Abstract
Background
Colorectal cancer (CRC) is the third most common malignancy and the second leading cause of cancer-related death in the world. The aim of this study was to investigate the geographic distribution and time trends of CRC in Brazil.
Methods
Data were retrospectively retrieved from January 2005 to December 2018 from the Brazilian Public Health System. The incidence and lethality rates of CRC per 100,000 inhabitants in each municipality were estimated from hospitalizations and in-hospital deaths and were classified by age, sex, and demographic features.
Results
During the study period, the mean incidence of CRC estimated from hospitalizations and adjusted to available hospital beds more than tripled from 14.6 to 51.4 per 100,000 inhabitants (352%). Increases in CRC incidence were detected in all age ranges, particularly among people aged 50–69 years (266%). Incidence rates increased in all 5 macroregions, with a clear South to North gradient. The greatest changes in incidence and lethality rates were registered in small-sized municipalities. CRC lethality estimated from in-hospital deaths decreased similarly in both sexes, from 12 to 8% for males and females, from 2005 to 2018. The decline in lethality rates was seen in all age ranges, mainly in people aged 50 to 69 years (− 38%).
Conclusions
CRC incidence is increasing, predominantly above fifty years of age, and also in areas previously considered as having low incidence, but the increase is not paralleled by lethality rates. This suggests recent improvements in CRC screening programs and treatment, but also supports the spread of environmental risk factors throughout the country.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) has been considered an emerging disease of this century, representing the third most commonly diagnosed malignancy in males and the second most commonly diagnosed malignancy in females [1]. Nevertheless, the overall CRC frequency presents broad variations among countries and geographic regions, but usually the highest incidence rates are reported in the more developed countries [2, 3].
Data from different studies have supported a relationship between the human development index (HDI), which consists of a combination of longevity, knowledge, and income, and the incidence and mortality rates of several types of cancer [4, 5], including CRC [6]. Aging alone has also been associated with CRC [7]. Nevertheless, CRC incidence has been rising consistently in people under the age of 50 over the last 20 years in Canada and the USA [8, 9]. Moreover, recent studies indicate that CRC incidence rates are rising rapidly in developing countries, particularly in Eastern Europe, Asia, and South America, where mortality rates tend to be proportionally higher [10, 11]. This has been attributed to the low availability of screening tests for CRC in less developed countries [12, 13].
The global rise in CRC incidence has been mainly associated with exposure to environmental risk factors, including changes referred to as westernization of the lifestyle. Such lifestyle modifications are usually associated with industrialization and economic development and are inexorably followed by changes in dietary patterns, including higher consumption of sugars, refined grains, animal fats, processed food, and a low supply of vegetables [14, 15]. In addition to dietary changes, overweight and obesity have been associated with an increased risk for CRC [16, 17]. Typical changes progressively seen in modern societies have also been associated with an increase in CRC, including type 2 diabetes [18], sedentarism [19], smoking [20], and alcohol consumption [21].
Regarding mortality, there has been a reduction in cancer-related deaths in Western Europe and North America during the last decade [22]. In particular, death rates from CRC have declined progressively since the mid-1980s in the USA, Australia, and the UK [23]. Screening strategies can definitively have collaborated to improve such favorable outcomes by detecting and removing colonic polyps as well as allowing the detection of CRC in early stages [24].
CRC occurs predominantly in a sporadic fashion, with an overall less than ten percent of cases being attributed to well-established cancer-related genes [25]. Hence, further investigation on pathogenic mechanisms including the epigenetic changes [26] and genomic instability [27], and a better understanding of the epidemiology of CRC might help in the elucidation of potential causes and risk factors and may become the foundation for novel preventive policies. Therefore, the aim of this study was to analyze the geographic distribution and time trends of CRC incidence and lethality in Brazil, hopefully providing clues to the identification of areas with differential risks and outcomes of CRC.
Methods
Data Source
Data were retrospectively retrieved from the Health Informatics Department of the Brazilian Ministry of Health (DATASUS) (http://www2.datasus.gov.br/DATASUS) with regard to hospital registries of patients whose diagnoses were included using the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision code of CRC (ICD 10 cod: C18; C18.0 to C18.9; C19; and C20), from January 2005 to December 2018. The C18.1 code was excluded because it is not representative of adenocarcinoma of the colon. DATASUS is a population-based health and disease registry that includes hospitalization information (admission and discharge data, medical procedures and in-hospital mortality). As DATASUS covers approximately the entire population, we assumed that hospital-based procedures for either CRC diagnosis or treatment would reflect the actual disease numbers in the country. Accordingly, CRC incidence and lethality rates were estimated from hospital discharge records. Information on colonoscopies from both outpatients and hospital procedures was also obtained from DATASUS registries.
Complementary data were obtained from VIGITEL (National System of Surveillance of Chronic Diseases) to access information on general health conditions of the population, such as overweight, obesity, diabetes, and smoking [28, 29]. All data are anonymously archived; hence, ethical approval was not required.
Study Design, Populations, and Variables
Similar to previous studies from our group [30, 31], we performed an ecological study based on DATASUS CRC registries in Brazil from January 2005 to December 2018. Ecological studies allow temporal and geographic analyses of risk factors, health status, and development of diseases in a given population. The period of the study refers to the most recent and consistent data available.
Data included age- and sex-standardized rates of admissions and lethality, as well as the municipality (town) of residence at the time of hospital admission. Incidence (rate of new hospital admissions for CRC) and lethality (intrahospital deaths caused by CRC) were estimated from hospitalization records. Age groups were stratified as 20 to 49 years, 50 to 69 years, and 70 years or older.
Geographic distribution resulted from the analysis of CRC hospitalization rates per 100,000 inhabitants in each 5568 Brazilian municipalities, gathered in 5 macroregions (North, Northeast, Central West, Southeast, and South). The results of this exploratory data analysis were included in a platform to plot maps depicting the estimates and distribution of CRC in the country.
Statistical Analyses
CRC hospitalization rates were adjusted to the totality of available hospital beds in Brazil during the study period. Estimates of the resident population were obtained from the Brazilian Institute of Geography and Statistics (IBGE; Instituto Brasileiro de Geografia e Estatística) [32]. The IBGE is the official governmental agency responsible for the collection of statistical, geographic, and environmental information.
Exploratory procedures with a quantitative approach were applied to the data using IBM SPSS software for Windows (version 20; SPSS Inc., Chicago, IL, USA) for the statistical and temporal trends analysis.
Descriptive summary statistics and graphical displays were generated by Tabwin3.2 (Tab for Windows 3.2, free software), which allowed organization of multiple applications into grouped tabs available at http://www2.datasus.gov.br/DATASUS. Linear regression was applied to evaluate temporal trends in CRC incidence and lethality by sex and age range using Excel software (Microsoft Excel for Mac 2011, version 14.4.9, 2010; Microsoft Corp, Redmond, Wash).
Results
Hospitalizations for Colorectal Cancer
The incidence of CRC in Brazil (estimated from hospitalizations and adjusted to available hospital beds) more than tripled (+ 352%), from 14.6 per 100,000 inhabitants in 2005 to 51.4 per 100,000 inhabitants in 2018. There were 20,389 CRC hospitalizations recorded in DATASUS registries in 2005 and 74,013 in 2018. The CRC-adjusted incidence increased from 14.4 per 100,000 inhabitants in 2005 to 53.1 per 100,000 inhabitants in 2018 in males and from 14.9 in 2005 to 49.6 in 2018 in females. Incidence rates by sex were similar over the 14-year period. The male/female incidence ratios were 0.96 in 2005 and 1.07 in 2018, which represented increases in incidence of 368.7% in males and 332.8% in females, respectively (Fig. 1A).
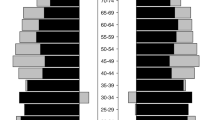
Steady increases in the estimated incidence of CRC were observed for all age ranges analyzed. During the study period, the rates of hospitalizations were lower among people aged 20 to 49 years (7.8 and 8.9 per 100,000 inhabitants for males and females in 2005, respectively), intermediate for those aged 50–69 years (52.2 and 46.7 per 100,000 inhabitants for males and females in 2005, respectively), and much higher for those 70 years or older (101.7 and 84 per 100,000 inhabitants for males and females in 2005). The rates of hospitalizations in 2018 were higher than those in 2005 in all age ranges: 19.5 for males and 22.2 for females aged 20 to 49 years; 167.7 for males and 139.6 for females aged 50–69 years; and 277.2 for males and 184.6 for females aged 70 years or over (Fig. 2). In particular, people aged 50–69 years showed the greatest difference between 2005 and 2018 (+ 266%) (Table 1).
Lethality Rates from Colorectal Cancer
CRC lethality estimated from in-hospital deaths decreased similarly in both sexes, from 12% in 2005 to 8% for males and females in 2018 (Fig. 1B). According to age, we observed a decline in lethality in all age ranges, mainly in people aged 50 to 69 years (-38%) (Fig. 3).
Geographic Distribution of Colorectal Cancer
Brazil, a continental country, shows relevant geographic, economic, and social disparities. Taking this into account, CRC rates were analyzed in the 5 Brazilian macroregions (North, Northeast, Central-west, Southeast, and South). Rates were also reviewed on the basis of demographic and commuting patterns of municipalities. A model that classifies municipalities considering the population, demographic density, and relation to metropolitan regions was used in this study, similar to other previous ecological studies by our group. 24,25,26 Although the rise occurred in all 5 macroregions, the CRC distribution was clearly different in each region, and the estimated incidence uncovered a remarkable South to North gradient. The South and Southeast, the most industrialized and economically developed regions, displayed the highest CRC incidence rates. The lowest rates were registered in the North region. Changes in estimated incidence rates were much higher in the South (+ 397%) and Northeast (+ 318%). In contrast to incidence, nationwide lethality decreased from 11.7% (in 2005) to 8% (in 2018). The greatest decrease in lethality was observed in the North (-79%) and the South (-55%) (Table 2).
Considering urban and rural demographic data, the greatest changes in incidence and lethality rates were registered in small-sized municipalities. In small-sized municipalities integrated into metropolitan regions (MRs), the CRC incidence rate increased 490%, and in municipalities not integrated into MRs, the CRC incidence rate increased 407% between 2005 and 2018. The greatest decline in lethality rates was observed in small-sized municipalities. However, the declines in lethality observed in small-sized municipalities were quite similar whether integrated (-46%) or not (-44%) to MR (Table 3).
Standardization defined 3 ranges for hospitalization rates (< 5/100.000, 5–15/100.000 and > 15/100.000 inhabitants). We considered 4 ranges for lethality rates: < 25%, 25–49%, 50–75%, and > 75%. Hospitalization (Fig. 4A) and lethality rates (Fig. 4B) of all municipalities in 2005 and 2018 were plotted in maps.
Associations of Colorectal Cancer with Other Health Disorders and Colonoscopy Availability
The analysis of data originating from the DATASUS and VIGITEL databases allowed the identification of changes in colonoscopy availability offered by the health system and of the prevalence of other potentially relevant health conditions of the population evolving in parallel with CRC during the study period.
According to DATASUS-based outpatients and hospital procedures, the rise in CRC estimated incidence was accompanied by a consistent rise in the availability of colonoscopies. A clear South to North gradient was also detected in relation to the number of colonoscopies offered for the population (Supplementary Fig. 2).
In parallel with the analysis from the DATASUS-derived data, in approximately the same period of time, we analyzed data obtained from the VIGITEL system and noted increases in the rates of overweight and obesity (as defined by the World Health Organization (https://www.who.int) and diabetes in all regions of the country (Supplementary Fig. 3A, B, C). However, a decrease in smoking rates was noted in all macroregions, with the lowest decrease in the South (-34%) and the highest in the North (-51%) (Supplementary Fig. 3D).
Discussion
The results of the present study indicate that the estimated incidence of CRC has increased, while the lethality rate has decreased from 2005 to 2018 in Brazil. No clear sex propensity was observed in this study, but as in other countries, the frequency of CRC in our study was higher in older people. Socioeconomic status may play a role in this finding since differences in life expectancy can be associated with more years of exposure to risk factors for CRC. Our age-stratified analysis showed that the CRC estimated incidence rates were higher for those aged seventy and above, intermediate for people from 50 to 69, and lower for those under 49 years old. Older people are more likely to be exposed to and accumulate environmental and lifestyle risk factors. Moreover, developing countries are dealing with a rapidly growing aging population. Brazil has the sixth largest population of elderly people in the world, with an estimate of more than 60 million seniors by 2050 [33]. Nevertheless, the greatest percentage difference in estimated incidence from 2005 to 2018 was observed in the age range from 50 to 69 years. Although screening can detect and remove precursor lesions of CRC, the implementation of screening programs needs considerable resources and the coordination of public policies. High-income nations have published society guidelines that recommend anticipation of CRC screening, as CRC rates have steadily increased in people younger than 50 years [34, 35]. In particular, the increase in CRC rates among people under 50 years of age in Brazil was higher than that among people 70 years or older. This may not only result from health policies but also reflect changes in lifestyle and dietary habits.
Although the distribution of CRC varies largely across world regions, incidence rates up to threefold higher have been reported in high and very high Human Development Index (HDI) settings [36]. The increase in CRC incidence rates observed in this study is in accordance with international data showing different gradients of CRC across distinct HDIs, as well as in countries in transition, displaying an upward trend in CRC incidence [37]. In agreement with other previous studies of gastrointestinal cancer in Brazil [30, 31], the highest rates of CRC were also observed in the South and Southeast, the more developed regions, concentrating more than 60% of the Brazilian gross domestic product (GDP) [38].
Studies suggesting the association between the HDI and CRC incidence and lethality rates also indicate a relationship with access to health services favoring early diagnosis [4, 37]. The wide diversity in economic and social support can significantly affect access to health services and, as a consequence, early detection and the resection of CRC premalignant conditions, such as colorectal polyps [39, 40]. This information is also probably related to the progressive availability of colonoscopies all over the country, which is proportionally greater in the Southeast and South regions. Although qualified health services tend to increase more rapidly in the more developed areas maintaining regional inequality, this study showed that the increase in CRC in the Northeast region, in which the number of colonoscopies and the HDI are lower than in the South, Southeast, and Central-west, ranked second in the country. Despite all the socioeconomic disparities within the country, the Northeast GDP increased 3% in recent years, more than triple of the average of the country [38, 41]. In addition, from 2010 to 2017, improvements in the HDI were recorded in 6 of the 9 northeastern federal units, currently classified as highly developed states [41, 42]. Moreover, the Northeast registered the same rate of decrease in CRC lethality as the Brazilian average in the period (-32%), reinforcing the idea of improvements in quality and access to health services.
Modifiable factors usually related to socioeconomic disparities, including physical inactivity, a high-fat diet, smoking, and obesity, may increase the risk of developing CRC. For example, overweight and obesity have been consistently associated with an increased risk for CRC [16, 17]. Type 2 diabetes is also regarded as an independent risk factor for CRC [18, 43]. The results of this study showing a temporal association of the rise of CRC in parallel with overweight, obesity, and diabetes in the Brazilian population appear to corroborate previous epidemiological associations elsewhere and to characterize the progressive “westernization” of the country. In fact, ongoing changes in lifestyle and dietary habits with a shift from a fiber-rich diet based on grains and vegetables to a high-calorie diet [44] may underlie the notable recent increases in overweight, obesity, and diabetes and probably also of CRC in Brazil. Both the general trend of CRC increase and the regional differences observed appear to be in agreement with the dietary changes within the country. Nevertheless, as the development of CRC is usually positively associated with the regular consumption of red and processed meat [45] and counterbalanced by fiber ingestion [46], this may again corroborate the South to North gradient, as red meat and derivatives are traditionally more commonly consumed in the South, while vegetables and natural products still predominate in the North.
Regarding smoking, another well-recognized risk factor for CRC [20], although this study showed marked reductions in all 5 macroregions, it appears that the decrease is less pronounced in the South, similar to previous studies [47]. Such a difference could explain, at least in part, the higher rates of CRC in the South, even when compared to the Southeast, uncovering particular regional characteristics of both metropolitan and rural southern areas. In fact, the South has 98% of the country’s tobacco [48], and some of the largest metropolises with the highest smoking frequencies [47]. Although smoking in Brazil has dropped steadily in the last 20 years, an urban–rural gradient in tobacco consumption is still present in the country [49].
The reduction in the lethality rate due to CRC observed in all macroregions and in both sexes shown in this study is in contrast to previous data supporting unfavorable trends for the near future [50]. Our results appear to indicate that despite great inequalities and varying medical resources, Brazil has shown improvements in some areas of health care, achieving numbers comparable to reports from more developed European countries [51]. As the prognosis and lethality of CRC are directly influenced by early detection, advanced surgical techniques, and adjuvant therapies, access to proper health care is of paramount importance for the outcome of CRC management [4, 6]. This may also help to explain the regional differences and dynamic changes detected in this study. Although a clear South to North gradient reflects the predominant CRC distribution in the country, socioeconomic improvements may have been particularly relevant in the North and Northeast regions, where lethality rates decreased proportionally more than in the Central-west and Southeast regions. However, socioeconomic improvements cannot explain the greater rise in CRC incidence in the Northeast than in the North. In fact, the continental dimension and heterogeneity of the country, with its marked geographic regions and variably distributed population and socioeconomic developmental levels, create a dynamic and complex scenario, which renders data difficult to interpret accurately in a single study.
Interestingly, the CRC incidence and lethality rates in light of geographic distribution considering municipalities’ characteristics showed different trends compared to other gastrointestinal cancers, reported in similar ecological studies performed by our group [30] [31]. In the present study, the greatest changes in admission rates for CRC occurred in small-sized municipalities associated or not with metropolitan regions. Regarding lethality, small-sized municipalities also ranked first in reduction rates throughout the period. Several factors should be analyzed in an attempt to explain such differences. Improvements in socioeconomic indicators [52, 53] and a growing urbanization process [54] observed all over the course might have positively affected the health system in general, including in municipalities not integrated into MRs. This would probably include better access to health services and the availability of medical diagnostic and treatment units, allowing an earlier diagnosis and proper CRC treatment.
The Brazilian public healthcare system covers roughly more than three-fourths of the population, who rely exclusively on the SUS for health services, distributed throughout the country offering medical consultation and complementary diagnostic methods [55]. This could explain the lower lethality rates and the higher incidence of CRC, probably related to improvements in the diagnostic capacity, in small-sized municipalities even when not associated with metropolitan regions. The greater proportional increase in CRC incidence observed in small-sized municipalities also suggests that societal changes and other important environmental risk factors might have been disseminated in the whole country before this study period.
Although the findings of this study provide new insights into CRC geographic distribution and time trends in Brazil, several limitations need to be addressed. First, despite the large amount of data covering the entire country, the database does not contain information on disease staging, comorbidities or therapy. Moreover, the analysis based on hospitalization records does not consider outpatients who had not been submitted to medical procedures or hospital admissions. It is also important to call attention to differences in the availability and quality of health care in less developed regions of the country, which may result in potential discrepancies in the available data. Another potentially controversial issue refers to the concept of municipality. In fact, in addition to geographic heterogeneities, Brazilian cities present substantial dissimilarities concerning population densities, but would be regarded as municipalities of the same level in the database. However, the limitations and the possibility of an ecological fallacy [56] have been greatly attenuated in this study due to the clarity and straightforwardness of the data entered in a single electronic database. Most importantly, the use of municipalities might compensate for potential underreporting or imperfection of the registry, since the system contains official data enclosing the entire country in its minimal administrative units.
In conclusion, similar to other countries, the incidence of CRC is rising in Brazil, particularly in the population above fifty years of age. Higher rates in the South and Southeast regions may reflect the better quality of diagnosis but also the presence of major environmental factors attributable to a progressively more “westernized” lifestyle. Moreover, geographic shifts in the incidence from the South toward the Northeast and from urbanized to rural areas appear to support the notion of ongoing dynamic changes within the socioeconomic environment, including in less developed regions. Decreasing lethality rates in the context of a consistent rise in the estimated incidence of CRC suggest a successful decentralization process and improvements in the quality of public health services during the study period. These observations may also suggest better access to health care beyond the limits of the great Brazilian metropolises related to the current urban phenomenon that affects contemporary cities, such as the increased availability of transportation systems providing mobility for people to travel to central towns to access their services, including healthcare units. Understanding the current patterns of CRC and its evolution in Brazil is critical for the implementation of more efficient health policies to direct future actions for both prevention and care.
Data availability
The datasets analyzed during the current study are available in the Health Informatics Department of the Brazilian Ministry of Health (DATASUS) repository (www.datasus.gov.br/DATASUS). DATASUS registries include hospital admission and discharge information, medical procedures and mortality, reference tables, and demographic data (municipality, age, sex) collected by the Instituto Brasileiro de Geografia e Estatística (IBGE—Brazilian Institute of Geography and Statistics).
Abbreviations
- CRC:
-
Colorectal cancer
- MR:
-
Metropolitan region
- HDI:
-
Human development index
References
Arnold M, Sierra MS, Laversanne M et al. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–691.
Fitzmaurice C, Allen C, Barber RM et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 2017;3:524–48.
Sung H, Ferlay J, Siegel RL et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249.
Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the human development index (2008–2030): a population-based study. Lancet Oncol. 2012;13:790–801.
Ferrari F, Reis MA. Study of risk factors for gastric cancer by populational databases analysis. World J Gastroenterol. 2013;19:9383–9391.
Rafiemanesh H, Mohammadian-Hafshejani A, Ghoncheh M et al. Incidence and mortality of colorectal cancer and relationships with the human development index across the world. Asian Pac J Cancer Prev. 2016;17:2465–2473.
Edwards BK, Ward E, Kohler BA et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544–573.
Brenner DR, Heer E, Sutherland RL et al. National trends in colorectal cancer incidence among older and younger adults in Canada. JAMA Netw Open. 2019;2:e198090.
Abualkhair WH, Zhou M, Ahnen D et al. Trends in incidence of early-onset colorectal cancer in the United States among those approaching screening age. JAMA Netw Open. 2020;3:e1920407.
Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev. 2010;19:1893–1907.
Jemal A, Bray F, Center MM et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Baxter NN, Warren JL, Barrett MJ, Stukel TA, Doria-Rose VP. Association between colonoscopy and colorectal cancer mortality in a US cohort according to site of cancer and colonoscopist specialty. J Clin Oncol. 2012;30:2664–2669.
Zauber AG, Winawer SJ, O’Brien MJ et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687–696.
Keum N, Giovannucci E. Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 2019;16:713–732.
Murphy N, Moreno V, Hughes DJ et al. Lifestyle and dietary environmental factors in colorectal cancer susceptibility. Mol Aspects Med. 2019;69:2–9.
Karahalios A, English DR, Simpson JA. Weight change and risk of colorectal cancer: a systematic review and meta-analysis. Am J Epidemiol. 2015;181:832–845.
Silva A, Faria G, Araujo A, Monteiro MP. Impact of adiposity on staging and prognosis of colorectal cancer. Crit Rev Oncol Hematol. 2020;145:102857.
He J, Stram DO, Kolonel LN et al. The association of diabetes with colorectal cancer risk: the Multiethnic Cohort. Br J Cancer. 2010;103:120–126.
Doubeni CA, Major JM, Laiyemo AO et al. Contribution of behavioral risk factors and obesity to socioeconomic differences in colorectal cancer incidence. J Natl Cancer Inst. 2012;104:1353–1362.
Botteri E, Iodice S, Bagnardi V et al. Smoking and colorectal cancer: a meta-analysis. JAMA. 2008;300:2765–2778.
Fedirko V, Tramacere I, Bagnardi V et al. Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Annals of oncol : Off J Eur Soc Med Oncol. 2011;22:1958–1972.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg. 2009;22:191–197.
Knudsen AB, Zauber AG, Rutter CM et al. Estimation of benefits, burden, and harms of colorectal cancer screening strategies: modeling study for the us preventive services task force. JAMA. 2016;315:2595–2609.
Rustgi AK. The genetics of hereditary colon cancer. Genes Dev. 2007;21:2525–2538.
Bonasio R, Tu S, Reinberg D. Molecular signals of epigenetic states. Science. 2010;330:612–616.
Pino MS, Chung DC. The chromosomal instability pathway in colon cancer. Gastroenterology. 2010;138:2059–2072.
Bernal RTI, Iser BPM, Malta DC, Claro RM. Surveillance System for Risk and Protective Factors for Chronic Diseases by Telephone Survey (Vigitel): changes in weighting methodology. Epidemiol e Serv de Saude : Rev do Sist Unico de Saude do Brasil. 2017;26:701–12.
Enes CC, Nucci LB. A telephone surveillance system for noncommunicable diseases in Brazil. Public Health Rep. 2019;134:324–27.
Perrotta de Souza LM, Moreira JPL, Fogaca HS, Luiz RR, de Souza HS. Pancreatic cancer incidence and lethality rates in Brazil: an ecological study. Pancreas. 2017;46:699–706.
Amorim CA, De Souza LP, Moreira JP et al. Geographic distribution and time trends of esophageal cancer in Brazil from 2005 to 2015. Mol Clin Oncol. 2019;10:631–638.
IBGE. Population Estimates. Instituto Brasileiro de Geografia e Estatistica (IBGE). 2018.
Tramujas Vasconcellos Neumann L, Albert SM. Aging in Brazil. Gerontologist. 2018;58:611–17.
Wolf AMD, Fontham ETH, Church TR et al. Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin. 2018;68:250–281.
Naumann DN, Kavanagh C, Hipkiss G et al. Impact of cumulative experience on the quality of screening colonoscopy: a 13-year observational study. J Med Screen. 2021;17:9691413211009562.
Blair A, Datta GD. Associations between area-level deprivation, rural residence, physician density, screening policy and late-stage colorectal cancer in Canada. Cancer Epidemiol. 2020;64:101654.
Xi Y, Xu P. Global colorectal cancer burden in 2020 and projections to 2040. Transl Oncol. 2021;14:101174.
IBGE. Health Statistics: Survey of Medical-Sanitary Assistance 2009. Instituto Brasileiro de Geografia e Estatistica (IBGE). 2009.
Gupta S, Lieberman D, Anderson JC et al. Recommendations for follow-up after colonoscopy and polypectomy: a consensus update by the us multi-society task force on colorectal cancer. Gastroenterology. 2020;158:1131–53 e5.
Rutter MD, East J, Rees CJ et al. British society of gastroenterology/association of coloproctology of great britain and ireland/public health England post-polypectomy and post-colorectal cancer resection surveillance guidelines. Gut. 2020;69:201–223.
IBGE. Annual Survey of Services. Instituto Brasileiro de Geografia e Estatistica (IBGE). 2018.
de Castro CP, Dos Santos GF, de Freitas AD et al. Socio-economic urban scaling properties: influence of regional geographic heterogeneities in Brazil. PloS one. 2020;15:e0242778.
Yang YX, Hennessy S, Lewis JD. Type 2 diabetes mellitus and the risk of colorectal cancer. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2005;3:587–594.
Granado FS, Maia EG, Mendes LL, Claro RM. Reduction of traditional food consumption in Brazilian diet: trends and forecasting of bean consumption (2007–2030). Public Health Nutr. 2021;24:1185–1192.
Bouvard V, Loomis D, Guyton KZ et al. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16:1599–1600.
Tabung FK, Liu L, Wang W et al. Association of dietary inflammatory potential with colorectal cancer risk in men and women. JAMA Oncol. 2018;4:366–373.
Malta DC, Stopa SR, Santos MAS et al. Evolution of tobacco use indicators according to telephone surveys, 2006–2014. Cadernos de saude publica. 2017;33Suppl 3:e00134915.
Bartholomay P, Iser BP, de Oliveira PP et al. Epidemiologic investigation of an occupational illness of tobacco harvesters in southern Brazil, a worldwide leader in tobacco production. Occup Environ Med. 2012;69:514–518.
Opaleye ES, Sanchez ZM, Moura YG et al. The Brazilian smoker: a survey in the largest cities of Brazil. Revista brasileira de psiquiatria. 2012;34:43–51.
Martin FL, Morais CLM, Sakita JY, Uyemura SA, Kannen V. Age-related and gender-related increases in colorectal cancer mortality rates in Brazil between 1979 and 2015: projections for continuing rises in disease. J Gastrointest Cancer. 2021;52:280–288.
Macinko J, Lima-Costa MF. Horizontal equity in health care utilization in Brazil, 1998–2008. Int J Equity Health. 2012;21:33.
Victora CG, Barreto ML, de Carmo Leal M et al. Health conditions and health-policy innovations in Brazil: the way forward. Lancet. 2011;377:2042–53.
UNESCO (United Nations Educational SaCO. Institute for Statistics. 2018. Data Centre. 2018.
Szwarcwald CL, Bastos FI, Barcellos C, Pina MF, Esteves MA. Health conditions and residential concentration of poverty: a study in Rio de Janeiro, Brazil. Journal of epidemiology and community health. 2000;54:530–536.
Castro MC, Massuda A, Almeida G et al. Brazil’s unified health system: the first 30 years and prospects for the future. Lancet. 2019;394:345–356.
Salkeld DJ, Antolin MF. Ecological fallacy and aggregated data: a case study of fried chicken restaurants. Obesity and Lyme Disease. Ecohealth. 2020;17:4–12.
Acknowledgment
The authors would like to thank the Brazilian Research Foundations CAPES, CNPq, and FAPERJ for their financial support.
Funding
This work was supported by grants from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brazil (CAPES)—Finance Code 001; the Brazilian Research Council (CNPq) (306634/2019–8) and the FAPERJ (Fundação Carlos Chagas Filho de Amparo a Pesquisa do Estado do Rio de Janeiro) (E26/202.781/2017 and E26/210.886/2014).
Author information
Authors and Affiliations
Contributions
APNS and LMPdS participated in the conception and design of the study, the acquisition, analysis, and interpretation of the data, and the drafting of the manuscript. JPM and RRL participated in the acquisition, analysis and interpretation of the data, and the drafting of parts of the manuscript. HSF and HSPdS participated in the conception and design of the study, obtained funding, analyzed and interpreted the data, and critically revised the manuscript for important intellectual content. All authors gave final approval of the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Ethical approval was waived by the local Ethics Committee of the University Hospital Clementino Fraga Filho, of the Federal University of Rio de Janeiro, in view of the retrospective nature of the study investigating a population-based health and disease registry, anonymously archived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sampaio, A.P.N., de Souza, L.P., de Lima Moreira, J.P. et al. Geographic Distribution and Time Trends of Colorectal Cancer in Brazil from 2005 to 2018. Dig Dis Sci 67, 4708–4718 (2022). https://doi.org/10.1007/s10620-021-07357-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07357-9