Abstract
Background
Cirrhosis is associated with poor health-related quality of life (HRQOL), cognitive dysfunction (CD), and lack of coordination leading to falls. Tandem gait (TG; heel-toe) can be used to assess coordination. The impact and relationship between CD, TG and falls pre-/post-liver transplant (LT) is unclear. We aimed to determine the impact of LT on CD, abnormal TG, and HRQOL in cirrhosis.
Methods
We analyzed patients who underwent complete neurological examination, cognitive testing by psychometric hepatic encephalopathy score (PHES), and HRQOL assessment using sickness impact profile (SIP). All patients were followed for 1 post-LT visit at 6 or 12 months post-LT for clinical course and falls. Change in CD, TD, and falls pre-/post-LT were compared.
Results
Off 131 recruited, 61 patients completed all visits. Majority were men (84%), with HCV etiology (34%). Pre-LT: Abnormal TG trended towards increased falls (OR 3.3, P = 0.08). Forty-nine % had abnormal TG, 61% had CD, 32.7% had CD + abnormal TG, 62% had prior OHE, and 14.7% had falls. Abnormal and normal TG patients had similar ages, BMI, sex, education level, and MELD scores. Abnormal TG group had higher prior overt HE (P = 0.03) and worse physical SIP score (P = 0.008). Post-LT: There was sustained improvement in CD, HRQOL, falls, and TG post-LT more at 12 than 6 months in all patients. Patients who had abnormal TG pre-LT continued to have a worse PHES (P = 0.0064) and physical SIP score (P = 0.008) compared to normal pre-LT TG patients.
Conclusion
After LT, there is a sustained improvement in coordination measured via tandem gait, accompanied by a lower rate of falls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with cirrhosis often have coexistent cognitive and physical impediments. Covert hepatic encephalopathy (CHE) manifesting as an anamnestic cognitive dysfunction (CD) can occur early on in cirrhosis, while frailty occurs in decompensated cirrhosis. Importantly impairment in HRQOL from CD and frailty ultimately can impair daily function [1] and result in falls that can impact morbidity and mortality [2, 3]. Patients on the liver transplant (LT) list have been examined for frailty with objective and subjective instruments such as the short physical performance battery (SPPB) [4], Fried frailty index [5], clinical frailty scale [6], and the novel liver frailty index (LFI) [7]. These batteries include measures such as gender-adjusted grip strength, number of chair stands per second, tandem standing, balance time, and gait speed, which have been studied in cirrhotic and non-cirrhotic patients. Another interesting tool that has not been used in this context, but has been validated in the non-cirrhotic population is the tandem walk (heel-toe) gait [8]. The tandem-gait (TG) test assesses locomotion, dynamic balance, and lower limb coordination all of which influence gait and falls.
Covert hepatic encephalopathy is usually diagnosed using the psychometric hepatic encephalopathy score (PHES) [9]. Cognitive dysfunction (measured as CHE) and frailty have been independently and jointly associated with readmission and poor outcomes on the LT waiting list [5, 10, 11]. Their concomitant post-LT course is unclear, but studies have shown a worsening frailty in the immediate post-LT period with improvement over 1 year [12].
Given the potential interaction of CD and physical incoordination [13], we hypothesized the following. (1) LT improves abnormal TG, a measure of coordination and associated falls and (2) Post-LT improvement of CD is associated with improvement of abnormal TG.
Methods
We performed an analysis of prospectively collected data of patients with cirrhosis listed for deceased solitary LT at the Virginia Commonwealth University (VCU) Medical Center from June 2011 to June 2015. Adults between 21 and 65 years of age who gave informed consent were followed up over 1-year post-LT. We excluded those with moderate depression (Beck Depression Inventory > 20), who were not able to give informed consent, previous transplant, human immunodeficiency virus infection, and those who are listed under priority 1 status. Demographic data, etiology for LT, pre- and post-LT falls/course, medications pre- and post-LT were documented. All patients underwent a complete neurological examination by an MD provider at all visits.
Psychometric and HRQOL Testing
At the pre-LT visit, the subjects were given the mini mental status examination and were only allowed to proceed if they scored ≥ 25. Patients were subjected to PHES testing [consisting of the number connection tests A and B (NCT-A, NCT-B), digit symbol test, serial dotting test, and line drawing test]. Tests were administered by two trained providers. CHE was diagnosed on PHES for a score ≤ − 4 based on our norms [9]. We evaluated individual test performances and considered impaired performance on PHES as diagnostic of CHE. Patients who tested positive were diagnosed to have CHE; this was irrespective of a history of OHE.
For HRQOL assessment, we utilized the sickness impact profile (SIP) test. The SIP is a validated HRQOL questionnaire with 136 items grouped into 12 scales: sleep and rest, eating, work, home management, recreation and pastimes, ambulation, mobility, body care and movement, social interaction, alertness, emotional behavior, and communication. Subjects are asked to mark only those questions which are pertinent to their health over the past 24 h. This questionnaire requires minimal explanation without physician involvement and can usually be completed within 5–20 min. The number of questions are weighted and divided from a total number to achieve a percentage which translates into the traditional HRQOL measure. A higher score indicates poor HRQOL.
Tandem Gait (Heel-Toe) Assessment
Participants were instructed to remove their shoes and stand with their feet together behind a starting line. When ready, participants walked forward using an alternating-foot heel-to-toe gait along a line 38 mm wide and 3 m long, ensuring that their heel and toe touched on each step. Once the participant crossed the end of the 3-m line, they turned 180° and returned to the starting position using the same gait. Participants were encouraged to complete the task as quickly as possible and free of error. Participants failed the trial if they stepped off the line, had a separation between their heel and toe at any time, or touched or grabbed the examiner or an object. Patients were monitored for form, i.e., swaying and to document completion of the walk without breaking stride. Successful completion was documented if the patients performed the task as described without any stoppage and line breaking. Abnormal TG was considered as a surrogate marker for physical frailty and coordination.
Statistical Analysis
Statistical analysis was done on JMP and SPSS (version 25). Appropriate t tests, Wilcoxon signed rank and rank sum tests, Chi square/fisher exact tests were performed. For the longitudinal analysis, linear mixed modeling (LMM) was done (continuous variables) along with generalized linear mixed modeling (categorical variables). For the continuous data, we used the log function to normalize the data to run the LMM. For the univariate analysis, age, sex, education, MELD score, history of prior OHE, ascites, variceal bleeding, PHES score, physical SIP score, serum sodium level were incorporated. Only significant variables (P < 0.05) were incorporated into multivariable linear regression models where applicable. Dependent variables were abnormal TG pre-LT, improvement in TG post-LT, and pre-LT CHE + abnormal TG.
Results
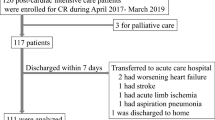
We enrolled a total of 131 patients with cirrhosis pre-LT of which 64 were alive and followed up in the post-LT period. The remaining patients either died while on the waitlist from complication related to cirrhosis (n = 15), improved spontaneously (n = 18), got transplanted at another center (n = 2), withdrew from the study for personal reasons (n = 15), did not show up for the follow-up and were automatically removed from the study (n = 12), or died in the post-LT period (n = 10).
Of the original 131, 97 had completed pre-LT data available. Out of the 64, 61 had complete documentation of one neurological examination pre- and post-LT and were included in the study. Forty-nine patients were seen 6 months post-LT, and 37 patients were seen at 12 months post-LT for their second post-LT follow-up visits.
Analysis of the excluded patients showed that of the 15 who died on the waitlist, 14 had neurological exams available and 8 of the 14, i.e., 57% had abnormal TG. Of the 10 that died post-LT, four did not have completed neurological exams but six of the nine, i.e., 66.6% had abnormal TG prior to LT.
Pre-LT clinical variables and peri-/post-LT clinical course: Of the 61 patients, 38 (62.2%) had a history of OHE, 39 (63.9%) had a history of ascites, and 5 (8%) had prior variceal bleeding. Of the 61 patients, 17 patients had hepatocellular carcinoma and were listed with MELD exception points. The median age and education of all eligible patients was 58 (52, 61) and 13 (12, 14) years, respectively. Median MELD score of all patients was 22 (16.5, 24). Males were predominant at 51 (83.6%). Caucasian race predominated at 49 (80.3%). The most common etiology for cirrhosis was HCV-21 (34.4%), followed by other etiologies 13 (21.3%), Alcohol + HCV-11 (18%), alcoholic liver disease—8 (13.1%) and NASH-8 (13%). The mean BMI was 30.5 ± 5.5.
The median time to LT was 54 (95% CI 16, 112.5) days after enrollment. After LT, all patients remained on stable immunosuppressive therapy apart from five patients who had changes to the combination prior to the first follow-up visit (all within a 6-month period post-LT). one patient had primary graft non-function with re-transplant, five had acute cellular rejection prior to first follow-up appointment. A total of six patients developed acute kidney injury in the peri-LT period and were started on hemodialysis post-LT.
Cognitive dysfunction was found in 61% of patients pre-LT, which reduced significantly 31% post-LT (P < 0.0019).
Pre-LT Impact of Abnormal TG
Of the 97 patients, 52 (53.6%) had abnormal TG. Total of 13 had falls. All 13 who had falls had abnormal TG. On univariate analysis with falls being the dependent variable and independent variables being abnormal TG, MHE, OHE, ascites, and MELD scores, only abnormal TG showed a trend towards significance (OR 3.3 (0.8–12.9), P = 0.08).
Tandem Gait Pre-LT
Pre-LT 30 of 61 patients had abnormal TG. Abnormal versus normal TG patients had similar age [58 (52, 62) vs 56 (52, 60) years, P = 0.3], male sex distribution (20 vs 17, P = 1), education level [12 (12, 14) vs 13 (12, 14) years, P = 0.4], MELD scores [19.5 (16, 25) vs 22 (18, 23), P = 0.5] and BMI [29.5 (27, 35) vs 30 (27, 3), P = 0.7]. Patients with abnormal TG had similar CD (20 vs 17, P = 0.3) but greater proportion with prior OHE (76% vs 48%, P = 0.03). Patients with abnormal TG had a worse physical component of the SIP score [24 (12.5, 39) vs 13.8 (3.2, 20.5), P = 0.008]. The psychosocial score [19.5 (5.7, 31.26) vs 14.6 (8.6, 31), P = 0.72] and total SIP score [27.5 (17.4, 37) vs 19.5 (21, 32), P = 0.13] were similar between patients with/without abnormal TD. On univariable analysis, prior OHE [OR 3.5 (1.16–10.5), P = 0.02], ascites [OR 3.08 (1.02–9.26), P = 0.04], and poor physical SIP score [OR 1.05 (1.03–1.09), P = 0.009] were significantly associated with abnormal TG. On multivariable analysis, only physical SIP score remained significantly associated with abnormal TG [OR 1.05 (1.006–1.09), P = 0.02].
Patients With Combined CD and Abnormal TG Pre-LT
As shown in Table 1, 20 of 61 patients showed abnormal TG and had CD. While age, education, cirrhosis etiology, cirrhosis severity, and BMI were similar, patients with abnormal TG and CD were more likely to be men with prior OHE who had a greater risk of falls compared to the others.
Change in TG Post-LT at 6 Months
Out of the 30 patients with abnormal TG pre-LT, 19 (63.3%) had improvement post-LT on the first scheduled follow-up visit. Details of demographics and other factors between the groups that improved or did not improve their TG are in Table 2. Both groups were similar in terms of age, pre-LT CD, and severity of liver disease. The only variable that was significantly different between groups was BMI which was higher in the group that did not improve TG.
Falls Pre- and Post-LT at 6 Months
Falls were higher in the pre-LT group compared to the post-LT group (9 (7.38%) vs 2 (3.2%) P = 0.02). The cause for all pre-LT falls was weakness, and falls were numerically higher in those with abnormal TG (n = 6). Of the two patients who fell post-LT, one was due to generalized weakness, while the other due to sepsis-induced hypotension.
Of the remaining 52 patients with no falls pre-LT, 24 had an abnormal TG. The group that fell pre-LT had a trend towards a greater proportion of abnormal TG (66.6% vs 46.7%, P = 0.3) compared to those who did not fall, although this was not statistically significant. Falls were higher in the pre-LT patients with CD (90% vs 55%), P = 0.02 compared to those without CD.
Changes Over 12 Months in Patients with 3 Visits
In the 37 patients who had complete cognitive, physical exams pre-LT, 6 and 12 months post-LT, there was a sustained improvement in CD and TG from 6 months through to 12 months. Importantly, the group with CD + abnormal TG also improved from 6 months to 12 months post-LT (Table 3). Patients with abnormal pre-LT TG had a worse PHES score at 6 months [− 4 (− 5, 0) vs − 0.5 (− 3, 1.25), P = 0.0064] with continued higher CD (48% vs 14%, P = 0.017). However, this improved at 12 months where these patients had statistically similar CD (11% vs 2%, P = 0.09) and PHES scores [− 1.5 (− 3.5,) vs 0 (− 2, 1), P = 0.16] compared to patients who had normal pre-LT TG. HRQOL in all aspects improved post-LT at 6 and 12 months compared to pre-LT values (Table 3).
Discussion
Most of the current evidence for the interrelation between CD and incoordination pre-LT have examined the 2 pre-LT, but their concurrent interaction post-LT is unclear. In this prospective cohort of LT patients, we found that abnormal TG is present in half of cirrhotic patients awaiting transplant, while CD with abnormal TG was present concurrently in up to a third of patients. Those that had falls pre-LT had abnormal TG. We also noted that patients with abnormal TG pre-LT had slower recovery from CD for up to 6 months post-LT compared to those with normal TG and that CD did not seem to associate with improvement in TG post-LT. Interestingly, just abnormal TG did not result in more falls pre-LT, CD showed a trend towards increased falls pre-LT, but CD with abnormal TG resulted in more falls pre-LT. Lastly CD, abnormal TG, falls, and HRQOL all improved post-LT.
Our study revealed that abnormal TG could predict falls in cirrhotic patients and was associated with a history of prior OHE and poor physical HRQOL (physical SIP score). Interestingly, pre-LT gait abnormalities were not associated with traditional markers of liver disease severity, such as the MELD score or with cognitive performance. Tandem gait abnormality and CD, therefore, do not appear to be redundant markers of brain function. For example, at the pre-LT and 12-month follow-up assessments, cognitive performance did not distinguish the TG groups. Tandem gait and the PHES evaluate different brain regions. PHES, our measure of CD, emphasizes psychomotor speed, response inhibition, and cognitive flexibility (i.e., frontal and parietal regions). In contrast, TG assesses the integrity of the vermis, or the vestibulo-cerebellar region, as well as white matter thalamic radiations, basal ganglia, and the corpus callosum. The relationship between TG abnormality and a prior history of OHE suggests that once a patient has suffered OHE, an enduring decline in brain reserve has taken place, i.e., a central rather than a peripheral etiology for the dynamic balance impairment seen in cirrhosis [3].
The mechanisms underlying postural control impairment in liver disease that contribute to falls are not well known and are multifactorial [13]. Urios et al. showed that cognitive impairment correlated with altered posture and stability in cirrhosis [14]. Felipo et al. demonstrated changes in cerebral blood flow, assessed by arterial spin labeling, with increase in the cerebellar vermis, and reduction in occipital regions in patients with encephalopathy [15]. Falls are unfortunately prevalent in the frail population, are independently associated with poor HRQOL, morbidity, and mortality [16], and hence, are an important clinical target. Cognitive dysfunction in cirrhotic patients is associated with a fall rate of up to 40% [2], and frailty is uniquely associated with a fall rate of up to 50% [12]. In our cohort, 90% with CD had falls as opposed to 55% with abnormal TG with a trend towards significance, which was worsened in those with CD with abnormal TD who had a significantly higher fall rate pre-LT. By examining CD and TG simultaneously in the present study, we were able to determine that both improved post-LT suggesting they may represent an overall marker of brain reserve.
Cognitive dysfunction associates with poor HRQOL and morbidity [17, 18]. We noted here that pre-LT CD is associated with a physical impairment of abnormal TG in decompensated cirrhosis and that those with abnormal TG pre-LT had a slower recovery in terms of CD post-LT. TG and CD were independently associated with outcome and may therefore represent the functional impact that liver disease has had on brain reserve. These data have practical clinical implication. For example, administering a 3-min dynamic balance test, such as the tandem walk, may inform the clinician regarding illness severity, likelihood for falls, and ultimately illness course following LT. The slower cognitive recovery in those with abnormal TG compared to those with normal TG despite having the same CD morbidity could possibly be because of the negative impact of CD on PF and of PF on CD [19, 20]. We also found that those with OHE had a higher abnormal TG which is not surprising and correlates with the PF findings as shown by Tapper et al. [21] and Lai et al.[22]. However, the finding of 32.7% with dual CHE and abnormal TG is surprisingly low here given that 49% had abnormal TG (Off whom 66.6% had CD and 76% had OHE) and 61% had CD overall. This discordance could potentially be because of the relatively small sample size.
The sustained improvement in CD and HRQOL follows prior studies, which we extend by noting improvement in TG and a lower rate of falls. The maximum improvement in CD and HRQOL was noted in the first 6 months post-LT with plateauing from 6 to 12 months. Surprisingly, those with abnormal TG pre-LT continued to have a persistent poor physical HRQOL at 12 months despite stable post-LT courses suggesting other physical impediments persisting apart from just the TG.
The use of the PHES as a marker of cognitive dysfunction is a strength in this study as is the study methodology and duration post-LT. Another limiting factor is our relatively small sample size and lack of formal sarcopenia and frailty testing.
We conclude that cognitive dysfunction is linked with impaired coordination manifested as abnormal tandem gait in decompensated cirrhosis. Abnormal tandem gait is a widely prevalent physical impairment in decompensated cirrhosis and could act as a potential marker of fall risk in this population and negatively influence cognitive recovery in the pre- and post-LT period. Lastly after LT, there is a sustained improvement in cognition, abnormal TG, and HRQOL for up to 12 months, which is accompanied by a lower rate of falls.
References
Bajaj JS. Minimal hepatic encephalopathy matters in daily life. World J Gastroenterol. 2008;14:3609–3615.
Roman E, Cordoba J, Torrens M, et al. Minimal hepatic encephalopathy is associated with falls. Am J Gastroenterol. 2011;106:476–482.
Soriano G, Roman E, Cordoba J, et al. Cognitive dysfunction in cirrhosis is associated with falls: a prospective study. Hepatology. 2012;55:1922–1930.
Lai JC, Dodge JL, Sen S, Covinsky K, Feng S. Functional decline in patients with cirrhosis awaiting liver transplantation: results from the functional assessment in liver transplantation (FrAILT) study. Hepatology. 2016;63:574–580.
Lai JC, Feng S, Terrault NA, Lizaola B, Hayssen H, Covinsky K. Frailty predicts waitlist mortality in liver transplant candidates. Am J Transplant. 2014;14:1870–1879.
Tandon P, Tangri N, Thomas L, et al. A rapid bedside screen to predict unplanned hospitalization and death in outpatients with cirrhosis: a prospective evaluation of the clinical frailty scale. Am J Gastroenterol. 2016;111:1759–1767.
Lai JC, Covinsky KE, Dodge JL, et al. Development of a novel frailty index to predict mortality in patients with end-stage liver disease. Hepatology. 2017;66:564–574.
Nemoto M, Yabushita N, Kim MJ, Matsuo T, Seino S, Tanaka K. Assessment of vulnerable older adults’ physical function according to the Japanese Long-Term Care Insurance (LTCI) system and Fried’s criteria for frailty syndrome. Arch Gerontol Geriatr. 2012;55:385–391.
Allampati S, Duarte-Rojo A, Thacker LR, et al. Diagnosis of minimal hepatic encephalopathy using stroop encephalapp: a multicenter US-based, norm-based study. Am J Gastroenterol. 2016;111:78–86.
Ney M, Tangri N, Dobbs B, et al. Predicting hepatic encephalopathy-related hospitalizations using a composite assessment of cognitive impairment and frailty in 355 patients with cirrhosis. Am J Gastroenterol. 2018;113:1506–1515.
Patidar KR, Thacker LR, Wade JB, et al. Covert hepatic encephalopathy is independently associated with poor survival and increased risk of hospitalization. Am J Gastroenterol. 2014;109:1757–1763.
Lai JC, Segev DL, McCulloch CE, Covinsky KE, Dodge JL, Feng S. Physical frailty after liver transplantation. Am J Transplant. 2018;18:1986–1994.
Murphy SL, Tapper EB, Blackwood J, Richardson JK. Why do individuals with cirrhosis fall? A mechanistic model for fall assessment, treatment, and research. Dig Dis Sci. 2019;64:316–323. https://doi.org/10.1007/s10620-018-5333-8.
Urios A, Mangas-Losada A, Gimenez-Garzo C, et al. Altered postural control and stability in cirrhotic patients with minimal hepatic encephalopathy correlate with cognitive deficits. Liver Int. 2017;37:1013–1022.
Felipo V, Urios A, Gimenez-Garzo C, et al. Non invasive blood flow measurement in cerebellum detects minimal hepatic encephalopathy earlier than psychometric tests. World J Gastroenterol. 2014;20:11815–11825.
Ezaz G, Murphy SL, Mellinger J, Tapper EB. Increased morbidity and mortality associated with falls among patients with cirrhosis. Am J Med. 2018;131:645–650.
Ahluwalia V, Wade JB, White MB, et al. Brain integrity changes underlying cognitive and functional recovery postliver transplant continue to evolve over 1 year. Transplantation. 2018;102:461–470.
Ahluwalia V, Wade JB, White MB, et al. Liver transplantation significantly improves global functioning and cerebral processing. Liver Transplant. 2016;22:1379–1390.
Fougère B, Daumas M, Lilamand M, et al. Association between frailty and cognitive impairment: cross-sectional data from toulouse frailty day hospital. J Am Med Dir Assoc. 2017;18:990.e1–990.e5.
Feng L, Nyunt MS, Gao Q, et al. Physical frailty, cognitive impairment, and the risk of neurocognitive disorder in the singapore longitudinal ageing studies. J Gerontol A Biol Sci Med Sci. 2017;72:369–375.
Tapper EB, Konerman M, Murphy S, Sonnenday CJ. Hepatic encephalopathy impacts the predictive value of the Fried Frailty Index. Am J Transplant. 2018;18:2566–2570.
Lai JC, Rahimi R, Verna EC, et al. Frailty associated with waitlist mortality independent of ascites and hepatic encephalopathy in a multi-center study. Gastroenterology. 2019;156:1675–1682.
Funding
Funding was provided by National Institutes of Health US (Grant Nos. R01DK089713, R21TR002024, T32DK007150) an VA merit Review Award (Grant No. 2I0CX001076).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None for any authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Acharya, C., White, M.B., Fagan, A. et al. Liver Transplant Is Associated with Sustained Improvement in Tandem Gait and Risk of Falls. Dig Dis Sci 66, 1360–1366 (2021). https://doi.org/10.1007/s10620-020-06261-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06261-y