Abstract
Although a great deal of emphasis has been placed on the vasculopathy that is associated with oxygen-induced retinopathy (OIR), our studies also revealed significant and irreversible structural (retinal histology) and functional (scotopic and photopic electroretinograms) impairments that were significantly more severe in pigmented Long–Evans rats compared to the more commonly used albino Sprague Dawley rats. In the following pages, we will highlight what we have learned about the retinal pathophysiological processes of OIR taking place in strains of both rats with the hope that this will trigger investigations into new therapeutic strategies to complement those geared at preventing the vasculopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous studies of ours revealed that the structural (retinal histology) and functional (electroretinogram) deficits that resulted from the exposure of albino Sprague Dawley (SD) rats to a hyperoxic environment within the first postnatal days were permanent [1–5]. This contrasts with the damage to the retinal vasculature which can, as previously documented by others as well, overcome the hyperoxic challenge thereby achieving full coverage while still under oxygen throughout the first 2 weeks of life [1]. The latter is reminiscent of the reversible vasculopathy that is often reported in human ROP [6]. Recent studies of ours also showed that compared to the albino SD rats, pigmented Long-Evans (LE) rats developed a more severe oxygen-induced retinopathy (OIR) [7] as evidenced functionally and structurally. In the following pages, we will briefly review what we have learned from the two models of OIR with the hope that our findings will contribute to a better understanding of the retinal pathophysiological processes that are triggered following exposure of an immature retina to a high level of oxygen. For the sake of clarity, the results reported were obtained following an exposure to 80% oxygen for 22.5 h per day from P0 to P14.
Functional consequences of OIR
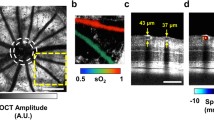
Functional impairments resulting from postnatal exposure to high oxygen are best summarized in Fig. 1 with representative examples of the saturated rod b-wave (a–c), the mixed rod-cone b-wave (d–f) and the photopic b-wave (g–i) parameters of the ERG obtained from control (a, d, g) and oxygen-exposed SD (b, e, h) and LE (c, f, i) rats. While, compared to control rats, the a-wave of the mixed rod-cone b-wave in SD rats was minimally affected following hyperoxic exposure (Fig. 1d, e), significant amplitude reduction in the scotopic (Fig. 1a, b, d, e) and photopic (Fig. 1g, h) ERG b-waves was observed.
Representative scotopic [saturated rod b-wave, flash intensity: −2.4 log cd.s.m−2 (a–c); and mixed rod-cone b-wave, flash intensity: 0.60 log cd.s.m−2 (d–f)] and photopic [b-wave, flash intensity: 0.9 log cd.s.m−2, background: 30 cd.m−2 (g–i)] ERGs obtained at P60 from LE rats raised in normoxia (21% O2) and LE and SD rats raised in hyperoxia (P0–P14, 80% O2), respectively. Calibrations: horizontal, 20 ms; vertical, 450 μV for scotopic saturated rod b-wave and mixed rod-cone b-wave ERG responses, 150 μV for photopic ERG responses. All tracings include a 20-ms prestimulus baseline; vertical arrows indicate flash onset. Representative retinal histological sections obtained at P60 from SD and LE rats raised in normoxic (j) and maximal hyperoxic conditions (k, l; SD and LE, respectively). RPE retinal pigment epithelium, OS outer segment, IS inner segment, ONL outer nuclear layer, OPL outer plexiform layer, INL inner nuclear layer, IPL inner plexiform layer, GCL ganglion cell layer. Calibration bar: 50 μm
It is interesting to note that the functional consequences of OIR in the SD rat, which is still to date the most commonly used strain, were significantly less severe than those observed in pigmented LE rats [7]. Briefly, while the a-wave remained relatively intact in SD rats, in LE rats it was found to be significantly compromised early on in the pathophysiology of OIR (Fig. 1f). Interestingly, as with the a-wave, the attenuation in the saturated rod b-wave response was notably more pronounced in LE rats (Fig. 1c). A comparable finding was also observed for the rod-cone b-wave of LE rats, where a significant attenuation in amplitude was observed (Fig. 1f). Similarly, attenuation of the photopic b-wave was also found to be significantly more pronounced in LE rats (Fig. 1i), suggesting again that the retinal function of LE rats is more prone to hyperoxic insult compared to that of SD rats.
Cytoarchitectural consequences of OIR
In SD rats, the only cytoarchitectural consequence of early postnatal hyperoxia found by our group was a dose-dependant thinning of the outer plexiform layer (OPL) along with a significant reduction in the horizontal cell count (Fig. 1k) [1–3]. In comparison, analysis of LE rat retinas revealed significantly more extensive damage to retinal cytoarchitecture compared to SD rats (Fig. 1l). In addition to the thinning of the OPL, we also noted a marked thinning of the inner nuclear layer (INL), the inner plexiform layer (IPL) and the outer nuclear layer (ONL; Fig. 1l), features of OIR never observed in SD rats that again point to the significantly more severe presentation of the OIR manifestations in LE rats.
Managing ROP: lessons from OIR
Our previous studies have shown that in albino SD rats, the pathophysiological consequences of OIR combine retinal cytoarchitectural damage (e.g. OPL thinning, reduced horizontal cell count) with a permanent deficit of retinal function (significantly attenuated scotopic and photopic ERGs) [1–5]. In comparison, postnatal hyperoxia exerts an even greater loss of retinal structure and function in the pigmented LE rat (greater vascular dropout, generalized deficit to retinal cytoarchitecture, more severely attenuated retinal function) [7]. Moreover, the damage observed in LE rats occurred earlier compared to SD rats, following exposure to hyperoxia that was limited to the first week of life (P0–P6).
Given that ROP is considered a disease of the retinal vasculature, it is not surprising to find that most studies on OIR have focused on the effect of postnatal hyperoxia on the development of the retinal vasculature. Although previous studies have also observed significant reductions in vascular coverage following postnatal hyperoxia in rats [8–14], few studies have examined the time course of this effect. We showed that despite the attenuation in vascular growth that is readily measurable after the first week of exposure (P0–P6) in SD rats, the vascular growth process is nonetheless able to overcome this hyperoxic insult thereby achieving full coverage while still under hyperoxic exposure (in P0–P14 exposures). This is reminiscent of the reversible vasculopathy that is observed in the human form of ROP [6]. In contrast, following oxygen exposure, the vascular supply is so severely compromised in pigmented LE rats that they never achieve a normal appearance, thus further suggesting unequal susceptibility among strains [7].
It is interesting to note that while the abnormal retinal vasculature has been documented to resolve itself, the functional sequelae that are associated with this disease have been shown to persist. Evidence of this has been published in several studies where, for example, significant alterations in the a- and b-waves of the ERG in patients with a history of ROP have been shown to continue into adulthood [15, 16]. Furthermore, scotopic visual threshold elevation has been documented in children with a history of resolved, mild ROP, thus suggesting the involvement of photoreceptors [17–19]. Finally, significant deficits in amplitude and implicit time of the multifocal ERG (mfERG) response, which stems from the central retina, have also been found in subjects who revealed complete resolution of clinical ROP more than 10–20 years earlier [20]. This would suggest that a history of ROP can alter the development of the central retina and, consequently, the mfERG response that it generates. Given that ON- and OFF-bipolar cells contribute to this central response, the attenuation in amplitude might therefore occur, should ROP specifically target these cells and thereby cause for an altered summation of depolarization and hyperpolarization in these subjects [20]. Therefore, despite the resolution of vascular abnormalities, which is a common occurrence in ROP patients, it is necessary to consider that neural dysfunction of the retina may still carry on throughout adulthood. Of course, this is not to say that the vasculopathy that results from postnatal hyperoxia does not contribute to the structural and functional consequences that we have reported. In a previous study by Penn’s et al. [12], it was shown that trolox-c (a water-soluble analogue of vitamin E) successfully limited the vascular consequences of postnatal hyperoxia, suggesting that hyperoxia was the main factor that triggered the vascular dropout observed in OIR. However, the same dose of trolox-c failed to offer an equivalent degree of protection to the retinal cytoarchitecture and function [5], suggesting again that some aspects of the vascular, structural and functional consequences of OIR may develop independently.
Our findings of impaired retinal function in our models of OIR support previous findings, where exposure of neonatal rats to 60% O2 from birth through P14 caused inner retinal dysfunction as evidenced by b-wave attenuation [21]. Similar findings also reported that cyclical (50/10% O2) exposure from P0 to P14 or constant exposure to 75% O2 from P7 to P14 led to postreceptoral functional deficits combined with retinal arteriole tortuosity [22]. Moreover, anomalies of the ERG oscillatory potentials (OPs) have also been shown to persist, despite the resolution of vascular abnormalities [3, 4, 23], which would further suggest the persistence of retinal functional deficits despite normalization of the retinal vasculature.
Evidence of a postreceptoral effect following postnatal hyperoxia were also reported by Penn et al. [21] where the amplitude of the ERG a-wave obtained from hyperoxic- and normoxic-cohorts were identical as of P21 and beyond, compared to severely attenuated b-waves. These results are also in line with those obtained by Reynaud et al. [9] who demonstrated that following postnatal hyperoxia from P0–P11, the amplitude of the a-wave gradually improved between P13 and P18, compared to that of the b-wave which remained significantly depressed at P18. Clearly, the above would suggest that the photoreceptors are significantly less susceptible to postnatal hyperoxia. One wonders whether this results from the relative immaturity of their outer segments at the time of oxygen exposure [24], or from the relatively intact choroidal vasculature that supplies them.The above would also further confirm that the more permanent sequelae of OIR occur in the inner retina. On the other hand, while the pathophysiological consequences of OIR are largely postreceptoral in the retina of albino rats, photoreceptor dysfunction may in fact also occur following exposure to hyperoxia, as suggested by different parameters of oxygen exposure including alternating between 50 and 10% oxygen from postnatal day P0–14, or exposure to 75% oxygen from P7 to P14 [22]. These findings would further support our observations of impaired photoreceptor function in the pigmented LE rat and would suggest that not all experimental models may react equally to an equivalent hyperoxic stress. Findings such as these warrant the evaluation of retinal structure, and studies of ours have also been geared towards better understanding of the impact of postnatal hyperoxia on retinal cytoarchitecture, which is often overlooked.
The cytoarchitectural manifestations of OIR occur, at least in the SD rat, during the period that the rats are still submitted to the hyperoxic regimen, as evidence of OPL thinning and HC count are already observed directly following exposure [1]. Furthermore, given that the most notable changes occur in the OPL and HCs, the relatively intact a-wave that can be recorded within the first few days following the cessation of hyperoxic exposure comes as little surprise, while as expected from histological findings, scotopic and photopic b-waves already tend to be attenuated in amplitude. Finally, whether the lower count of horizontal cells results from their susceptibility to oxygen (or to the relative hypoxia that follows hyperoxia) or from another degenerative process that might impact the establishment of proper synaptic connections remains to be fully understood.
Our recent findings have revealed that the pigmented Long–Evans rat is also a good working model of OIR, demonstrating a more exaggerated form of the disease with a more severe pathophysiological course, involving greater damage to retinal vasculature, structure and function. In both models, findings would suggest that OIR is initiated at a postreceptoral level, where synaptic impairment at the level of the OPL prevents signal transmission to the inner retina. The particular susceptibility of the scotopic and photopic b-waves would further support this inference [1–5, 7]. Involvement of other inner retinal structures such as the INL, IPL and GCL as well as the impaired a-wave in LE rats suggests that the pathophysiological consequences in this model are indeed more severe. Interestingly, studies have revealed that not only can an environmental stress such as exposure to hyperoxia result in structural damage to the retina, but other mechanisms that may involve the generation of reactive oxygen species, such as the reaction of iron with oxygen, can also result in such an effect. For example, intravitreal injection with FeSO4 has been shown to cause selective thinning of the ONL [25] as well as impaired retinal function. Similarly, intravitreous injection of paraquat (an herbicide known to generate reactive oxygen species) was shown to cause thinning of the ONL and INL along with vacuolization, folds in the ONL and functional impairment [26]. These findings in addition to those which we have previously reported [1–5, 7] would collectively suggest the importance not only of retinal vasculature and functional assessment in models of retinal diseases, namely OIR, but also of retinal cytoarchitecture which can give further insight and help to explain the pathophysiological processes that characterize OIR. Future investigations are certainly warranted in order to clarify the disparities between oxygen exposure regimens and the results obtained among studies in order to not only further our understanding of the disease processes but also to enable testing of new therapeutic modalities that could eventually help to manage human infants born with retinal disorders such as ROP as well as others. In that respect, if we interpret our results as evidence that not all premature infants will react similarly to the same hyperoxic shock, experimental approaches that would make use of the SD and LE rats would be instrumental in the design of new therapeutic strategies aimed at better protecting the developing retina from postnatal hyperoxia, irrespective of the degree of maturity reached at the time of oxygen exposure or the severity of the underlying retinopathy.
References
Dorfman A, Dembinska O, Chemtob S, Lachapelle P (2008) Early manifestations of postnatal hyperoxia on the retinal structure and function of the neonatal rat. Invest Ophthalmol Vis Sci 49:458–466
Lachapelle P, Dembinska O, Rojas LM, Benoit J, Almazan G, Chemtob S (1999) Persistent functional and structural retinal anomalies in newborn rats exposed to hyperoxia. Can J Physiol Pharmacol 77:48–55
Dembinska O, Rojas LM, Varma DR, Chemtob S, Lachapelle P (2001) Graded contribution of retinal maturation to the development of oxygen-induced retinopathy in rats. Invest Ophthalmol Vis Sci 42:1111–1118
Dembinska O, Rojas LM, Chemtob S, Lachapelle P (2002) Evidence for a brief period of enhanced oxygen susceptibility in the rat model of oxygen-induced retinopathy. Invest Ophthalmol Vis Sci 43:2481–2490
Dorfman AL, Dembinska O, Chemtob S, Lachapelle P (2006) Structural and functional consequences of trolox C treatment in the rat model of postnatal hyperoxia. Invest Ophthalmol Vis Sci 47:1101–1108
Hammer DX, Iftimia NV, Ferguson RD, Bigelow CE, Ustun TE, Barnaby AM, Fulton AB (2008) Foveal fine structure in retinopathy of prematurity: an adaptive optics Fourier domain optical coherence tomography study. Invest Ophthalmol Vis Sci 49:2061–2070
Dorfman AL, Polosa A, Joly S, Chemtob S, Lachapelle P (2009) Functional and structural changes resulting from strain differences in the rat model of OIR. Invest Ophthalmol Vis Sci 50:2436–2450
Hardy P, Peri KG, Lahaie I, Varma DR, Chemtob S (1996) Increased nitric oxide synthesis and action preclude choroidal vasoconstriction to hyperoxia in newborn pigs. Circ Res 79:504–511
Reynaud X, Dorey CK (1994) Extraretinal neovascularization induced by hypoxic episodes in the neonatal rat. Invest Ophthalmol Vis Sci 35:3169–3177
Penn JS, Thum LA, Naash MI (1992) Oxygen-induced retinopathy in the rat: vitamins C and E as potential therapies. Invest Ophthalmol Vis Sci 33:1836–1845
Penn JS, Tolman BL, Henry MM (1994) Oxygen-induced retinopathy in the rat: relationship of retinal nonperfusion to subsequent neovascularization. Invest Ophthalmol Vis Sci 35:3429–3435
Penn JS, Tolman BL, Bullard LE (1997) Effect of a water-soluble vitamin E analog, trolox C, on retinal vascular development in an animal model of retinopathy of prematurity. Free Radic Biol Med 22:977–984
Benjamin LE, Hemo I, Keshet E (1998) A plasticity window for blood vessel remodelling is defined by pericyte coverage of the preformed endothelial network and is regulated by PDGF-B and VEGF. Development 125:1591–1598
Hardy P, Beauchamp M, Sennlaub F, Gobeil F Jr, Tremblay L, Mwaikambo B, Lachapelle P, Chemtob S (2005) New insights into the retinal circulation: inflammatory lipid mediators in ischemic retinopathy. Prostaglandins Leukot Essent Fatty Acids 72:301–325
Fulton AB, Hansen RM (1996) Photoreceptor function in infants and children with a history of mild retinopathy of prematurity. J Opt Soc Am A Opt Image Sci Vis 13:566–571
Fulton AB, Hansen RM, Petersen RA, Vanderveen DK (2001) The rod photoreceptors in retinopathy of prematurity: an electroretinographic study. Arch Ophthalmol 119:499–505
Hansen RM, Fulton AB (2000) Background adaptation in children with a history of mild retinopathy of prematurity. Invest Ophthalmol Vis Sci 41:320–324
Reisner DS, Hansen RM, Findl O, Petersen RA, Fulton AB (1997) Dark adapted thresholds in children with histories of mild retinopathy of prematurity. Invest Ophthalmol Vis Sci 38:1175–1183
Barnaby AM, Hansen RM, Moskowitz A, Fulton AB (2007) Development of scotopic visual thresholds in retinopathy of prematurity. Invest Ophthalmol Vis Sci 48:4854–4860
Fulton AB, Hansen RM, Moskowitz A, Barnaby AM (2005) Multifocal ERG in subjects with a history of retinopathy of prematurity. Doc Ophthalmol 111:7–13
Penn JS, Thum LA, Rhem MN, Dell SJ (1988) Effects of oxygen rearing on the electroretinogram and GFA-protein in the rat. Invest Ophthalmol Vis Sci 29:1623–1630
Akula JD, Hansen RM, Martinez-Perez ME, Fulton AB (2007) Rod photoreceptor function predicts blood vessel abnormality in retinopathy of prematurity. Invest Ophthalmol Vis Sci 48:4351–4359
Liu K, Akula JD, Hansen RM, Moskowitz A, Kleinman MS, Fulton AB (2006) Development of the electroretinographic oscillatory potentials in normal and ROP rats. Invest Ophthalmol Vis Sci 47:5447–5452
Weidman TA, Kuwabara T (1968) Postnatal development of the rat retina. An electron microscopic study. Arch Ophthalmol 79:470–484
Rogers BS, Symons RC, Komeima K, Shen J, Xiao W, Swaim ME, Gong YY, Kachi S, Campochiaro PA (2007) Differential sensitivity of cones to iron-mediated oxidative damage. Invest Ophthalmol Vis Sci 48:438–445
Cingolani C, Rogers B, Lu L, Kachi S, Shen J, Campochiaro PA (2006) Retinal degeneration from oxidative damage. Free Radic Biol Med 40:660–669
Acknowledgments
This study was supported by a research grant (MOP-13383) from the Canadian Institutes of Health Research (CIHR), from the FRSQ-Réseau Vision as well as from the McGill University-Montreal Children’s Hospital Research Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dorfman, A.L., Chemtob, S. & Lachapelle, P. Postnatal hyperoxia and the developing rat retina: beyond the obvious vasculopathy. Doc Ophthalmol 120, 61–66 (2010). https://doi.org/10.1007/s10633-009-9208-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-009-9208-3