Abstract
Background
Short bowel syndrome (SBS) resulting from extensive intestinal resection is thought to significantly affect gut microbiota. Data are limited on the signatures of the intestinal microbiome in SBS with different anatomical types.
Aims
The aim of our investigation was to characterize the composition and function of gut microbiota in SBS with or without ileocecal resection (ICR).
Methods
Six-week-old male Sprague-Dawley rats underwent 75% small bowel resection (SBR) with the ileocecal junction intact (SBR group, jejunoileal anastomosis, n = 10) or removed (ICR group, jejunocolic anastomosis, n = 10), or sham surgery (sham group, n = 10). Colonic contents of the rats were collected 28 days after operation, and 16S rRNA gene sequencing was performed on the MiSeq Illumina platform to analyze bacterial composition.
Results
Overall structures of the gut microbiome differed significantly among the three groups. The bacterial α-diversity of the ICR group was remarkably lower than that of the sham group. ICR rats were enriched with Lactobacillus and opportunistic pathogens from Proteobacteria but depleted of commensal genera belonging to the Lachnospiraceae, Ruminococcaceae and Erysipelotrichaceae families. Genera from the Bacteroidales S24-7 group, Porphyromonadaceae, Prevotellaceae, Rikenellaceae and Christensenellaceae were prevalent in SBR rats. Functional pathways of branched-chain and aromatic amino acid biosynthesis, lipopolysaccharide biosynthesis and infectious diseases were abundant in the ICR group, while SBR rats featured pathways of C5 branched dibasic acid metabolism, biotin metabolism and one carbon pool folate.
Conclusions
ICR causes dramatically more severe intestinal dysbiosis than SBR only in SBS rat models, resulting in altered functional profiles of the gut microbiome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Short bowel syndrome (SBS) is defined as the inability of the gastrointestinal tract to maintain protein-energy, fluid, electrolyte or micronutrient balances because of an insufficient absorptive area resulting from extensive small bowel resection, congenital defects or disease [1]. Patients with SBS are at high risk of malnutrition and long-term dependence on parenteral nutrition (PN) for survival. During the first 2 years after intestinal resection, the remnant small bowel undergoes some adaptive process, both structurally and functionally, to compensate for malabsorption and help patients wean off PN [2]. Factors influencing intestinal adaptation include the extent and anatomy of intestinal loss, gut microbiota and intestinal hormones [3,4,5].
The gut microbiota plays a major role in energy salvage, metabolic functions and immune modulation, and disturbance in the composition and function of these intestinal microbes is associated with numerous diseases [6, 7]. In recent years, a host of studies with growing frequency have investigated the altered intestinal microbiota in patients with SBS, reporting decreased microbial diversity, increased relative abundance of pathogenic bacteria and small bowel bacterial overgrowth [8,9,10]. SBS-associated gut dysbiosis could result in mucosal inflammation, delayed enteral diet, prolonged PN dependence, D-lactic acidosis, hepatobiliary complications, poor growth and consequently impaired outcomes [11,12,13].
SBS can be divided into different anatomical types based on whether ileocecal resection (ICR) was performed [14]. Patients who undergo ICR usually have poorer intestinal adaptation and worse clinical outcomes, which is probably associated with changes in the gut microbiome [15]. Although there is no lack of studies focusing on the bacterial alterations in SBS patients so far, few studies have distinguished between the two anatomical types. Additionally, in research, the most commonly studied model of SBS resects the mid-intestine of varying lengths but maintains the intact ileocecal junction [16, 17], although the intestinal anatomy of human SBS patients is more represented by ICR. The ileocecal junction is composed of the terminal ileum, ileocecal valve and colon in continuity, the value of which is evidenced by slower transit due to the ileal brake effect, a barrier to anterograde reflux from the large to the small intestine and colonic salvage of extra calories from bacterial fermentation [14, 15, 18]. Therefore, this project was carried out to describe the compositional and functional profiles of the intestinal microbiome in rat SBS models with/without ICR by high-throughput sequencing technology. We hypothesize that the resection of the ileocecal junction will have a greater impact on the alterations of the gut microbiome in SBS due to the severely disrupted microenvironment.
Methods
Animals and Experimental Procedures
Four-week-old male Sprague-Dawley rats (Cavens Lab Animals, Changzhou, China) were housed in groups of five in an animal facility with a 12-h light-dark cycle. Animals were allowed water and solid chow ad libitum before the experiment. All animals received humane care, and this study was approved by the Animal Experimental Ethics Committee of the Shanghai Ninth People’s Hospital, Shanghai JiaoTong University School of Medicine.
At 5 weeks of age, rats were transferred to a nutrient-fortified water gel (DietGel Recovery, ClearH2O, USA) and kept on this diet for 1 week until operation. At 6 weeks of age, rats were randomly assigned to three surgical groups (10 rats per group): sham, SBR (75% mid-intestinal resection with the ileocecal junction intact) and ICR (75% distal-intestinal resection with the ileocecal junction removed). Rats were anesthetized by inhalation with 2% isoflurane before surgery. The sham operation was performed by transection and reanastomosis of the bowel approximately 75 cm proximal to the ileocecal junction. In the SBR group, the small intestine was divided approximately 4–5 cm distal to the ligament of Treitz and 20 cm proximal to the ileocecal junction. In the ICR group, the intestine was transected at the site 75 cm proximal to the ileocecal junction and the site 1 cm distal to the cecum in the colon. The mesentery was ligated, and the intervening bowel was excised. The resection margins were anastomosed by an end-to-end, single-layer method using 7–0 braid sutures. During the operation, we measured the entire resected bowel to ensure 75% resection, and, if necessary, we made adjustments by resecting the bowel further. The rats were resuscitated by intraperitoneal injection of 4 ml 0.9% saline solution and kept in a warm incubator with free access to water for the first postoperative 24 h. After that, rats were housed individually, fed on the water gel for 1 week and then allowed water and solid chow ad libitum until the end of the study.
Sample Collection and DNA Extraction
On postoperative day 28, rats were killed, and colonic contents were collected from a section of descending colon that was 5 cm proximal to the anal verge. Samples were flash frozen in liquid nitrogen and then stored at − 80 °C until analysis. Genomic DNA was extracted from each sample using the QIAamp DNA Stool Mini Kit (Qiagen, Valencia, CA) according to the manufacturer’s instructions with minor modifications.
Bacterial Sequencing
The bacterial 16S rRNA genes were amplified using 515F (5′-GTGCCAGCMGCCGCGGTAA-3′) and 926R (5′-CCGTCAATTCMTTTGAGTTT-3′) primers targeting the V4–V5 hypervariable region. The primers were tailed with sequences to incorporate Illumina flow cell adapters with indexing barcodes. After polymerase chain reaction (PCR), barcoded 16S amplicons were purified and quantified and then pooled and paired-end (2 × 300 bp) sequenced on the MiSeq platform (Illumina, San Diego, CA).
Raw sequences were demultiplexed using exact matches to the supplied DNA barcodes and quality filtered with the parameters of SLIDINGWINDOW: 50:20 and MINLEN: 50. The paired-end reads were merged using the FLASH program [19], and low-quality merged reads were filtered with Mothur (V.1.33.3) based on read lengths < 200 bp and reads containing ambiguous bases containing homopolymers > 8 nucleotides or identified as a chimeric artifact [20]. The trimmed sequences were then clustered into operational taxonomical units (OTUs) at 97% similarity by the UPARSE algorithm [21]. Representative sequences in each OTU were classified taxonomically against the SILVA 128 database at 80% confidence using Mothur [22].
The sequencing data for our study are available in the NCBI Sequence Read Archive under accession no. SRP186877.
Bioinformatic and Statistical Analysis
Prior to further analysis, each sequence library was randomly subsampled to an even depth across all sequences. Microbial α-diversity indices were calculated by sampling-based OTUs using Mothur and compared by one-way ANOVA with the multiple correction test of Bonferroni. Differences in the relative abundance of bacterial taxa were evaluated with the Kruskal-Wallis test and corrected by Dunn’s test for multiple comparisons. The β-diversity was estimated using phylogenetic UniFrac (unweighted and weighted), Bray-Curtis and Jaccard distances. Permutational multivariate analysis of variance (PERMANOVA) was applied to compare β-diversity indices among the three groups, and significance was determined through 10,000 permutations. The dissimilarity among samples was explored by principal coordinate analysis (PCoA) based on Bray-Curtis distance and partial least squares discriminant analysis (PLS-DA). A heatmap of genus-level bacterial OTUs was built to identify the key variables of different groups. The PICRUSt (Phylogenetic Investigation of Communities by Reconstruction of Unobserved States) software was used to predict functional profiles based on 16S rRNA gene data [23]. Linear discriminant analysis (LDA) effect size (LEfSe) analysis was used to elucidate taxa and genes distinguishing the sham, SBR or ICR states. Both PICRUSt and LEfSe are available online in the Galaxy workflow framework (http://huttenhower.sph.harvard.edu/galaxy/). Adjusted p values < 0.05 were considered significant. The ANOVA and nonparametric tests were performed by GraphPad Prism version 7 (GraphPad software, La Jolla, CA), and the PERMANOVA, PCoA, PLS-DA and heatmap were conducted in R (V.3.5.1).
Results
A total of 30 rats, 10 in each group, underwent sham, SBR or ICR surgical procedures. Colonic contents were collected from each rat for final analysis, and a total of 919192 V4–V5 16S sequences were generated.
Community Structure of the Intestinal Microbiota in SBS Rat Models
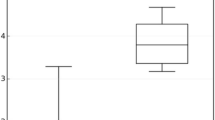
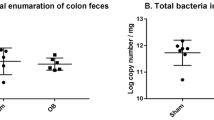
Rarefaction analysis showed that estimated OTU richness basically approached saturation in each group, and the richness significantly decreased in ICR rats versus sham and SBR rats (Fig. 1a). Likewise, ICR was associated with a lower microbial α-diversity of colonic content than sham and SBR when surveyed by the ACE index (P < 0.001), Shannon index (P < 0.001), Invsimpson index (P = 0.003 and P < 0.001, respectively) and phylogenetic diversity (PD; P < 0.001). However, there was no significant difference in α-diversity between the sham and SBR groups (Fig. 1b–e).
Comparative analyses of the microbial α-diversity among the sham and short bowel syndrome rat models with/without ileocecal resection (ICR). a Rarefaction curves of each group at 97% similarity. The estimated operational taxonomy unit (OTU) richness basically approached parallel, indicating that the total bacterial diversity present was well represented. Microbial α-diversity estimated by ACE index (b), Shannon index (c), Invsimpson index (d) and phylogenetic diversity (PD; e). The box plots depict the median and interquartile range (IQR), their whiskers denote 1.5 × IQR, and points indicate outlying values. **P < 0.01; ***P < 0.001 compared with the ICR group. SBR, small bowel resection
Using a variety of measures (unweighted and weighted UniFrac, Bray-Curtis and Jaccard distances), we detected remarkable differences (P = 0.0001) in β-diversity among different surgical models for all four distances. We visualized Bray-Curtis dissimilarity by PCoA, which suggested different overall microbial community structures among the sham, SBR and ICR groups. Although partial overlap was observed, samples from the same group were more homogeneous and tended to cluster together (Fig. 2a). Additionally, PLS-DA, a supervised analysis method, also allowed for the detection of a separated distribution among three groups, indicating a distinctive intestinal microbial composition (Fig. 2b).
Comparative analyses of the microbial structure of the sham and short bowel syndrome rat models with/without ileocecal resection (ICR). a Bacterial β-diversity of principal coordinates analysis (PCoA) based on Bray-Curtis distance indicated a separated distribution of the colonic microbial communities among all groups (P = 0.0001). b Partial least squares discriminant analysis (PLS-DA) plots based on the operational taxonomy unit (OTU) level showed the trend that the three groups were well separated. SBR, small bowel resection
Alterations in Intestinal Microbial Composition of SBS Rats Relative to Sham Rats
Bacteria identified in the colonic contents of the three surgical models included those from the six most dominant phyla such as Firmicutes, Bacteroidetes, Proteobacteria, Actinobacteria, Fusobacteria and Verrucomicrobia (Fig. 3a). Rats undergoing intestine resection displayed perturbed microbiota signatures relative to sham rats, while remarkable differences between SBR and ICR were also visible. In SBR rats, Firmicutes significantly decreased compared with sham and ICR (P = 0.033 and P = 0.006). For rats with ICR, Proteobacteria was dramatically enriched (P = 0.006 and P = 0.008), and Bacteroidetes was deficient (P = 0.021 and P < 0.001) compared with sham and SBR. In addition, relative to sham, Actinobacteria was less abundant in samples from ICR (P = 0.029). Both SBR and ICR rats had higher proportions of Fusobacteria (P = 0.006 and P = 0.007) and lower proportions of Verrucomicrobia (P = 0.034 and P < 0.001) than sham rats (Fig. 3b–g).
The taxonomic assessment of the colonic bacterial composition in the short bowel syndrome rat models with small bowel resection (SBR) only or ileocecal resection (ICR) at the phylum level. a Proportion of the phyla. b–g Median and interquartile range (IQR) of the relative abundance of each phylum in the colonic contents of rats with sham, SBR and ICR. *P < 0.05; **P < 0.01, sham vs. SBR; †P < 0.05; ††P < 0.01; †††P < 0.001, sham vs. ICR; ##P < 0.01; ###P < 0.001, SBR vs. ICR
Although no significant difference was found in the relative abundance of Firmicutes between ICR and sham, the families within the Firmicutes phylum were remarkably changed in ICR rats compared with sham and SBR rats, which included the loss of bacteria within the Lachnospiraceae (P < 0.001 and P = 0.018), Ruminococcaceae (P = 0.001 and P < 0.001) and Erysipelotrichaceae (P = 0.007 and P < 0.001) families and the enrichment of bacteria within the Lactobacillaceae (P = 0.036 and P < 0.001) family. Samples from SBR rats tended to have a lower abundance of Lachnospiraceae (P = 0.033) and Veillonellaceae (P = 0.021) than sham rats. The Bacteroidales S24-7 group dominated a large proportion of the Bacteroidetes phylum in SBR rats (P = 0.036 vs. sham and P < 0.001 vs. ICR); nevertheless, most families belonging to the Bacteroidetes phylum were nearly undetectable in ICR rats. Enterobacteriaceae contributed mostly to the prevalence of Proteobacteria in the ICR group compared with sham and SBR. Other pathogenic bacteria within the Proteobacteria phylum, including Pasteurellaceae (P = 0.008) and Comamonadaceae (P < 0.001), were also more abundant in ICR than sham. Conversely, some residential bacteria in sham, such as Coriobacteriaceae (P = 0.001), Deferribacteraceae (P = 0.001) and Verrucomicrobiaceae (P < 0.001), were lacking in the colonic contents of ICR rats. Compared with sham, both SBR and ICR samples had significantly increased relative abundance of the Fusobacteriaceae family (P = 0.006 and P = 0.007), which was considered to be pathogenic (Table 1, Fig. 4a).
Family and genus-level variations in the microbial community in the short bowel syndrome rat models with small bowel resection (SBR) only or ileocecal resection (ICR) relative to sham surgery. a Cladogram showing the taxonomic hierarchical structure of the distinguished phylotype generated by linear discriminant analysis effect size (LEfSe) analysis. Each filled circle represents one phylotype. b Heatmap representing the predominant genus-level microbes that significantly differed among the three surgical groups. The colored squares of each row were scaled to represent the relative ratios of the genera among 30 samples
Genus-Level Microbes Distinguishing Sham, SBR and ICR Rats
Genus-level bacterial taxa distinguishing three surgical groups were clustered by heatmap (Fig. 4b). There were statistically significant differences in the taxa dominating the ICR group and the other two groups, whereas rats with SBR had unique microbial signatures in addition to sharing similarity with the sham and ICR groups. Specifically, a variety of commensal bacterial genera distributed across the Verrucomicrobiaceae, Lachnospiraceae, Ruminococcaceae, Erysipelotrichaceae and Desulfovibrionaceae families, such as Akkermansia, Blautia, Butyrivibrio, Lachnoclostridium, Roseburia, Anaerotruncus, Butyricicoccus, Flavonifractor, Ruminiclostridium, Allobaculum and Desulfovibrio, were identified to be abundant in sham but depleted in ICR. In contrast, Lactobacillus and some pathogenic genera, including Escherichia-Shigella, Klebsiella, Proteus and Pasteurella, were indicative of ICR state. Additionally, several genera from the Bacteroidales S24-7 group, Porphyromonadaceae, Prevotellaceae, Rikenellaceae and Christensenellaceae, were unique to SBR.
Signatures of the Functional Profiles of Gut Microbiota in SBS Rats With/Without ICR
Using PICRUSt, we examined how the microbial metabolic and functional pathways changed after SBR and ICR based on the KEGG pathway. As a whole, the genetic profiles clustered together by surgical procedures despite some overlaps between sham and SBR. Our PCoA plot showed a statistically significant distinction among the three groups based on Bray-Curtis distances (P < 0.0001, Fig. 5a). We also identified 18 metabolic modules that discriminated between different surgical anatomies by LEfSe (Fig. 5b). Within amino acid metabolism, the sham group was characterized by lysine biosynthesis and arginine and proline metabolism; instead, the ICR group was enriched with branched-chain and aromatic amino acid biosynthesis and cysteine and methionine metabolism. Furthermore, pathways responsible for glycolysis/gluconeogenesis, the pentose phosphate pathway, starch and sucrose metabolism and riboflavin metabolism were correlated with sham, whereas pathways of C5 branched dibasic acid metabolism, biotin metabolism and one carbon pool folate were featured in SBR. Additionally, lipopolysaccharide (LPS) biosynthesis and infectious diseases were abundant, while oxidative phosphorylation was depleted in the ICR group.
Functional metagenomic pathways of colonic microbiomes predicted by PICRUSt (Phylogenetic Investigation of Communities by Reconstruction of Unobserved States). a Results from linear discriminant analysis (LDA) effect size (LEfSe) analysis, identifying pathways that differentiated the sham and short bowel syndrome (SBS) rat models with/without ileocecal resection (ICR). Only significant pathways with LDA > 3.0 are shown. b Principal coordinates analysis (PCoA) of Bray-Curtis dissimilarity based on the relative abundance of pathways of the sham and SBS rat models with/without ICR. SBR, small bowel resection
Discussion
In this study, we comprehensively described the colonic microbial signatures of rats following massive SBR with/without ICR. To date, several murine models of SBS that differ in the extent and site of intestine resection have been studied [5, 24]. Although murine models with 50% proximal SBR have lower mortality and may serve as useful tools to explore the mechanisms of intestinal adaptation, they do not mimic extensive SBR or severe ICR conditions, which are more commonly observed in human patients with SBS and intestinal failure [18]. Hence, we performed 75% SBR with/without ICR in the present study to better understand the pathophysiologic and microbial variations of the intestine in SBS conditions. As few differences in gut microbiota have been detected between sham and nonoperative animal models [16], we used only sham-operated rats as controls in this study.
The similar clustering patterns of both the PCoA and PLS-DA strongly suggested distinguished microbial structures among the sham, SBR and ICR groups. Moreover, the significant differences in β-diversity based on unweighted and weighted UniFrac, Bray-Curtis and Jaccard distances indicated that the alterations in the microbial community were due not only to the change in the number of bacterial species but also to the change in specific bacterial abundance [25]. Surprisingly, we did not find significant differences in bacterial α-diversity arising only from SBR; instead, decreased bacterial diversity and richness were observed only in the ICR group, which reveals the importance of the ileocecal junction in maintaining the relatively normal intestinal microbiome. Although both SBR and ICR lead to shortened small bowel, ICR remarkably alters the luminal microenvironment, as loss of the ileocecal valve causes rapid shunting of luminal content from the upper intestine into the colon and loss of the distal ileum results in bile salt malabsorption [16, 26]. These changes expose the residential bacteria in the colon to both digesta and bile acids, which is conducive to the proliferation of only specific opportunistic bacteria and against the survival of numerous commensal bacteria.
There was a striking overabundance of Proteobacteria and its family Enterobacteria in the colonic contents of ICR rats, which composes only a minor proportion of the healthy gut microbiota. The findings were in line with previous studies in which such a change was seen in pediatric and adult SBS patients, the majority of whom lost the ileocecal valve [9, 10, 27]. Many opportunistic pathogens within the Enterobacteria family, including Escherichia, Shigella, Klebsiella and Proteus, were dramatically prevalent in the ICR group, and their potential ability to produce LPS led to the upregulation of proinflammatory cytokines, the disruption of the intestinal epithelial barrier and the translocation of bacteria [28, 29]. Thus, the phylum Proteobacteria has been reported as a possible contributing factor to parenteral nutrition-associated liver disease (PNALD) and central line-associated blood stream infection (CLABSI) [12]. The gut dysbiosis featured by the dominance of gram-negative proinflammatory bacteria further reflects the pathologic conditions of the intestine after ICR with impaired microbial balances and mucosal innate immunity.
Although the phylum Firmicutes dominates the healthy gut, it unexpectedly thrived in rats with ICR at the expense of depletion of Bacteroidetes, which was primarily triggered by the increase in Lactobacillus. This change was consistent with other studies focusing on SBS patients, but the intestinal anatomy had not been distinguished [1, 4, 28, 30]. Given that members of Lactobacillus are more commonly found in the small intestine of healthy subjects [31], the unconventional dominance of Lactobacillus in the colonic contents of ICR rats conformed to the surgical procedures of ileocecal valve resection and jejunocolic anastomosis, which were favorable for the growth of species within Lactobacillus. However, certain Lactobacillus species are able to produce D-lactic acid by fermenting mono- and oligosaccharides, the poor metabolism and accumulation of which may contribute to neurologic dysfunction [32]. In addition to acidosis, the acid-producing Lactobacillus was also reported to play a role in causing diarrheal symptoms in the context of a short bowel in children [27]. Another study of pediatric SBS patients clarified that lack of Lactobacillus was associated with poor growth [10], and some strains of Lactobacillus can promote intestinal adaptation [33]. Consequently, the overgrowth of Lactobacillus may also compensate for the poor intestinal structures and functions of ICR rats, as SBR and sham rats had similar proportions of Lactobacillus.
Another prominent alteration within the Firmicutes phylum in ICR rats was the deficiency of genera from the Lachnospiraceae and Ruminococcaceae families, which are capable of producing short-chain fatty acids (SCFAs). As important bacterial metabolites, SCFAs, especially butyrate, can easily be oxidized in intestinal epithelial cells after being absorbed and serve as energy-supplying fuel for colonocytes [34]. Since the SCFA receptor, free fatty acid receptor 3 (FFA3), is expressed on glucagon-like peptide 2 (GLP-2)-secreting enteroendocrine L cells [35, 36], SCFAs are thought to be important in achieving intestinal adaptation because of the intestinotrophic activity of GLP-2, which induces enterocyte proliferation and differentiation [37]. SCFAs can also promote epithelial cell secretion of antimicrobial peptides and help maintain epithelial integrity by modulating the production of immune mediators such as IL-18 [38]. In addition, inhibition of histone deacetylase by butyrate leads to a decrease in the expression of proinflammatory cytokine in intestinal macrophages and dendritic cells [39]. As a consequence, loss of these SCFA-producing bacteria in ICR rats could delay gut adaptation and increase intestinal inflammation. Alternatively, in SBS patients, it might be promising to supplement SCFAs as a trophic factor to stimulate intestinal adaptation, and fecal SCFAs may also be used as a biomarker to judge intestinal conditions and guide clinical practice, such as the timing of enteral nutrition [40].
When considering the functional profiles of gut microbiota, their changes reflected host physiology. The enriched lysine biosynthesis pathway mapped to the normal dominant phyla of Firmicutes and Bacteroidetes in sham rats [41], while the enhanced LPS biosynthesis was in accordance with the prevalence of Proteobacteria in ICR rats. Intriguingly, the pathways of branched-chain and aromatic amino acid biosynthesis, which were identified as biomarkers for poor growth in pediatric SBS patients [10], were featured in the ICR rats. Arginine might prevent serious infection in newborns [42], and biotin was confirmed to inhibit Escherichia coli adherence and infection in the large intestine [43]. Therefore, the enrichment of arginine and biotin metabolism pathways in sham and SBR rats, respectively, demonstrated better intestinal immunity conditions and perhaps lower gut inflammation levels than in ICR rats. Conversely, the overabundance of the pathways of infectious disease in rats with ICR revealed colonization of pathogenic bacteria. The greater proportions of pathways responsible for galactose and starch metabolism in sham rats suggested SCFA-producing Lachnospiraceae proliferation [41]. Additionally, lysine provides a substrate for acetate and butyrate synthesis [44], and butyrate stress can promote the upregulation of riboflavin synthesis [45]; as a result, the enrichment of lysine synthesis and riboflavin metabolism pathways in sham rats indicated adaptation to SCFAs. The reduction in carbohydrate metabolism, including glycolysis, gluconeogenesis and the pentose phosphate pathway, and oxidative phosphorylation in both SBR and ICR rats strongly signified the low capacity of energy harvest and poor growth. Although high overall accuracy was obtained, the limitations of PICRUSt in inferring gene functions should be considered. For example, the prediction depends on a database of reference genomes, and it cannot summarize gene families into pathways if those genes are not included in the input genomic data used [23]. The PICRUSt output may also allocate particular pathways to specific bacteria even though those do not represent the true function in the bacteria [46]. Additionally, functional pathways with highly variable distributions may lead to incorrect predictions in individual cases [23]. Thus, the predicted functional profiles must be confirmed by further metagenomic shotgun analysis.
In summary, our study determines that, compared with SBR only, ICR results in more robust disturbances in the intestinal microbiome, including prominently decreased bacterial diversity, overabundance of Proteobacteria and Lactobacillus, lack of SCFA-producing commensal bacteria, and subsequent altered metabolic pathways. Because ICR is a common surgical choice for intestinal diseases, such as radiation enteritis and inflammatory bowel disease, our findings may primarily contribute to the development of targeted therapy strategies for intestinal rehabilitation in different types of SBS patients based on gut microbes and their metabolites. However, further studies assessing mucosa-associated microflora and using metagenomic sequencing technology are needed to provide deep insights into SBS clinical management.
References
Engstrand Lilja H, Wefer H, Nyström N, Finkel Y, Engstrand L. Intestinal dysbiosis in children with short bowel syndrome is associated with impaired outcome. Microbiome. 2015;3:18.
Tappenden KA. Intestinal adaptation following resection. J Parenter Enter Nutr. 2014;38:23S–31S.
Engelstad HJ, Barron L, Moen J, et al. Remnant small bowel length in pediatric short bowel syndrome and the correlation with intestinal dysbiosis and linear growth. J Am Coll Surg. 2018;227:439–449.
Gillard L, Mayeur C, Robert V, et al. Microbiota is involved in post-resection adaptation in humans with short bowel syndrome. Front Physiol. 2017;8:224.
Berlin P, Reiner J, Wobar J, et al. Villus growth, increased intestinal epithelial sodium selectivity, and hyperaldosteronism are mechanisms of adaptation in a murine model of short bowel syndrome. Dig Dis Sci. 2019;64:1158–1170. https://doi.org/10.1007/s10620-018-5420-x
Clemente JC, Ursell LK, Parfrey LW, Knight R. The impact of the gut microbiota on human health: an integrative view. Cell. 2012;148:1258–1270.
Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375:2369–2379.
Huang Y, Guo F, Li Y, Wang J, Li J. Fecal microbiota signatures of adult patients with different types of short bowel syndrome. J Gastroenterol Hepatol. 2017;32:1949–1957.
Boccia S, Torre I, Santarpia L, et al. Intestinal microbiota in adult patients with short bowel syndrome: preliminary results from a pilot study. Clin Nutr. 2017;36:1707–1709.
Piper HG, Fan D, Coughlin LA, et al. Severe gut microbiota dysbiosis is associated with poor growth in patients with short bowel syndrome. J Parenter Enter Nutr. 2017;41:1202–1212.
Korpela K, Mutanen A, Salonen A, Savilahti E, de Vos WM, Pakarinen MP. Intestinal microbiota signatures associated with histological liver steatosis in pediatric-onset intestinal failure. J Parenter Enter Nutr. 2017;41:238–248.
Wang P, Wang Y, Lu L, et al. Alterations in intestinal microbiota relate to intestinal failure-associated liver disease and central line infections. J Pediatr Surg. 2017;52:1318–1326.
Cole CR, Frem JC, Schmotzer B, et al. The rate of bloodstream infection is high in infants with short bowel syndrome: relationship with small bowel bacterial overgrowth, enteral feeding, and inflammatory and immune responses. J Pediatr. 2010;156:941–947.
Bechtold ML, McClave SA, Palmer LB, et al. The pharmacologic treatment of short bowel syndrome: new tricks and novel agents. Curr Gastroenterol Rep. 2014;16:392.
Jeppesen PB. Spectrum of short bowel syndrome in adults: intestinal insufficiency to intestinal failure. J Parenter Enter Nutr. 2014;38:8S–13S.
Lapthorne S, Pereira-Fantini PM, Fouhy F, et al. Gut microbial diversity is reduced and is associated with colonic inflammation in a piglet model of short bowel syndrome. Gut Microbes. 2013;4:212–221.
Sommovilla J, Zhou Y, Sun RC, et al. Small bowel resection induces long-term changes in the enteric microbiota of mice. J Gastrointest Surg. 2015;19:56–64.
Matsumoto Y, Mochizuki W, Akiyama S, et al. Distinct intestinal adaptation for vitamin B12 and bile acid absorption revealed in a new mouse model of massive ileocecal resection. Biol Open. 2017;6:1364–1374.
Magoč T, Salzberg SL. FLASH: fast length adjustment of short reads to improve genome assemblies. Bioinformatics. 2011;27:2957–2963.
Schloss PD, Westcott SL, Ryabin T, et al. Introducing mothur: open-source, platform-independent, community-supported software for describing and comparing microbial communities. Appl Environ Microbiol. 2009;75:7537–7541.
Edgar RC. UPARSE: highly accurate OTU sequences from microbial amplicon reads. Nat Methods. 2013;10:996–998.
Quast C, Pruesse E, Yilmaz P, et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 2013;41:590–596.
Langille MG, Zaneveld J, Caporaso JG, et al. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat Biotechnol. 2013;31:814–821.
Sangild PT, Ney DM, Sigalet DL, Vegge A, Burrin D. Animal models of gastrointestinal and liver diseases. Animal models of infant short bowel syndrome: translational relevance and challenges. Am J Physiol Gastrointest Liver Physiol. 2014;307:G1147–G1168.
Levesque CL, Turner J, Li J, et al. In a neonatal piglet model of intestinal failure, administration of antibiotics and lack of enteral nutrition have a greater impact on intestinal microflora than surgical resection alone. J Parenter Enter Nutr. 2017;41:938–945.
Devine AA, Gonzalez A, Speck KE, et al. Impact of ileocecal resection and concomitant antibiotics on the microbiome of the murine jejunum and colon. PLoS ONE. 2013;8:e73140.
Davidovics ZH, Carter BA, Luna RA, Hollister EB, Shulman RJ, Versalovic J. The Fecal microbiome in pediatric patients with short bowel syndrome. J Parenter Enter Nutr. 2016;40:1106–1113.
Shin NR, Whon TW, Bae JW. Proteobacteria: microbial signature of dysbiosis in gut microbiota. Trends Biotechnol. 2015;33:496–503.
Bizari L, da Silva Santos AF, Foss NT, et al. Parenteral nutrition in short bowel syndrome patients, regardless of its duration, increases serum proinflammatory cytokines. Nutr Res. 2016;36:751–755.
Joly F, Mayeur C, Bruneau A, et al. Drastic changes in fecal and mucosa-associated microbiota in adult patients with short bowel syndrome. Biochimie. 2010;92:753–761.
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104:13780–13785.
Kowlgi NG, Chhabra L. D-lactic acidosis: an underrecognized complication of short bowel syndrome. Gastroenterol Res Pract. 2015;2015:476215.
Tolga Muftuoglu MA, Civak T, Cetin S, Civak L, Gungor O, Saglam A. Effects of probiotics on experimental short-bowel syndrome. Am J Surg. 2011;202:461–468.
Schönfeld P, Wojtczak L. Short- and medium-chain fatty acids in energy metabolism: the cellular perspective. J Lipid Res. 2016;57:943–954.
Akiba Y, Inoue T, Kaji I, et al. Short-chain fatty acid sensing in rat duodenum. J Physiol. 2015;593:585–599.
Iwasaki M, Akiba Y, Kaunitz JD. Duodenal chemosensing of short-chain fatty acids: implications for GI diseases. Curr Gastroenterol Rep. 2019;21:35.
Jeppesen PB. Teduglutide, a novel glucagon-like peptide 2 analog, in the treatment of patients with short bowel syndrome. Ther Adv Gastroenterol. 2012;5:159–171.
Qing Y, Xie H, Su C, et al. Gut microbiome, short-chain fatty acids, and mucosa injury in young adults with human immunodeficiency virus infection. Dig Dis Sci. 2019;64:1830–1843. https://doi.org/10.1007/s10620-018-5428-2
Chang PV, Hao L, Offermanns S, et al. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc Natl Acad Sci USA. 2014;111:2247–2252.
Neelis E, de Koning B, Rings E, et al. The gut microbiome in patients with intestinal failure: current evidence and implications for clinical practice. J Parenter Enter Nutr. 2019;43:194–205.
Baumann-Dudenhoeffer AM, D’Souza AW, Tarr PI, Warner BB, Dantas G. Infant diet and maternal gestational weight gain predict early metabolic maturation of gut microbiomes. Nat Med. 2018;24:1822–1829.
Badurdeen S, Mulongo M, Berkley JA. Arginine depletion increases susceptibility to serious infections in preterm newborns. Pediatr Res. 2015;77:290–297.
Yang B, Feng L, Wang F, Wang L. Enterohemorrhagic Escherichia coli senses low biotin status in the large intestine for colonization and infection. Nat Commun. 2015;6:6592.
Neis EP, Dejong CH, Rensen SS. The role of microbial amino acid metabolism in host metabolism. Nutrients. 2015;7:2930–2946.
Alsaker KV, Paredes C, Papoutsakis ET. Metabolite stress and tolerance in the production of biofuels and chemicals: gene-expression-based systems analysis of butanol, butyrate, and acetate stresses in the anaerobe Clostridium acetobutylicum. Biotechnol Bioeng. 2010;105:1131–1147.
Shapiro J, Cohen NA, Shalev V, Uzan A, Koren O, Maharshak N. Psoriatic patients have a distinct structural and functional fecal microbiota compared with controls. J Dermatol. 2019 [Epub ahead of print]. https://doi.org/10.1111/1346-8138.14933.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (grant no. 81270945) and Clinical Research Program of 9th People’s Hospital, Shanghai JiaoTong University School of Medicine (grant no. JYLJ022).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national and/or institutional guidelines for the care and use of animals were followed. All procedures performed in the study involving animals were approved by the Animal Experimental Ethics Committee of the Shanghai Ninth People’s Hospital, Shanghai JiaoTong University School of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, Y., Chen, A., Guo, F. et al. Severe Intestinal Dysbiosis in Rat Models of Short Bowel Syndrome with Ileocecal Resection. Dig Dis Sci 65, 431–441 (2020). https://doi.org/10.1007/s10620-019-05802-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05802-4