Abstract
Background
The comparative long-term survival of first-line biologics for UC and reasons for drug discontinuation are poorly understood. We sought to compare the long-term drug survival related to non-response (NR) and adverse effects (AEs) for vedolizumab, adalimumab, and infliximab among biologic-naïve patients with UC.
Methods
This was a retrospective cohort study of adult biologic-naïve patients with moderate-to-severe UC initiating vedolizumab, adalimumab, or infliximab 6/1/14–12/31/20 at a large academic medical center. The primary outcome was time to biologic discontinuation for primary or secondary NR (including colectomy). The secondary outcome was time to biologic discontinuation due to AEs. Inverse probability of treatment-weighted (IPTW) Cox regression was used to perform three pair-wise comparisons of drug survival.
Results
The cohort included 805 patients with UC who initiated vedolizumab (n = 195), adalimumab (n = 278), or infliximab (n = 332). The adjusted hazard of biologic discontinuation for NR was significantly lower for vedolizumab vs adalimumab (HR 0.51, 95% CI 0.34–0.75), similar for vedolizumab vs infliximab (HR 1.32, 95% CI 0.79–2.18), and greater for adalimumab vs infliximab (HR 2.07, 95% CI 1.51–2.86). The adjusted hazard of discontinuation for AEs was significantly lower for vedolizumab vs adalimumab (HR 0.25, 95% CI 0.09–0.64), lower for vedolizumab vs infliximab (HR 0.21, 95% CI 0.10–0.46), and similar for adalimumab vs infliximab (HR 0.85, 95% CI 0.53–1.35).
Conclusions
There was greater survival of vedolizumab compared to adalimumab for clinical response and greater survival of vedolizumab compared to both adalimumab and infliximab for AEs. These long-term data support the use of vedolizumab as a first-line biologic over adalimumab for biologic-naïve patients with UC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biologic therapy is essential to the management of moderate-to-severe ulcerative colitis (UC) [1]. According to clinical guidelines, first-line biologic agents for UC include vedolizumab, a gut-selective integrin antagonist, and the more systemically active anti-tumor necrosis factor α (TNFα) agent infliximab [2]. Adalimumab can be considered as an alternative first-line anti-TNFα agent [2]. This positioning was influenced by the only head-to-head clinical trial of biologics in UC, which demonstrated the superiority of vedolizumab to adalimumab in achieving clinical remission, but not corticosteroid-free clinical remission, at 52 weeks [3]. Singh and colleagues [4] conducted a systematic review and network meta-analysis of clinical trials that identified infliximab as the preferred biologic for induction of remission in biologic-naïve patients with UC. However, when considering diverse patient characteristics and risk factors that are poorly represented in clinical trials, the optimal real-world positioning of these agents is unclear.
In contrast to Singh et al. [4], real-world comparative data of first-line biologics in UC suggest similar or better clinical efficacy of vedolizumab compared to anti-TNFα agents. Several small, retrospective studies with 12 or fewer months of follow-up reported no differences in clinical efficacy [5,6,7,8]. A recent multinational study of biologic-naïve patients found greater treatment persistence, fewer disease exacerbations, and similar rates of adverse events at 24 months with vedolizumab compared to anti-TNFα agents [9]. However, most real-world studies with long-term follow-up have not analyzed infliximab and subcutaneous anti-TNFα agents separately, likely due to sample size limitations [5, 9,10,11,12,13,14].
A growing body of evidence suggests that vedolizumab is more clinically effective and safer in the biologic-naïve than in individuals with prior anti-TNFα exposure [15,16,17,18,19]. Therefore, a better understanding of the relative long-term durability of vedolizumab as a first-line agent is imperative to optimize its positioning and therapeutic potential. To address this need, we performed a real-world retrospective cohort study comparing the long-term drug survival of vedolizumab, adalimumab, and infliximab initiated between 2014 and 2020 among biologic-naïve patients with UC. We separately assessed drug survival related to non-response (NR) and drug survival related to adverse effects (AEs). We also compared reasons for biologic discontinuation and proportions of clinical and endoscopic remission at 24 and 48 months.
Materials and Methods
Study Design and Patient Selection
This was a retrospective cohort study of adult biologic-naïve patients with UC (ICD-10-CM 51x) who initiated vedolizumab, adalimumab, or infliximab between 6/1/2014–12/31/3020 at Brigham and Women’s Hospital (Boston, MA, USA), Massachusetts General Hospital (Boston, MA, USA), or affiliate hospitals (MA, USA). Electronic health records were manually reviewed for clinical, endoscopic, prescription, and laboratory data. Patients were initiated on biologic therapy per provider assessment of moderate-to-severe UC, which could include endoscopic, biochemical, and/or clinical parameters. Patients with Crohn’s disease, inflammatory bowel disease unclassified (IBDU), prior biologic exposures or colectomy, and those who initiated biologic agents for non-UC indications were excluded. Patients were followed until biologic discontinuation or the last available gastroenterology encounter through 8/1/21, which was the pre-set end date of eligible clinical data for chart review. The date of biologic discontinuation was defined as the earliest of the following: the first missed due date of biologic administration among those with at least two consecutive missed doses, the date of switch to a new biologic agent, or colectomy. The primary documented reason for biologic discontinuation was extracted from gastroenterology clinic notes (Supplementary Methods).
Outcomes
The primary outcome was time from biologic initiation to discontinuation due to primary or secondary NR. For this outcome, patients who required colectomy for refractory UC within 6 weeks after biologic initiation (i.e., prior to completion of induction) were excluded. This strategy eliminates bias from the most refractory cases of acute severe UC where infliximab is disproportionately utilized in our health system. The secondary outcome was time to biologic discontinuation due to an adverse effect (AE), which was extracted from gastroenterology clinic notes. Specific AEs that led to biologic discontinuation were characterized as any of the following: acute reaction (onset of symptoms within 24 h of administration, including anaphylaxis), joint/soft tissue (arthralgia, arthritis, myalgias, soft tissue swelling, or lupus-like reactions), subacute rash (onset > 24 h after administration), infection, elevated liver enzymes, neurologic (headache, seizure, or sensory disturbance), malignancy, pulmonary (pneumonitis or interstitial lung disease), renal (interstitial nephritis), vascular (vasculitis or thromboembolism), weight gain, and other non-acute signs or symptoms reported.
Additional outcomes included corticosteroid-free clinical remission (CFCR) and deep remission (DR; defined as CFCR with endoscopic mucosal healing with Mayo endoscopic subscore ≤ 1) at 24 months and 48 months after biologic initiation. CFCR was defined as no use of systemic corticosteroids or oral budesonide for at least 30 days after achieving clinical remission (simple clinical colitis activity index [SCCAI] ≤ 2, 9-point Mayo score ≤ 2, or gastroenterology provider documentation of “remission” when the aforementioned indices were not documented). Due to variability in timing of clinical and endoscopic assessments, 24 and 48 month outcomes were based on the closest available data within 6 months of these endpoints. However, only patients with a minimum of 24 and 48 months of potential follow-up between biologic initiation and 8/1/21 were eligible for these outcome assessments. Patients who discontinued therapy due to an AE prior to these time points and those who underwent colectomy for refractory disease within 6 weeks after biologic initiation were ineligible for these outcomes. Lastly, data were obtained regarding the primary documented reason for biologic discontinuation (Supplementary Methods) and regarding dose escalation, defined as any dose increase or dose interval reduction of the biologic for at least two consecutive doses.
Independent Variables
The primary exposure was choice of biologic (vedolizumab, adalimumab, or infliximab). Other baseline independent variables included demographics, concomitant medications (corticosteroids and immunomodulators), Mayo endoscopic subscore, disease extent, and other factors related to IBD severity (Supplementary Methods).
Statistical Analysis
Continuous and categorical data were compared using the Kruskal–Wallis and Chi-squared tests, respectively. Kaplan–Meier (KM) analyses with log-rank tests stratified by biologic therapy were performed for overall drug survival and time to discontinuation for NR and AEs. Patients were censored at loss of follow-up, biologic discontinuation for reasons other than the outcome being assessed, colectomy, or death.
To adjust for treatment selection bias, inverse probability of treatment weighting (IPTW) using propensity scores was performed for the three pairwise comparisons of vedolizumab vs adalimumab, vedolizumab vs infliximab, and adalimumab vs infliximab. IPTW was preferred over propensity score matching in order to maximize the statistical power for each comparison. Propensity scores were calculated using logistic regression of biologic choice on the following covariates selected a priori: age, sex, Caucasian race, BMI, disease duration > 5 years (dichotomized using median value), concomitant corticosteroid use (prednisone, methylprednisolone, or oral budesonide) at the time of biologic initiation, concomitant immunomodulator use, any UC-related hospitalization within the prior 12 months, last Mayo endoscopic subscore (3 versus < 3), last Montreal disease extent (> E1 versus ≤ E1), serum albumin, and history of malignancy. Covariate balance was assessed using standardized mean differences. SCCAI was excluded from propensity score calculations due to missing data in > 20% of the sample; however a sensitivity analysis was performed with SCCAI added as a separate covariate to the IPTW Cox regression models for NR. Propensity scores involving vedolizumab also incorporated biologic initiation two years after the date of FDA approval (May 20, 2014) of vedolizumab as a binary covariate to account for the delay in uptake of vedolizumab prescribing. Two years was specifically chosen as more than 90% of vedolizumab-treated patients in the cohort were prescribed the biologic after this time. The proportional hazards assumption was confirmed using Schoenfeld residuals.
Unadjusted and adjusted odds ratios were calculated using logistic regression of unweighted and IPT-weighted samples to determine the associations between choice of biologic with CFCR and DR at 24 and 48 months. P-values below 0.05 were considered statistically significant. Data regarding treatment discontinuation, types of AEs, and dose escalation are intended to be descriptive, and therefore p-values were not calculated. STATA/SE 17.0 (College Station, TX) was used for all analyses.
Results
Cohort Characteristics
The cohort included 805 patients with UC who initiated vedolizumab (n = 195), adalimumab (n = 278), or infliximab (n = 332). There were significant differences in age, BMI, malignancy history, concomitant immunomodulator and corticosteroid use, endoscopic inflammation and extent, albumin, CRP, bowel frequency, SCCAI, and UC hospitalizations within 12 months prior to biologic initiation (Table 1).
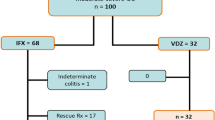
Drug Survival
The proportions of patients who discontinued therapy during follow-up were 76/195 (39.0%) for vedolizumab, 180/278 (64.8%) for adalimumab, and 175/332 (52.7%) for infliximab. Median time until discontinuation or censoring was 587 (IQR 254–956) days for vedolizumab, 286.5 (119–1132) days for adalimumab, and 473.5 (IQR 165–1063.5) days for infliximab. Among those who discontinued therapy (431/805), the common reasons were NR (63.8%), AEs (26.0%), and non-adherence (5.3%) (Fig. 1).
KM analysis of overall drug survival demonstrated the greatest drug survival for vedolizumab (log-rank test p < 0.01; Fig. 2a). KM analysis for NR demonstrated greater drug survival of vedolizumab and infliximab relative to adalimumab (log-rank test p < 0.01; Fig. 2b) and KM analysis for AEs demonstrated the greatest drug survival for vedolizumab (log-rank test p < 0.01; Fig. 2c). Among those who discontinued therapy for AEs (n = 112), the most common reported AEs were joint/soft tissue (21.4%), acute reaction (18.8%), and subacute rash (18.8%) (Fig. 3). No adverse effects in this study were associated with patient death.
There were complete covariate data for 728/805 (90.4%) patients. Covariate balance after IPTW was confirmed with < 10% absolute standardized differences across all covariates (Fig. 4). For the NR analysis, an additional 13 patients (1 vedolizumab, 1 adalimumab, 11 infliximab) were excluded due to colectomy within 6 weeks after biologic initiation. The IPTW Cox models demonstrated a significantly lower hazard of discontinuation for NR for vedolizumab vs adalimumab (HR 0.51, 95% CI 0.34–0.75), greater hazard for adalimumab vs infliximab (HR 2.08, 95% CI 1.51–2.86), and similar hazard for vedolizumab vs infliximab (HR 1.32, 95% CI 0.79–2.18). The sensitivity analysis for NR, which added SCCAI as a covariate in the IPTW Cox models, demonstrated similar results for vedolizumab vs adalimumab (HR 0.53, 95% CI 0.35–0.82) and adalimumab vs infliximab (2.62, 95% CI 1.78–3.86), but a significantly greater hazard for vedolizumab vs infliximab (2.14, 95% CI 1.17–3.93).
For the AE analysis, IPTW Cox models demonstrated significantly lower hazard of discontinuation for vedolizumab vs adalimumab (HR 0.25, 95% CI 0.09–0.64), similar hazard for adalimumab vs infliximab (HR 0.85, 95% CI 0.53–1.35), and lower hazard for vedolizumab vs infliximab (HR 0.21, 95% CI 0.10–0.46). The complete unweighted and weighted Cox proportional hazard models for NR and AEs are presented in Table 2.
24- and 48-Month Outcomes
Proportions of eligible patients achieving CFCR at 24 months were 61/104 (58.7%) for vedolizumab, 74/182 (40.7%) for adalimumab, and 112/178 (62.9%) for infliximab (p < 0.01). Proportions for deep remission at 24 months proportions were 38/89 (41.8%) for vedolizumab, 61/177 (34.5%) for adalimumab, and 76/153 (49.7%) for infliximab (p = 0.021). Proportions for CFCR at 48 months were 12/23 (52.2%) for vedolizumab, 31/103 (30.1%) for adalimumab, and 45/87 (51.7%) for infliximab (p < 0.01). Proportions for deep remission at 48 months were 10/22 (45.5%) for vedolizumab, 18/90 (20.0%) for adalimumab, and 28/73 (38.4%) for infliximab (p < 0.01) (Fig. 5).
24- and 48-month outcomes. For CFCR at 24 months, eligible n = 104 vedolizumab, 182 adalimumab, 178 infliximab. For DR at 24 months, eligible n = 89 vedolizumab, 177 adalimumab, 153 infliximab. For CFCR at 48 months, eligible n = 23 vedolizumab, 103 adalimumab, 87 infliximab. For DR at 48 months, eligible n = 22 vedolizumab, 90 adalimumab, 73 infliximab. Abbreviations: CFCR = corticosteroid-free clinical remission, DR = deep remission
For vedolizumab vs adalimumab, IPTW logistic regression demonstrated significantly greater odds of CFCR at 24 months (OR 1.99, 95% CI 1.11–3.54) and deep remission at 48 months (OR 4.06, 95% CI 1.28–12.94). For adalimumab vs infliximab, there was significantly lower odds of CFCR at 24 months (OR 0.39, 95% CI 0.24–0.64), DR at 24 months (0.50, 95% CI 0.30–0.83), CFCR at 48 months (OR 0.44, 95% CI 0.22–0.86), and DR at 48 months (OR 0.34, 95% CI 0.16–0.76). Other biologic comparisons for CFCR and DR at 24 months and 48 months (Supplementary Table) were not statistically significant.
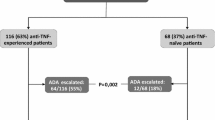
Dose Escalation
Proportions of patients who underwent dose escalation during follow-up were 79/195 (40.5%) after a median of 110 days (IQR 57–274 days) for vedolizumab, 101/278 (36.3%) after a median of 138 days (IQR 65–358 days) for adalimumab, and 210/332 (63.3%) after a median of 207 days (IQR 133.5–410 days) for infliximab.
Discussion
In this real-world study with up to 6 years of clinical follow-up, vedolizumab demonstrated the greatest overall drug survival for biologic-naïve patients with UC. When considering drug survival related only to NR, vedolizumab was superior to adalimumab, infliximab was superior to adalimumab, and vedolizumab was similar to infliximab after IPTW to control for treatment selection bias. In our sensitivity analysis that also controlled for baseline SCCAI (for the subset of patients with this data available), results were similar except infliximab was found to be superior to vedolizumab, which could represent residual confounding by indication for this comparison of NR. However, like other clinical disease activity scores, the SCCAI is comprised of subjective, patient-reported data that may be less reliable than other covariates.
When considering drug survival related only to AEs, which is likely less susceptible to confounding by indication, vedolizumab was superior to both adalimumab and infliximab. Vedolizumab therapy was also associated with a greater weighted odds of CFCR at 24 months and DR at 48 months when compared to adalimumab but performed similarly to infliximab. Adalimumab was associated with a lower weighted odds of CFCR and DR compared to infliximab at both time points. The lower rate of AEs with vedolizumab compared to adalimumab is not felt to be related to the higher rate of CFCR with vedolizumab, as patients who discontinued therapy due to an AE prior to 24 or 48 months were not eligible for the analysis of the corresponding CFCR and DR outcomes.
Few real-world UC studies to-date have examined differences in long-term efficacy between vedolizumab and specific anti-TNFα therapies for the biologic-naïve [10, 12, 19]. In the multicenter cohort study by Lukin et al. [10], vedolizumab-treated patients achieved CFCR and DR at higher rates compared to infliximab and sub-cutaneous anti-TNFα therapies. However, only 303/722 (41.9%) patients were biologic-naïve, limiting conclusions that can be drawn for this population. CFCR and DR were also assessed as time-to-event analyses, which may introduce bias. Retrospective study designs are subject to inaccuracies in the time of remission outcomes, as they depend entirely on the scheduling of follow-up clinical assessments that may vary due to patient, provider, and institutional factors. Patients may therefore achieve clinical remission several weeks before it is documented in a clinic visit. For this reason, we chose discrete events (i.e., date of biologic discontinuation) for our survival analyses that maximized precision.
A recent population-based registry study in Australia compared the 12-month persistence of vedolizumab, adalimumab, and infliximab among 864 patients with UC, among which 632 were biologic-naïve [19]. Similar to our findings, vedolizumab demonstrated the greatest treatment persistence. However, in line with the limitations of other database studies, the authors were unable to determine the specific reasons for drug discontinuation and baseline disease severity variables with known prognostic impact, such as corticosteroid use, endoscopic inflammation, disease activity scores, or biochemical markers, which may confound their results [20, 21].
Our study has several strengths. We include separate comparisons of treatment persistence for vedolizumab versus specific anti-TNFα agents, whereas many similar studies to-date have compared only classes of biologic therapy [5, 9, 11, 14]. Consequently, our study identified differential treatment persistence by specific agents within the anti-TNFα class. Unlike other studies of overall treatment persistence, this study also distinguished persistence related to NR and persistence related to AEs. We were able to include specific variables related to baseline UC activity such as endoscopic severity and extent, BMI, and albumin, among other factors which were not available in prior database studies that have attempted to answer similar questions [5, 12]. While there were differences in baseline factors that likely represent clinically significant differences in disease severity, IPTW successfully balanced these covariates to minimize confounding by indication in our regression analyses. We also provided granular detail regarding specific AEs that led to treatment discontinuation, which improves our understanding about the real-world risks associated with first-line biologics. Studies that report serious AEs may utilize inconsistent and subjective definitions for this outcome, whereas AEs leading to biologic discontinuation may be less prone to bias.
Limitations include the retrospective design and potential for missing data, though there were complete covariate data for > 90% of the cohort. The study took place at a large, urban academic referral center, and therefore results may be less generalizable to other settings. Assessment of baseline characteristics suggests significantly greater disease severity in the infliximab group compared to adalimumab and vedolizumab. While covariates were balanced after IPTW, unmeasured confounding may still exist. To further mitigate confounding by indication, the NR analysis excluded patients with failure of therapy within the first 6 weeks. This limits potential bias against infliximab, which, due to its rapid onset of action, is utilized disproportionately for patients with acute severe colitis who may be more likely to fail all medical therapies. While the overall cohort is large (n = 805), results of the 48-month outcome analyses are subject to type II error, as only 213 patients were eligible among which 23 were treated with vedolizumab. Finally, the study lacks detailed data regarding therapeutic drug monitoring, which should be prioritized in future prospective studies.
Conclusion
In summary, this study identified greater drug survival of vedolizumab compared to adalimumab but not infliximab for NR and greater drug survival of vedolizumab compared to both adalimumab and infliximab for AEs. Vedolizumab was also associated with greater odds of CFCR at 24 months and DR at 48 months compared to adalimumab but not infliximab. Infliximab was superior to adalimumab for drug survival related to NR and CFCR and DR at 24 and 48 months. These long-term data support the use of vedolizumab as a first-line biologic over adalimumab while suggesting differential durability and efficacy within the anti-TNFα class for biologic-naïve patients with UC.
References
Mao EJ, Hazlewood GS, Kaplan GG, Peyrin-Biroulet L, Ananthakrishnan AN. Systematic review with meta-analysis: comparative efficacy of immunosuppressants and biologics for reducing hospitalisation and surgery in Crohn’s disease and ulcerative colitis. Aliment Pharmacol Ther. 2017;45:3–13. https://doi.org/10.1111/apt.13847.
Feuerstein JD, Isaacs KL, Schneider Y et al. AGA Clinical Practice Guidelines on the Management of Moderate to Severe Ulcerative Colitis. Gastroenterology. 2020;158:1450–1461. https://doi.org/10.1053/j.gastro.2020.01.006.
Sands BE, Peyrin-Biroulet L, Loftus EV et al. Vedolizumab versus Adalimumab for Moderate-to-Severe Ulcerative Colitis. N Engl J Med. 2019;381:1215–1226. https://doi.org/10.1056/NEJMoa1905725.
Singh S, Murad MH, Fumery M, Dulai PS, Sandborn WJ. First- and Second-Line Pharmacotherapies for Patients With Moderate to Severely Active Ulcerative Colitis: An Updated Network Meta-Analysis. Clin Gastroenterol Hepatol. 2020;18:2179-2191.e6. https://doi.org/10.1016/j.cgh.2020.01.008.
Helwig U, Mross M, Schubert S et al. Real-world clinical effectiveness and safety of vedolizumab and anti-tumor necrosis factor alpha treatment in ulcerative colitis and Crohn’s disease patients: a German retrospective chart review. BMC Gastroenterol. 2020;20:211. https://doi.org/10.1186/s12876-020-01332-w.
Davis R, McParland P, Dodd S et al. Comparative effectiveness of antitumour necrosis factor agents and vedolizumab in ulcerative colitis. Eur J Gastroenterol Hepatol. 2019;31:661–667. https://doi.org/10.1097/MEG.0000000000001395.
Allamneni C, Venkata K, Yun H, Xie F, DeLoach L, Malik TA. Comparative Effectiveness of Vedolizumab vs. Infliximab Induction Therapy in Ulcerative Colitis: Experience of a Real-World Cohort at a Tertiary Inflammatory Bowel Disease Center. Gastroenterology Res. 2018;11:41–45.https://doi.org/10.14740/gr934w
Adar T, Faleck D, Sasidharan S et al. Comparative safety and effectiveness of tumor necrosis factor α antagonists and vedolizumab in elderly IBD patients: a multicentre study. Aliment Pharmacol Ther. 2019;49:873–879. https://doi.org/10.1111/apt.15177.
Bressler B, Yarur A, Silverberg MS et al. Vedolizumab and Anti-TNFα Real-World Outcomes in Biologic-Naïve Inflammatory Bowel Disease Patients: Results from the EVOLVE Study. J Crohns Colitis. 2021. https://doi.org/10.1093/ecco-jcc/jjab058.
Lukin D, Faleck D, Xu R et al. Comparative Safety and Effectiveness of Vedolizumab to Tumor Necrosis Factor Antagonist Therapy for Ulcerative Colitis. Clin Gastroenterol Hepatol. 2020. https://doi.org/10.1016/j.cgh.2020.10.003.
Kochar B, Pate V, Kappelman MD et al. Vedolizumab Is Associated With a Lower Risk of Serious Infections Than Anti-TNF Agents in Older Adults. Clin Gastroenterol Hepatol. 2021. https://doi.org/10.1016/j.cgh.2021.08.047.
Patel H, Latremouille-Viau D, Burne R, Shi S, Adsul S. Comparison of Real-World Treatment Outcomes With Vedolizumab Versus Infliximab in Biologic-Naive Patients With Inflammatory Bowel Disease. Crohn's & Colitis 360. 2019;1.https://doi.org/10.1093/crocol/otz022
Kopylov U, Verstockt B, Biedermann L et al. Effectiveness and Safety of Vedolizumab in Anti-TNF-Naïve Patients With Inflammatory Bowel Disease-A Multicenter Retrospective European Study. Inflamm Bowel Dis. 2018;24:2442–2451. https://doi.org/10.1093/ibd/izy155.
Rundquist S, Sachs MC, Eriksson C et al. Drug survival of anti-TNF agents compared with vedolizumab as a second-line biological treatment in inflammatory bowel disease: results from nationwide Swedish registers. Aliment Pharmacol Ther. 2021;53:471–483. https://doi.org/10.1111/apt.16193.
Feagan BG, Rubin DT, Danese S et al. Efficacy of Vedolizumab Induction and Maintenance Therapy in Patients With Ulcerative Colitis, Regardless of Prior Exposure to Tumor Necrosis Factor Antagonists. Clin Gastroenterol Hepatol. 2017;15:229-239.e5. https://doi.org/10.1016/j.cgh.2016.08.044.
Narula N, Peerani F, Meserve J et al. Vedolizumab for Ulcerative Colitis: Treatment Outcomes from the VICTORY Consortium. Am J Gastroenterol. 2018;113:1345. https://doi.org/10.1038/s41395-018-0162-0.
Colombel J-F, Sands BE, Rutgeerts P et al. The safety of vedolizumab for ulcerative colitis and Crohn’s disease. Gut. 2017;66:839–851. https://doi.org/10.1136/gutjnl-2015-311079.
Barré A, Colombel J-F, Ungaro R. Review article: predictors of response to vedolizumab and ustekinumab in inflammatory bowel disease. Aliment Pharmacol Ther. 2018;47:896–905. https://doi.org/10.1111/apt.14550.
Ko Y, Paramsothy S, Yau Y, Leong RW. Superior treatment persistence with ustekinumab in Crohn’s disease and vedolizumab in ulcerative colitis compared with anti-TNF biological agents: real-world registry data from the Persistence Australian National IBD Cohort (PANIC) study. Aliment Pharmacol Ther. 2021;54:292–301. https://doi.org/10.1111/apt.16436.
Khan N, Patel D, Shah Y, Trivedi C, Yang YX. Albumin as a prognostic marker for ulcerative colitis. World J Gastroenterol. 2017;23:8008–8016. https://doi.org/10.3748/wjg.v23.i45.8008.
Dalal RS, Osterman MT, Buchner AM, Praestgaard A, Lewis JD, Lichtenstein GR. A User-Friendly Prediction Tool to Identify Colectomy Risk in Patients With Ulcerative Colitis. Inflamm Bowel Dis. 2019. https://doi.org/10.1093/ibd/izz014.
Funding
This study was funded in part by the National Institute of Diabetes and Digestive and Kidney Diseases (5T32DK007533-35 to R.S.D.). JRA serves as a consultant for Takeda, Janssen, Pfizer, Pandion, Servatus, Finch Therapeutics, Iterative Scopes and Artugen and has grant support from Merck.
Author information
Authors and Affiliations
Contributions
RSD was involved in the study concept and design, acquisition of data, statistical analysis, analysis and interpretation of data, and drafting of manuscript. EM and JM contributed to the acquisition of data. JRA contributed to the study concept and design, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and study supervision.
Corresponding author
Ethics declarations
Conflict of interest
RSD, EM, and JM have no financial or personal conflicts of interest to disclose.
Ethical approval
This study was approved by the institutional review board of Brigham and Women’s Hospital (Boston, MA, USA). All authors have approved the final version of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dalal, R.S., McClure, E.L., Marcus, J. et al. Comparative Long-Term Drug Survival of Vedolizumab, Adalimumab, and Infliximab in Biologic-Naïve Patients with Ulcerative Colitis. Dig Dis Sci 68, 223–232 (2023). https://doi.org/10.1007/s10620-022-07472-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07472-1