naka–Rushton models were analysed. It was not possible to fit the Naka–Rushton model to all the data from the skin electrodes, due to a poor signal-to-noise ratio at some stimulus intensities, particularly for the low-amplitude BT PhNR measure. Over the 2 visits, 1 patient was excluded from skin RE calculations for the BT PhNR measurement, 2 were excluded from skin LE calculations; one of these individuals was also excluded for the PT PhNR measurement. Data from the remaining participants are summarised in Table 1.
The Naka–Rushton model provided a good fit to the PhNR intensity–response data from both right and left eyes, using both skin and DTL electrodes. This is illustrated by the normalised RMSE value in Table 1. The b-wave and the peak-to-trough (PT) PhNR data showed comparable goodness of fit of the Naka–Rushton model, whilst the baseline-to-trough (BT) PhNR intensity–response data resulted in higher RMSE values. This difference was statistically significant for the BT PhNR data recorded using a skin electrode (RE), for which the RMSE was significantly higher than that of the b-wave and PT PhNR model fits (one-way ANOVA, Bonferroni post hoc analysis; P < 0.05).
From Table 1, it can be seen that Vmax was greater for DTL electrodes than for skin electrodes; this difference was significant for b-wave (paired t test: P < 0.001 RE, P < 0.001 LE) and PhNR data, measured from peak-to-trough (PT: paired t test: P < 0.001 RE, P < 0.001 LE), and from baseline (BT: paired t test: P < 0.01 RE, P < 0.01 LE). Vmax ranged from being 1.48 times greater with the DTL compared to the skin electrode (BT PhNR, RE) to 2.07 times greater (b-wave, LE). For both DTL and skin active electrodes, the coefficient of variation (CoV) for Vmax was comparable for b-wave and PT PhNR measurements but was higher for BT PhNR measurements, indicating a higher level of variability for measurements from baseline.
There was no significant difference in K between any of the amplitude parameters i.e. between b-wave, PT and BT, for skin and DTL electrodes (one-way ANOVA: P = 0.865 RE, P = 0.06 LE). This suggests that the stimulus intensity required for 50% of Vmax to be achieved is similar for the b-wave and PhNR, and for DTL and skin electrodes (mean K ranged from 0.88 to 1.06 log phot td.s for the different parameters). The CoV for K was highest for baseline-to-trough (BT) PhNR measurements and for skin electrode measurements (see Table 1).
In order to further assess the ability of the Naka–Rushton model to reliably describe the intensity–response series of the PhNR, Bland–Altman plots were constructed to assess inter-ocular and inter-session variability, and limits of agreement were calculated (see Figs 4, 5). Limits of agreement were also expressed as a percentage of the mean value of each parameter to facilitate the comparison of variability between parameters with different absolute values. The LoA for the inter-ocular calculations was expressed as a percentage of mean Vmax/K for pooled right eye and left eye data (visit 1). The inter-session LoA was expressed as a percentage of the mean Vmax/K for pooled visits 1 and 2 (right eye data). These values are shown in Table 2, along with 95% confidence intervals for the % LoA. The parameters of the best-fitting Naka–Rushton models to PhNR data measured from baseline-to-trough (BT) were generally more variable than the parameters of the models fitted to b-wave and PT PhNR amplitudes. However, Table 2 shows some overlap of the confidence intervals for the LoA, which suggests that this difference was only significant in some cases (e.g. the inter-ocular and inter-session LoA for K were significantly higher for BT PhNR than PT PhNR or b-wave for the DTL electrode). The skin electrode responses tended to be more variable than DTL responses, although the overlap of confidence intervals again suggested that this difference was not always statistically significant.
A comparison of the variability of the two parameters of the Naka–Rushton function is possible by examination of Tables 1 and 2. It can be seen that Vmax showed lower CoV than K for all parameters (confidence intervals did not overlap). The inter-ocular and inter-session variability were not significantly different for K and Vmax, apart from both skin electrode PhNR measures, for which K was significantly less repeatable.
Discussion
The findings of this study suggest that the generalized (hyperbolic) Naka–Rushton function is an appropriate means of describing the intensity–response relationship of the PhNR measured from b-wave peak (PT) or from pre-stimulus baseline (BT), particularly when the DTL active electrode is used. Other studies have demonstrated that the photopic b-wave intensity–response data are well characterised by the Naka–Rushton function at low to moderate stimulus strengths (up to around 0.8 log cd.s.m−2) [27, 35], a finding which we have replicated in the b-wave and report for the first time in the PhNR.
The reduction in PhNR amplitude observed at the highest stimulus intensity in the majority of participants, whether measured from baseline (BT) or from the peak of the b-wave (PT), is an intriguing finding. This reduction in amplitude to high intensity stimuli might be expected with respect to the modelling of PT PhNR data, as the peak-to-trough measurement is the sum of b-wave and PhNR amplitudes, and the photopic b-wave is known to show a reduction in amplitude at high stimulus intensities, a phenomenon known as the ‘photopic hill’ [21, 27, 39–43]. In this study, the data indicated that a reduction in b-wave and PT PhNR amplitude was apparent in most participants when the stimulus strength reached 2.11 log phot tds (equivalent to 0.53 log cd.s.m−2). This is comparable to the stimulus strength reported in the literature as corresponding to Vmax for the photopic b-wave luminance response function (from around 0.5 log cd.s.m−2 [44] to 0.86 log cd.s.m−2 [27]). However, the fact that the reduction in amplitude at the highest stimulus intensity was more marked for the PT PhNR data than the b-wave data, and the apparent reduction in BT PhNR amplitude in 10 individuals at the highest stimulus intensity, both suggest that this effect is not solely attributable to the well-recognised ‘photopic hill’ of the b-wave.
Several studies have investigated the saturating characteristics of the PhNR intensity–response series [9–11, 13, 45]. Sustar et al. [11] in their intensity–response series to red flashes on a blue background showed a maximum response at 0.40 log cd.s.m−2 (slightly dimmer than our highest intensity) and found a reduction in amplitude with increased stimulus luminance, although they attributed this to blinking artefacts [11]. Rangaswamy et al. [10] measured PhNR amplitude (from baseline) to 5 brief flash strengths ranging from −1.36 to 0.45 log cd.s.m−2 [10]. They found response amplitude had saturated by the highest stimulus intensity in all individuals (slightly dimmer than our highest intensity flash). Viswanathan et al. [13] reported that the PhNR had generally saturated by their highest intensity of 2 log phot td.s (around 0.20 log cd.s.m−2, assuming the 9 mm pupil diameter described in their study) [13]. Rangaswamy et al. [9] recorded photopic ERGs to a similar range of stimuli, and also reported amplitude saturation at 1.7–2.0 log td.s (equivalent to −0.10–0.20 log cd.s.m−2, with a 9 mm pupil). Only one study has reported a further increase in PhNR amplitude beyond around 0.50 log phot cd.s.m−2 [45], finding that PhNR amplitude continued to increase in amplitude up to 0.70 log phot cd.s.m−2, showing signs of saturation at 0.85 log cd.s.m−2. However, they only employed 3 stimulus intensities. None of the current literature describes the amplitude of the PhNR beyond response saturation.
In this study, we stimulated the retina with brief red flashes on a rod saturating blue background, a stimulus combination which has been shown to give higher amplitude responses than other combinations of chromatic or achromatic stimuli [10, 11]. Rangaswamy et al. [10] and Sustar et al. [11] investigated the effect of stimulus colour on the intensity–response series and generally reported that red on blue gave the largest amplitude responses at low stimulus intensities, but the intensity–response functions converged for all colours at the highest intensities [10, 11]. This indicates that the gradient of the intensity–response series will be dependent on stimulus colour, and should be considered when comparing results using different stimulus parameters.
For both DTL and skin active electrodes, there was an increase in the variability of the responses with increasing stimulus intensity, as has previously been reported for other electrophysiological signals [28, 46]. This was evident in the increasing standard error with increasing stimulus intensity, and also in greater variability between the two eyes for the higher intensities. Fortune et al. [4] similarly found the variability in PhNR amplitude between right and left eyes to be largest for the dimmest and brightest stimuli [4].
There was no significant difference in the goodness of fit of the generalized Naka–Rushton model (assessed using the normalised RMSE) to b-wave and PT PhNR data. However, the model fit to BT PhNR data collected using the skin active electrode showed a significantly higher RMSE than the other parameters, suggesting either ‘noisier’ data or a poorer model fit. This is an agreement with our finding in a previous report that the PhNR measured from pre-stimulus baseline tends to be more variable than measurements from b-wave peak [20]. The skin electrode data of 3 participants were excluded on one visit due to a poor signal-to-noise ratio, preventing a feasible fit of the Naka–Rushton model. The skin electrode responses also tended to show slightly more variability in the parameters of the Naka–Rushton function between subjects, between eyes and between visits than those recorded using the DTL electrode (although overlapping confidence intervals suggested that this difference was not significant in all cases). These factors indicate that the DTL electrode is more suitable for clinically assessing the intensity–response series of the PhNR. Wali and Leguire [47] compared the parameters of the dark-adapted b-wave intensity–response function recorded using skin and corneal (jet contact lens) electrodes [47] and also reported that Vmax was more variable for the skin electrode, although they found the variability of K to be similar between electrode types.
As expected, the magnitude of the parameters of the Naka–Rushton function also differed between the skin and the DTL electrodes. We found Vmax recorded using the DTL electrode to be around 2× larger for DTL than skin electrodes, for both PT PhNR and b-wave amplitudes, whilst Vmax for the BT PhNR amplitude was approximately 1.5× larger for DTL electrode responses. This is consistent with the magnitude of increased amplitude reported from signals recorded using DTL electrode compared with skin electrodes [48–50].
Despite the discrepancy in Vmax between electrode types, there was no significant difference in K between skin and DTL electrodes. This indicates a decreased maximum amplitude with the skin electrode, but a similar sensitivity of the intensity–response relationship. Bradshaw et al. [51] also found that, when scaled for amplitude, the b-wave intensity–response series of the skin and corneal electrodes were similar [51]. In contrast, Wali and Leguire [47] found skin electrode responses to have a lower K value than corneal electrode responses [47], indicating a greater sensitivity of the responses recorded using the skin electrode. However, they were analysing scotopic b-wave amplitudes, rather than photopic ERGs. In our results, Vmax was significantly less variable than K in terms of inter-subject CoV and also, in some cases, for inter-ocular and inter-session LoA. Wali and Leguire also found K to be the most variable parameter for the intensity–response series of the scotopic b-wave [47]. In a previous paper, we reported the variability of PhNR amplitudes measured in different ways in response to a stimulus of 1.76 log phot td.s [20]. When the variability of the published absolute PhNR amplitudes (PT and BT) is compared to the CoV and LoA parameters found in this study for the Vmax and K values, Vmax is found to be very similar in repeatability to the absolute amplitude measure, but K is markedly more variable.
One benefit of recording the intensity–response series of the PhNR is that different types of disease damage are likely to differentially affect different parameters of the Naka–Rushton model. With regard to the b-wave, a reduction in Vmax is generally thought to reflect a loss of photoreceptors [24, 34, 52], although it has been suggested that the local loss of rods may influence K more than Vmax [36]. The parameter K reflects the sensitivity of the retina and will generally be increased either if the healthiest region of the retina has receptors less sensitive than normal or if a large proportion of the photoreceptors have a decreased sensitivity [36]. The PhNR intensity–response series is also likely to reflect the type of disease effect and would be affected by the level of input from the distal retina to the retinal ganglion cells (RGCs), as well as by the functioning of the RGCs. On a basic level, a diffuse loss of RGCs may result in a reduction in Vmax on the basis of fewer generating neurones to produce the response, whilst abnormally functioning RGCs may result in a reduced retinal sensitivity and an increase in ‘K’. It is known that a loss of RGC function in experimental animals (using TTX) eliminates the PhNR at a range of stimulus intensities [1]; however, it may be that an earlier stage of the disease process, before ganglion cell death, could result in a change in the ‘K’ parameter.
To conclude, this study has demonstrated that the generalized Naka–Rushton model is able to well characterise the intensity–response relationship of the PhNR recorded from b-wave peak or from baseline. The DTL active electrode data, when modelled, elicit Vmax and K parameters which are slightly less variable than the skin electrode, whilst the parameters of the PT PhNR measure are less variable than the modelled BT data. The goodness of fit of the Naka–Rushton model and the variability of the parameters recorded using the DTL electrode are comparable between PT PhNR data and photopic b-wave data. The assessment of the intensity–response data may provide additional information about inner retinal disease process.
Abbreviations
- PT:
-
Peak-to-trough
- BT:
-
Baseline-to-trough
References
Viswanathan S, Frishman LJ, Robson JG, Harwerth RS, Smith EL (1999) The photopic negative response of the macaque electroretinogram: reduction by experimental glaucoma. Invest Ophth Vis Sci 40(6):1124–1136
Colotto A, Falsini B, Salgarello T, Iarossi G, Galan ME, Scullica L (2000) Photopic negative response of the human ERG: Losses associated with glaucomatous damage. Invest Ophth Vis Sci 41(8):2205–2211
Drasdo N, Aldebasi YH, Chiti Z, Mortlock KE, Morgan JE, North RV (2001) The s-cone PhNR and pattern ERG in primary open angle glaucoma. Invest Ophth Vis Sci 42(6):1266–12724
Fortune B, Bui BV, Cull G, Wang L, Cioffi GA (2004) Inter-ocular and inter-session reliability of the electroretinogram photopic negative response (PhNR) in non-human primates. Exp Eye Res 78(1):83–93
Gotoh Y, Machida S, Tazawa Y (2004) Selective loss of the photopic negative response in patients with optic nerve atrophy. Arch Ophthalmol 122(3):341–346
Kizawa J, Machida S, Kobayashi T, Gotoh Y, Kurosaka D (2006) Changes of oscillatory potentials and photopic negative response in patients with early diabetic retinopathy. Jpn J Ophthalmol 50(4):367–373
Machida S, Gotoh Y, Tanaka M, Tazawa Y (2004) Predominant loss of the photopic negative response in central retinal artery occlusion. Am J Ophthalmol 137(5):938–940
Machida S, Gotoh Y, Toba Y, Ohtaki A, Kaneko M, Kurosaka D (2008) Correlation between photopic negative response and retinal nerve fiber layer thickness and optic disc topography in glaucomatous eyes. Invest Ophth Vis Sci 49(5):2201–2207
Rangaswamy NV, Frishman LJ, Dorotheo EU, Schiffman JS, Bahrani HM, Tang RA (2004) Photopic ERGs in patients with optic neuropathies: comparison with primate ERGs after pharmacologic blockade of inner retina. Invest Ophth Vis Sci 45(10):3827–3837
Rangaswamy NV, Shirato S, Kaneko M, Digby BI, Robson JG, Frishman LJ (2007) Effects of spectral characteristics of ganzfeld stimuli on the photopic negative response (PhNR) of the ERG. Invest Ophth Vis Sci 48:4818–4828
Sustar M, Cvenkel B, Brecelj J (2009) The effect of broadband and monochromatic stimuli on the photopic negative response of the electroretinogram in normal subjects and in open-angle glaucoma patients. Doc Ophthalmol 118(3):167–177
Viswanathan S, Frishman LJ, Robson JG, Walters JW (2000) The photopic negative response of the flash electroretinogram (ERG) in primary open angle glaucoma. Invest Ophth Vis Sci 41(4):1533 B1908
Viswanathan S, Frishman LJ, Robson JG, Walters JW (2001) The photopic negative response of the flash electroretinogram in primary open angle glaucoma. Invest Ophth Vis Sci 42(2):514–522
Bach M, Hoffmann MB (2008) Update on the pattern electroretinogram in glaucoma. Optometry Vision Sci 85(6):386–395
Bach M, Speidel-Fiaux A (1989) Pattern electroretinogram in glaucoma and ocular hypertension. Doc Ophthalmol 73(2):173–181
Papst N, Bopp M, Schnaudigel OE (1984) Pattern electroretinogram and visually evoked cortical potentials in glaucoma. Graefes Arch Clin Exp Ophthalmol 222(1):29–33
Trick GL, Bickler-Bluth M, Cooper DG, Kolker AE, Nesher R (1988) Pattern reversal electroretinogram (PrERG) abnormalities in ocular hypertension: correlation with glaucoma risk factors. Curr Eye Res 7(2):201–206
van Lith G, Ringens P, de Heer LJ (1984) Pattern electroretinogram and glaucoma. Dev Ophthalmol 9:133–139
Bach M, Mathieu M (2004) Different effect of dioptric defocus vs. light scatter on the pattern electroretinogram (PERG). Doc Ophthalmol 108(1):99–106
Mortlock KE, Binns AM, Aldebasi YH, North RV (2010) Inter-subject, inter-ocular and inter-session repeatability of the photopic negative response of the electroretinogram recorded using DTL and skin electrodes. Doc Ophthalmol 121(2):123–134
Wali N, Leguire LE (1992) Fundus pigmentation and the dark-adapted electroretinogram. Doc Ophthalmol 80(1):1–11
Westall CA, Dhaliwal HS, Panton CM, Sigesmun D, Levin AV, Nischal KK, Heon E (2001) Values of electroretinogram responses according to axial length. Doc Ophthalmol 102(2):115–130
Miyata K, Ueno S, Kondo M, Koyasu T, Terasaki H (2008) Comparison of photopic negative responses elicited by red and white xenon flashes in monkeys. Jpn J Ophthalmol 52(4):327–330
Arden GB, Carter RM, Hogg CR, Powell DJ, Ernst WJ, Clover GM, Lyness AL, Quinlan MP (1983) A modified ERG technique and the results obtained in x-linked retinitis pigmentosa. Br J Ophthalmol 67(7):419–430
Fulton AB, Rushton WA (1978) The human rod ERG: correlation with psychophysical responses in light and dark adaptation. Vision Res 18(7):793–800
Massof RW, Wu L, Finkelstein D, Perry C, Starr SJ, Johnson MA (1984) Properties of electroretinographic intensity-response functions in retinitis pigmentosa. Doc Ophthalmol 57(3):279–296
Wali N, Leguire LE (1992) The photopic hill—a new phenomenon of the light adapted electroretinogram. Doc Ophthalmol 80(4):335–342
Severns ML, Johnson MA (1993) The care and fitting of Naka-Rushton functions to electroretinographic intensity-response data. Doc Ophthalmol 85(2):135–150
Sustar M, Stirn-Kranjc B, Hawlina M, Brecelj J (2008) Photopic on- and off-responses in complete type of congenital stationary night blindness in relation to stimulus intensity. Doc Ophthalmol 117(1):37–46
Dawson WW, Trick GL, Litzkow CA (1979) Improved electrode for electroretinography. Invest Ophth Vis Sci 18(9):988–991
Hebert M, Vaegan, Lachapelle P (1999) Reproducibility of ERG responses obtained with the DTL electrode. Vision Res 39 (6):1069–1070
Aguilar M, Stiles W (1954) Saturation of the rod mechanism of the retina at high levels of stimulation. Opt Acta 1:59–66
Birch DG, Fish GE (1987) Rod ERGs in retinitis pigmentosa and cone-rod degeneration. Invest Ophth Vis Sci 28(1):140–150
Fulton AB, Hansen RM (1988) Scotopic stimulus/response relations of the b-wave of the electroretinogram. Doc Ophthalmol 68(3–4):293–304
Peachey NS, Alexander KR, Fishman GA, Derlacki DJ (1989) Properties of the human cone system electroretinogram during light adaptation. Appl Opt 28(6):1145–1150
Hood DC, Shady S, Birch DG (1994) Understanding changes in the b-wave of the ERG caused by heterogeneous receptor damage. Invest Ophth Vis Sci 35(5):2477–2488
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Bland JM, Altman DG (1995) Multiple significance tests: the bonferroni method. Brit Med J 310(6973):170
Kondo M, Piao CH, Tanikawa A, Horiguchi M, Terasaki H, Miyake Y (2000) Amplitude decrease of photopic ERG b-wave at higher stimulus intensities in humans. Jpn J Ophthalmol 44(1):20–28
Rufiange M, Dumont M, Lachapelle P (2005) Modulation of the human photopic ERG luminance-response function with the use of chromatic stimuli. Vision Res 45(17):2321–2330
Rufiange M, Dassa J, Dembinska O, Koenekoop RK, Little JM, Polomeno RC, Dumont M, Chemtob S, Lachapelle P (2003) The photopic ERG luminance-response function (photopic hill): method of analysis and clinical application. Vision Res 43(12):1405–1412
Rufiange M, Rousseau S, Dembinska O, Lachapelle P (2002) Cone-dominated ERG luminance-response function: the photopic hill revisited. Doc Ophthalmol 104(3):231–248
Ueno S, Kondo M, Niwa Y, Terasaki H, Miyake Y (2004) Luminance dependence of neural components that underlies the primate photopic electroretinogram. Invest Ophthalmol Vis Sci 45(3):1033–1040
Rufiange M, Dassa J, Dembinska O, Koenekoop RK, Little JM, Polomeno RC, Dumont M, Chemtob S, Lachapelle P (2003) The photopic ERG luminance-response function (photopic hill): method of analysis and clinical application. Vision Res 43(12):1405–1412
Chen HL, Wu DZ, Huang SZ, Yan H (2006) The photopic negative response of the flash electroretinogram in retinal vein occlusion. Doc Ophthalmol 113(1):53–59
Birch DG, Anderson JL (1992) Standardized full-field electroretinography. Normal values and their variation with age. Arch Ophthalmol 110(11):1571–1576
Wali N, Leguire LE (1991) Dark-adapted luminance-response functions with skin and corneal electrodes. Doc Ophthalmol 76(4):367–375
Esakowitz L, Kriss A, Shawkat F (1993) A comparison of flash electroretinograms recorded from burian allen, jet, c-glide, gold foil, DTL and skin electrodes. Eye 7:169–171
Kriss A (1994) Skin ERGs—their effectiveness in pediatric visual assessment, confounding factors, and comparison with ERGs recorded using various types of corneal electrode. Int J Psychophysiol 16(2–3):137–146
McCulloch DL, Van Boemel GB, Borchert MS (1997) Comparisons of contact lens, foil, fiber and skin electrodes for pattern electroretinograms. Doc Ophthalmol 94(4):327–340
Bradshaw K, Hansen R, Fulton A (2004) Comparison of ERGs recorded with skin and corneal-contact electrodes in normal children and adults. Doc Ophthalmol 109(1):43–55
Birch DG, Herman WK, deFaller JM, Disbrow DT, Birch EE (1987) The relationship between rod perimetric thresholds and full-field rod ERGs in retinitis pigmentosa. Invest Ophthalmol Vis Sci 28(6):954–965
Acknowledgments
We would like to thank Fiona Duncan, Jeffery Tse and Sheryl Chung, who helped to collect some data for this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Binns, A.M., Mortlock, K.E. & North, R.V. The relationship between stimulus intensity and response amplitude for the photopic negative response of the flash electroretinogram. Doc Ophthalmol 122, 39–52 (2011). https://doi.org/10.1007/s10633-010-9257-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-010-9257-7