Abstract
Background
Pretreatment biopsy may not correctly diagnose mixed-type early gastric cancers. Despite reports on the usefulness of magnifying endoscopy with narrow-band imaging in diagnosing early gastric cancers, no reports exist on differences in magnifying endoscopy with narrow-band imaging findings between differentiated-type-predominant mixed-type and undifferentiated-type-predominant mixed-type early gastric cancers.
Aim
This study aimed to clarify differences in magnifying endoscopy with narrow-band imaging findings and investigate the additive effect of combining magnifying endoscopy with narrow-band imaging and biopsy findings for pretreatment histological-type diagnosis.
Methods
Patients undergoing endoscopic submucosal dissection as initial treatment between April 2005 and March 2017 participated in this retrospective study. There were 156 differentiated-type-predominant mixed-type and 36 undifferentiated-type-predominant mixed-type lesions. We extracted the most significant magnifying endoscopy with narrow-band imaging findings of differentiated-type-predominant mixed-type and undifferentiated-type-predominant mixed-type lesions using multivariate analysis and compared the accuracy, sensitivity, and specificity between pretreatment biopsy alone and a combination of biopsy and magnifying endoscopy with narrow-band imaging findings.
Results
Significant magnifying endoscopy with narrow-band imaging findings was fine network pattern in differentiated-type-predominant and corkscrew pattern in undifferentiated-type-predominant mixed-type lesions. Accuracy, sensitivity, and specificity were significantly higher with combined biopsy and magnifying endoscopy with narrow-band imaging findings than with pretreatment biopsy alone.
Conclusions
The study results demonstrated the additive effect of magnifying endoscopy with narrow-band imaging with biopsy for diagnosing mixed-type early gastric cancers. This study may be beneficial in routine practice because it indicates a possibility of reducing additional surgery after endoscopic submucosal resection because of incorrect diagnosis of histological type.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the development of endoscopic submucosal dissection (ESD) for early gastric cancer (EGC) [1,2,3,4], lesions that previously required surgical treatment have become amenable through less invasive endoscopic resection procedures. The indication for ESD is stipulated in the Japanese Gastric Cancer Treatment Guidelines (JGCTG) [5] and depends on the histological type of gastric cancer [6, 7]. For differentiated-type (DT) EGCs, indication for ESD is intramucosal carcinoma with or without an ulcer and the tumor measuring ≤ 30 mm in diameter [5]. For undifferentiated-type (UDT) EGCs, intramucosal carcinoma without an ulcer and the tumor measuring ≤ 20 mm is the only indication for ESD [5].
Mixed-type (MT) gastric cancer demonstrates the components of DT and UDT. According to the JGCTG, DT-predominant mixed-type (D-MT) cancers should be considered as DT cancers, whereas UDT-predominant mixed-type (UD-MT) cancers should be considered as UDT cancers [5].
Generally, the histological type is diagnosed by pretreatment biopsy [5, 8, 9]. Gastric cancer with only the DT or UDT component can be correctly diagnosed to be of the same histological type with pretreatment biopsy or posttreatment histological analysis. However, pretreatment biopsy may be unable to diagnose the predominant MT histology because both DT and UDT components are present in MT. For example, in UD-MT cancer, if the pretreatment biopsy specimen is obtained from a patient with DT, the histological type may be diagnosed as DT. Thus, indication for ESD should be determined for UDT in this case; however, indication for ESD might be determined for DT as well. Therefore, if UDT cancer is diagnosed as DT by pretreatment biopsy, chances of additional surgery after ESD because of incorrect diagnosis of histological type might increase.
The findings of magnifying endoscopy with narrow-band imaging (ME-NBI) are useful in diagnosing gastric cancer [10,11,12] and exhibit characteristics of DT and UDT [13,14,15,16,17,18]. Thus, diagnosis with ME-NBI is suggested for MT gastric cancers; however, there are no reports available for MT. Furthermore, when characteristics of DT and UDT findings are observed, it is necessary to distinguish D-MT from UD-MT. To the best of our knowledge, there are no studies evaluating the difference between ME-NBI findings of D-MT and UD-MT EGCs.
Thus, this study aimed to clarify the difference between ME-NBI findings of D-MT and UD-MT EGCs. The study also aimed to clarify the additive effect of combining ME-NBI with biopsy in diagnosing pretreatment histological type in MT-EGCs.
Methods
Patients
This was a single-center retrospective study. Patients were diagnosed with either D-MT or UD-MT and underwent ESD as initial treatment at our institution between April 2005 and March 2017. All patient information was extracted from electronic records. All patients undergoing treatment for EGCs were provided a detailed explanation of the advantages and disadvantages of ESD.
Criteria
Inclusion criteria were as follows: (1) The pretreatment biopsy specimen was obtained from the center of the lesion (retrospectively, we can confirm biopsy location on imaging) and evaluated by pathologists in our hospital (to ensure uniformity of pathological diagnosis); (2) ME-NBI of the whole lesion was performed under high magnification, and the endoscopic image was available to be viewed later; and (3) the case was determined as MT on posttreatment histological-type diagnosis. The exclusion criteria were as follows: (1) Endoscopic images could not be evaluated because of poor image quality (owing to bleeding, halation, defocus, blur, or mucus); (2) ME-NBI was performed under high magnification in only part of the lesion; (3) biopsy was performed at another hospital, and multiple biopsies were performed on the lesion (because only one biopsy is usually performed at our hospital in principle); and (4) no cancer was detected in the biopsy specimen.
Diagnosis and Comparison
After obtaining biopsy results, the predominant histological type was considered the pretreatment histological type. In the posttreatment pathological diagnosis, we classified MT as either D-MT or UD-MT. Age, sex, pretreatment factors (e.g., location, macroscopic type, main histological type by pretreatment biopsy, and ME-NBI findings), and posttreatment factors (e.g., tumor diameter, depth of invasion, presence of ulcerative findings, presence of lymphovascular invasion, number of R0 resections, number of curative resections, and number of additional surgeries after ESD because of incorrect diagnosis of histological type by biopsy) were recorded, and ME-NBI findings between the D-MT and UD-MT groups were compared. After extracting the most significant findings of D-MT and UD-MT by multivariate analysis, we clarified the breakdown of ME-NBI findings by pretreatment biopsy for posttreatment histological UD-MT and D-MT.
If both differentiated and undifferentiated findings are recognized, we cannot distinguish D-MT and UD-MT. Therefore, we defined the combined biopsy and ME-NBI group as follows: If the result of pretreatment biopsy was DT and there are no significant ME-NBI findings of D-MT, but there are significant ME-NBI findings of UD-MT, we diagnosed UD-MT as the pretreatment histological type. If the result of pretreatment biopsy was UDT and there are no significant ME-NBI findings of UD-MT, but there are significant ME-NBI findings of D-MT, we diagnosed D-MT as the pretreatment histological type. If the result of pretreatment biopsy was DT and there are only significant ME-NBI findings of D-MT or no significant ME-NBI findings, we diagnosed D-MT as the pretreatment histological type. If the result of pretreatment biopsy was UDT and there are only significant ME-NBI findings of UD-MT or no significant ME-NBI findings, we diagnosed UD-MT as the pretreatment histological type.
Based on this, we clarified the breakdown of posttreatment histology in the group who underwent pretreatment biopsy alone and the group with combined biopsy and ME-NBI findings. Next, we compared the sensitivity, specificity, and accuracy of pretreatment biopsy and the combination of pretreatment biopsy and ME-NBI.
This was done to clarify the additive effect of ME-NBI with biopsy for the diagnosis of pretreatment histological type in MT-EGCs.
Evaluation by ME-NBI
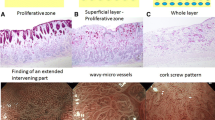
To evaluate ME-NBI findings, two specialists at the Japanese Gastrointestinal Endoscopy Society studied the findings from electronic medical records. They understood that the cases were diagnosed as having MT but were blinded to the histological-type (D-MT or UD-MT). We adopted the findings with consensus; if there was discrepancy between their opinions, they discussed the findings and reached a consensus. DT was defined by the fine network pattern and loop pattern, and UDT was defined by extended intervening parts, wavy microvessels, and the corkscrew pattern [13,14,15,16,17] (Fig. 1). The fine network pattern was defined as having a network like a mesh [13]. The loop pattern was defined as having loop-like microvessels not connected but having tubule-like or villus-like mucosal structures along them [13, 15]. The extended intervening part was defined as spaces between crypts being wider in cancerous mucosa compared to the surrounding noncancerous mucosa [17, 18]. Wavy microvessels were defined as vessels that draw curves or spirals without being connected [16]. The corkscrew pattern was defined as an isolated and disordered quality.14
Evaluation Criteria
We defined the evaluation criteria as follows:
Accuracy = (cases of correctly diagnosed posttreatment DT by pretreatment diagnosis + cases of correctly diagnosed posttreatment UDT by pretreatment diagnosis)/total cases.
Sensitivity = cases of correctly diagnosed posttreatment DT by pretreatment diagnosis/all cases of posttreatment DT.
Specificity = cases of correctly diagnosed posttreatment UDT by pretreatment diagnosis/all cases of posttreatment UDT.
Positive predictive value of DT = cases of correctly diagnosed posttreatment DT by pretreatment diagnosis/all cases of diagnosed pretreatment histology of DT.
Negative predictive value of DT = cases of correctly diagnosed posttreatment UDT by pretreatment diagnosis/all cases of diagnosed pretreatment histology of UDT.
Treatment After Diagnosis
All patients with EGCs treated by ESD underwent preoperative conventional endoscopy, dye-spraying endoscopy, and ME-NBI for determining tumor extent and depth. For ME-NBI, we first determined the demarcation between cancerous and noncancerous portions using low-magnification ME-NBI and observed all parts of the lesion under high magnification.
For each resected specimen of ESD, sections were prepared at 2.0-mm intervals for pathological evaluation. All pathological examinations were performed by two or more pathologists specialized in gastrointestinal pathology and were recorded as pathological reports of ESD in the electrical medical record. In this study, N.Y. (pathologist) confirmed that the actual pathological specimens and pathological reports were consistent in all cases. As a result, the pathological results indicate a consensus between two or more pathologists with regard to the diagnosis. End points were maximum tumor diameter, maximum invasion depth, histological type, ulcer, lymphovascular invasion, horizontal margin, and vertical margin. DT lesions measuring ≤ 30 mm with invasion into the superficial layer of the submucosa (SM < 500 µm) or with an ulcer, including a scar and intramucosal carcinomas measuring > 30 mm with no ulcers or scars, were regarded as curative criteria for ESD, and ESD was performed according to the JGCTG.5 UDT lesions measuring ≤ 20 mm with no ulcer or scar were regarded as curative criteria for ESD, and ESD was performed accordingly. The pathologists evaluated the resected specimen and measured the length of the component (DT or UDT). Accordingly, D-MT was defined as a case in which the DT component exceeded 50% of the lesion. Similarly, UD-MT was defined as a case in which the UDT component exceeded 50% of the lesion.
Differences among well-differentiated, moderately differentiated, and papillary types in DT components and those between signet ring cell carcinoma and poorly differentiated adenocarcinoma in UDT components were not considered different.
We used an electronic endoscopy system (EVIS LUCERA system and EVIS LUCERA ELITE system; Olympus Medical Systems, Tokyo, Japan) and standard endoscopy (GIF-H240Z, GIF-H260Z, and GIF-H290Z; Olympus Medical Systems) along with a soft hood (MAJ-1990 and MAJ-1989; Olympus Medical Systems) on the tip of the endoscope to enable mucosal fixation at a distance of approximately 2 mm, so that high magnification of ME-NBI could be easily obtained.
Statistical Analyses
Fisher’s exact probability test was used for two-group comparisons. On comparing ME-NBI findings between the posttreatment histological D-MT and UD-MT groups, items showing significant differences on univariate analysis were subjected to multivariate analysis, where the odds ratios (OR) and 95% confidence intervals (CI) were calculated. Sensitivity, specificity, and accuracy were compared between pretreatment biopsy and the combined pretreatment biopsy and ME-NBI group using McNemar’s test. Statistical significance was set at P < 0.05 for univariate and multivariate analyses. JMP software version 13.2 (SAS® Institute, Cary, NC, USA) was used for statistical processing.
Results
Among 3491 patients who underwent ESD as initial treatment at our hospital between April 2005 and March 2017, 2804 patients had pure DT, 324 patients had pure UDT, 297 patients with 298 lesions had D-MT, and 66 patients with 68 lesions had UD-MT EGC. On the basis of the exclusion criteria (biopsy performed at another hospital: 141 patients [including 20 patients who underwent multiple biopsies and 17 patients who underwent ME-NBI of only part of the lesion], poor image quality or ME-NBI performed in only part of the lesion: 32 patients, no cancer detected in the biopsy specimen: 0 patients), 142 D-MT patients with 142 lesions and 31 UD-MT patients with 32 lesions were excluded. Finally, 155 D-MT patients with 156 lesions and 35 UD-MT patients with 36 lesions were included.
Table 1 shows the background of the patients in the posttreatment histological D-MT and UD-MT groups. In the D-MT group, 87.8% of the main histological-type (DT) lesions were identified by pretreatment biopsy. The detection rate of DT findings by ME-NBI was 100% and that of UDT findings was 53.8%. In the UD-MT group, 33.3% of the main histological-type (UDT) lesions were identified by pretreatment biopsy. The detection rate of UDT findings by ME-NBI was 91.7%, whereas that of DT findings was 72.2%. The proportion of additional surgeries after ESD owing to incorrect diagnosis of histological type by biopsy was 0% in D-MT and 25.0% in UD-MT groups.
Table 2 shows the ME-NBI findings (fine network pattern, loop pattern, extended intervening part, wavy micro vessels, and corkscrew pattern) of the posttreatment histological D-MT and UD-MT groups. According to multivariate analysis, significant differences were present between the D-MT and UD-MT groups; this included the fine network pattern and corkscrew pattern. In D-MT, the significant ME-NBI finding was the fine network pattern. In UD-MT, the significant ME-NBI finding was corkscrew pattern.
Based on Table 2, Table 3 shows the breakdown of ME-NBI findings (fine network and corkscrew patterns) by pretreatment biopsy for posttreatment histological UD-MT and D-MT lesions.
Only corkscrew pattern, both fine network pattern and corkscrew pattern, only fine network pattern, and no findings were found.
Based on Table 3, we believed that combining biopsy and ME-NBI findings resulted in high accuracy. Therefore, Fig. 2 shows the algorithm for pretreatment diagnosis by combining biopsy and ME-NBI findings in the group with both DT and UDT findings and the group without those findings. In the group without ME-NBI findings, pretreatment biopsy findings become the pretreatment diagnosis of histological type. Based on Table 3 and Fig. 2, we show the breakdown of posttreatment histology by pretreatment biopsy and by combining biopsy and ME-NBI findings (Table 4). Using the data of Table 4, we compared the accuracy, sensitivity, and specificity of pretreatment biopsy alone and combined biopsy and ME-NBI findings (Table 5). The accuracy, sensitivity, and specificity were significantly higher with combined biopsy and ME-NBI findings than when using pretreatment biopsy alone.
Discussion
In this study, we investigated the difference between ME-NBI findings of D-MT and UD-MT and the additive effect of combining ME-NBI and biopsy findings for diagnosing pretreatment histological type in MT-EGC patients. To the best of our knowledge, this study is the first to report ME-NBI findings in cases of D-MT and UD-MT and discuss the additive effect of combining ME-NBI and biopsy findings in cases of MT-EGC.
In previous reports, the main histological-type detection rate according to preoperative biopsy was approximately 90% for DT (combined with the pure differentiated-type and D-MT) and approximately 80% for UDT (pure undifferentiated-type and UD-MT) [19, 20]. Moreover, Komatsu et al. [21] reported that 41/44 (93.2%) specimens with histologic-type discrepancy between pretreatment biopsy and surgically resected specimens were derived from MT gastric cancers. In this study, the histologic-type discrepancy between pretreatment biopsy and ESD specimens in MT was also present. Therefore, it was suggested that histological diagnosis based on pretreatment biopsy alone may be limited in MT.
Based on the above-mentioned data, we compared ME-NBI findings between D-MT and UD-MT groups. In the comparison, when both DT and UDT findings were observed, it suggested that the presence of the fine network pattern increased the possibility of D-MT and the presence of the corkscrew pattern increased the possibility of UD-MT. The following can be considered as the reason for this finding. Although the fine network pattern and corkscrew pattern are not similar, the loop pattern and wavy microvessels are similar, and it is difficult to distinguish them when they are simultaneously recognized. Because it was reported that the extended intervening part is also recognized in the presence of invading inflammatory cells [18], it is considered that there was no significant difference between D-MT and UD-MT.
However, if the above is considered, there were cases in which both DT (fine network pattern) and UDT (corkscrew pattern) findings were found or none of them was found. It was concluded that it is difficult to diagnose MT with ME-NBI alone. Therefore, we believe that combining biopsy and ME-NBI findings, as shown in Fig. 2, could be helpful for diagnosing MT and increasing accuracy.
Accuracy, sensitivity, and specificity were significantly higher when combining biopsy and ME-NBI findings than when using pretreatment biopsy alone. In other words, when combining biopsy and ME-NBI findings, both D-MT and UD-MT can be correctly diagnosed before treatment, and the accuracy is considered to be increased. Biopsy alone has limitations in local diagnosis and ME-NBI is considered to make a wider range of diagnoses; by combining biopsy and ME-NBI findings or diagnosis, accuracy was improved compared to that with pretreatment biopsy alone. Moreover, the proportion of additional surgeries after ESD owing to incorrect diagnosis of histological type by only biopsy was 25.0% in UD-MT group. However, according to the algorithm in Fig. 2, the proportion of additional surgeries after ESD owing to incorrect diagnosis became 8.3% (3 cases out of 36 cases) in the UD-MT group by combining ME-NBI with biopsy.
From the above, the additive effect of combining ME-NBI and biopsy findings for the diagnosis of pretreatment histological type in MT-EGCs was recognized. Since adding ME-NBI findings increased the possibility of distinction between D-MT and UD-MT, this study may be beneficial in routine practice.
This study has some limitations. First, because this study is a single-center, retrospective study, the sample size may be insufficient. Moreover, the outcomes in actual clinical practice may differ from the results of this study, depending on the doctor. Thus, further prospective multicenter research by many doctors is necessary to verify the possibility of identifying the dominant histological type using ME-NBI. Other limitations of this study include the use of a different system of NBI because of the chronological trends and it is impossible to know whether the diagnosis based on the biopsy was supported by a random biopsy in the lesion or not. Further, selective bias is likely in this study as patients who underwent surgery as the first line of treatment and those for whom ME-NBI was performed under high magnification in only part of the lesion were excluded. However, given that this study included MT cases over a period of 12 years at a cancer specialty hospital, our results do support routine practice.
In conclusion, the most notable difference between ME-NBI findings of D-MT and UD-MT is a fine network pattern in D-MT and corkscrew pattern in UD-MT. The additive effect of combining ME-NBI and biopsy findings for diagnosis of pretreatment histological type in MT-EGCs was recognized. This study may be beneficial in routine practice for patients with MT-EGC as there is a possibility of reducing additional surgeries after ESD because of incorrect histological-type diagnosis before treatment.
References
Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001;48:225–229.
Gotoda T, Kondo H, Ono H, et al. A new endoscopic mucosal resection procedure using an insulation-tipped diathermic knife for rectal flat lesions: report of two cases. Gastrointest Endosc. 1999;50:560–5763.
Ohkuwa M, Hosokawa K, Boku N, Ohtu A, Tajiri H, Yoshida S. New endoscopic treatment for intramucosal gastric tumors using an insulated-tip diathermic knife. Endoscopy. 2001;33:221–226.
Yamamoto H, Kawata H, Sunada K, et al. Success rate of curative endoscopic mucosal resection with circumferential mucosal incision assisted by submucosal injection of sodium hyaluronate. Gastrointest Endosc. 2002;56:507–512.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Gotoda T, Yanagisawa A, Sasako M, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225.
Hirasawa T, Gotoda T, Miyata S, et al. Incidence of lymph node metastasis and the feasibility of endoscopic resection for undifferentiated-type early gastric cancer. Gastric Cancer. 2009;12:148–152.
Allum WH, Blazeby JM, Griffin SM, et al. Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland, the British Society of Gastroenterology and the British Association of Surgical Oncology. Gut. 2011;60:1449–1472.
Thrumurthy SG, Chaudry MA, Hochhauser D, Mughal M. The diagnosis and management of gastric cancer. BMJ. 2013;347:f6367.
Yao K, Anagnostopoulos GK, Ragunath K. Magnifying endoscopy for diagnosing and delineating early gastric cancer. Endoscopy. 2009;41:462–467.
Ezoe Y, Muto M, Uedo N, et al. Magnifying narrowband imaging is more accurate than conventional white-light imaging in diagnosis of gastric mucosal cancer. Gastroenterology. 2011;141:2017–2025.
Muto M, Yao K, Kaise M, et al. Magnifying endoscopy simple diagnostic algorithm for early gastric cancer (MESDA-G). Dig Endosc. 2016;28:379–393.
Yagi K, Nakamura A, Sekine A, Umezu H. Magnifying endoscopy with narrow band imaging for early differentiated gastric adenocarcinoma. Dig Endosc. 2008;20:115–122.
Nakayoshi T, Tajiri H, Matsuda K, Kaise M, Ikegami M, Sasaki H. Magnifying endoscopy combined with narrow band imaging system for early gastric cancer: correlation of vascular pattern with histopathology (including video). Endoscopy. 2004;12:1080–1084.
Yokoyama A, Inoue H, Minami H, et al. Novel narrow-band imaging magnifying endoscopic classification for early gastric cancer. Dig Liver Dis. 2010;42:704–708.
Yagi K, Sato T, Nakamura A, Sekine A. The possibility and limitation of magnifying endoscopic diagnosis using NBI in the extent of undifferentiated intramucosal gastric adenocarcinoma. Stomach Intest. 2009;44:60–70. (in Japanese).
Okada K, Fujisaki J, Kasuga A, et al. Diagnosis of undifferentiated-type early gastric cancers by magnification endoscopy with narrow-band imaging. J Gastroenterol Hepatol. 2011;26:1262–1269.
Horiuchi Y, Fujisaki J, Yamamoto N, et al. Accuracy of diagnostic demarcation of undifferentiated-type early gastric cancers for magnifying endoscopy with narrow-band imaging: endoscopic submucosal dissection cases. Gastric Cancer. 2016;19:515–523.
Takao M, Kakushima N, Takizawa K, et al. Discrepancies in histologic diagnoses of early gastric cancer between biopsy and endoscopic mucosal resection specimens. Gastric Cancer. 2012;15:91–96.
Lim H, Jung HY, Park YS, et al. Discrepancy between endoscopic forceps biopsy and endoscopic resection in gastric epithelial neoplasia. Surg Endosc. 2014;28:1256–1262.
Komatsu S, Ichikawa D, Miyamae M, et al. Discrepancies in the histologic type between biopsy and resected specimens: a cautionary note for mixed-type gastric carcinoma. World J Gastroenterol. 2015;21:4673–4679.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
There are no conflicts of interest associated with this study.
Research involving human participants and/or animals
The study was approved by the Institutional Review Board (IRB) of our institution (IRB no. 2017-1068). This study was conducted in compliance with the principles of the Declaration of Helsinki and its later amendments. Before recording the data, all personal identification information was removed.
Informed consent
Written informed consent for use of pathological specimens and imaging data for research purposes was obtained from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Horiuchi, Y., Tokai, Y., Yamamoto, N. et al. Additive Effect of Magnifying Endoscopy with Narrow-Band Imaging for Diagnosing Mixed-Type Early Gastric Cancers. Dig Dis Sci 65, 591–599 (2020). https://doi.org/10.1007/s10620-019-05762-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05762-9