Abstract
Background
Many diseases have been associated with intestinal microbial dysbiosis. Host–microbial interactions regulate immune function, which influences the development of gastric cancer.
Aims
The aims were to investigate the characteristics of intestinal microbiota composition in gastric cancer patients and correlations between the intestinal microbiota and cellular immunity.
Methods
Fecal samples were collected from 116 gastric cancer patients and 88 healthy controls from Shanxi Province, China. The intestinal microbiota was investigated by 16S rRNA gene sequencing. Peripheral blood samples were also collected from the 66 gastric cancer patients and 46 healthy controls. The populations of peripheral T lymphocyte subpopulations and NK cells were analyzed by flow cytometry.
Results
The intestinal microbiota in gastric cancer patients was characterized by increased species richness, decreased butyrate-producing bacteria, and the enrichment of other symbiotic bacteria, especially Lactobacillus, Escherichia, and Klebsiella. Lactobacillus and Lachnospira were key species in the network of gastric cancer-associated bacterial genera. The combination of the genera Lachnospira, Lactobacillus, Streptococcus, Veillonella, and Tyzzerella_3 showed good performance in distinguishing gastric cancer patients from healthy controls. There was no significant difference in enterotype distribution between healthy controls and gastric cancer patients. The percentage of CD3+ T cells was positively correlated with the abundance of Lactobacillus and Streptococcus, and CD3+ T cells, CD4+ T cells, and NK cells were associated with Lachnospiraceae taxa.
Conclusions
Our study revealed a dysbiotic intestinal microbiota in gastric cancer patients. The abundance of some intestinal bacterial genera was correlated with the population of peripheral immune cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is the second highest cause of cancer-related deaths in China. In 2015, 498,000 Chinese people died from gastric cancer, which accounted for 17.7% of all cancer-related deaths [1]. Although Helicobacter pylori has been acknowledged as the most important carcinogen in the stomach, it is regarded as the initial factor for progression to gastric cancer. When the gastric mucosa is in a state of atrophy, H. pylori eradication cannot prevent gastric cancer. Moreover, H. pylori is less abundant or absent in later steps of gastric carcinogenesis [2]. Recently, an increasing number of studies have shown that the gastric microbiota is substantially altered during the development of gastric cancer. However, the mechanisms underlying this observation warrant further study.
The relationship of the gut microbiota with diseases has been a research hot spot in recent years. The gut microbiome is considered the second genome in the human body. On the one hand, emerging studies have indicated that the intestinal microbiota is closely associated with many diseases including colorectal cancer, pancreatic cancer, type 2 diabetes, Parkinson’s disease, nephrolithiasis, and cardiovascular disease [3,4,5,6,7,8]. Although a study investigating the relationship between gastric cancer and the intestinal microbiota has not been reported so far, it is possible that an unbalanced intestinal microbiota regulates the immune response or tolerance, resulting in the occurrence of gastric disease. On the other hand, the intestinal microbiota influences anticancer efficacy [9]. The intestinal lumen is the downstream tract of the gastral cavity; therefore, gastric carcinogenesis may have a substantial impact on bacterial composition in the intestine. The first aim of this study was to profile the intestinal microbiota in gastric cancer patients. To date, several potential biomarkers have been identified for the detection of colorectal cancer, such as Clostridium symbiosum and Fusobacterium nucleatum [10, 11]. Similarly, we tried to identify fecal bacterial markers for the detection of gastric cancer. Additionally, interactions between the intestinal microbiota and the immune system occur constantly in human health and disease [12]. The second aim was to explore the correlations between the intestinal microbiota and peripheral immune cells.
Methods
Study Population
A total of 204 individuals, 88 healthy subjects and 116 patients with gastric cancer, were recruited from November 2017 to February 2018. Healthy subjects were recruited from Department of Health Examination Center, Shanxi Cancer Hospital. No abnormal findings were observed for all healthy subjects in medical examination reports. Gastric carcinoma was confirmed by pathological examination at Shanxi Cancer Hospital, and only patients with gastric adenocarcinoma were included in the study. Common exclusion criteria for all participants were as follows: other ethnicities except Han Chinese; age under 18 years; living in Shanxi Province for less than 10 years; exposure to antibiotics, probiotics, immunomodulators and acid blockers for the past month; history of gastrointestinal tract infections, such as Campylobacter and Salmonella, for the past month; presence of digestive diseases except gastric cancer; presence of type 2 diabetes, autoimmune diseases and other malignant tumors; and history of gastrointestinal tract surgery, chemoradiotherapy, and cholecystectomy. Eighty-eight healthy subjects were referred to as the healthy control group (HC), and one hundred and sixteen patients with gastric cancer were referred to as the gastric cancer group (GC). Informed consent was obtained from all individual participants included in the study. The study was approved by the Ethics Committee of the Shanxi Cancer Hospital and conducted at Shanxi Cancer Hospital.
Fecal and Blood Sample Collection
All 204 participants provided fecal samples, and 112 out of 204 participants provided peripheral blood samples. Fecal samples and blood samples were collected without any medical treatment. Samples were discarded if patients underwent surgery and were not diagnosed with gastric adenocarcinoma by postoperative pathological examination. All fresh fecal samples were obtained within 2 h after excretion and stored immediately at − 80 °C until analysis. Blood samples were immediately used for analyzing the populations of peripheral T lymphocyte subpopulations and natural killer (NK) cells.
Flow Cytometry Analysis
The populations of total T cells (CD45+CD3+), helper T cells (CD3+CD4+), cytotoxic T cells (CD3+CD8+), regulatory T cells (Treg cells, CD4+CD25hiCD127lo), and NK cells (CD45+CD3−CD16+CD56+) were analyzed. The following monoclonal antibodies were used: CD45-PerCP, CD3-FITC, CD4-APC, CD8-PE, CD16+CD56-PE, CD4-FITC, CD25-APC, and CD127-PE (Tongsheng, Beijing, China). Whole blood samples were labeled with the monoclonal antibodies above. The mixture was incubated for 15 min at room temperature in the dark and then lysed with 1 mL of erythrocyte lysing solution, followed by incubation for 10 min. The cells were analyzed by flow cytometry (BD Biosciences, Franklin Lakes, USA).
DNA Isolation and PCR Amplification
Microbial DNA was isolated from fecal samples using the E.Z.N.A.® Stool DNA Kit (Omega Biotek, Norcross, USA) according to the manufacturer’s instructions. The DNA concentration was measured by a NanoDrop 2000 UV–vis spectrophotometer (Thermo Scientific, Wilmington, USA). The V3–V4 variable regions of the 16S rRNA gene were amplified with primers 338F (5′-ACTCCTACGGGAGGCAGCAG-3′) and 806R (5′-GGACTACHVGGGTWTCTAAT-3′). The PCR conditions were as follows: 95 °C for 3 min, followed by 27 cycles of 95 °C for 30 s, 55 °C for 30 s, and 72 °C for 45 s, and a final step at 72 °C for 10 min. The PCR amplification products were further purified using QuantiFluor™-ST (Promega, USA). Paired-end reads (2 × 300) were generated from purified amplicons on an Illumina MiSeq platform (Illumina, San Diego, USA). The raw reads were deposited into the NCBI Sequence Read Archive database (Accession Number: SRP151498).
Bioinformatics and Statistical Analysis
Raw reads were filtered by Trimmomatic and merged by FLASH using the following criteria: (1) the reads were truncated with an average quality score < 20 based on a 50-base-pair (bp) sliding window; (2) the number of overlapped bp was higher than 10 and the mismatched rate was less than 2%; and (3) reads containing ambiguous bases were discarded. Sequences with 97% similarity were grouped into an operational taxonomic unit (OTU) using UPARSE (version 7.1). The taxonomy of 16S rRNA gene sequences was assigned by the RDP classifier algorithm (http://rdp.cme.msu.edu/) against the Silva128 16S rRNA database with a confidence threshold of 70%.
Taxon abundances were normalized using the least number of sequences among all groups of samples. Alpha diversity was defined as diversity within samples, which was analyzed using Mothur (version v.1.30.1). The community diversity and richness were described by the Shannon index and Sobs index, respectively. Beta diversity was defined as comparisons between groups among samples and assessed by principal coordinates analysis (PCoA) and analysis of similarities (ANOSIM). The permutation number in ANOSIM was 999. Linear discriminant analysis (LDA) effect size (LEfSe) was used to identify differentially abundant bacterial taxa associated with groups of participants. The LDA value threshold was set at 3.5. A microbial association network was constructed using NetworkX. The threshold of the Spearman correlation coefficient between taxa was 0.3. Bacterial community types were analyzed using the following methods. Intestinal bacterial clusters were formed by partitioning around medoids (PAM). Jensen–Shannon distance (JSD) was calculated according to the relative abundance of bacterial genera. The optimal cluster number was obtained by calculating the Calinski–Harabasz (CH) index. The Wilcoxon rank-sum test was used to analyze the dissimilarity between groups. Dissimilarity with a P value < 0.05 was considered statistically significant.
Results
Summarization of 16S rRNA Gene Sequencing Results
The characteristics of all participants are shown in Supplementary Table 1. A total of 10,895,559 reads were generated from 204 samples. The average number of reads per sample in HC and GC was 51,996 and 54,482, respectively, and no significant difference was observed (P = 0.074). Rarefaction curves displayed the sequencing depth per sample, which indicated that most bacterial species had been detected (Supplementary Figure 1). With the increasing number of samples, the numbers of total OTUs and shared OTUs showed stable trends in both groups (Supplementary Figure 2). Notably, the number of shared OTUs for all samples from GC was zero. Venn diagram analysis showed that 1034 OTUs were shared between HC and GC. Thirty-five unique OTUs existed in HC, and two hundred and forty unique OTUs existed in GC.
Alpha Diversity and Beta Diversity Analysis
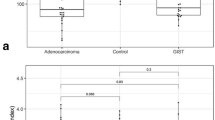
To assess the overall difference in intestinal microbiota composition between HC and GC, we conducted alpha diversity and beta diversity analyses. The Sobs index at the OTU level was significantly higher in GC than HC (Fig. 1a, P = 0.0019). The Shannon index at the OTU level did not differ between HC and GC (Fig. 1b, P = 0.1559). A PCoA plot based on unweighted UniFrac distance showed that although a small number of samples from HC overlapped with those from GC, mild separation between HC and GC was observed (Fig. 1c). Correspondingly, ANOSIM also showed a significant difference between HC and GC (R = 0.1322, P < 0.001, for unweighted UniFrac distance). A PCoA plot based on weighted UniFrac distances showed that samples from HC and GC mostly overlapped with one another (Fig. 1d). Correspondingly, ANOSIM showed no difference between HC and GC (R = 0.0138, P = 0.141, for weighted UniFrac distance). GC samples were more dispersed than HC samples in the PCoA plots. The alpha diversity and beta diversity analyses indicated that the microbiota differences between HC and GC resulted primarily from alterations in bacterial species richness.
Overall difference in the intestinal microbiota profiles between healthy controls and gastric cancer patients. Sob index (a) and Shannon index (b) at the OTU level in HC and GC. Principal coordinate analysis (PCoA) plots and analysis of similarity (ANOSIM) for c unweighted and d weighted UniFrac distances at the OTU level. Boxplots represent the interquartile range (IQR), and the line inside the boxplot represents the median. Whiskers below and above the box indicate the 10th and 90th percentiles, respectively. Black filled circles denote outliers beyond the whiskers. Red triangles and green circles denote samples from GC and HC, respectively. HC healthy control group, GC gastric cancer group, OTU operational taxonomic unit
To demonstrate that the difference was not caused by potential confounders, we performed age- and sex-matched comparisons of intestinal microbiota profiles between HC and GC (Supplementary Table 2). The results of the matched comparison resembled those of the comparison above (Supplementary Figure 3A, B, C, D). Furthermore, we compared the microbiota profiles of tumor stages, tumor sites and histological types in gastric cancer. No significant difference was observed.
Taxonomic Analysis and Enterotype Analysis
The bacterial community from 204 fecal samples was classified into 17 phyla, 30 classes, 57 orders, 106 families, and 312 genera. At the phylum level, the intestinal microbiota was dominated by Firmicutes, Bacteroidetes, and Proteobacteria (Fig. 2a). Compared with HC, GC had mainly increased Actinobacteria and Proteobacteria and reduced Firmicutes (Actinobacteria for HC vs GC: 0.6598% vs 1.654%, P = 0.0217; Proteobacteria: 2.61% vs 8.26%, P < 0.001; Firmicutes: 52.76% vs 43.44%, P < 0.001).
The compositional analysis of intestinal microbiota in healthy controls and gastric cancer patients. a Bacterial relative abundance at the phylum level for each fecal sample. Samples above the black line are from HC, and those above the red line are from GC. b The average relative abundance of intestinal microbiota at the genus level in HC and GC. HC healthy control group, GC gastric cancer group
At the genus level, the average relative abundance of intestinal microbiota in HC and GC is shown in Fig. 2b. Differentially abundant bacterial genera between HC and GC are shown in Supplementary Figure 4.
The intestinal microbiota genera from all fecal samples were separated into two clusters, which were referred to as enterotype 1 and enterotype 2 (Fig. 3a, b). Enterotype 1 was dominated by the Bacteroides genus, and enterotype 2 was dominated by the Prevotella_9 genus (Fig. 3c, d). There was no significant difference in enterotype distribution between HC and GC (Supplementary Table 3, P = 0.707).
The enterotype analysis for all fecal samples. a Microbial clusters were formed using partitioning around medoids (PAM). The optimal number of clusters was two using the Calinski–Harabasz (CH) criterion. b Two enterotype clusters at the genus level were visualized in a principal coordinate analysis (PCoA) plot. c, d Proportions of the dominant bacterial genera of each enterotype. HC healthy control group, GC gastric cancer group
Specific Bacterial Taxa Associated with Gastric Cancer and Potential Diagnostic Biomarkers of Gastric Cancer
To identify specific taxa associated with gastric cancer, we conducted LEfSe analysis. The 38 taxa were identified by LEfSe analysis, which included 3 phyla, 4 classes, 4 orders, 10 families, and 17 genera (Fig. 4). At the genus level, there were five bacterial genera depleted in GC, including Lachnoclostridium, [Eubacterium]_rectale_group, Roseburia, Lachnospira, and Faecalibacterium. There were 12 bacterial genera enriched in GC, including Prevotella_9, Escherichia–Shigella, Klebsiella, Lactobacillus, Streptococcus, Alistipes, Veillonella, Bifidobacterium, Ruminococcaceae_UCG-002, Christensenellaceae_R-7_group, Parabacteroides, and Prevotella_2. At the family level, Lachnospiraceae and Enterobacteriaceae were most worthy of consideration. First, their LDA values ranked first in GC-depleted and GC-enriched bacterial families, respectively (LDA values = 5.394 and 4.809, respectively). Second, four out of five GC-depleted genera were all assigned to the family Lachnospiraceae. Escherichia–Shigella and Klebsiella belonged to the family Enterobacteriaceae (Supplementary Table 4).
The most differentially abundant taxa between healthy controls and gastric cancer patients by linear discriminant analysis (LDA) effect size (LEfSe) analysis. Red bars indicate taxa enriched gastric cancer, and green bars indicate taxa depleted in gastric cancer. HC healthy control group, GC gastric cancer group
The results of the LEfSe analysis in the age-sex-matched subset are shown in Supplementary Figure 3E. Although the number of specific taxa associated with gastric cancer was slightly reduced perhaps due to a decrease in the number of samples, the majority of bacterial taxa strongly associated with gastric cancer were retained.
Furthermore, we conducted receiver operating characteristic (ROC) curve analysis to evaluate the performance of the 17 bacterial genera in discriminating between HC and GC. Lachnospira, Lactobacillus, and Streptococcus distinguished GC from HC with areas under the curve (AUCs) of 0.82, 0.86, and 0.81, respectively. In addition, Tyzzerella_3 distinguished GC from HC with an AUC of 0.84 (Fig. 5). Random forest analysis showed that the combination of Lactobacillus, Tyzzerella_3, Veillonella, Streptococcus, and Lachnospira distinguished GC from HC with an AUC of 0.95. In terms of relative abundance, Lactobacillus, Veillonella, and Streptococcus of GC increased by 58.92-fold, 32.38-fold, and 15.93-fold, respectively, and Lachnospira and Tyzzerella_3 decreased by 3.37-fold and 8.85-fold, respectively.
The performance of 4 bacterial genera in discriminating between GC and HC by receiver operating characteristic (ROC) curve analysis. a The discriminatory potential of Lactobacillus and Streptococcus, which were enriched in gastric cancer. b The discriminatory potential of Lachnospira and Tyzzerella_3, which were depleted in gastric cancer. HC healthy control group, GC gastric cancer group; AUC area under the curve
Microbial Association Network Analysis
To explore the interplay between GC-associated bacterial genera mentioned in LEfSe analysis, we constructed a microbial association network across populations. The network contained 16 nodes and 30 edges (Fig. 6). All correlations between GC-depleted and GC-enriched genera were negative. All correlations between GC-depleted genera were positive, and all correlations between GC-enriched genera were also positive. Lachnospira and Lactobacillus had the highest degree centrality among GC-depleted and GC-enriched genera, respectively. Lachnospira abundance was negatively correlated with Lactobacillus abundance (r = − 0.384, P < 0.001).
Microbial association network for gastric cancer-associated genera across populations. Nodes are colored by phylum. Red edges denote positive correlations and green edges denote negative correlations. Microbial correlation coefficients are all greater than 0.3 with statistical significance (P < 0.05)
Correlation Analysis Between Intestinal Microbiota and Peripheral Immune Cells
To explore the correlations between peripheral immune cells and intestinal microbiota, we created a correlation heatmap across populations (Fig. 7). At the genus level, the abundance of Lactobacillus was positively correlated with CD3+ T cell count (r = 0.209, P = 0.027). The abundance of Streptococcus was positively correlated with the CD3+ T cell count and negatively correlated with the NK cell count (CD3+ T cells, r = 0.19, P = 0.045; NK cells, r = − 0.223, P = 0.018, respectively). Lachnospiraceae taxa were associated with peripheral immune cells, in which the genera Lachnospiraceae_NK4A136_group and Lachnospiraceae_ND3007_group were positively correlated with NK cells and negatively correlated with CD3+ T cells and CD4+ T cells.
Correlation analysis between peripheral immune cells and intestinal microbiota. The label on the lower right shows that the intensity of the colors represents the correlative degree between the abundance of bacterial genera and the percentage of immune cells. Significance level is labeled with * (*P < 0.05, **P < 0.01, ***P < 0.001)
Additionally, we compared the distribution of CD3+ T cells, CD4+/CD8+ ratio, Treg cells, and NK cells between HC and GC, but no significant difference was observed (Supplementary Table 5).
Discussion
To the best of our knowledge, this is the first study by far to explore the intestinal microbial profiles in patients with gastric cancer and healthy subjects from Shanxi Province, China. The intestinal bacterial community of healthy subjects was dominated by the phyla Firmicutes, Bacteroidetes, and Proteobacteria, which was consistent with some previous studies from other regions [13, 14]. Two enterotypes were, respectively, dominated by Bacteroides and Prevotella_9, as described in a prior study [15].
The present case–control study showed that the intestinal microbiota in gastric cancer patients was distinct from that in healthy controls, which was primarily attributed to an increase in species richness. However, the intestinal bacterial diversity in gastric cancer was not markedly altered. The number of shared OTUs for all GC samples was zero, and fecal samples of gastric cancer patients were more dispersed in the PCoA plots, which both indicated that the intestinal microbiota in gastric cancer patients showed more intersubject variation. Again, this result suggested that the intestinal microbiota in gastric cancer patients was altered. Although age influenced the composition of intestinal microbiota, the microbiota dissimilarities between cases and controls were not nearly altered after adjusting for sex and age. The reason may be that the age distribution of the present study population was mainly between the ages of 40 and 70, and the intestinal microbiota composition in this age group was relatively stable. There was no significant difference in enterotype distribution between HC and GC. This result reveals that the enterotypes probably have less influence on gastric carcinogenesis. On the other hand, our group comparison results were not biased by enterotype distribution.
We identified 38 intestinal bacterial taxa closely associated with gastric cancer by LEfSe analysis. In gastric cancer, the Lachnospiraceae family and the Faecalibacterium genus were underrepresented. Some members of the Lachnospiraceae family and the Faecalibacterium genus are butyrate-producing bacteria. Butyrate not only provides energy for microbial and host epithelial cell growth but also protects against colitis and colorectal cancer by reducing inflammatory cytokine production, inducing tumor cell apoptosis, and activating antitumor immunity [16,17,18,19,20]. The family Lachnospiraceae diminishes substantially in inflammatory bowel disease (IBD) and familial adenomatous polyposis infection, supporting its protective role in the intestine [21, 22]. In contrast, studies on the gastric microbiota revealed an overabundance of Lachnospiraceae in gastric cancer [23, 24]. The present study showed that CD3+ T cells, CD4+ T cells, and NK cells were associated with Lachnospiraceae taxa. Detailed mechanistic studies focusing on the functional roles of Lachnospiraceae in multiple diseases are required. The genus Faecalibacterium includes the only known Faecalibacterium prausnitzii species, which is reduced in IBD [21].
Some commensal bacteria were overrepresented in gastric cancer. An enrichment in Enterobacteriaceae taxa was observed, including the genera Escherichia–Shigella and Klebsiella. Colibactin-producing Escherichia coli and Klebsiella pneumoniae can induce chronic inflammation and trigger DNA damage and mutation [25, 26]. The co-occurrence of polyketide synthase+E. coli and enterotoxigenic Bacteroides fragilis promotes the shift from familial adenomatous polyposis to colon cancer by inducing inflammation and damaging epithelial cell DNA [22]. A higher proportion of Escherichia–Shigella and K. pneumoniae was also observed in the gastric mucosa of gastric cancer patients. [23, 27]. Notably, the abundance of Lactobacillus from fecal samples of gastric cancer patients increased by 58.92-fold in our study. Various studies investigating the gastric microbiota have suggested that Lactobacillus has a tendency toward higher abundance in progressive histological stages of gastric carcinogenesis and a markedly higher proportion in gastric cancer patients [2, 23, 24, 28]. Therefore, we infer that an increase in Lactobacillus species in the intestinal lumen may partly result from the downward movement of Lactobacillus species from the upper digestive tract.
At present, the links between some microbes and diseases have been reported in many studies, but the effect of intestinal dysbacteriosis as a whole on patients with gastric cancer remains unclear. It is worth mentioning a study about Clostridium difficile infection by Antharam VC et al. It was thought that marked depletion of butyrate-producing bacteria including the families Lachnospiraceae and Ruminococcaceae may partly account for increased susceptibility to C. difficile infection [29]. In this regard, patients with gastric cancer may have an increased risk of enteric infections.
Our results showed that the combination of the genera Lactobacillus, Veillonella, Streptococcus, Lachnospira, and Tyzzerella_3 has the capacity to distinguish gastric cancer from control. Additionally, large fold changes in the relative abundance of Lactobacillus, Veillonella, Streptococcus, Lachnospira, and Tyzzerella_3 were observed in gastric cancer patients. These observations suggested that the genera Lactobacillus, Veillonella, Streptococcus, Lachnospira, and Tyzzerella_3 were used as potential markers for predicting gastric cancer. However, unlike the direct interactions between the intestinal microbiota and intestinal diseases, the association between gastric cancer and the intestinal microbiota is probably indirect. The differential taxa between GC and the HC are most likely dependent on the bacterial composition of the participants. Therefore, the bacterial genera that provide diagnostic clues for gastric cancer may be applicable only in native Shanxi people or other cohorts with similar bacterial composition.
Next, we analyzed the interplay between GC-associated bacterial genera. In the network analysis, Lactobacillus, Streptococcus, and Veillonella were positively and strongly correlated with one another with robust statistical significance (Lactobacillus—Streptococcus: r = 0.42, P < 0.001; Lactobacillus–Veillonella: r = 0.34, P < 0.001; Streptococcus–Veillonella: r = 0.57, P < 0.001). These three genera were probably interactive and interdependent to a high degree. In addition, our study showed that the percentage of CD3+ T cells was positively correlated with the abundance of Lactobacillus and Streptococcus. Lactobacillus and Lachnospira were key species among GC-enriched and GC-depleted genera, respectively, and they were negatively correlated with each other with robust statistical significance. These findings suggest that Lachnospira and Lactobacillus may play vital roles in the alterations to the intestinal microbiota in gastric cancer patients. As a result, Lachnospira and Lactobacillus may be important targets for restoring the homeostasis of the intestinal bacterial community in patients with gastric cancer.
Like other microbial studies, a key question remains as to whether intestinal bacterial dysbiosis is the cause or the consequence of gastric cancer. One hypothesis is that intestinal dysbiosis results from noncancer factors and subsequently contribute to the occurrence of gastric cancer. This hypothesis may need to be verified by animal models. Another hypothesis is that gastric carcinogenesis results in intestinal dysbiosis. In our opinion, intestinal bacterial dysbiosis is probably the consequence of gastric cancer. First, it has been suggested that proton pump inhibitors alter the intestinal microbiota by suppressing acid production [30, 31]. Gastric carcinogenesis also reduces gastric acid secretion due to gastric gland atrophy. Therefore, the microbiota dysbiosis in gastric cancer patients may be associated with changes in gastric acid secretion. Second, a dysbiotic microbial community, once established, substantially affects the landscape of immune cells [32]. The cross-regulation between the immune system and the intestinal microbiota may aggravate existing dysbiosis in gastric cancer patients. In our study, there was no significant difference in peripheral T cell subpopulations and NK cells between cases and controls. It may be more important to analyze the distribution of local immune cells, which directly interact with the intestinal microbiota.
It is universally acknowledged that there are marked differences in the intestinal microbial profiles between enterotypes. The major advantage of our study is that the enterotypes were matched when the intestinal microbiota of patients with gastric cancer and healthy controls were compared. However, there are several limitations to our study. First, serum concentrations of cytokines have not been measured to explore the possible interplay between serum cytokines and the intestinal microbiota in gastric cancer. Second, the intestinal candidate biomarkers were not validated further in other cohorts. Third, the biological effects of microbes are strain specific, but 16S rRNA gene sequencing usually enables taxonomic identification down to the genus level. Most species-level bacteria are not identified, let alone strains. The effect of intestinal dysbacteriosis on patients with gastric cancer needs to be explored in depth via the application of metagenomics and metabolomics.
In conclusion, our study revealed a dysbiotic intestinal microbiota in patients with gastric cancer. Butyrate-producing bacteria were underrepresented, and proinflammatory bacteria, such as Escherichia–Shigella and Klebsiella, were overabundant. The abundance of some intestinal bacterial genera was correlated with the population of peripheral immune cells. It will be more helpful to explore the intestinal diagnostic biomarkers of gastric cancer by studying the characteristics of gastric and intestinal microbiota composition simultaneously in patients with gastric cancer. Ultimately, intestinal microbial community profiling will deepen the understanding of gastric carcinogenesis, providing novel insights for the diagnosis and treatment of gastric cancer.
References
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115–132.
Ferreira RM, Pereira-Marques J, Pinto-Ribeiro I, et al. Gastric microbial community profiling reveals a dysbiotic cancer-associated microbiota. Gut. 2018;67:226–236.
Hibberd AA, Lyra A, Ouwehand AC, et al. Intestinal microbiota is altered in patients with colon cancer and modified by probiotic intervention. BMJ Open Gastroenterol. 2017;4:e145.
Pushalkar S, Hundeyin M, Daley D, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 2018;8:403–416.
Zhao L, Zhang F, Ding X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359:1151–1156.
Sampson TR, Debelius JW, Thron T, et al. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson’s disease. Cell. 2016;167:1469–1480.
Ticinesi A, Milani C, Guerra A, et al. Understanding the gut-kidney axis in nephrolithiasis: an analysis of the gut microbiota composition and functionality of stone formers. Gut. 2018;2017:315–734.
Brown JM, Hazen SL. Microbial modulation of cardiovascular disease. Nat Rev Microbiol. 2018;16:171–181.
Roy S, Trinchieri G. Microbiota: a key orchestrator of cancer therapy. Nat Rev Cancer. 2017;17:271–285.
Xie YH, Gao QY, Cai GX, et al. Fecal Clostridium symbiosum for noninvasive detection of early and advanced colorectal cancer: test and validation studies. EBioMedicine. 2017;25:32–40.
Dai Z, Coker OO, Nakatsu G, et al. Multi-cohort analysis of colorectal cancer metagenome identified altered bacteria across populations and universal bacterial markers. Microbiome. 2018;6:70.
Geuking MB, Köller Y, Rupp S, McCoy KD. The interplay between the gut microbiota and the immune system. Gut Microbes. 2014;5:411–418.
Li K, Dan Z, Gesang L, et al. Comparative analysis of gut microbiota of native Tibetan and Han populations living at different altitudes. PLoS ONE. 2016;11:e155863.
Allali I, Boukhatem N, Bouguenouch L, et al. Gut microbiome of moroccan colorectal cancer patients. Med Microbiol Immunol. 2018;207:211–225.
Costea PI, Hildebrand F, Arumugam M, et al. Enterotypes in the landscape of gut microbial community composition. Nat Microbiol. 2018;3:8–16.
Meehan CJ, Beiko RG. A phylogenomic view of ecological specialization in the Lachnospiraceae, a family of digestive tract-associated bacteria. Genome Biol Evol. 2014;6:703–713.
Zhou L, Zhang M, Wang Y, et al. Faecalibacterium prausnitzii produces butyrate to maintain Th17/Treg balance and to ameliorate colorectal colitis by inhibiting histone deacetylase 1. Inflamm Bowel Dis. 2018;12:S110–S111.
McIntyre A, Gibson PR, Young GP. Butyrate production from dietary fibre and protection against large bowel cancer in a rat model. Gut. 1993;34:386–391.
Roy MJ, Dionne S, Marx G, et al. In vitro studies on the inhibition of colon cancer by butyrate and carnitine. Nutrition. 2009;25:1193–1201.
Perrin P, Cassagnau E, Burg C, et al. An interleukin 2/sodium butyrate combination as immunotherapy for rat colon cancer peritoneal carcinomatosis. Gastroenterology. 1994;107:1697–1708.
Berry D, Reinisch W. Intestinal microbiota: a source of novel biomarkers in inflammatory bowel diseases? Best Pract Res Clin Gastroenterol. 2013;27:47–58.
Dejea CM, Fathi P, Craig JM, et al. Patients with familial adenomatous polyposis harbor colonic biofilms containing tumorigenic bacteria. Science. 2018;359:592–597.
Wang L, Zhou J, Xin Y, et al. Bacterial overgrowth and diversification of microbiota in gastric cancer. Eur J Gastroenterol Hepatol. 2016;28:261–266.
Aviles-Jimenez F, Vazquez-Jimenez F, Medrano-Guzman R, Mantilla A, Torres J. Stomach microbiota composition varies between patients with non-atrophic gastritis and patients with intestinal type of gastric cancer. Sci Rep. 2014;4:4202.
Cuevas-Ramos G, Petit CR, Marcq I, Boury M, Oswald E, Nougayrede JP. Escherichia coli induces DNA damage in vivo and triggers genomic instability in mammalian cells. Proc Natl Acad Sci USA. 2010;107:11537–11542.
Kaur CP, Vadivelu J, Chandramathi S. Impact of Klebsiella pneumoniae in lower gastrointestinal tract diseases. J Dig Dis. 2018;19:262–271.
Jo HJ, Kim J, Kim N, et al. Analysis of gastric microbiota by pyrosequencing: minor role of bacteria other than Helicobacter pylori in the gastric carcinogenesis. Helicobacter. 2016;21:364–374.
Coker OO, Dai Z, Nie Y, et al. Mucosal microbiome dysbiosis in gastric carcinogenesis. Gut. 2018;67:1024–1032.
Antharam VC, Li EC, Ishmael A, et al. Intestinal dysbiosis and depletion of butyrogenic bacteria in Clostridium difficile infection and nosocomial diarrhea. J Clin Microbiol. 2013;51:2884–2892.
Jackson MA, Goodrich JK, Maxan ME, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016;65:749–756.
Imhann F, Bonder MJ, Vich VA, et al. Proton pump inhibitors affect the gut microbiome. Gut. 2016;65:740–748.
Gao F, Li M, Liu Y, Gao C, Wen S, Tang L. Intestinal dysbacteriosis induces changes of T lymphocyte subpopulations in Peyer’s patches of mice and orients the immune response towards humoral immunity. Gut Pathog. 2012;4:19.
Acknowledgments
This study was funded by the National Natural Science Foundation of China (Grant Numbers: 81272696) and the Special Foundation for Talents of Shanxi Province of China (Grant Numbers: 201705D211021). We thank AJE (www.aje.com) for its linguistic assistance during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10620_2018_5411_MOESM1_ESM.tif
Supplementary Figure 1. Rarefaction curves of the number of OTUs versus the number of reads. The x-axis shows the number of OTUs; the y-axis shows the number of reads sampled randomly. HC, healthy control group; GC, gastric cancer group, OTUs, operational taxonomic units (TIFF 3379 kb)
10620_2018_5411_MOESM2_ESM.tif
Supplementary Figure 2. The plots of the number of total OTUs (A) and the number of shared OTUs (B) versus the number of samples. HC, healthy control group; GC, gastric cancer group (TIFF 892 kb)
10620_2018_5411_MOESM3_ESM.tif
Supplementary Figure 3. Comparison of intestinal microbiota composition between healthy controls and gastric cancer patients in the sex-age-matched subset. Sob index (A) and Shannon index (B) at the OTU level in HC and GC. Principal coordinate analysis (PCoA) plots and analysis of similarity (ANOSIM) for (C) unweighted and (D) weighted UniFrac distances at the OTU level. (E) The most differentially abundant taxa between HC and GC by linear discriminant analysis (LDA) effect size (LEfSe) analysis. HC, healthy control group; GC, gastric cancer group (TIFF 4123 kb)
10620_2018_5411_MOESM4_ESM.tif
Supplementary Figure 4. The top 30 differentially abundant genera of bacteria between HC and GC by Wilcoxon rank-sum test. The left panel shows the average relative abundance of bacterial genera in both groups. The right panel shows 95% confidence intervals and P values. HC, healthy control group; GC, gastric cancer group (TIFF 2955 kb)
Rights and permissions
About this article
Cite this article
Qi, Yf., Sun, Jn., Ren, Lf. et al. Intestinal Microbiota Is Altered in Patients with Gastric Cancer from Shanxi Province, China. Dig Dis Sci 64, 1193–1203 (2019). https://doi.org/10.1007/s10620-018-5411-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5411-y