Abstract
Background
Declining Helicobacter pylori (H. pylori) eradication rates have prompted a switch in first-line therapy from standard triple (PPI, clarithromycin, and amoxicillin) to bismuth-based quadruple therapy. A caveat of the ACG 2017 H. pylori treatment guidelines was a paucity of recent US eradication data.
Aim
To determine Rhode Island H. pylori eradication data, in the largest US study from the last two decades.
Methods
Electronic records were queried for patients with H. pylori infection diagnosed by pathology, urea breath test, or stool antigen from 2015 to 2017. Demographics, diagnostic test, treatment regimen, and test of cure were extracted. Eradication rates were calculated, and treatment regimens were compared.
Results
A total of 1710 patients were identified (64% female): 825 (46%) diagnosed by breath test, 755 (42%) by biopsy, and 191 (12%) by stool antigen. Full data were obtained on 1101 patients. Seven regimens were used: quadruple (64%), triple (25%), doxycycline quadruple (5%), and miscellaneous (6%). Quadruple was superior to triple: (85% vs. 75%, P = 0.002), quadruple 14 days versus triple 14 days (87% vs. 79%, P = 0.0052), quadruple 10 days versus triple 10 days (77% vs. 67%, P = 0.33). Increased therapy length improved eradication (quadruple 14 days vs. 10 days, 87% vs. 77%, P = 0.002; triple 14 days versus 10 days 79% vs. 67%, P = 0.13). Finally, substituting doxycycline for tetracycline yielded lower eradication (85% vs. 67%, P = 0.006).
Conclusion
Quadruple therapy is superior to triple therapy within the Rhode Island population. Fourteen-day therapy achieves superior eradication compared to 10-day therapy, and doxycycline is inferior to tetracycline for quadruple therapy. Our findings support adherence to ACG and international guidelines advising 14-day quadruple therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori) has a well-established role in the etiology of gastroduodenal ulcers, gastritis, and gastric malignancies. Prompt eradication of H. pylori has been shown to be the most cost-effective long-term management strategy to prevent ulcer recurrence and has long been considered the standard of care [1, 2]. However, emerging antibiotic resistance has resulted in changes regarding the selection of optimal therapy for H. pylori infection [3, 4].
Declining H. pylori eradication rates and rising antibiotic resistance rates worldwide have prompted authorities such as the American College of Gastroenterology (ACG), the European Helicobacter and Microbiota study group, and a group of Canadian experts (the Toronto consensus) to recommend quadruple therapy as one of the first-line choices over the commonly used clarithromycin-based triple regimen [4,5,6]. A major caveat in the development of the ACG 2017 guidelines was acknowledged to be a paucity of USA-based eradication data from the last two decades. For example, back in 2000 Laine et al. [7] published a three-center double-blind trial with 448 patients which reported 84% eradication with 10-day triple therapy. Vakil et al. in 2004 published an eradication rate of 7-day triple therapy of 77% in 803 patients [8]. These are among the largest USA studies published in the last twenty years, none of which evaluated the currently recommended first-line bismuth quadruple therapy. This deficit prompted us to examine H. pylori eradication results in our local population of Rhode Island. Our objective was to evaluate whether first-line quadruple therapy was actually supported by a large series of cases from the USA, as recommended in the ACG 2017 guidelines [4].
Methods
The electronic medical records and separate pathology databases of the two major Rhode Island academic hospitals (Rhode Island Hospital and The Miriam Hospital) were queried for patients with H. pylori infection diagnosed by endoscopic biopsy, urea breath test (UBT), or stool antigen testing during calendar years 2015, 2016, and 2017. Basic demographic information, diagnostic test result, treatment regimen, and test of cure (TOC) results were collected. For comparing the collected patients’ characteristics, we used ANOVA for age, Chi-square for sex and ethnicity, and Fisher’s exact for TOC. Finally, we calculated eradication rates for commonly used regimens and analyzed results with adjustment for multiple variables (age, gender, ethnicity, and whether or not TOC was performed at least 4 weeks after finishing therapy) using logistic regression models. The data were analyzed in JMP® (SAS institute) software, and the study was approved by the local institutional review board.
Results
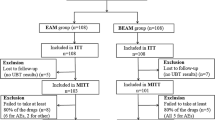
A total of 1710 patients were identified, of which 1094 were female (64%) and 616 were male (36%). A total of 825 patients (46%) were diagnosed by UBT, 755 (42%) by endoscopic biopsy, and 191 (12%) by stool antigen testing. Complete data required to calculate eradication rates were obtained for 1101 patients where treatment regimen, duration of therapy, and TOC were all documented (Fig. 1). Seven different treatment regimens were utilized. Sixty-four percentage of cases employed quadruple therapy (tetracycline, metronidazole, proton pump inhibitor, and a bismuth salt), 25% used triple therapy (proton pump inhibitor, clarithromycin, amoxicillin), 5% used quadruple therapy with doxycycline in place of tetracycline, and in 6% of cases, miscellaneous regimens were prescribed (e.g., levofloxacin-based triple, metronidazole-based triple, or levofloxacin sequential therapy). Patient demographics are shown in Table 1. Among the TOC, the most common method utilized was the breath test (60%), followed by stool antigen testing (36%), with only 4% of patients undergoing repeat endoscopy (Table 2). Overall, 85.6% of patients had their TOC performed at least four weeks after finishing eradication therapy. This proportion of patients was not significantly different across the different treatment groups (Table 3). For the remaining patients, we were not able to determine whether TOC was performed at least four weeks post-eradication therapy.
Eradication rates for each regimen are shown in Fig. 2, and with statistical comparisons given in Table 4, demonstrating the overall superiority of bismuth quadruple therapy compared to triple therapy (82% vs. 73%, P = 0.002). We compared the eradication efficacy of various treatment regimens including quadruple 14 days versus triple 14 days (eradication 87% vs. 79%, P = 0.006) and quadruple 10 days versus triple 10 days (77% vs. 67%, P = 0.33). Increased duration of therapy yielded statistically significantly higher eradication rates for quadruple therapy (quadruple 14 vs. 10 days, 87% vs. 77%, P = 0.005), though this was not statistically significant when comparing triple 14 days versus 10 days (79% vs. 67%, P = 0.33). No significant trends in eradication were noted across the three-year time frame for each regimen and no difference for age, gender, and ethnicity between eradicated versus non-eradicated group. Finally, substituting doxycycline for tetracycline resulted in lower eradication rates (82% vs. 70%, P = 0.006) for a 14-day regimen. In comparison with doxycycline 10-day therapy although the tetracycline group had higher eradication rates, this was not statistically significant (77% vs. 67%, P = 0.07).
Discussion
In the Rhode Island local population, quadruple therapy was clearly superior to triple therapy. A longer 14-day regimen of quadruple therapy yielded statistically significant increases in eradication rates when compared with a 10-day regimen. Doxycycline is sometimes prescribed instead of tetracycline due to its lower cost and wider availability (this was likely due to a temporary tetracycline shortage in the USA that lasted for several years prior to 2013, followed by higher pricing). Our results show that doxycycline is inferior to tetracycline when used as a part of quadruple therapy, and thus, we do not recommend this substitution if it can be avoided. This conclusion regarding doxycycline’s lack of efficacy compared with tetracycline is consistent with a recent study by Liou et al. [9] in Taiwan in which doxycycline sequential therapy achieved an eradication rate of only 58%. Our findings strongly support current ACG and international H. pylori eradication guidelines advising 14-day quadruple therapy as a first-line empiric regimen when local resistance profiles are not known [4,5,6].
Our study reflects usual clinical practice and is based on a large number of patients compared with previous studies performed over the last decade in the USA [4]. Other recently reported series have far fewer cases. For example, in a single-center retrospective chart review from El Paso, Texas, of 104 patients, slightly higher eradication rates were demonstrated with a 14-day triple therapy versus 10-day quadruple therapy (89% vs. 75%); however, the results were not found to be statistically significant [10]. Another single-center retrospective chart review from San Diego, California, of 131 patients reported higher eradication rates with quadruple therapy versus triple therapy (88% vs. 77%), results which again were not found to be statistically significant [11]. A very high 97% (per protocol) eradication rate with a 14-day combination of bismuth, metronidazole, tetracycline and omeprazole was reported by Salazar et al. [12] who studied 47 Hispanic patients in El Paso, Texas. Regarding clarithromycin-based triple therapy, a retrospective series of 156 patients from New Jersey [13], and of 662 patients at the University of Michigan (described briefly in reference 4) reported eradication rates of 84% from 2011 to 2017 and of 79.5% from 2001 to 2015, respectively. In contrast to these smaller series, our study is the largest from the USA for at least 20 years. It is likely the larger sample size, short duration of study of 3 years and multiple treatment regimens which generated the power to yield multiple statistically significant results.
The limitations of our study are similar to those of several previous recent reports of H. pylori eradication from the USA. These include its retrospective nature and the fact it was from the two major Rhode Island academic hospitals; thus, results may not necessarily represent local community practices or extrapolate to other areas of the country, especially if resistance rates vary geographically [14]. Continuing usage of a PPI can cause false-negative TOC results, and thus, a TOC should be performed at least 2 weeks after stopping these medications. Unfortunately, due to the fact that the patients had almost always been discharged when they underwent TOC and without accurate records of their outpatient prescriptions, we were not able to establish whether or not they had stopped their PPI appropriately 2 weeks before the TOC was performed. False-negative results would inflate apparent eradication rates but should theoretically be evenly distributed among the various treatment regimens and are therefore unlikely to preferentially influence comparisons of eradication rates across regimens. Similarly, since this was a retrospective study of clinical practice, there was no uniform method used to diagnose H. pylori infection, nor to confirm eradication. However, given the large number of patients in each group this would be unlikely to alter our study’s major findings. An additional issue is that the medical records in almost all cases failed to mention whether or not there had been any prior H. pylori treatment attempts. This limits our ability to categorize patients into subsets such as initial empiric therapy or subsequent treatment-refractory patients. The relatively small number of patients treated with doxycycline-based bismuth quadruple therapy could also be seen as a limitation of our study. However, due to the paucity of prior publications on doxycycline, we believe it is important to highlight our findings that while doxycycline remains much more affordable than tetracycline, it is much less effective. Only 79% of patients had a documented TOC, likely reflecting changes in US clinical practice as routine post-treatment testing for cure has only recently been recommended [4]. However, the demographic and treatment characteristics in this excluded subset of patients who did not have a test of cure were no different from those of the entire study cohort.
Additional potential limitations of our study include the lack data on medication adherence and on H. pylori antibiotic resistance in our patients. Resistance data would be very helpful complementary information given emerging widespread resistance globally to clarithromycin, metronidazole, and levofloxacin [14]. Unfortunately, unlike many other countries, there is a paucity of data on antibiotic resistance from USA H pylori strains. A consortium of 11 centers collected 347 stains from 1998 to 2002, reporting clarithromycin resistance in 13% and metronidazole resistance in 25% of them [15]. More recently, Shiota et al. reported rates of 16% for clarithromycin, 25% for metronidazole, and 31% for levofloxacin in 110 strains at the Houston, Texas Veterans Affairs Hospital, and Park et al. found clarithromycin resistance had exceeded 30% in 124 strains collected from four US geographic centers [16, 17]. In these studies, resistance to tetracycline and amoxicillin remains low, which is consistent with the literature from throughout the world.
Resistance testing is not routinely performed clinically in the USA; data on fewer than 1000 strains have been published this century and resistance testing was not available for the cases in our study either [15,16,17]. Further prospective research from various geographical locations throughout the USA is needed to better understand local and nationwide eradication rates. Correlation of eradication rates with local resistance patterns is an important next step, which would permit investigation of how resistance profiling, both individually and on a population level, could impact H. pylori treatment regimens and their efficacy. Nevertheless, the results of our retrospective large series of patients treated for H. pylori infection do strongly support recent guidelines recommending 14-day quadruple therapy as the best empiric choice for most patients.
Abbreviations
- ACG:
-
American College of Gastroenterology
- PPI:
-
Proton pump inhibitor
- TOC:
-
Test of cure
- UBT:
-
Urea breath test
References
NIH Consensus Conference. Helicobacter pylori in peptic ulcer disease. NIH consensus development panel on Helicobacter pylori in Peptic ulcer disease. JAMA. 1994;272:65–69.
McColl KEL. Clinical practice. Helicobacter pylori infection. N Engl J Med. 2010;362:1597–1604.
Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut. 2010;59:1143–1153.
Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of Helicobacter pylori infection. Am J Gastroenterol. 2017;112:212–239.
Malfertheiner P, Megraud F, O'Morain CA, et al. Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut. 2017;66:6–30.
Fallone CA, Chiba N, van Zanten SV, et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology. 2016;151:51.e14–69.e14.
Laine L, Fennerty MB, Osato M, et al. Esomeprazole-based Helicobacter pylori eradication therapy and the effect of antibiotic resistance: results of three US multicenter, double-blind trials. Am J Gastroenterol. 2000;95:3393–3398.
Vakil N, Lanza F, Schwartz H, Barth J. Seven-day therapy for Helicobacter pylori in the United States. Aliment Pharmacol Ther. 2004;20:99–107.
Liou J-M, Fang YJ, Chen CC, et al. Concomitant, bismuth quadruple, and 14-day triple therapy in the first-line treatment of Helicobacter pylori: a multicentre, open-label, randomised trial. Lancet. 2016;388:2355–2365.
Liu RP, Romero R, Sarosiek J, Dodoo C, Dwivedi AK, Zuckerman MJ. Eradication rate of Helicobacter pylori on the US-Mexico border using the urea breath test. South Med J. 2018;111:51–55.
Rubin J, Lai A, Dulai P, Gupta S, Crowe SE. Low rates of H. pylori eradication testing and cure rates in usual care (abstract). Gastroenterology. 2018;154:S-503–S-504.
Salazar CO, Cardenas VM, Reddy RK, Dominguez DC, Snyder LK, Graham DY. Greater than 95% success with 14-day bismuth quadruple anti- Helicobacter pylori therapy: a pilot study in US Hispanics. Helicobacter. 2012;17:382–390.
Nayar DS. Current eradication rate of Helicobacter pylori with clarithromycin-based triple therapy in a gastroenterology practice in the New York metropolitan area. Infect Drug Resist. 2018;11:205–211.
Savoldi A, Carrara E, Graham DY, Conti M, Tacconelli E. Prevalence of antibiotic resistance in Helicobacter pylori: a systematic review and meta-analysis in World Health Organization regions. Gastroenterology. 2018;155:1372.e17–1382.e17.
Duck WM, Sobel J, Pruckler JM, et al. Antimicrobial resistance incidence and risk factors among Helicobacter pylori-infected persons, United States. Emerg Infect Dis. 2004;10:1088–1094.
Shiota S, Reddy R, Alsarraj A, El-Serag HB, Graham DY. Antibiotic resistance of Helicobacter pylori among male United States veterans. Clin Gastroenterol Hepatol. 2015;13:1616–1624.
Park JY, Dunbar KB, Mitui M, et al. Helicobacter pylori Clarithromycin resistance and treatment failure are common in the USA. Dig Dis Sci. 2016;61:2373–2380.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the manuscript. Dr. SFM conceived and supervised the study and Drs. MAA and SFM wrote the IRB proposal. Dr. MAA, Dr. ECV and Dr. GA-G performed chart review and data collection. Dr. KS and Dr. MAA performed all statistical analysis with input from Dr. SFM., Dr. MAA, and Dr. ECV wrote the initial draft of the manuscript with critical input from Dr. SFM and all other listed authors. Each author read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr Moss receives grant support from American Molecular Laboratories for an unrelated clinical study. There were no other financial, professional, or personal conflicts of interests to declare on behalf of all authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alsamman, M.A., Vecchio, E.C., Shawwa, K. et al. Retrospective Analysis Confirms Tetracycline Quadruple as Best Helicobacter pylori Regimen in the USA. Dig Dis Sci 64, 2893–2898 (2019). https://doi.org/10.1007/s10620-019-05694-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05694-4